Smoking Awareness and Intention to Quit Smoking in Smoking Female Workers: Secondary Data Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Study Participants and Data Collection
2.3. Instruments
2.3.1. Intention to Quit Smoking
2.3.2. Smoking Awareness
2.3.3. Demographic, Occupational, and Smoking-Related Characteristics
2.4. Ethical Consideration
2.5. Data Analysis
3. Results
3.1. Demographic, Occupational, and Smoking-Related Characteristics
3.2. Differences in Intention to Quit Smoking according to Demographic, Occupational, and Smoking-Related Characteristics
3.3. Correlation between Smoking Awareness and Intention to Quit Smoking
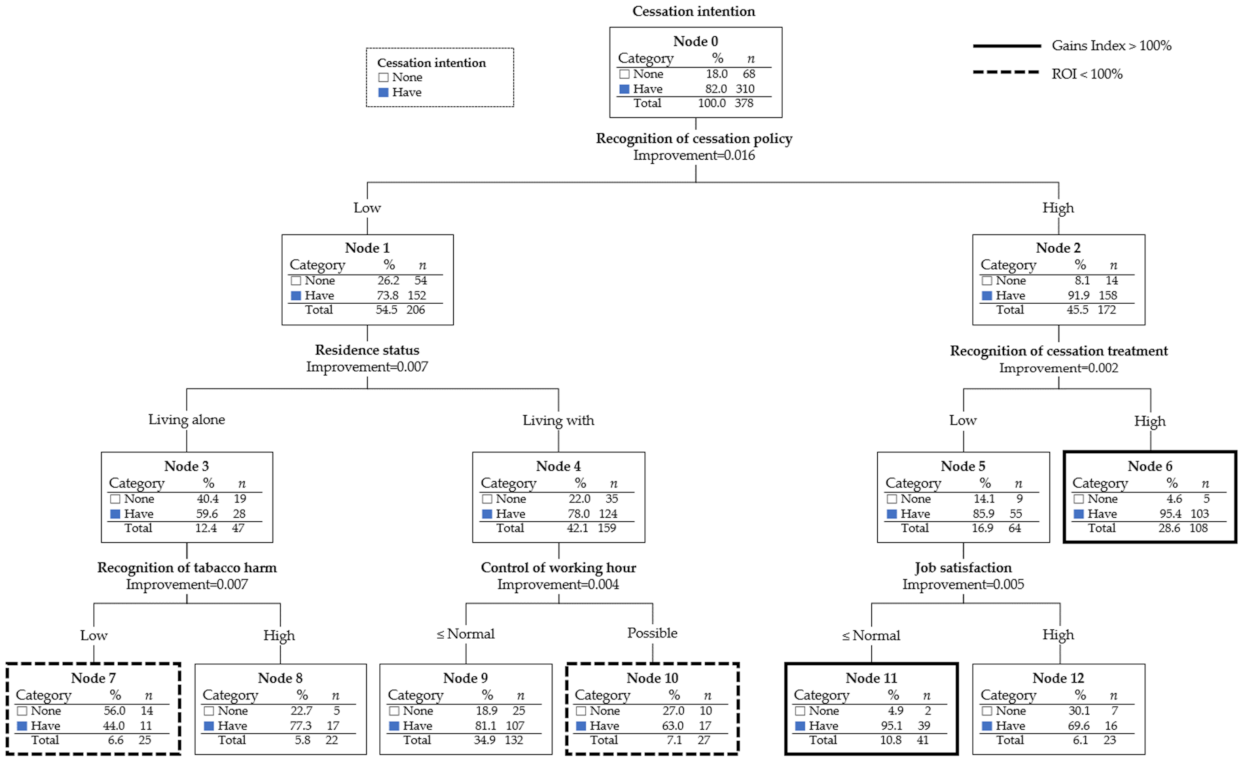
3.4. Decision Tree for Intention to Quit Smoking
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Korea Center for Disease Control and Prevention. National Health Statistics: The Seventh Korea National Health and Nutrition Examination Survey; Ministry of Health and Welfare: Sejong, Korea, 2019. [Google Scholar]
- Jeong, G.C. Development of the Perception Scale of Tobacco ⦁ Smoking by Population Group; Korea Health Promotion Institute Reserch Report (No. Research-04-2020-020-01); Korea Health Promotion Institute: Seoul, Korea, 2020. [Google Scholar]
- Sreeramareddy, C.T.; Pradhan, P.M.S. Prevalence and social determinants of smoking in 15 countries from North Africa, Central and Western Asia, Latin America and Caribbean: Secondary data analyses of demographic and health surveys. PLoS ONE 2015, 10, e0130104. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.N.; Furst, R.T. Stigma and outdoor smoking breaks: Self-perceptions of outdoor smokers in Manhattan. Soc. Theory Health 2016, 14, 275–292. [Google Scholar] [CrossRef]
- Lee, E.H.; Shin, S.R. Female Smoking Experience Illuminated from a Gender-Perspective. J. Qual. Res. 2020, 21, 75–84. [Google Scholar] [CrossRef]
- Suh, K.H. Updates in the Smoking and Smoking Cessation of Korean Women. Korean J. Health Psychol. 2007, 12, 695–713. [Google Scholar]
- Kang, J.W. An Analysis on Multi-Level Factors Related to Employees’ Smoking and Smoking Cessation Using a Mixed Method; Ewha Womans University, Department of Health Convergenc: Seoul, Korea, 2019. [Google Scholar]
- Park, A.H.; Choi, J.H.; Kim, H.K. Smoking characteristics and motivational strategies in cessation interventions for female smokers. Korean J. Health Educ. Promot. 2020, 37, 29–42. [Google Scholar] [CrossRef]
- Hughes, J.R. Motivating and helping smokers to stop smoking. J. Gen. Intern. Med. 2003, 18, 1053–1057. [Google Scholar] [CrossRef]
