Intervention for Children with Obesity and Overweight and Motor Delays from Low-Income Families: Fostering Engagement, Motor Development, Self-Perceptions, and Playtime
Abstract
:1. Introduction
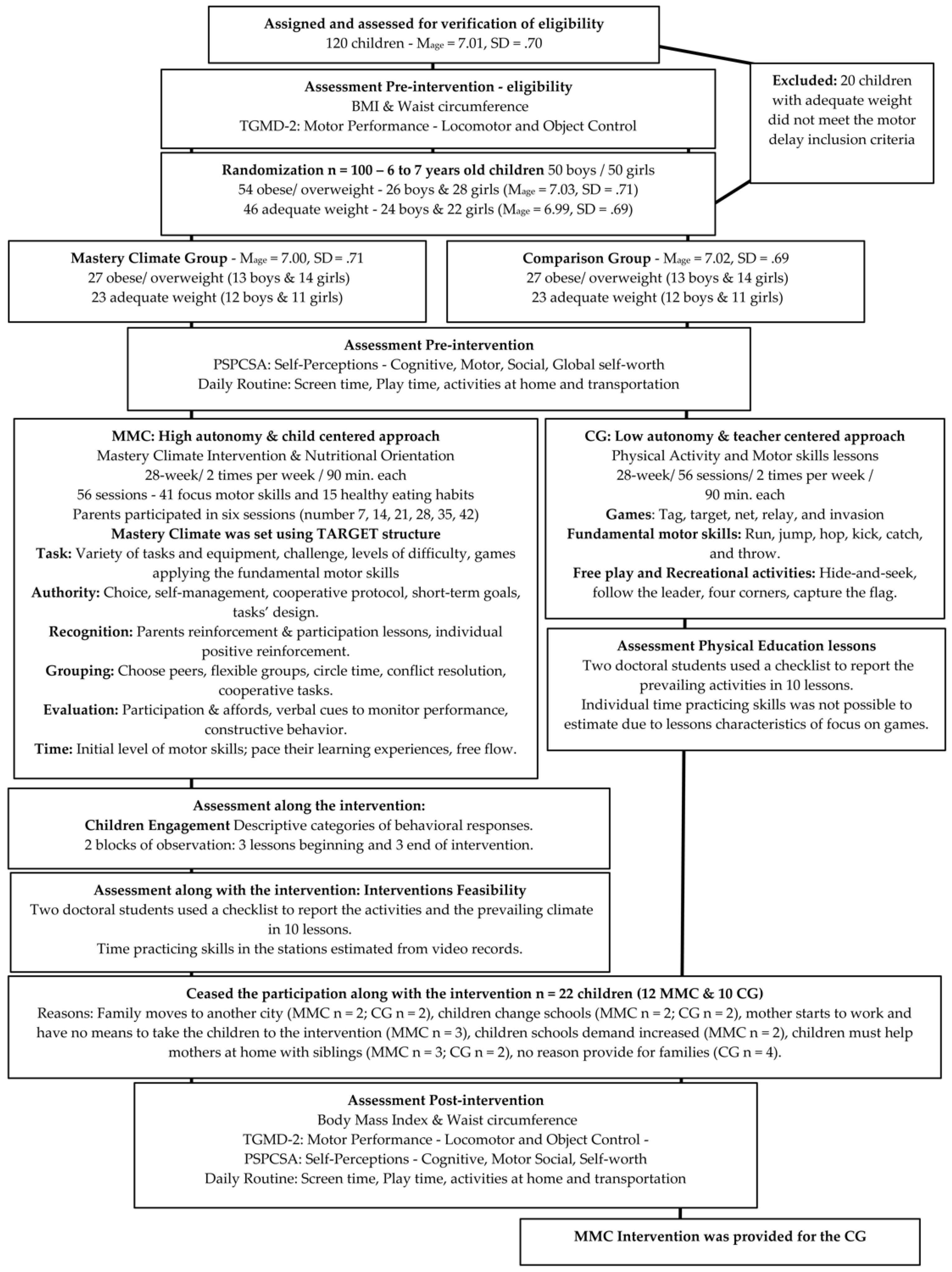
2. Materials and Methods
2.1. Participants
2.2. Instruments and Procedures
2.2.1. Children’s Routine at Home
2.2.2. Self-Perception
2.2.3. Body Mass Index
2.2.4. Motor Skills
2.2.5. Engagement in Intervention Lessons
2.3. Design and Implementation
2.3.1. Mastery Climate Group
2.3.2. Control Group
2.4. Data Analysis
3. Results
3.1. Children’s Daily Routine
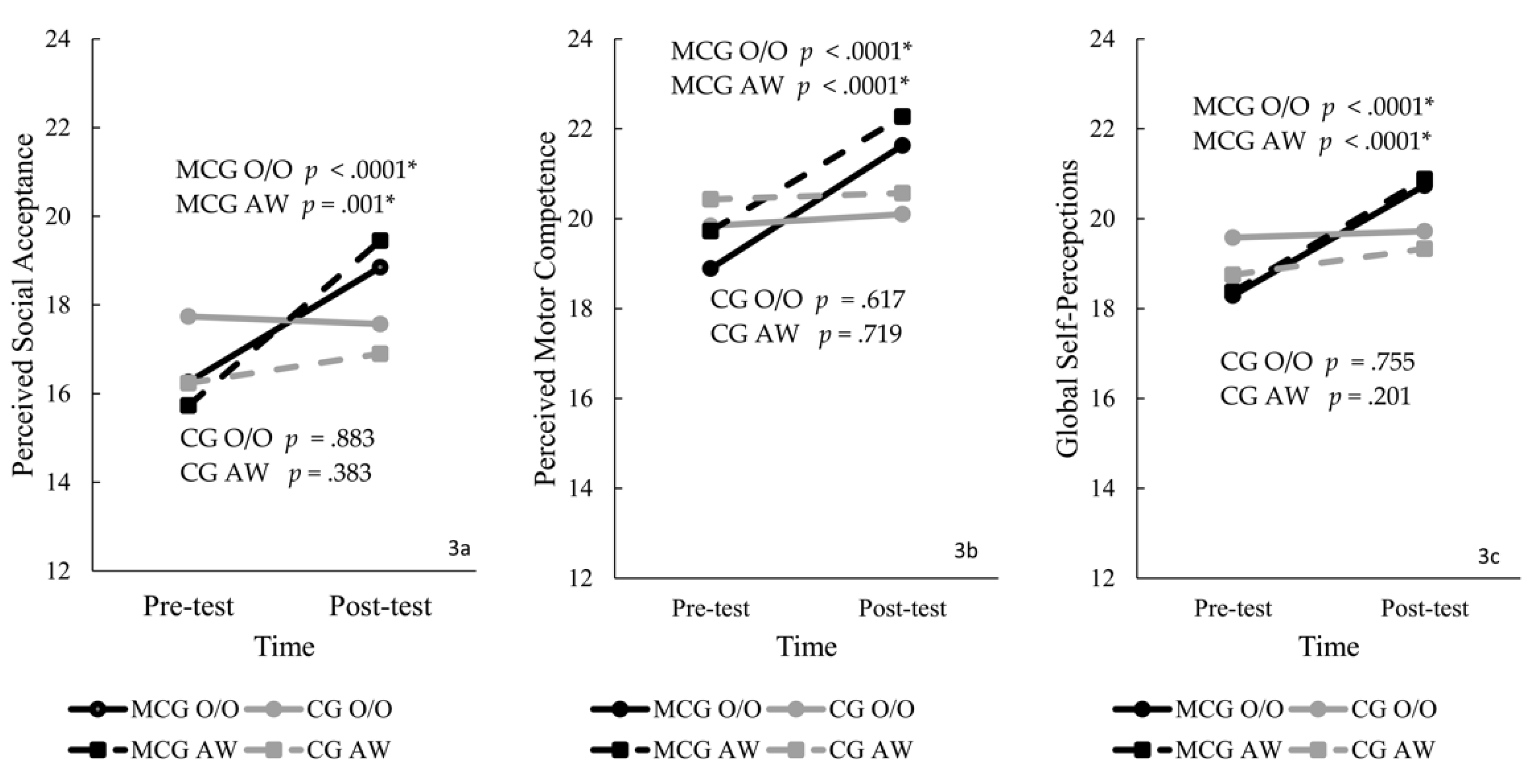
3.2. Self-Perceptions
3.3. Body Mass Index and Waist Circumference
3.4. Motor Skills
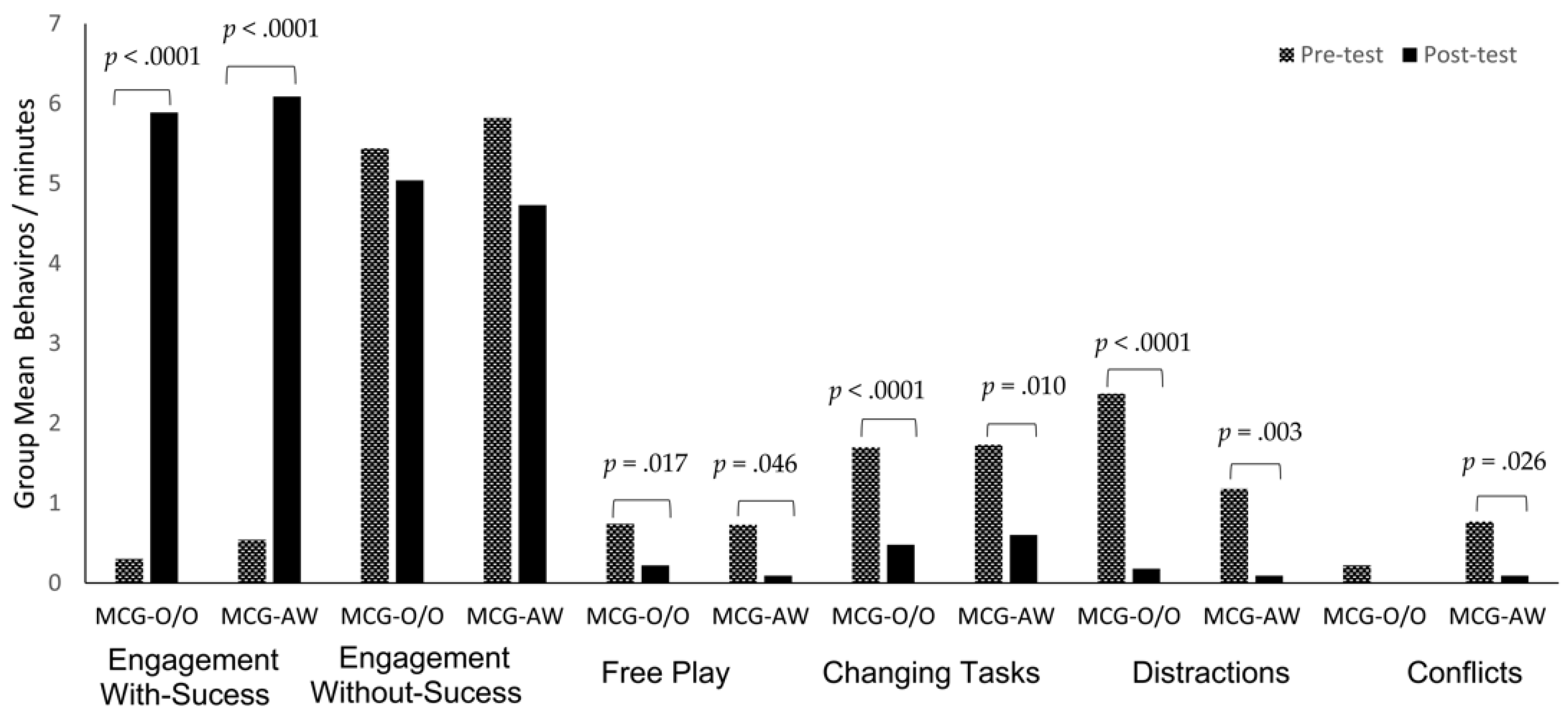
3.5. Engagement in the Intervention Lessons
4. Discussion
4.1. Children’s Daily Routine
4.2. Self-Perceptions
4.3. Body Mass Index and Waist Circumference
4.4. Motor Skills
4.5. Engagement in the Intervention Lessons
4.6. Study Limitations and Recommendations for Future Research
4.7. Practical Implication
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nemet, D. Childhood Obesity, Physical Activity, and Exercise—The Year That Was 2017: Normal-Weight Obese—Are We Missing a Population in Need? Pediatric Exerc. Sci. 2018, 30, 54–55. [Google Scholar] [CrossRef] [PubMed]
