What Is the Role of Night-Time Noise Exposure in Childhood Allergic Disease?
Abstract
1. Introduction
2. Materials and Methods
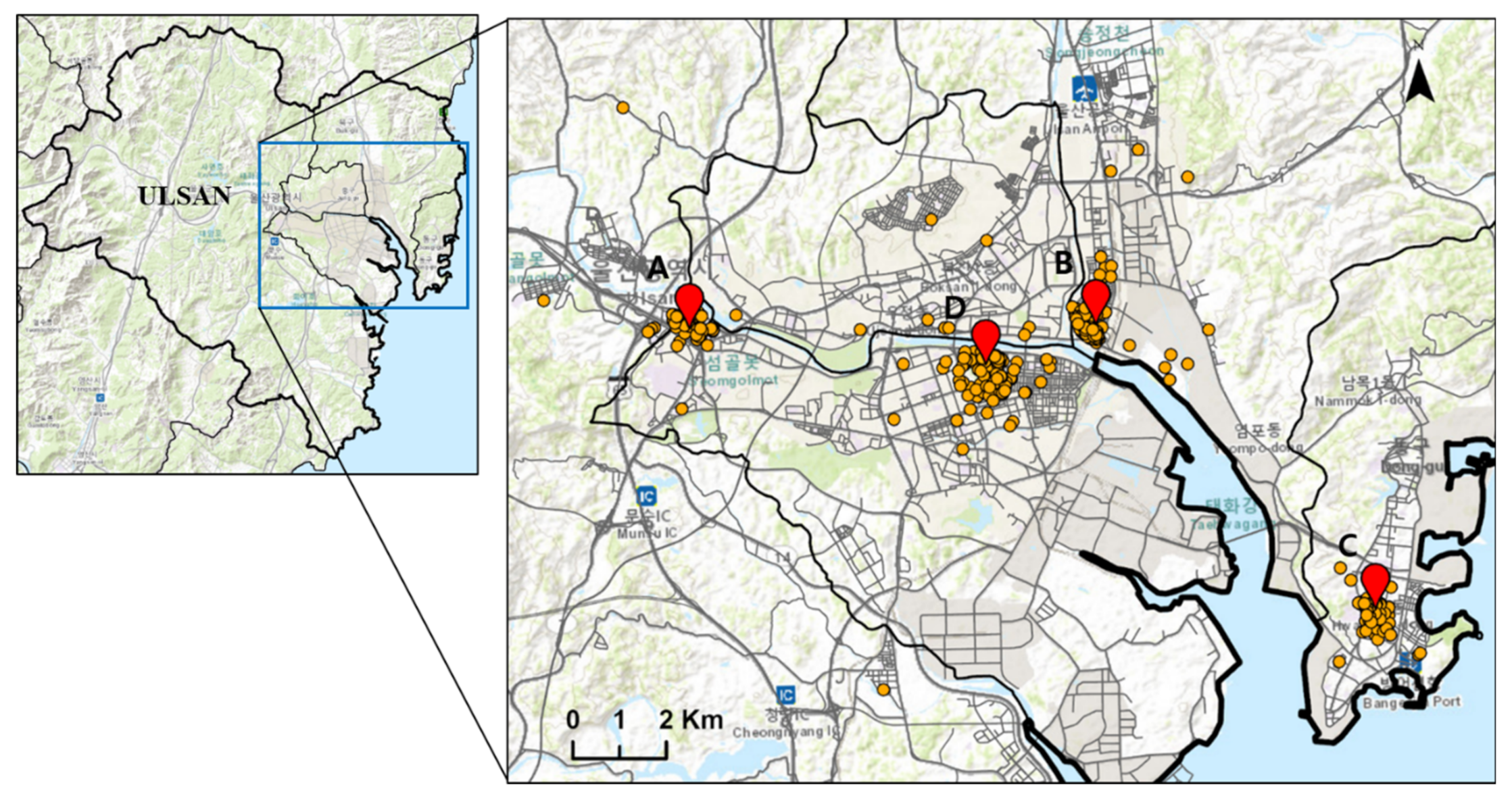
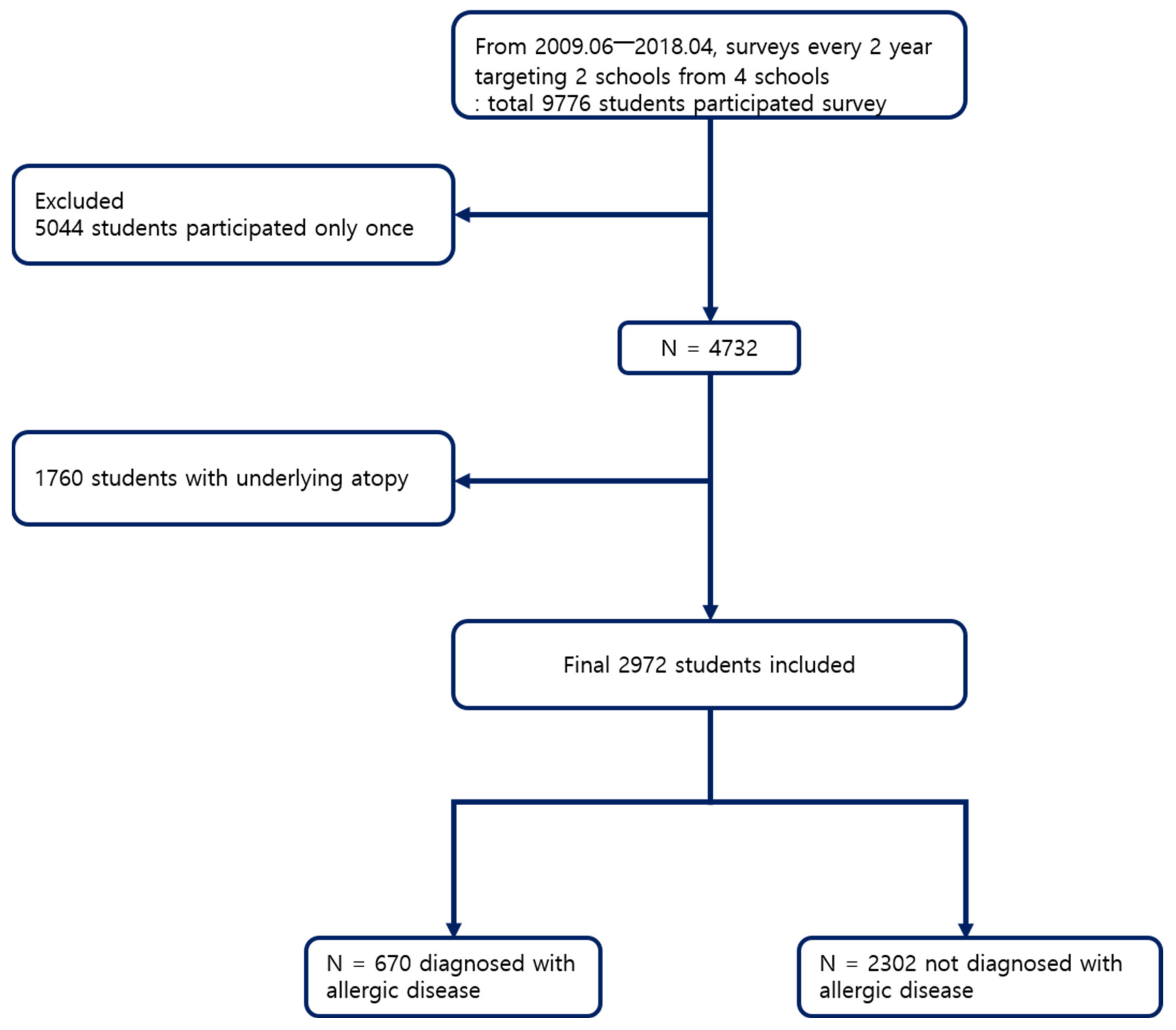
2.1. Sububject Selection
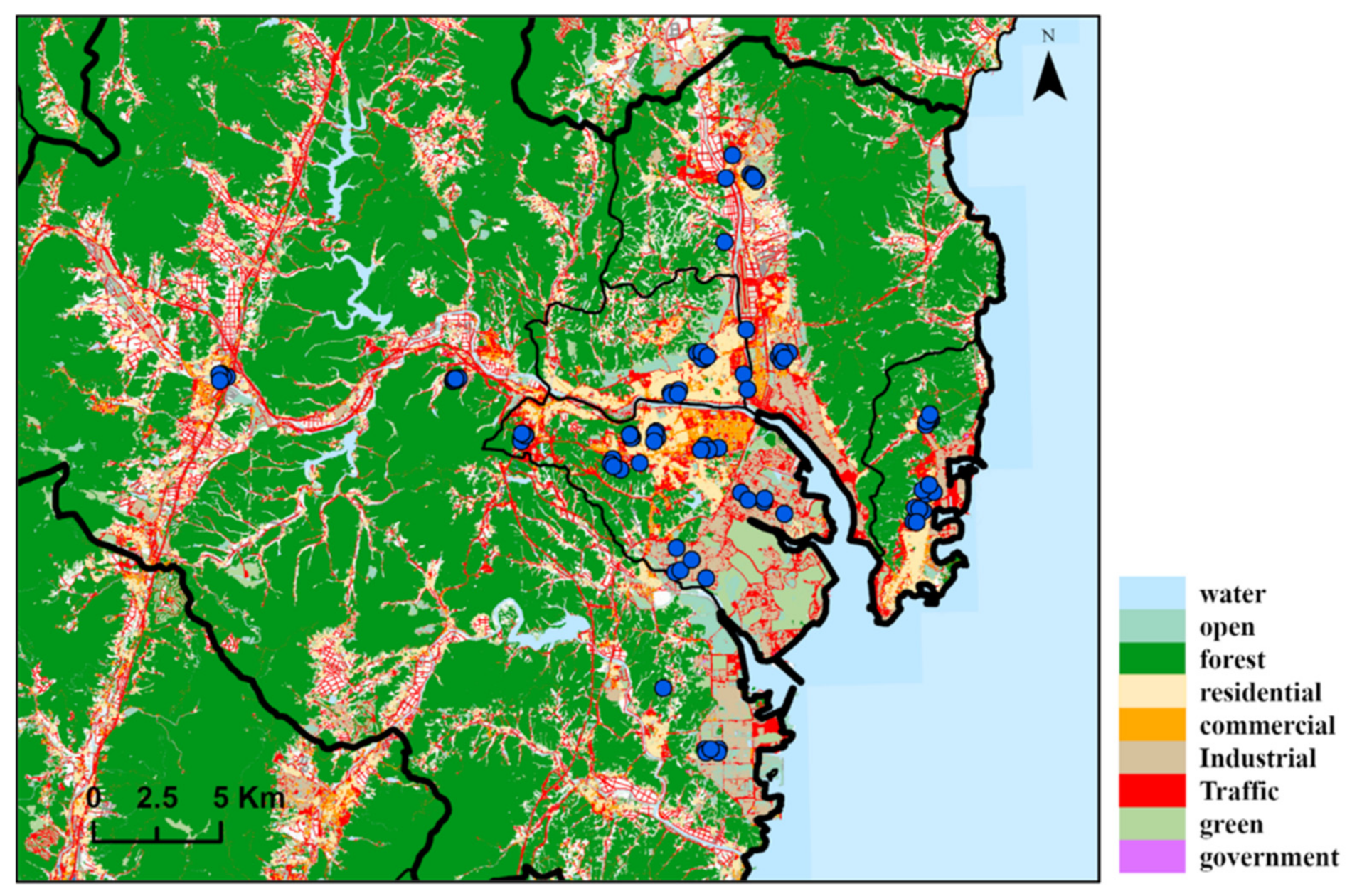
2.2. Exposure Assessment
2.2.1. Night-Time Noise
2.2.2. Air Pollution Level
2.3. Definition of the Outcome
2.4. Definition of the Exposure
2.5. Statistical Analysis
3. Results
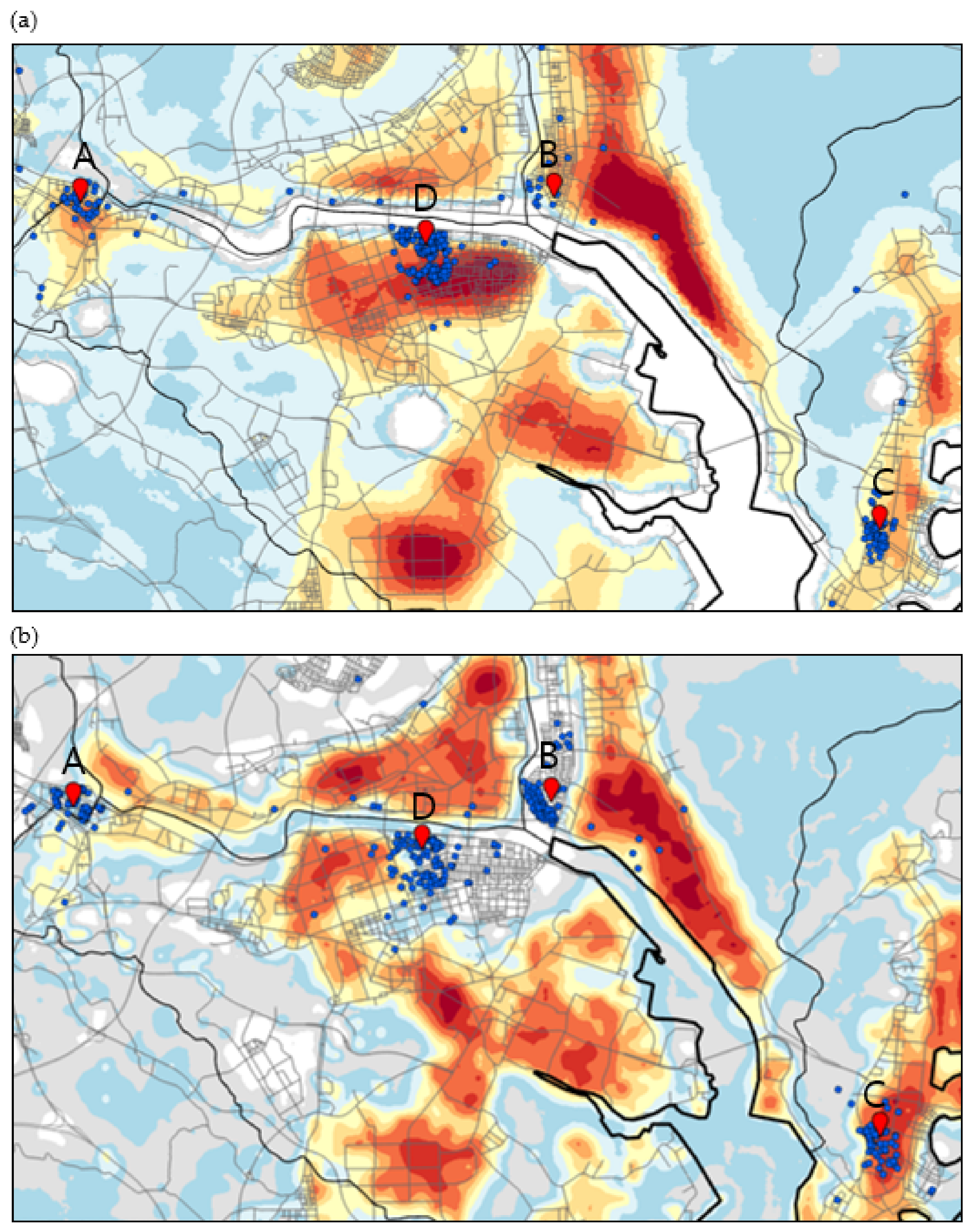
3.1. Air Pollutant Estimates
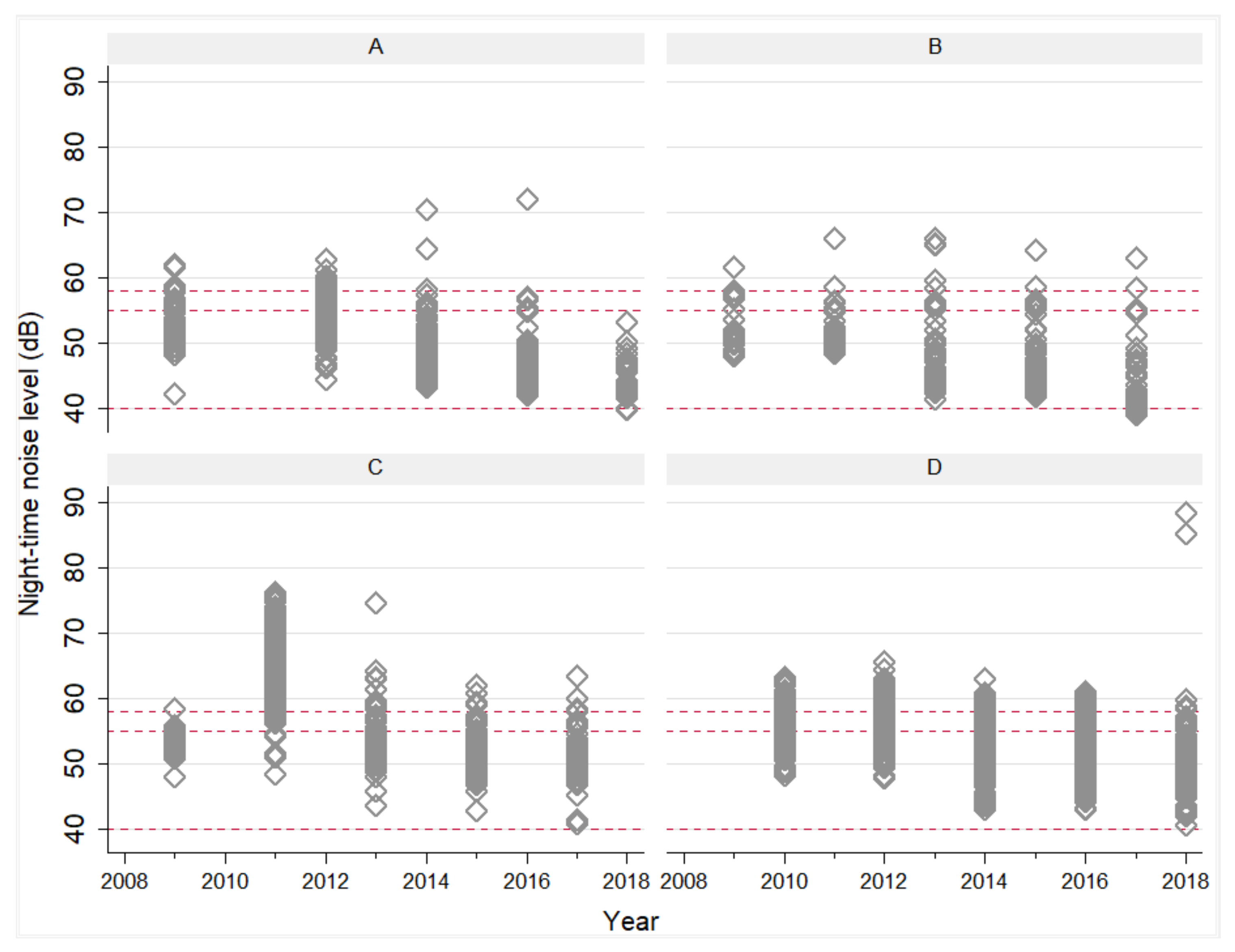
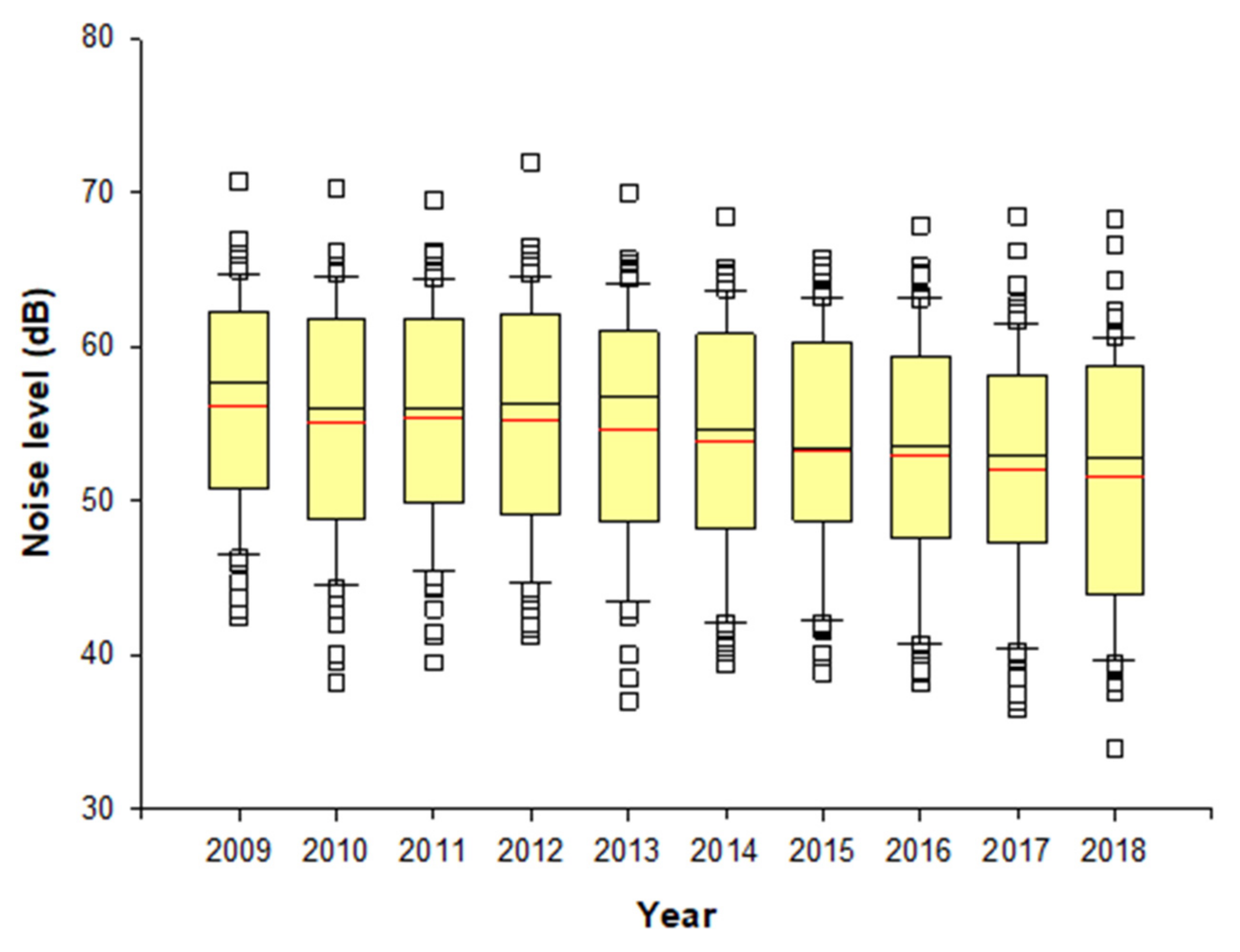
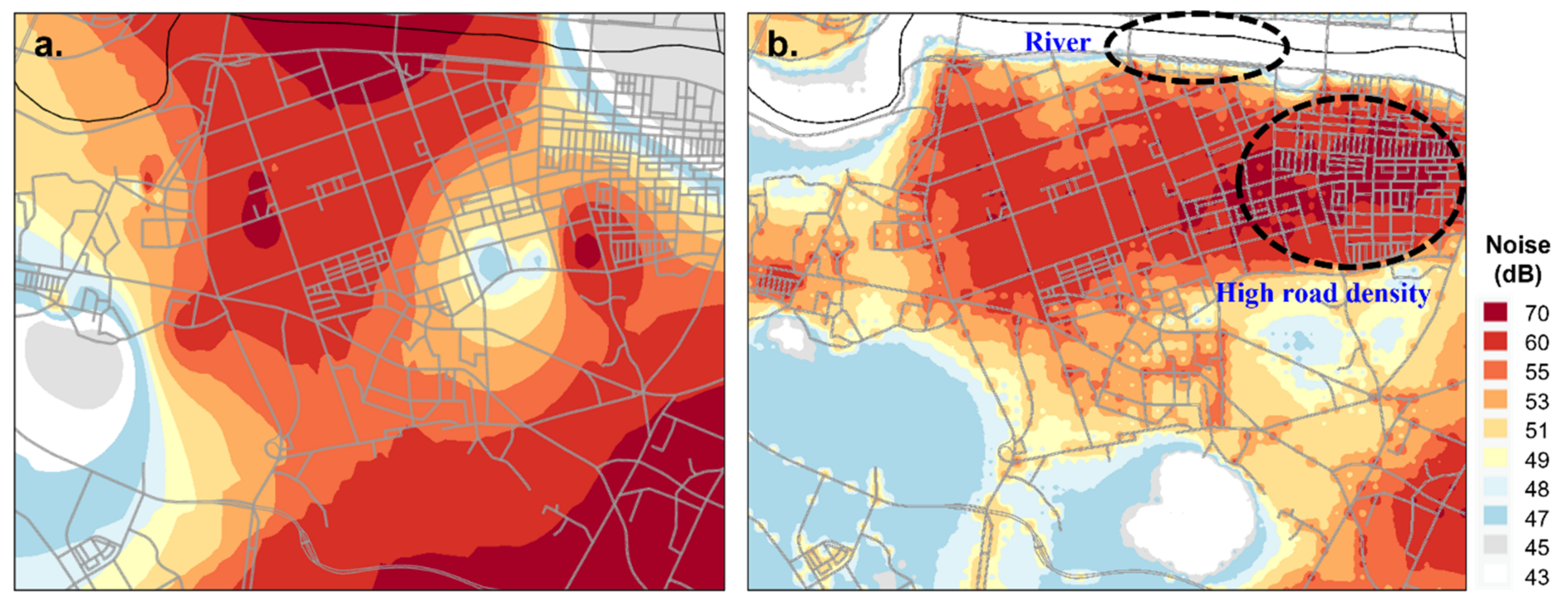
3.2. Night-Time Noise Estimates
3.3. Correlation between Night-Time Noise Estimates and Air Pollitants
3.4. Association between Night-Time Noise Exposure and Incidence of Allergic Disease
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Stone, K.D. Atopic diseases of childhood. Curr. Opin. Pediatr. 2003, 15, 495–511. [Google Scholar] [CrossRef] [PubMed]
- Wright, R.J.; Cohen, R.T.; Cohen, S. The impact of stress on the development and expression of atopy. Curr. Opin. Allergy Clin. Immunol. 2005, 5, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Moreno, M.A. Atopic Diseases in Children. JAMA Pediatr. 2016, 170, 96. [Google Scholar] [CrossRef][Green Version]
- David Boothe, W.; Tarbox, J.A.; Tarbox, M.B. Atopic Dermatitis: Pathophysiology. Adv. Exp. Med. Biol. 2017, 1027, 21–37. [Google Scholar] [PubMed]
- Ha, J.; Lee, S.W.; Yon, D.K. Ten-year trends and prevalence of asthma, allergic rhinitis, and atopic dermatitis among the Korean population, 2008–2017. Clin. Exp. Pediatr. 2020, 63, 278–283. [Google Scholar] [CrossRef]
- Dave, N.D.; Xiang, L.; Rehm, K.E.; Marshall, G.D., Jr. Stress and allergic diseases. Immunol. Allergy Clin. N. Am. 2011, 31, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Koszorú, K.; Borza, J.; Gulácsi, L.; Sárdy, M. Quality of life in patients with atopic dermatitis. Cutis 2019, 104, 174–177. [Google Scholar] [PubMed]
- Sibbald, C.; Drucker, A.M. Patient Burden of Atopic Dermatitis. Derm. Clin. 2017, 35, 303–316. [Google Scholar] [CrossRef]
- Kim, Y.M.; Kim, J.; Han, Y.; Jeon, B.H.; Cheong, H.K.; Ahn, K. Short-term effects of weather and air pollution on atopic dermatitis symptoms in children: A panel study in Korea. PLoS ONE 2017, 12, e0175229. [Google Scholar] [CrossRef]
- Thomsen, S.F. Epidemiology and natural history of atopic diseases. Eur. Clin. Respir. J. 2015, 2, 24642. [Google Scholar] [CrossRef]
- Schwela, D.; Kephalopoulos, S.; Prasher, D. Confounding or aggravating factors in noise-induced health effects: Air pollutants and other stressors. Noise Health 2005, 7, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Goines, L.; Hagler, L. Noise pollution: A modem plague. South. Med. J. 2007, 100, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Muzet, A. Environmental noise, sleep and health. Sleep Med. Rev. 2007, 11, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.B.; Fecht, D.; Gulliver, J.; Beevers, S.D.; Dajnak, D.; Blangiardo, M.; Ghosh, R.E.; Hansell, A.L.; Kelly, F.J.; Anderson, H.R.; et al. Impact of London’s road traffic air and noise pollution on birth weight: Retrospective population based cohort study. BMJ 2017, 359, j5299. [Google Scholar] [CrossRef]