- Prochaska, J.O.; DiClemente, C.C. Stages and processes of self-change of smoking: Toward an integrative model of change. J. Consult. Clin. Psychol. 1983, 51, 390. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Noh, Y.M.; Lee, Y.J.; Kim, J.Y.; Noh, J.W. Factors Affecting Intention to Quit Smoking of Current Smokers by Gender. J. Korea Contents Assoc. 2019, 19, 321–328. [Google Scholar] [CrossRef]
- Kim, J.S.; Yu, J.O.; Kim, M.S. Factors Contributing to the Intention to Quit Smoking in Community-dwelling Elderly Smokers. J. Korean Acad. Community Health Nurs. 2012, 23, 358–365. [Google Scholar] [CrossRef][Green Version]
- Park, K.Y. Predictors of Intention to Quit Smoking among Woman Smokers in Korea. J. Korean Acad. Fundam. Nurs. 2014, 21, 253–263. [Google Scholar] [CrossRef]
- Jung-Choi, K.-H.; Khang, Y.-H.; Cho, H.-J. Hidden female smokers in Asia: A comparison of self-reported with cotinine-verified smoking prevalence rates in representative national data from an Asian population. Tob. Control 2012, 21, 536–542. [Google Scholar] [CrossRef]
- Oh, M.Y. Influence of Smoking Perception and Attitude on the Image of Tobacco Company and the Perception of Its CSR Activities. Speech Commun. 2010, 13, 145–183. [Google Scholar]
- Kang, L.J.; Kim, H.S. Risk and Protective Factors Related to CigaretteSmoking among Korean Male High School Students. Consum. Cult. Res. 2005, 8, 121–142. [Google Scholar]
- Lee, K.J.; Lee, H.J.; Oh, K.J. Using fuzzy-neural network to predict hedge fund survival. J. Korean Data Inf. Sci. Soc. 2015, 26, 1189–1198. [Google Scholar] [CrossRef]
- Kang, S.H.; Choi, S.H. Group classification on management behavior of diabetic mellitus. J. Korea Acad.-Ind. Coop. Soc. 2011, 12, 765–774. [Google Scholar] [CrossRef]
- Shin, S.H. Analysis of subgroups with lower level of patient safety perceptions using decision-tree analysis. J. Korean Acad. Nurs. 2020, 50, 686–698. [Google Scholar] [CrossRef]
- Shin, S.R.; Jeong, G.C. Predictive Variables on Intention to Stay as a Nonsmoker Based on Educational Environment Related Factors. Health Soc. Sci. 2007, 21, 5–24. [Google Scholar]
- Siahpush, M.; McNeill, A.; Borland, R.; Fong, G. Socioeconomic variations in nicotine dependence, self-efficacy, and intention to quit across four countries: Findings from the International Tobacco Control (ITC) Four Country Survey. Tob. Control 2006, 15, iii71–iii75. [Google Scholar] [CrossRef]
- Lee, S.E.; Kim, C.-W.; Im, H.-B.; Park, J.A.; Lee, T.-Y.; Bae, J.E.; Lee, S.-Y. Factors associated with success of smoking cessation services among female emotional laborers over a 6 month period. Korean J. Health Educ. Promot. 2019, 36, 15–21. [Google Scholar] [CrossRef]
- Lee, S. The effects of job characteristics on smoking and mediating effects of job stress among older workers. Korean J. Health Educ. Promot. 2014, 31, 51–61. [Google Scholar] [CrossRef]
