Emotional Dysregulation, Anxiety Symptoms and Insomnia in Individuals with Alcohol Use Disorder
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Data Analysis
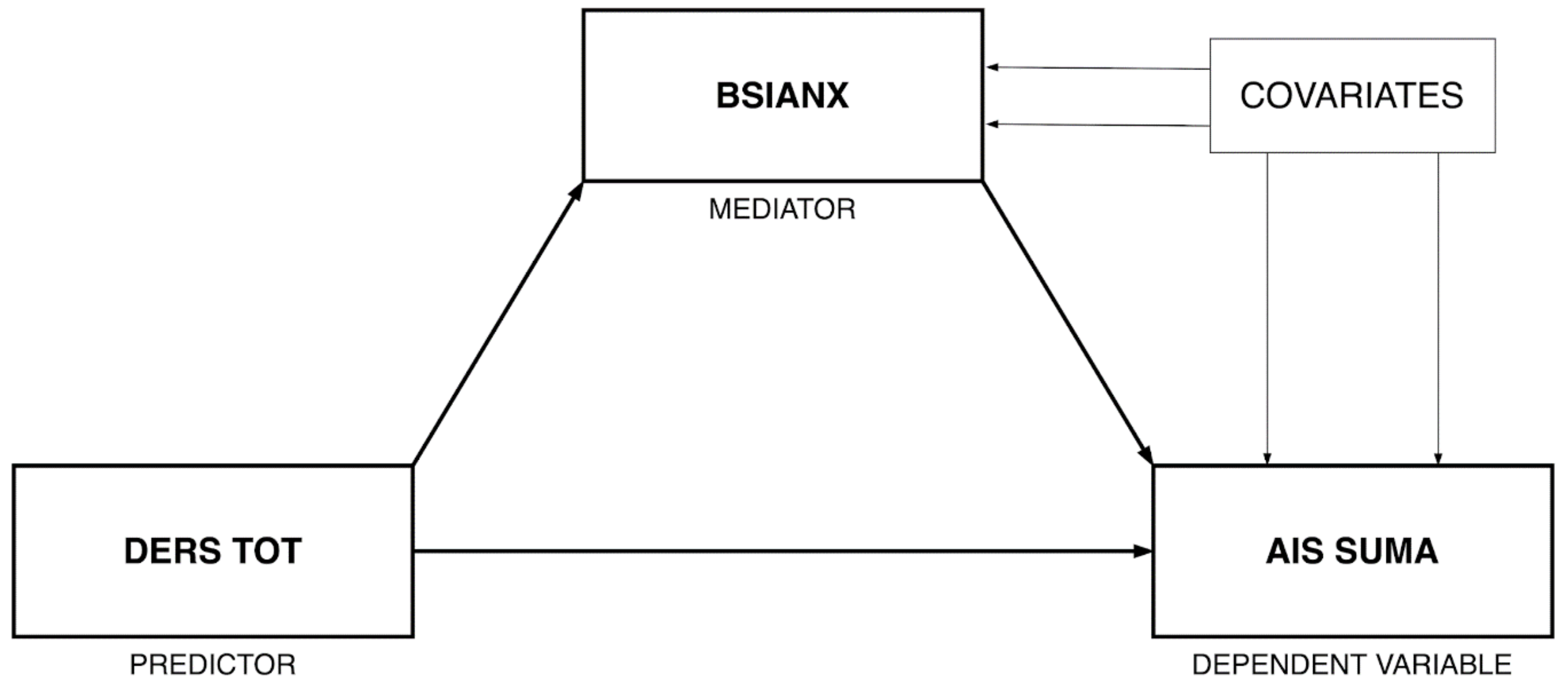
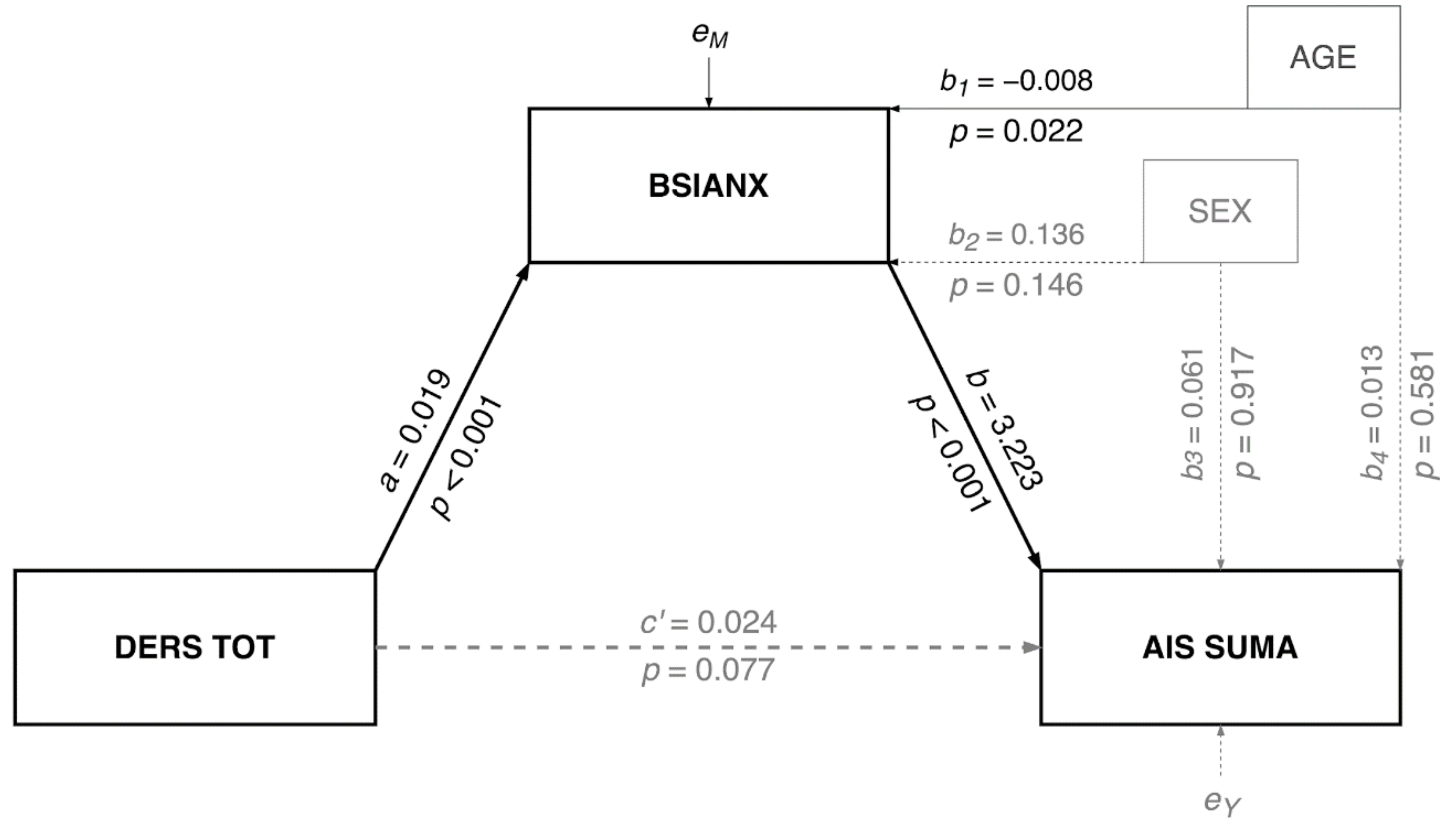
2.3.1. Mediation Model
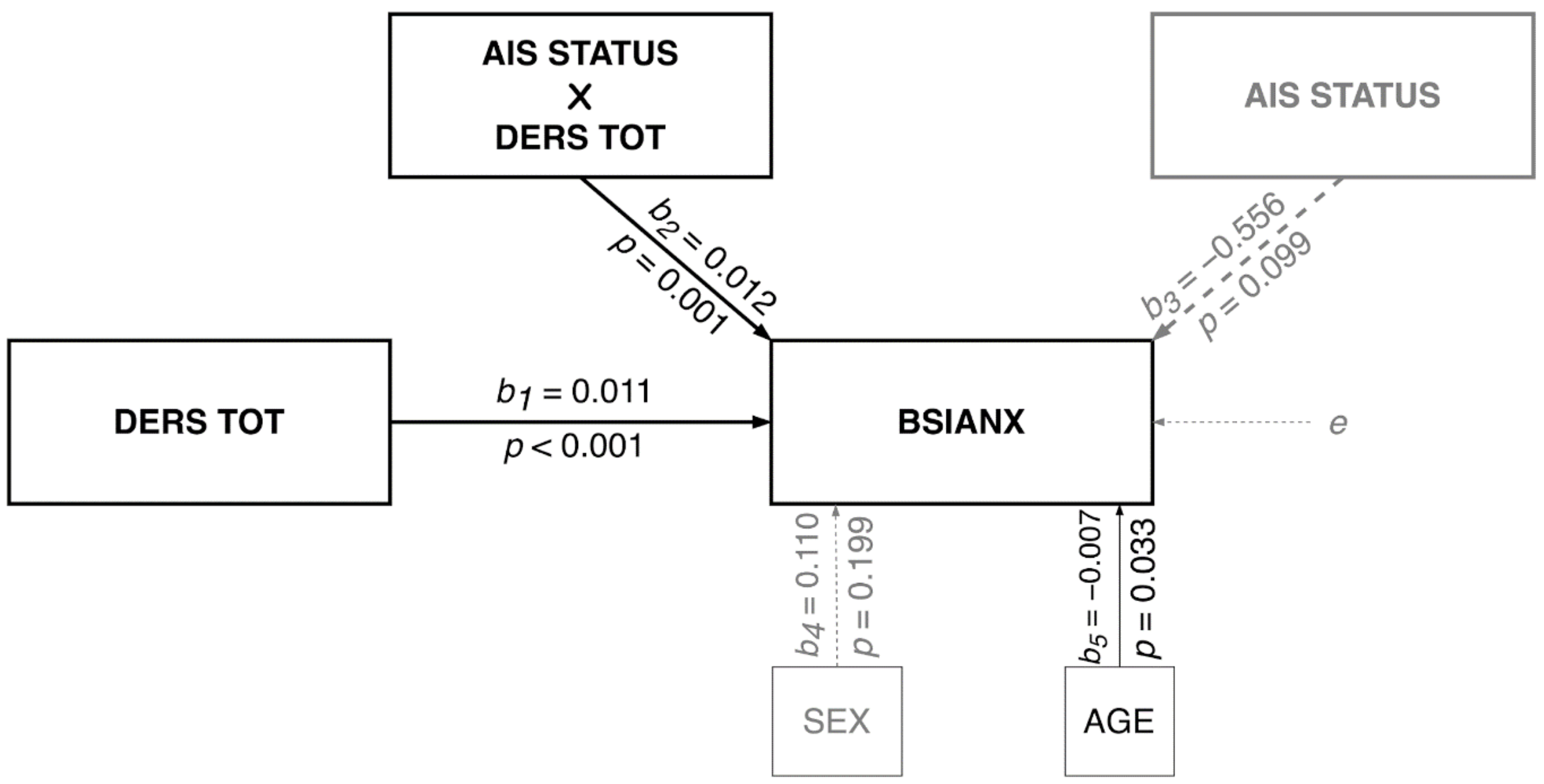
2.3.2. Moderation Model
3. Results
3.1. Mediation Model
3.2. Moderation Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baekeland, F.; Lundwall, L.; Shanahan, T.; Kissin, B. Clinical correlates of reported sleep disturbance in alcoholics. Q. J. Stud. Alcohol 1974, 35, 1230–1241. [Google Scholar] [CrossRef]
- Bokström, K.; Balldin, J. A rating scale for assessment of alcohol withdrawal psychopathology (AWIP). Alcohol. Clin. Exp. Res. 1992, 16, 241–249. [Google Scholar] [CrossRef]
- Brower, K.J.; Aldrich, M.S.; Robinson, E.A.; Zucker, R.A.; Greden, J.F. Insomnia, self-medication, and relapse to alcoholism. Am. J. Psychiatry 2001, 158, 399–404. [Google Scholar] [CrossRef] [Green Version]
- Caetano, R.; Clark, C.; Greenfield, T. Prevalence, trends, and incidence of alcohol withdrawal symptoms. Alcohol Health. Res. World 1998, 22, 73–79. [Google Scholar] [PubMed]
- Cohn, T.J.; Foster, J.H.; Peters, T.J. Sequential studies of sleep disturbance and quality of life in abstaining alcoholics. Addict. Biol. 2003, 8, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Escobar-Cordoba, F.; Avila-Cadavid, J.D.; Cote-Menendez, M. Complaints of insomnia in hospitalized alcoholics. Rev. Bras. Psiquiatr. 2009, 31, 261–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feuerlein, W. The acute alcohol withdrawal syndrome: Findings and problems. Br. J. Addict. Alcohol. Other Drugs. 1974, 69, 141–148. [Google Scholar] [CrossRef]
- Foster, J.; Marshall, E.; Peters, T. Application of a quality of life measure, the life situation survey (LSS), to alcohol dependent subjects in relapse and remission. Alcohol. Clin. Exp. Res. 2000, 24, 1687–1692. [Google Scholar] [CrossRef]