- Passchier-Vermeer, W.; Passchier, W.F. Noise exposure and public health. Environ. Health Perspect 2000, 108 (Suppl. 1), 123–131. [Google Scholar]
- Ristovska, G.; Laszlo, H.E.; Hansell, A.L. Reproductive outcomes associated with noise exposure—A systematic review of the literature. Int. J. Environ. Res. Public Health 2014, 11, 7931–7952. [Google Scholar] [CrossRef]
- Guski, R.; Schreckenberg, D.; Schuemer, R. WHO Environmental Noise Guidelines for the European Region: A Systematic Review on Environmental Noise and Annoyance. Int. J. Environ. Res. Public Health 2017, 14, 1539. [Google Scholar] [CrossRef]
- Dang-Vu, T.T.; McKinney, S.M.; Buxton, O.M.; Solet, J.M.; Ellenbogen, J.M. Spontaneous brain rhythms predict sleep stability in the face of noise. Curr. Biol. 2010, 20, R626–R627. [Google Scholar] [CrossRef]
- Basner, M.; Babisch, W.; Davis, A.; Brink, M.; Clark, C.; Janssen, S.; Stansfeld, S. Auditory and non-auditory effects of noise on health. Lancet 2014, 383, 1325–1332. [Google Scholar] [CrossRef]
- Kumar, A. Thematic issue: Noise impacts on health Environment. Sci. Environ. Policy 2015, 47, 3–13. [Google Scholar]
- Schlatter, F.; Piquerez, A.; Habermacher, M.; Ragettli, M.S.; Röösli, M.; Brink, M.; Cajochen, C.; Probst-Hensch, N.; Foraster, M.; Wunderli, J.-M. Validation of large scale noise exposure modelling by long-term measurements. Noise Mapp. 2017, 4, 75–86. [Google Scholar] [CrossRef]
- Bravo, M.A.; Fuentes, M.; Zhang, Y.; Burr, M.J.; Bell, M.L. Comparison of exposure estimation methods for air pollutants: Ambient monitoring data and regional air quality simulation. Environ. Res. 2012, 116, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Gao, S.; Zhang, H.; Sun, Y.; Ma, Z.; Vedal, S.; Mao, J.; Bai, Z. Spatiotemporal modeling of PM2.5 concentrations at the national scale combining land use regression and Bayesian maximum entropy in China. Environ. Int. 2018, 116, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Ihl, T.; Bautista, F.; Cejudo Ruíz, F.R.; Delgado, M.d.C.; Quintana Owen, P.; Aguilar, D.; Goguitchaichvili, A. Concentration of toxic elements in topsoils of the metropolitan area of Mexico City: A spatial analysis using Ordinary kriging and Indicator kriging. Rev. Int. Contam. Ambient. 2015, 31, 47–62. [Google Scholar]
- Selby, B.; Kockelman, K.M. Spatial prediction of traffic levels in unmeasured locations: Applications of universal kriging and geographically weighted regression. J. Transp. Geogr. 2013, 29, 24–32. [Google Scholar] [CrossRef]
- Hornung, R.W.; Greife, A.L.; Stayner, L.T.; Kyle Steenland, N.; Herrick, R.F.; Elliott, L.J.; Ringenburg, V.L.; Morawetz, J. Statistical model for prediction of retrospective exposure to ethylene oxide in an occupational mortality study. Am. J. Ind. Med. 1994, 25, 825–836. [Google Scholar] [CrossRef]
- Seixas, N.S.; Checkoway, H. Exposure assessment in industry specific retrospective occupational epidemiology studies. Occup. Environ. Med. 1995, 52, 625–633. [Google Scholar] [CrossRef]