- Park, H.J.; Jung, H.S. Health behaviors by job stress level in large-sized company with male and female workers. J. Korean Acad. Nurs. 2010, 40, 852–862. [Google Scholar] [CrossRef]
- Kim, Y.S.; Jo, H.S. Smoking behavior and related factors of female smokers from public health center in Incheon. Korean J. Health Educ. Promot. 2008, 25, 125–138. [Google Scholar]
- Zaatari, G.S.; Bazzi, A. Impact of the WHO FCTC on non-cigarette tobacco products. Tob. Control 2019, 28, s104–s112. [Google Scholar] [CrossRef]
- Amul, G.G.H.; Pang, T. The state of tobacco control in ASEAN: Framing the implementation of the FCTC from a health systems perspective. Asia Pac. Policy Stud. 2018, 5, 47–64. [Google Scholar] [CrossRef]
- Shin, J.S.; Kim, Y.K. Female Smokers’ Experiences of the Process of Smoking Cessation Attempts. Acad. Qual. Res. 2018, 19, 142–155. [Google Scholar] [CrossRef]
- Kim, E.Y.; Seo, H.G.; Kim, Y.; Choi, Y.J.; Fong, G.T.; Yan, M.; Driezen, P. Change of Support for Smoke-Free Area and Perception of Effectiveness of Smoking Ban Policy among Korean Smokers: Findings from the 2010, 2016 International Tobacco Control Policy Evaluation Survey in Korea. J. Korean Soc. Res. Nicotine Tob. 2018, 9, S39–S50. [Google Scholar] [CrossRef][Green Version]
- Kim, J.S.; Kang, S.J.; Kim, D.J.; Choi, I.Y.; Choi, B.S. Success factors of new enrollees at smoking cessation clinics in the nationwide public health centers in Korea based on gender differences. Korean Public Health Res. 2018, 44, 17–30. [Google Scholar]
- Kwak, M.Y.; Hwang, E.J. The effects of smoking cessation coaching program based on motivation stage to stop smoking of patients at a public hospital. J. Korea Acad. -Ind. Coop. Soc. 2016, 17, 188–198. [Google Scholar] [CrossRef]
- Kim, Y.J. Comparison of health practices between single-and multiple-member households by gender in Korean adults. J. Korean Public Health Nurs. 2009, 23, 219–231. [Google Scholar]
- Kim, M.A.; Choi, S.E.; Moon, J.H. Effect of heath behavior, physical health and mental health on heath-related quality of life in middle aged women: By using the 2014 Korea Health Panel Data. J. Korean Acad. Soc. Home Health Care Nurs. 2019, 26, 72–80. [Google Scholar] [CrossRef]
- Kim, E.G.; Park, S.K. Comparison of health behaviors, disease prevalence between one-person women and multiple households women in Korea. J. Korean Public Health Nurs. 2016, 30, 483–494. [Google Scholar] [CrossRef]
- O’Leary, R.; Polosa, R. Tobacco harm reduction in the 21st century. Drugs Alcohol Today 2020, 20, 219–234. [Google Scholar] [CrossRef]
- Zeller, M.; Hatsukami, D. The Strategic Dialogue on Tobacco Harm Reduction: A vision and blueprint for action in the US. Tob. Control 2009, 18, 324–332. [Google Scholar] [CrossRef]
- Warner, K.E. How to think—not feel—about tobacco harm reduction. Nicotine Tob. Res. 2019, 21, 1299–1309. [Google Scholar] [CrossRef]