- Mello, N.; Mendelson, J. Behavioral studies of sleep patterns in alcoholics during intoxication and withdrawal. J. Pharmacol. Exp. Ther. 1970, 175, 94–112. [Google Scholar]
- Zhabenko, N.; Wojnar, M.; Brower, K.J. Prevalence and correlates of insomnia in a polish sample of alcohol-dependent patients. Alcohol. Clin. Exp. Res. 2012, 36, 1600–1607. [Google Scholar] [CrossRef] [Green Version]
- Szelenberger, W.; Skalski, M. Epidemiologia zaburzeń snu w Polsce. Doniesienie wstępne. In Zaburzenia snu. Diagnostyka i leczenie. Wybrane zagadnienia; Nowicki, Z., Szelenberger, W., Eds.; Biblioteka Psychiatrii Polskiej: Kraków, Poland, 1999; pp. 57–63. [Google Scholar]
- Kiejna, A.; Wojtyniak, B.; Rymaszewska, J.; Stokwiszewski, J. Prevalence of insomnia in Poland—Results of the National Health Interview Survey. Acta Neuropsychiatr. 2004, 16, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Vgontzas, A.N.; Tsigos, C.; Bixler, E.O.; Stratakis, C.A.; Zachman, K.; Kales, A.; Vela-Bueno, A.; Chrousos, G.P. Chronic insomnia and activity of the stress system: A preliminary study. J. Psychosom. Res. 1998, 45, 21–31. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Bixler, E.O.; Lin, H.M.; Prolo, P.; Mastorakos, G.; Vela-Bueno, A.; Kales, A.; Chrousos, G.P. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: Clinical implications. J. Clin. Endocrinol. Metab. 2001, 86, 3787–3794. [Google Scholar] [CrossRef]
- Bonnet, M.H.; Arand, D.L. 24-hour metabolic rate in insomnia and matched normal sleepers. Sleep 1995, 18, 581–588. [Google Scholar] [CrossRef]
- Nofzinger, E.A.; Buysse, D.; Germain, A.; Price, J.C.; Miewald, J.M.; Kupfer, D.J. Functional neuroimaging evidence for hyperarousal in insomnia. Am. J. Psychiatry 2004, 161, 2126–2129. [Google Scholar] [CrossRef]
- Bonnet, M.H. Hyperarousal and insomnia. Sleep Med. Rev. 2010, 14, 33. [Google Scholar] [CrossRef]