- Xie, X.; Semanjski, I.; Gautama, S.; Tsiligianni, E.; Deligiannis, N.; Rajan, R.T.; Pasveer, F.; Philips, W. A review of urban air pollution monitoring and exposure assessment methods. ISPRS Int. J. Geo-Inf. 2017, 6, 389. [Google Scholar] [CrossRef]
- Aguilera, I.; Foraster, M.; Basagaña, X.; Corradi, E.; Deltell, A.; Morelli, X.; Phuleria, H.C.; Ragettli, M.S.; Rivera, M.; Thomasson, A.; et al. Application of land use regression modelling to assess the spatial distribution of road traffic noise in three European cities. J. Expo. Sci. Environ. Epidemiol. 2015, 25, 97–105. [Google Scholar] [CrossRef]
- Hoek, G. Methods for Assessing Long-Term Exposures to Outdoor Air Pollutants. Curr. Environ. Health Rep. 2017, 4, 450–462. [Google Scholar] [CrossRef]
- Saucy, A.; Röösli, M.; Künzli, N.; Tsai, M.-Y.; Sieber, C.; Olaniyan, T.; Baatjies, R.; Jeebhay, M.; Davey, M.; Flückiger, B.; et al. Land Use Regression Modelling of Outdoor NO2 and PM2.5 Concentrations in Three Low Income Areas in the Western Cape Province, South Africa. Int. J. Environ. Res. Public Health 2018, 15, 1452. [Google Scholar] [CrossRef]
- National Noise Information System Data (NOISE Infor). Available online: https://www.noiseinfo.or.kr (accessed on 10 June 2021).
- Environmental Geographic Information Service (EGIS). Available online: https://egis.me.go.kr (accessed on 10 February 2021).
- Farr, T.G.; Rosen, P.A.; Caro, E.; Crippen, R.; Duren, R.; Hensley, S.; Kobrick, M.; Paller, M.; Rodriguez, E.; Roth, L. The shuttle radar topography mission. Rev. Geophys. 2007, 45, 1–33. [Google Scholar] [CrossRef]
- Beelen, R.; Hoek, G.; Vienneau, D.; Eeftens, M.; Dimakopoulou, K.; Pedeli, X.; Tsai, M.-Y.; Künzli, N.; Schikowski, T.; Marcon, A. Development of NO2 and NOx land use regression models for estimating air pollution exposure in 36 study areas in Europe—The ESCAPE project. Atmos. Environ. 2013, 72, 10–23. [Google Scholar] [CrossRef]
- Bloemsma, L.D.; Gehring, U.; Klompmaker, J.O.; Hoek, G.; Janssen, N.A.; Lebret, E.; Brunekreef, B.; Wijga, A.H. Green space, air pollution, traffic noise and cardiometabolic health in adolescents: The PIAMA birth cohort. Environ. Int. 2019, 131, 104991. [Google Scholar] [CrossRef] [PubMed]
- Cesaroni, G.; Porta, D.; Badaloni, C.; Stafoggia, M.; Eeftens, M.; Meliefste, K.; Forastiere, F. Nitrogen dioxide levels estimated from land use regression models several years apart and association with mortality in a large cohort study. Environ. Health 2012, 11, 48. [Google Scholar] [CrossRef] [PubMed]
- Hoek, G.; Beelen, R.; De Hoogh, K.; Vienneau, D.; Gulliver, J.; Fischer, P.; Briggs, D. A review of land-use regression models to assess spatial variation of outdoor air pollution. Atmos. Environ. 2008, 42, 7561–7578. [Google Scholar] [CrossRef]
- Oliver, M.A.; Webster, R. Kriging: A method of interpolation for geographical information systems. Int. J. Geogr. Inf. Syst. 1990, 4, 313–332. [Google Scholar] [CrossRef]
- Siska, P.P.; Hung, I.-K. Assessment of Kriging Accuracy in the GIS Environment. In Proceedings of the 21st Annual ESRI International Conference, San Diego, CA, USA, 9–13 July 2001. [Google Scholar]