- Sun, P.H. Survey on the perception of electronic cigarette. Tob. Forum 2018, 17, 18–36. [Google Scholar]
- Kim, J.E.; Chung, H.E.; Nam, Y.J. A study on the current status of female single-person households for policy improvement: Focusing on Gyeonggi province with secondary data analyses. Korean J. Fam. Welf. 2018, 23, 463–488. [Google Scholar] [CrossRef]
- Park, D.J.; Kwon, M.S.; Choi, J.H. The Influence of Health Information Orientation, Attitude of Internet Health Information, and e-Health Literacy on Personal Health Behaviors. J. Public Relat. 2013, 17, 379–413. [Google Scholar]
- Stewart, D.W.; Adams, C.E.; Cano, M.A.; Correa-Fernández, V.; Li, Y.; Waters, A.J.; Wetter, D.W.; Vidrine, J.I. Associations between health literacy and established predictors of smoking cessation. Am. J. Public Health 2013, 103, e43–e49. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.-S.; Kim, H.-R.; Myong, J.-P.; Kim, H.W. Association Between Work Conditions and Smoking in South Korea. Saf. Health Work 2013, 4, 197–200. [Google Scholar] [CrossRef]
- Angrave, D.; Charlwood, A.; Wooden, M. Working time and cigarette smoking: Evidence from Australia and the United Kingdom. Soc. Sci. Med. 2014, 112, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.J.; Lee, K.S.; Ul, P.H.; Lee, Y.J.; Gu, H.J.; Jeon, M.J. The effectiveness of workplace health promotion programs using break time and environmental support on tobacco cessation among female call-center employees. Korean J. Health Educ. Promot. 2017, 34, 95–102. [Google Scholar] [CrossRef]
- Halpern, M.T.; Taylor, H. Employee and employer support for workplace-based smoking cessation: Results from an international survey. J. Occup. Health 2010, 52, 375–382. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Categories | n (%) | Intention to Quit Smoking | χ2 (p) | |
|---|---|---|---|---|---|
| No (n = 68) | Yes (n = 310) | ||||
| n (%) | n (%) | ||||
| Age (year) | 20–29 | 129 (34.1) | 17 (13.2) | 112 (86.8) | 3.12 (0.210) |
| 30–39 | 163 (43.1) | 34 (20.9) | 129 (79.1) | ||
| ≥40 | 86 (22.8) | 17 (19.8) | 69 (80.2) | ||
| Body mass index | ≤19 | 69 (18.3) | 12 (17.4) | 57 (82.6) | 0.27 (0.875) |
| 20–24 | 258 (68.3) | 48 (18.6) | 210 (81.4) | ||
| ≥25 | 51 (13.5) | 8 (15.7) | 43 (84.3) | ||
| Education level | Highschool diploma or lower | 95 (25.1) | 22 (23.2) | 73 (76.8) | 2.30 (0.089) |
| University degree or higher | 283 (74.9) | 46 (16.3) | 237 (83.7) | ||
| Marital status | Single | 207 (54.8) | 42 (20.3) | 165 (79.7) | 3.77 (0.151) |
| Married | 148 (39.2) | 20 (13.5) | 128 (86.5) | ||
| Other | 23 (6.1) | 6 (26.1) | 17 (73.9) | ||
| Cohabitant | Live alone | 77 (20.4) | 21 (27.3) | 56 (72.7) | 2.27 (0.044) |
| Non-smoking cohabitant | 137 (36.2) | 24 (17.5) | 113 (82.5) | ||