- Riemann, D.; Spiegelhalder, K.; Feige, B.; Voderholzer, U.; Berger, M.; Perlis, M.; Nissen, H. The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Med. Rev. 2010, 14, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Brower, K.J.; Aldrich, M.S.; Hall, J.M. Polysomnographic and subjective sleep predictors of alcoholic relapse. Alcohol Clin. Exp. Res. 1998, 22, 1864–1871. [Google Scholar] [CrossRef]
- Gann, H.; Feige, B.; Hohagen, F.; van Calker, D.; Geiss, D.; Dieter, R. Sleep and the cholinergic rapid eye movement sleep induction test in patients with primary alcohol dependence. Biol. Psychiatry 2001, 50, 383–390. [Google Scholar] [CrossRef]
- Gillin, J.C.; Smith, T.L.; Irwin, M.; Butters, N.; Demodena, A.; Schuckit, M. Increased pressure for rapid eye movement sleep at time of hospital admission predicts relapse in nondepressed patients with primary alcoholism at 3-month follow-up. Arch. Gen. Psychiatry 1994, 51, 189–197. [Google Scholar] [CrossRef]
- Colrain, I.M.; Turlington, S.; Baker, F.C. Impact of alcoholism on sleep architecture and EEG power spectra in men and women. Sleep 2009, 32, 1341–1352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drummond, S.P.; Gillin, J.C.; Smith, T.L.; DeModena, A. The sleep of abstinent pure primary alcoholic patients: Natural course and relationship to relapse. Alcohol. Clin. Exp. Res. 1998, 22, 1796–1802. [Google Scholar] [CrossRef] [PubMed]
- Currie, S.R.; Clark, S.; Rimac, S.; Malhotra, S. Comprehensive assessment of insomnia in recovering alcoholics using daily sleep diaries and ambulatory monitoring. Alcohol. Clin. Exp. Res. 2003, 27, 1262–1269. [Google Scholar] [CrossRef]
- Wong, M.M.; Brower, K.J.; Nigg, J.T.; Zucker, R.A. Childhood sleep problems, response inhibition, and alcohol and drug outcomes in adolescence and young adulthood. Alcohol. Clin. Exp. Res. 2010, 34, 1033–1044. [Google Scholar] [CrossRef] [Green Version]
- Ohayon, M.M.; Caulet, M.; Lemoine, P. Comorbidity of mental and insomnia disorders in the general population. Compr. Psychiatry 1998, 39, 185–197. [Google Scholar] [CrossRef]