- Childs, C. Interpolating surfaces in ArcGIS spatial analyst. ArcUser 2004, 3235, 32–35. [Google Scholar]
- Kim, S.H.; Lee, J.; Oh, I.; Oh, Y.; Sim, C.S.; Bang, J.H.; Park, J.; Kim, Y. Allergic rhinitis is associated with atmospheric SO2: Follow-up study of children from elementary schools in Ulsan, Korea. PLoS ONE 2021, 16, e0248624. [Google Scholar] [CrossRef]
- Åberg, N.; Sundell, J.; Eriksson, B.; Hesselmaf, B.; Åberg, B. Prevalence of allergic diseases in schoolchildren in relation to family history, upper respiratory infections, and residential characteristics. Allergy 1996, 51, 232–237. [Google Scholar]
- Baek, J.O.; Hong, S.; Son, D.K.; Lee, J.R.; Roh, J.Y.; Kwon, H.J. Analysis of the Prevalence of and Risk Factors for Atopic Dermatitis Using an ISAAC Questionnaire in 8750 Korean Children. Int. Arch. Allergy Immunol. 2013, 162, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Christensen, J.S.; Hjortebjerg, D.; Raaschou-Nielsen, O.; Ketzel, M.; Sørensen, T.I.; Sørensen, M. Pregnancy and childhood exposure to residential traffic noise and overweight at 7 years of age. Environ. Int. 2016, 94, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Cuppari, C.; Manti, S.; Salpietro, A.; Alterio, T.; Arrigo, T.; Leonardi, S.; Salpietro, C. Mode of delivery and risk for development of atopic diseases in children. Allergy Asthma Proc. 2015, 36, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Hartwig, I.R.V.; Sly, P.D.; Schmidt, L.A.; Van Lieshout, R.J.; Bienenstock, J.; Holt, P.G.; Arck, P.C. Prenatal adverse life events increase the risk for atopic diseases in children, which is enhanced in the absence of a maternal atopic predisposition. J. Allergy Clin. Immunol. 2014, 134, 160–169.e7. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Wu, H.; Zhang, S.; Lin, Y.; Li, R.; Xie, L.; Li, Z.; Sun, W.; Huang, X.; Zhang, C.J. The association between secondhand smoke and childhood asthma: A systematic review and meta-analysis. Pediatr. Pulmonol. 2020, 55, 2518–2531. [Google Scholar] [CrossRef] [PubMed]
- Morgenstern, V.; Zutavern, A.; Cyrys, J.; Brockow, I.; Koletzko, S.; Krämer, U.; Behrendt, H.; Herbarth, O.; Von Berg, A.; Bauer, C.P.; et al. Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am. J. Respir. Crit. Care Med. 2008, 177, 1331–1337. [Google Scholar] [CrossRef]
- Palagini, L.; Gemignani, A.; Banti, S.; Manconi, M.; Mauri, M.; Riemann, D. Chronic sleep loss during pregnancy as a determinant of stress: Impact on pregnancy outcome. Sleep Med. 2014, 15, 853–859. [Google Scholar] [CrossRef]
- Schmitz, R.; Atzpodien, K.; Schlaud, M. Prevalence and risk factors of atopic diseases in German children and adolescents. Pediatr. Allergy Immunol. 2012, 23, 716–723. [Google Scholar] [CrossRef]
- Thacher, J.D.; Gruzieva, O.; Pershagen, G.; Neuman, Å.; Van Hage, M.; Wickman, M.; Kull, I.; Melén, E.; Bergström, A. Parental smoking and development of allergic sensitization from birth to adolescence. Allergy 2016, 71, 239–248. [Google Scholar] [CrossRef]