| Smoking cohabitant | 164 (43.4) | 23 (14.0) | 141 (86.0) | ||
| Workplace size | Large corporations/public institutions | 62 (16.4) | 10 (16.1) | 52 (83.9) | 0.45 (0.799) |
| Small and medium businesses | 232 (61.4) | 41 (17.7) | 191 (82.3) | ||
| Private businesses | 84 (22.2) | 17 (20.2) | 67 (79.8) | ||
| Workplace title | Employee | 307 (81.2) | 52 (16.9) | 255 (83.1) | 1.22 (0.174) |
| Manager/management position | 71 (18.8) | 16 (22.5) | 55 (77.5) | ||
| Employment type | Regular | 318 (84.1) | 57 (17.9) | 261 (82.1) | 0.01 (0.532) |
| Non-regular | 60 (15.9) | 11 (18.3) | 49 (81.7) | ||
| Number of smoking co-workers (number) | None | 53 (14.0) | 12 (22.6) | 41 (77.4) | 6.92 (0.074) |
| 1–2 | 111 (29.4) | 26 (23.4) | 85 (76.6) | ||
| 3–9 | 132 (34.9) | 22 (16.7) | 110 (83.3) | ||
| ≥ 10 | 82 (21.7) | 8 (9.8) | 74 (90.2) | ||
| Physical labor intensity | Low intensity | 161 (42.6) | 34 (21.1) | 127 (78.9) | 1.94 (0.379) |
| Neutral | 164 (43.4) | 25 (15.2) | 139 (84.8) | ||
| High intensity | 53 (14.0) | 9 (17.0) | 44 (83.0) | ||
| Emotional labor intensity | Low intensity | 28 (7.4) | 7 (25.0) | 21 (75.0) | 1.41 (0.495) |
| Neutral | 139 (36.8) | 22 (15.8) | 117 (84.2) | ||
| High intensity | 211 (55.8) | 39 (18.5) | 172 (81.5) | ||
| Pressure for work performance | Not pressured | 206 (54.5) | 38 (18.4) | 168 (81.6) | 0.33 (0.847) |
| Neutral | 90 (23.8) | 17 (18.9) | 73 (81.1) | ||
| Pressured | 82 (21.7) | 13 (15.9) | 69 (84.1) | ||
| Work hour autonomy | Not autonomous | 117 (31.0) | 24 (20.5) | 93 (79.5) | 3.65 (0.161) |
| Neutral | 183 (48.4) | 26 (14.2) | 157 (85.8) | ||
| Autonomous | 78 (20.6) | 18 (23.1) | 60 (76.9) | ||
| Job satisfaction | Unsatisfied | 60 (15.9) | 8 (13.3) | 52 (86.7) | 4.77 (0.092) |
| Neutral | 183 (48.4) | 28 (15.3) | 155 (84.7) | ||
| Satisfied | 135 (35.7) | 32 (23.7) | 103 (76.3) | ||
| Desire to smoke | Low | 171 (45.2) | 37 (21.6) | 134 (78.4) | 2.82 (0.062) |
| High | 207 (54.8) | 31 (15.0) | 176 (85.0) | ||
| Amount of smoking per instance (number) | 1–2 | 223 (59.0) | 40 (17.9) | 183 (82.1) | 2.69 (0.261) |
| 3–10 | 144 (38.1) | 24 (16.7) | 120 (83.3) | ||
| ≥11 | 11 (2.9) | 4 (36.4) | 7 (63.6) | ||
| Smoking type | Behavioral/dependent | 151 (39.9) | 33 (21.9) | 118 (78.1) | 4.99 (0.172) |
| Stress relief | 129 (34.1) | 16 (12.4) | 113 (87.6) | ||
| Stimulus-seeking/boredom relief | 65 (17.2) | 14 (21.5) | 51 (78.5) | ||
| Effect-seeking | 33 (8.7) | 5 (15.2) | 28 (84.8) | ||
| Smoking cessation education | No | 293 (77.5) | 59 (20.1) | 234 (79.9) | 4.07 (0.028) |
| Yes | 85 (22.5) | 9 (10.6) | 76 (89.4) | ||
| Smoking harmfulness awareness | Low | 200 (52.9) | 41 (20.5) | 159 (79.5) | 1.82 (0.183) |
| High | 178 (47.1) | 27 (15.2) | 151 (84.8) | ||