- Saletu-Zyhlarz, G.; Saletu, B.; Anderer, P.; Brandstätter, N.; Frey, R.; Gruber, G.; Klösch, G.; Mandl, M.; Grünberger, J.; Linzmayer, L. Nonorganic insomnia in generalized anxiety disorder. Controlled studies on sleep, awakening and daytime vigilance utilizing polysomnography and EEG mapping. Neuropsychobiology 1997, 36, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Monti, J.M.; Monti, D. Sleep disturbance in generalized anxiety disorder and its treatment. Sleep Med. Rev. 2000, 4, 263–276. [Google Scholar] [CrossRef]
- Harvey, A.G. A cognitive model of insomnia. Behav. Res. Ther. 2002, 40, 869–893. [Google Scholar] [CrossRef]
- Neckelmann, D.; Mykletun, A.; Dahl, A.A. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep 2007, 30, 873–880. [Google Scholar] [CrossRef] [Green Version]
- Grant, B.F.; Goldstein, R.B.; Saha, T.D.; Chou, S.P.; Jung, J.; Zhang, H.; Pickering, R.P.; Ruan, W.J.; Smith, S.M.; Huang, B.; et al. Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 2015, 72, 757–766. [Google Scholar] [CrossRef] [Green Version]
- Kushner, M.G.; Abrams, K.; Thuras, P.; Hanson, K.L.; Brekke, M.; Sletten, S. Follow-up study of anxiety disorder and alcohol dependence in comorbid alcoholism treatment patients. Alcohol Clin. Exp. Res. 2005, 29, 1432–1443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geoffroy, P.A.; Tebeka, S.; Blanco, C.; Dubertret, C.; Le Strat, Y. Shorter and longer durations of sleep are associated with an increased twelve-month prevalence of psychiatric and substance use disorders: Findings from a nationally representative survey of US adults (NESARC-III). J. Psychiatr. Res. 2020, 124, 34–41. [Google Scholar] [CrossRef]
- Mennin, D.S.; Heimberg, R.G.; Turk, C.L.; Fresco, D.M. Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behav. Res. Ther. 2005, 43, 1281–1310. [Google Scholar] [CrossRef] [PubMed]