- Hammer, M.S.; Swinburn, T.K.; Neitzel, R.L. Environmental noise pollution in the United States: Developing an effective public health response. Environ. Health Perspect. 2014, 122, 115–119. [Google Scholar] [CrossRef]
- Barceló, M.A.; Varga, D.; Tobias, A.; Diaz, J.; Linares, C.; Saez, M. Long term effects of traffic noise on mortality in the city of Barcelona, 2004–2007. Environ. Res. 2016, 147, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Hahad, O.; Prochaska, J.H.; Daiber, A.; Münzel, T. Environmental Noise-Induced Effects on Stress Hormones, Oxidative Stress, and Vascular Dysfunction: Key Factors in the Relationship between Cerebrocardiovascular and Psychological Disorders. Oxidative Med. Cell. Longev. 2019, 2019, 4623109. [Google Scholar] [CrossRef]
- Halperin, D. Environmental noise and sleep disturbances: A threat to health? Sleep Sci. 2014, 7, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Hammersen, F.; Niemann, H.; Hoebel, J. Environmental Noise Annoyance and Mental Health in Adults: Findings from the Cross-Sectional German Health Update (GEDA) Study 2012. Int. J. Environ. Res. Public Health 2016, 13, 954. [Google Scholar] [CrossRef]
- Münzel, T.; Sørensen, M.; Schmidt, F.; Schmidt, E.; Steven, S.; Kröller-Schön, S.; Daiber, A. The Adverse Effects of Environmental Noise Exposure on Oxidative Stress and Cardiovascular Risk. Antioxid. Redox Signal. 2018, 28, 873–908. [Google Scholar] [CrossRef] [PubMed]
- Tobías, A.; Recio, A.; Díaz, J.; Linares, C. Does traffic noise influence respiratory mortality? Eur. Respir. J. 2014, 44, 797–799. [Google Scholar] [CrossRef]
- Schmidt, F.P.; Basner, M.; Kröger, G.; Weck, S.; Schnorbus, B.; Muttray, A.; Sariyar, M.; Binder, H.; Gori, T.; Warnholtz, A.; et al. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur. Heart J. 2013, 34, 3508–3514. [Google Scholar] [CrossRef]
- Medic, G.; Wille, M.; Hemels, M.E. Short- and long-term health consequences of sleep disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef]
- Maschke, C.; Hecht, K. Stress hormones and sleep disturbances—Electrophysiological and hormonal aspects. Noise Health 2004, 6, 49–54. [Google Scholar]
- Meerlo, P.; Sgoifo, A.; Suchecki, D. Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Med. Rev. 2008, 12, 197–210. [Google Scholar] [CrossRef]
- Smith, P.C.; Mong, J.A. Neuroendocrine Control of Sleep. Curr. Top. Behav. Neurosci. 2019, 43, 353–378. [Google Scholar]
- Hirotsu, C.; Tufik, S.; Andersen, M.L. Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Sci. 2015, 8, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Boer, E.; Schroten, A. Traffic Noise Reduction in Europe: Health Effects, Social Costs and Technical and Policy Options to Reduce Road and Rail Traffic Noise; CE Delft, Solutions for Environment, Economy and Technology: Delft, The Netherlands, 2007. [Google Scholar]
- Maschke, C. Excretion of Cortisol under Nocturnal Noise and Differences due to Analytic Techniques. Noise Health 2003, 5, 47–52. [Google Scholar] [PubMed]
- Spiegel, K.; Leproult, R.; Van Cauter, E. Impact of sleep debt on metabolic and endocrine function. Lancet 1999, 354, 1435–1439. [Google Scholar] [CrossRef]