| Smoking cessation treatment awareness | Low | 214 (56.6) | 49 (22.9) | 165 (77.1) | 8.05 (0.005) |
| High | 164 (43.4) | 19 (11.6) | 145 (88.4) | ||
| Smoking cessation policy awareness | Low | 206 (54.5) | 54 (26.2) | 152 (73.8) | 20.76 (<0.001) |
| High | 172 (45.5) | 14 (8.1) | 158 (91.9) | ||
| Variables | Smoking Awareness | Smoking Harmfulness Awareness | Smoking Cessation Treatment Awareness | Smoking Cessation Policy Awareness | Mean ± SD | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|
| r (p) | |||||||
| Intention to quit smoking | 0.32 (<0.001) | 0.02 (0.735) | 0.17 (0.001) | 0.38 (<0.001) | 2.36 ± 0.96 | 0.34 | −0.81 |
| Smoking awareness | 0.40 (<0.001) | 0.69 (<0.001) | 0.85 (<0.001) | 3.18 ± 0.37 | 0.64 | 0.95 | |
| Smoking harmfulness awareness | −0.12 (0.022) | −0.01 (0.873) | 2.58 ± 0.59 | 0.10 | 0.80 | ||
| Smoking cessation treatment awareness | 0.53 (<0.001) | 3.58 ± 0.41 | −0.01 | 0.89 | |||
| Smoking cessation policy awareness | 3.24 ± 0.66 | 0.27 | −0.23 | ||||
| Node | Node | Gain | Response | Gains Index | Profit | ROI | ||
|---|---|---|---|---|---|---|---|---|
| n | Percentage | n | Percentage | |||||
| 6 | 108 | 28.6% | 103 | 33.2% | 95.4% | 116.3% | 0.907 | 1960.0% |
| 11 | 41 | 10.8% | 39 | 12.6% | 95.1% | 116.0% | 0.902 | 1850.0% |
| 9 | 132 | 34.9% | 107 | 34.5% | 81.1% | 98.8% | 0.621 | 328.0% |
| 8 | 22 | 5.8% | 17 | 5.5% | 77.3% | 94.2% | 0.545 | 240.0% |
| 12 | 23 | 6.1% | 16 | 5.2% | 69.6% | 84.8% | 0.391 | 128.6% |
| 10 | 27 | 7.1% | 17 | 5.5% | 63.0% | 76.8% | 0.259 | 70.0% |
| 7 | 25 | 6.6% | 11 | 3.5% | 44.0% | 53.7% | −0.120 | −21.4% |
| ROI = Return on investment. | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, E.-H.; Shin, S.-H.; Jeong, G.-C. Smoking Awareness and Intention to Quit Smoking in Smoking Female Workers: Secondary Data Analysis. Int. J. Environ. Res. Public Health 2022, 19, 2841. https://doi.org/10.3390/ijerph19052841
Lee E-H, Shin S-H, Jeong G-C. Smoking Awareness and Intention to Quit Smoking in Smoking Female Workers: Secondary Data Analysis. International Journal of Environmental Research and Public Health. 2022; 19(5):2841. https://doi.org/10.3390/ijerph19052841
Chicago/Turabian StyleLee, Eun-Hye, Sun-Hwa Shin, and Goo-Churl Jeong. 2022. "Smoking Awareness and Intention to Quit Smoking in Smoking Female Workers: Secondary Data Analysis" International Journal of Environmental Research and Public Health 19, no. 5: 2841. https://doi.org/10.3390/ijerph19052841
APA StyleLee, E.-H., Shin, S.-H., & Jeong, G.-C. (2022). Smoking Awareness and Intention to Quit Smoking in Smoking Female Workers: Secondary Data Analysis. International Journal of Environmental Research and Public Health, 19(5), 2841. https://doi.org/10.3390/ijerph19052841