- Tsypes, A.; Aldao, A.; Mennin, D.S. Emotion dysregulation and sleep difficulties in generalized anxiety disorder. J. Anxiety. Disord. 2013, 27, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Roth, T. Insomnia: Definition, prevalence, etiology, and consequences. J. Clin. Sleep Med. 2007, 3 (Suppl. 5), S7–S10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández-Mendoza, J.; Vela-Bueno, A.; Vgontzas, A.N.; Ramos-Platón, M.J.; Olavarrieta-Bernardino, S.; Bixler, E.O.; De la Cruz-Troca, J.J. Cognitive-emotional hyperarousal as a premorbid characteristic of individuals vulnerable to insomnia. Psychosom. Med. 2010, 72, 397–403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palagini, L.; Cipollone, G.; Masci, I.; Caruso, D.; Paolilli, F.; Perugi, G.; Riemann, D. Insomnia symptoms predict emotional dysregulation, impulsivity and suicidality in depressive bipolar II patients with mixed features. Compr. Psychiatry 2019, 89, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Cano, G.; Mochizuki, T.; Saper, C.B. Neural circuitry of stress-induced insomnia in rats. J. Neurosci. 2008, 28, 10167–10184. [Google Scholar] [CrossRef]
- Markarian, S.A.; Pickett, S.M.; Deveson, D.F.; Kanona, B.B. A model of BIS/BAS sensitivity, emotion regulation difficulties, and depression, anxiety, and stress symptoms in relation to sleep quality. Psychiatry Res. 2013, 210, 281–286. [Google Scholar] [CrossRef]
- Kirwan, M.; Pickett, S.M.; Jarrett, N.L. Emotion regulation as a moderator between anxiety symptoms and insomnia symptom severity. Psychiatry Res. 2017, 254, 40–47. [Google Scholar] [CrossRef]
- Petit, G.; Luminet, O.; Maurage, F.; Tecco, J.; Lechantre, S.; Ferauge, M.; Gross, J.J.; De Timary, P. Emotion Regulation in Alcohol Dependence. Alcohol. Clin. Exp. Res. 2015, 39, 2471–2479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kober, H. Emotion Regulation in Substance Use Disorders. In Handbook of Emotion Regulation; Gross, J.J., Ed.; The Guilford Press: New York, NY, USA, 2014; pp. 428–446. [Google Scholar]
- Yoo, S.S.; Gujar, N.; Hu, P.; Jolesz, F.A.; Walker, M.P. The human emotional brain without sleep—A prefrontal amygdala disconnect. Curr. Biol. 2007, 17, R877-8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstein, A.N.; Walker, M.P. The role of sleep in emotional brain function. Annu. Rev. Clin. Psychol. 2014, 10, 679–708. [Google Scholar] [CrossRef] [Green Version]