- Wright, K.P., Jr.; Drake, A.L.; Frey, D.J.; Fleshner, M.; Desouza, C.A.; Gronfier, C.; Czeisler, C.A. Influence of sleep deprivation and circadian misalignment on cortisol, inflammatory markers, and cytokine balance. Brain Behav. Immun. 2015, 47, 24–34. [Google Scholar] [CrossRef]
- Ising, H.; Braun, C. Acute and chronic endocrine effects of noise: Review of the research conducted at the Institute for water, soil and air hygiene. Noise Health 2000, 2, 7–24. [Google Scholar]
- Zhang, A.; Zou, T.; Guo, D.; Wang, Q.; Shen, Y.; Hu, H.; Ye, B.; Xiang, M. The Immune System Can Hear Noise. Front. Immunol. 2020, 11, 619189. [Google Scholar] [CrossRef] [PubMed]
- Prasher, D. Is there evidence that environmental noise is immunotoxic? Noise Health 2009, 11, 151–155. [Google Scholar] [CrossRef]
- Kitagaki, H.; Hiyama, H.; Kitazawa, T.; Shiohara, T. Psychological stress with long-standing allergic dermatitis causes psychodermatological conditions in mice. J. Investig. Derm. 2014, 134, 1561–1569. [Google Scholar] [CrossRef] [PubMed]
- Morren, M.A.; Przybilla, B.; Bamelis, M.; Heykants, B.; Reynaers, A.; Degreef, H. Atopic dermatitis: Triggering factors. J. Am. Acad. Derm. 1994, 31 Pt 1, 467–473. [Google Scholar] [CrossRef]
- Tao, Y.; Chai, Y.; Kou, L.; Kwan, M.-P. Understanding noise exposure, noise annoyance, and psychological stress: Incorporating individual mobility and the temporality of the exposure-effect relationship. Appl. Geogr. 2020, 125, 102283. [Google Scholar] [CrossRef]
- Besedovsky, L.; Lange, T.; Born, J. Sleep and immune function. Pflug. Arch. 2012, 463, 121–137. [Google Scholar] [CrossRef]
- Oztürk, L.; Pelin, Z.; Karadeniz, D.; Kaynak, H.; Cakar, L.; Gözükirmizi, E. Effects of 48 hours sleep deprivation on human immune profile. Sleep Res. Online 1999, 2, 107–111. [Google Scholar] [PubMed]
- Chang, Y.S.; Chiang, B.L. Sleep disorders and atopic dermatitis: A 2-way street? J. Allergy Clin. Immunol. 2018, 142, 1033–1040. [Google Scholar] [CrossRef]
- Villafuerte, G.; Miguel-Puga, A.; Rodríguez, E.M.; Machado, S.; Manjarrez, E.; Arias-Carrión, O. Sleep deprivation and oxidative stress in animal models: A systematic review. Oxid. Med. Cell. Longev. 2015, 2015, 234952. [Google Scholar] [CrossRef]
- Niemann, H.; Maschke, C. WHO LARES Final Report Noise Effects and Morbidity; World Health Organization: Berlin, Germany, 2004. [Google Scholar]
- Paunovic, K. Noise and children’s health: Research in Central, Eastern and South-Eastern Europe and Newly Independent States. Noise Health 2013, 15, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Jernelöv, S.; Lekander, M.; Almqvist, C.; Axelsson, J.; Larsson, H. Development of atopic disease and disturbed sleep in childhood and adolescence—A longitudinal population-based study. Clin. Exp. Allergy 2013, 43, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Babisch, W. The Noise/Stress Concept, Risk Assessment and Research Needs. Noise Health 2002, 4, 1. [Google Scholar]
- Peris, E. Noise Pollution Is a Major Problem, Both for Human Health and the Environment. EEA Newsletter. 2020. Available online: https://www.eea.europa.eu/articles/noise-pollution-is-a-major (accessed on 15 December 2021).
- Exposure of Europe’s Population to Environmental Noise. Available online: https://www.eea.europa.eu/data-and-maps/indicators/exposure-to-and-annoyance-by-2/assessment-4 (accessed on 7 December 2020).
- Clean Air Act Title IV—Noise Pollution. Available online: https://www.epa.gov/clean-air-act-overview/clean-air-act-title-iv-noise-pollution (accessed on 7 December 2020).
- Desa, U. World Urbanization Prospects: The 2018 Revision, Key Facts. Available online: https://population.un.org/wup/Publications/ (accessed on 20 December 2018).
- Farooqi, Z.U.R.; Sabir, M.; Zeeshan, N.; Murtaza, G.; Hussain, M.M.; Ghani, M.U. Vehicular noise pollution: Its environmental implications and strategic control. In Autonomous Vehicle and Smart Traffic; IntechOpen: London, UK, 2020. [Google Scholar]
- Park, Y.M.; Kang, G.K.; Kim, K.M. Rationalization (Unification) of Traffic Noise Management Standards. Res. Rep. 2019, 2019, 1–93. [Google Scholar]
- Kaliski, K.; Haac, R.; Brese, D.; Duncan, E.; Reiter, D.; Williamson, R.; Pratt, G.; Salomons, E.; Wayson, R.; McDonald, J. How Weather Affects the Noise You Hear from Highways. National Cooperative Highway Research Program; Federal Highway Administration: Washington, DC, USA, 2018.
- Davies, H.W.; Vlaanderen, J.J.; Henderson, S.B.; Brauer, M. Correlation between co-exposures to noise and air pollution from traffic sources. Occup. Environ. Med. 2009, 66, 347–350. [Google Scholar] [CrossRef]
- Kendrick, C.M.; Koonce, P.; George, L.A. Diurnal and seasonal variations of NO, NO2 and PM2.5 mass as a function of traffic volumes alongside an urban arterial. Atmos. Environ. 2015, 122, 133–141. [Google Scholar] [CrossRef]
- Cheng, L.; Ji, D.; He, J.; Li, L.; Du, L.; Cui, Y.; Wang, Y.; Zhang, H.; Zhou, L.; Li, Z.; et al. Characteristics of Air Pollutants and Greenhouse Gases at a Regional Background Station in Southwestern China. Aerosol Air Qual. Res. 2019, 19, 1007–1023. [Google Scholar] [CrossRef]
- Khreis, H.; Warsow, K.M.; Verlinghieri, E.; Guzman, A.; Pellecuer, L.; Ferreira, A.; Jones, I.; Heinen, E.; Rojas-Rueda, D.; Mueller, N. The health impacts of traffic-related exposures in urban areas: Understanding real effects, underlying driving forces and co-producing future directions. J. Transp. Health 2016, 3, 249–267. [Google Scholar] [CrossRef]
- Hill, E.; Billington, R.; Krageloh, C. Noise sensitivity and diminished health: Testing moderators and mediators of the relationship. Noise Health 2014, 16, 47. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.; Sung, J.H.; Bang, J.-H.; Cho, S.W.; Lee, J.; Sim, C.S. Effects of self-reported sensitivity and road-traffic noise levels on the immune system. PLoS ONE 2017, 12, e0187084. [Google Scholar] [CrossRef]

| Variables | No Event | Event | p-Value | |||
|---|---|---|---|---|---|---|
| Time to event a,* (days) | 961.7 | (356.5) | 865.2 | (295.7) | 0.000 * | |
| Age a,* (years) | 7.6 | (1.20) | 7.3 | (1.10) | 0.000 * | |
| Sex b | Male | 1120 | (48.7%) | 348 | (52.0%) | 0.140 |
| Female | 1181 | (51.3%) | 321 | (48.0%) | ||
| History of Allergic disease, Father b | No | 1777 | (77.2%) | 454 | (67.8%) | 0.000 * |
| Yes | 525 | (22.8%) | 216 | (32.2%) | ||
| History of Allergic disease, Mother b | No | 1680 | (73.0%) | 422 | (63.0%) | 0.000 * |
| Yes | 622 | (27.0%) | 248 | (37.0%) | ||
| History of bronchiolitis b | No | 2091 | (90.8%) | 559 | (83.4%) | 0.000 * |
| Yes | 211 | (9.2%) | 111 | (16.6%) | ||
| Income b | <1.0 | 21 | (0.9%) | 9 | (1.3%) | 0.060 * |
| (million Korean won) | 1.0~2.0 | 190 | (8.3%) | 31 | (4.6%) | |
| 2.0~3.0 | 673 | (29.4%) | 204 | (30.6%) | ||
| 3.0~4.0 | 635 | (27.7%) | 188 | (28.2%) | ||
| 4.0~5.0 | 452 | (19.7%) | 139 | (20.8%) | ||
| >5.0 | 321 | (14.0%) | 96 | (14.4%) | ||
| Lactation b | No | 507 | (22.0%) | 138 | (20.6%) | 0.460 |
| Yes | 1794 | (78.0%) | 532 | (79.4%) | ||
| Variables | No Event | Event | p-Value | |||
|---|---|---|---|---|---|---|
| Secondhand smoke | No | 1800 | (78.2%) | 525 | (78.4%) | 0.960 |
| Yes | 502 | (21.8%) | 145 | (21.6%) | ||
| Air purifier | No | 1694 | (73.7%) | 466 | (69.6%) | 0.030 * |
| Yes | 604 | (26.3%) | 204 | (30.4%) | ||
| Humidifier | No | 1678 | (73.1%) | 482 | (72.0%) | 0.620 |
| Yes | 618 | (26.9%) | 187 | (28.0%) | ||
| Pet | No | 1828 | (79.5%) | 535 | (79.9%) | 0.870 |
| Yes | 471 | (20.5%) | 135 | (20.1%) | ||
| Vicinity to road | Near | 365 | (15.9%) | 112 | (16.7%) | 0.910 |
| (unit: meter) | <50 | 414 | (18.0%) | 123 | (18.4%) | |
| <100 | 608 | (26.4%) | 173 | (25.9%) | ||
| <200 | 518 | (22.5%) | 149 | (22.3%) | ||
| <300 | 217 | (9.4%) | 69 | (10.3%) | ||
| <400 | 104 | (4.5%) | 24 | (3.6%) | ||
| <500 | 75 | (3.3%) | 19 | (2.8%) | ||
| Amount of traffics † | Low | 178 | (7.7%) | 36 | (5.4%) | 0.120 |
| Medium | 885 | (38.4%) | 261 | (39.1%) | ||
| High | 1239 | (53.8%) | 371 | (55.5%) | ||