- Buysse, D.J. Insomnia. JAMA 2013, 309, 706–716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lugaresi, E.; Cirignotta, F.; Zucconi, M.; Mondini, S.; Lenzi, P.L.; Coccagna, G. Good and poor sleepers: An epidemiological survey of the San Marino population. In Sleep/Wake Disorders. Natural History, Epidemiology, and LongTerm Evolution; Guilleminault, C., Lugaresi, E., Eds.; Raven Press: New York, NY, USA, 1983; pp. 1–12. [Google Scholar]
- Alterman, A.I.; Cacciola, J.S.; Ivey, M.A.; Habing, B.; Lynch, K.G. Reliability and Validity of the Alcohol Short Index of Problems and a Newly Constructed Drug Short Index of Problems. J. Stud. Alcohol Drugs 2009, 70, 304–307. [Google Scholar] [CrossRef] [Green Version]
- Smith, G.R.; Burnam, M.A.; Mosley, C.L.; Hollenberg, J.A.; Mancino, M.; Grimes, W. Reliability and Validity of the Substance Abuse Outcomes Module. Psychiatr. Serv. 2006, 57, 1452–1460. [Google Scholar] [CrossRef]
- Dragan, M. Problemowe Picie Alkoholu Przez Młode Kobiety. Rola Niekorzystnych Doświadczeń z Dzieciństwa i Samoregulacji Emocji; Wydawnictwo Naukowe Scholar: Warsaw, Poland, 2016. [Google Scholar]
- Gratz, K.L.; Roemer, L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Melisaratos, N. The Brief Symptom Inventory: An introductory report. Psychol. Med. 1983, 13, 595–605. [Google Scholar] [CrossRef] [Green Version]
- Fornal-Pawłowska, M.; Wołyńczyk-Gmaj, D.; Szelenberger, W. Walidacja Ateńskiej Skali Bezsenności [Validation of the Polish version of the Athens Insomnia Scale]. Psychiatr. Pol. 2011, 45, 211–221. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Spielman, A.J.; Caruso, L.S.; Glovinsky, P.B. A behavioral perspective on insomnia treatment. Psychiatr. Clin. N. Am. 1987, 10, 541–553. [Google Scholar] [CrossRef]