| Variable | Noise | NO2 | SO2 | O3 | CO | PM10 |
|---|---|---|---|---|---|---|
| Noise | 1 | −0.296 ** | 0.231 ** | −0.370 ** | −0.079 ** | −0.191 ** |
| NO2 | −0.296 ** | 1 | −0.510 ** | −0.220 ** | −0.161 ** | 0.037 ** |
| SO2 | 0.231 ** | −0.510 ** | 1 | 0.463 ** | 0.186 ** | 0.095 ** |
| O3 | −0.370 ** | −0.220 ** | 0.463 ** | 1 | 0.351 ** | −0.070 ** |
| CO | −0.079 ** | −0.161 ** | 0.186 ** | 0.351 ** | 1 | −0.445 ** |
| PM10 | −0.191 ** | 0.037 ** | 0.095 ** | −0.070 ** | −0.445 ** | 1 |
| Variable | Univariate Model | Multivariate Model § | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||||||
| Night noise difference a | 1.077 | 1.057 | – | 1.099 | 0.000 | 1.710 | 1.424 | – | 2.052 | 0.000 | |
| Age | 1.243 | 1.154 | – | 1.339 | 0.000 | 1.167 | 1.078 | – | 1.263 | 0.000 | |
| History of Allergic disease, Father | 1.577 | 1.341 | – | 1.854 | 0.000 | 1.460 | 1.225 | – | 1.740 | 0.000 | |
| History of Allergic disease, Mother | 1.428 | 1.220 | – | 1.670 | 0.000 | 1.364 | 1.152 | – | 1.615 | 0.000 | |
| O3 difference | 0.956 | 0.936 | – | 0.977 | 0.000 | 0.942 | 0.919 | – | 0.966 | 0.000 | |
| CO difference | 0.998 | 0.997 | – | 1.000 | 0.056 | 0.996 | 0.994 | – | 0.998 | 0.000 | |
| NO2 difference | 1.047 | 1.002 | – | 1.095 | 0.042 | 1.088 | 1.039 | – | 1.139 | 0.000 | |
| Income b | <1.0 | Reference | 0.042 | Reference | 0.020 | ||||||
| 1.0~2.0 | 0.761 | 0.172 | – | 0.761 | 0.172 | 0.298 | 0.140 | – | 0.634 | 0.002 | |
| 2.0~3.0 | 1.217 | 0.320 | – | 1.217 | 0.320 | 0.518 | 0.265 | – | 1.014 | 0.055 | |
| 3.0~4.0 | 1.104 | 0.290 | – | 1.104 | 0.290 | 0.449 | 0.229 | – | 0.879 | 0.020 | |
| 4.0~5.0 | 1.051 | 0.273 | – | 1.051 | 0.273 | 0.445 | 0.226 | – | 0.879 | 0.020 | |
| >5.0 | 1.090 | 0.278 | – | 1.090 | 0.278 | 0.462 | 0.231 | – | 0.925 | 0.029 | |
| Air purifier | 1.236 | 1.048 | – | 1.457 | 0.012 | 1.225 | 1.031 | – | 1.456 | 0.021 | |
| History of bronchiolitis | 1.702 | 1.388 | – | 2.087 | 0.000 | 1.538 | 1.243 | – | 1.902 | 0.000 | |
| Variables | Univariate Model | Multivariate Model § | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||||||
| Night-noise difference rate (%) a | <−5.74 | Reference | 0.000 | Reference | 0.000 | ||||||
| −5.74~−1.82 | 1.016 | 0.822 | – | 1.255 | 0.886 | 0.989 | 0.794 | – | 1.233 | 0.924 | |
| −1.82~1.04 | 1.627 | 1.310 | – | 2.021 | 0.000 | 1.313 | 1.032 | – | 1.669 | 0.026 | |
| >1.04 | 2.006 | 1.610 | – | 2.499 | 0.000 | 1.724 | 1.360 | – | 2.185 | 0.000 | |
| Age | 1.243 | 1.154 | – | 1.339 | 0.000 | 1.170 | 1.081 | – | 1.267 | 0.000 | |
| History of allergic disease, Father | 1.577 | 1.341 | – | 1.854 | 0.000 | 1.467 | 1.231 | – | 1.750 | 0.000 | |
| History of allergic disease, Mother | 1.428 | 1.220 | – | 1.670 | 0.000 | 1.370 | 1.156 | – | 1.624 | 0.001 | |
| O3 difference rate | 0.956 | 0.936 | – | 0.977 | 0.000 | 0.979 | 0.970 | – | 0.987 | 0.000 | |
| CO difference rate | 0.998 | 0.997 | – | 1.000 | 0.056 | 0.982 | 0.974 | – | 0.989 | 0.000 | |
| NO2 difference rate | 1.021 | 0.997 | – | 1.045 | 0.086 | 1.022 | 1.011 | – | 1.033 | 0.000 | |
| Income b | <1.0 | Reference | 0.042 | Reference | 0.019 | ||||||
| 1.0~2.0 | 0.761 | 0.172 | – | 0.761 | 0.172 | 0.284 | 0.133 | – | 0.604 | 0.001 | |
| 2.0~3.0 | 1.217 | 0.320 | – | 1.217 | 0.320 | 0.496 | 0.253 | – | 0.970 | 0.041 | |
| 3.0~4.0 | 1.104 | 0.290 | – | 1.104 | 0.290 | 0.440 | 0.224 | – | 0.863 | 0.017 | |
| 4.0~5.0 | 1.051 | 0.273 | – | 1.051 | 0.273 | 0.438 | 0.222 | – | 0.865 | 0.017 | |
| >5.0 | 1.090 | 0.278 | – | 1.090 | 0.278 | 0.443 | 0.222 | – | 0.887 | 0.022 | |
| Air purifier | 1.236 | 1.048 | – | 1.457 | 0.012 | 1.229 | 1.034 | – | 1.406 | 0.019 | |
| History of bronchiolitis | 1.702 | 1.388 | – | 2.087 | 0.000 | 1.504 | 1.215 | – | 1.861 | 0.000 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, A.-R.; Bang, J.-H.; Lee, S.-H.; Lee, J. What Is the Role of Night-Time Noise Exposure in Childhood Allergic Disease? Int. J. Environ. Res. Public Health 2022, 19, 2748. https://doi.org/10.3390/ijerph19052748
Kim A-R, Bang J-H, Lee S-H, Lee J. What Is the Role of Night-Time Noise Exposure in Childhood Allergic Disease? International Journal of Environmental Research and Public Health. 2022; 19(5):2748. https://doi.org/10.3390/ijerph19052748
Chicago/Turabian StyleKim, A-Ram, Jin-Hee Bang, Sung-Hee Lee, and Jiho Lee. 2022. "What Is the Role of Night-Time Noise Exposure in Childhood Allergic Disease?" International Journal of Environmental Research and Public Health 19, no. 5: 2748. https://doi.org/10.3390/ijerph19052748
APA StyleKim, A.-R., Bang, J.-H., Lee, S.-H., & Lee, J. (2022). What Is the Role of Night-Time Noise Exposure in Childhood Allergic Disease? International Journal of Environmental Research and Public Health, 19(5), 2748. https://doi.org/10.3390/ijerph19052748