- Palagini, L.; Moretto, U.; Novi, M.; Masci, I.; Caruso, D.; Drake, C.L.; Riemann, D. Lack of Resilience Is Related to Stress-Related Sleep Reactivity, Hyperarousal, and Emotion Dysregulation in Insomnia Disorder. J Clin Sleep Med. 2018, 14, 759–766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brower, K.J. Insomnia, alcoholism and relapse. Sleep. Med. Rev. 2003, 7, 523–539. [Google Scholar] [CrossRef]
- Fairholme, C.P.; Nosen, E.L.; Nillni, Y.I.; Schumacher, J.A.; Tull, M.T.; Coffey, S.F. Sleep disturbance and emotion dysregulation as transdiagnostic processes in a comorbid sample. Behav. Res. Ther. 2013, 51, 540–546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altena, E.; Micoulaud-Franchi, J.A.; Geoffroy, P.A.; Sanz-Arigita, E.; Bioulac, S.; Philip, P. The bidirectional relation between emotional reactivity and sleep: From disruption to recovery. Behav. Neurosci. 2016, 130, 336–350. [Google Scholar] [CrossRef] [PubMed]
- Van Someren, E.J.; Cirelli, C.; Dijk, D.J.; Van Cauter, E.; Schwartz, S.; Chee, M.W. Disrupted sleep: From molecules to cognition. J. Neurosci. 2015, 35, 13889–13895. [Google Scholar] [CrossRef]
- Perogamvros, L.; Schwartz, S. Sleep and emotional functions. Curr. Top. Behav. Neurosci. 2015, 25, 411–431. [Google Scholar] [CrossRef] [PubMed]
- McCall, W.V.; Black, C.G. The link between suicide and insomnia: Theoretical mechanisms. Curr. Psychiatry Rep. 2013, 15, 389. [Google Scholar] [CrossRef] [Green Version]
- Harvey, A.G.; Murray, G.; Chandler, R.A.; Soehner, A. Sleep disturbance as transdiagnostic: Consideration of neurobiological mechanisms. Clin. Psychol. Rev. 2011, 3, 225–235. [Google Scholar]
- Kolla, B.P.; Mansukhani, M.P.; Schneekloth, T. Pharmacological treatment of insomnia in alcohol recovery: A systematic review. Alcohol Alcohol. 2011, 46, 578–585. [Google Scholar] [CrossRef]
- Smith, M.T.; Huang, M.I.; Manber, R. Cognitive behavior therapy for chronic insomnia occurring within the context of medical and psychiatric disorders. Clin. Psych. Rev. 2005, 25, 559–592. [Google Scholar] [CrossRef]


| Individuals with Insomnia | Individuals without Insomnia | p a | |
|---|---|---|---|
| Age (years) b | 43.04 (10.59) (N = 107) | 42.73 (10.59) (N = 231) | 0.81 |
| Education (years) b | 12.97 (3.31) (N = 106) | 13.35 (4.17) (N = 231) | 0.41 |
| Biological sex (man/woman) | 88/19 (N = 107) | 195/36 (N = 231) | 0.36 |
| Severity of anxiety symptoms c | 1.12 (0.89) (N = 107) | 0.48 (0.56) (N = 231) | <0.001 |
| Duration of problematic alcohol use (years) b | 24.83 (34.55) (N = 75) | 12.15 (14.01) (N = 179) | 0.34 |
| Mean abstinence length (days) a | 71.21 (91.43) (N = 66) | 104.13 (178.13) (N = 94) | 0.17 |
| Emotional dysregulation | 91.88 (19.52) (N = 75) | 77.02 (18.49) (N = 179) | <0.001 |
| Severity of insomnia | 11.74 (3.21) (N = 107) | 3.71 (2.08) (N = 231) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wołyńczyk-Gmaj, D.; Jakubczyk, A.; Trucco, E.M.; Kobyliński, P.; Zaorska, J.; Gmaj, B.; Kopera, M. Emotional Dysregulation, Anxiety Symptoms and Insomnia in Individuals with Alcohol Use Disorder. Int. J. Environ. Res. Public Health 2022, 19, 2700. https://doi.org/10.3390/ijerph19052700
Wołyńczyk-Gmaj D, Jakubczyk A, Trucco EM, Kobyliński P, Zaorska J, Gmaj B, Kopera M. Emotional Dysregulation, Anxiety Symptoms and Insomnia in Individuals with Alcohol Use Disorder. International Journal of Environmental Research and Public Health. 2022; 19(5):2700. https://doi.org/10.3390/ijerph19052700
Chicago/Turabian StyleWołyńczyk-Gmaj, Dorota, Andrzej Jakubczyk, Elisa M. Trucco, Paweł Kobyliński, Justyna Zaorska, Bartłomiej Gmaj, and Maciej Kopera. 2022. "Emotional Dysregulation, Anxiety Symptoms and Insomnia in Individuals with Alcohol Use Disorder" International Journal of Environmental Research and Public Health 19, no. 5: 2700. https://doi.org/10.3390/ijerph19052700
APA StyleWołyńczyk-Gmaj, D., Jakubczyk, A., Trucco, E. M., Kobyliński, P., Zaorska, J., Gmaj, B., & Kopera, M. (2022). Emotional Dysregulation, Anxiety Symptoms and Insomnia in Individuals with Alcohol Use Disorder. International Journal of Environmental Research and Public Health, 19(5), 2700. https://doi.org/10.3390/ijerph19052700