- D’Hondt, E.; Deforche, B.; De Bourdeaudhuij, I.; Lenoir, M. Relationship between motor skill and body mass index in 5- to 10-year-old children. Adapt. Phys. Act. Q. 2009, 26, 21–37. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M.; Liu, T.; ElGarhy, S. The Relationship Between Body Weight and Motor Skill Competence in Hispanic Low-SES Preschool Children. Early Child. Educ. J. 2017, 45, 529–535. [Google Scholar] [CrossRef] [Green Version]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental Movement Skills in Children and Adolescents. Sports Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hemmingsson, E. Early Childhood Obesity Risk Factors: Socioeconomic Adversity, Family Dysfunction, Offspring Distress, and Junk Food Self-Medication. Curr. Obes. Rep. 2018, 7, 204–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fairclough, S.J.; Dumuid, D.; Mackintosh, K.A.; Stone, G.; Dagger, R.; Stratton, G.; Davies, I.; Boddy, L.M. Adiposity, fitness, health-related quality of life and the reallocation of time between children’s school day activity behaviours: A compositional data analysis. Prev. Med. Rep. 2018, 11, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Elmesmari, R.; Martin, A.; Reilly, J.J.; Paton, J.Y. Comparison of accelerometer measured levels of physical activity and sedentary time between obese and non-obese children and adolescents: A systematic review. BMC Pediatr. 2018, 18, 2–22. [Google Scholar] [CrossRef] [PubMed]
- D’Hondt, E.; Gentier, I.; Deforche, B.; Tanghe, A.; Bourdeaudhuij, I.D.; Lenoir, M. Weight Loss and Improved Gross Motor Coordination in Children as a Result of Multidisciplinary Residential Obesity Treatment. Obesity 2011, 19, 1999–2005. [Google Scholar] [CrossRef] [PubMed]
- Morano, M.; Colella, D.; Rutigliano, I.; Fiore, P.; Pettoello-Mantovani, M.; Campanozzi, A. A multi-modal training programme to improve physical activity, physical fitness and perceived physical ability in obese children. J. Sports Sci. 2014, 32, 345–353. [Google Scholar] [CrossRef]
- Cooper, A.R.; Goodman, A.; Page, A.S.; Sherar, L.B.; Esliger, D.W.; van Sluijs, E.M.F.; Andersen, L.B.; Anderssen, S.; Cardon, G.; Davey, R.; et al. Objectively measured physical activity and sedentary time in youth: The International children’s accelerometry database (ICAD). Int. J. Behav. Nutr. Phys. Act. 2015, 12, 2–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Todendi, P.F.; Brand, C.; de Castro Silveira, J.F.; Burns, R.D.; Martínez, J.A.; Fiegenbaum, M.; Reis Gaya, A.; Pollo Renner, J.D.; Reuter, C.P.; de Moura Valim, A.R. Cardiorespiratory Fitness and Muscular Strength Moderates the Relationship between FNDC5 Polymorphism and Adiposity in Children and Adolescents. Int. J. Environ. Res. Public Health 2021, 18, 9797. [Google Scholar] [CrossRef]
- Nooijen, C.F.; Galanti, M.R.; Engström, K.; Möller, J.; Forsell, Y. Effectiveness of interventions on physical activity in overweight or obese children: A systematic review and meta-analysis including studies with objectively measured outcomes. Obes. Rev. 2017, 18, 195–213. [Google Scholar] [CrossRef] [PubMed]
- Cliff, D.P.; Wilson, A.; Okely, A.D.; Mickle, K.J.; Steele, J.R. Feasibility of SHARK: A physical activity skill-development program for overweight and obese children. J. Sci. Med. Sport 2007, 10, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Griffin, K.; Meaney, K.; Hart, M. The Impact of a Mastery Motivational Climate on Obese and Overweight Children’s Commitment to and Enjoyment of Physical Activity: A Pilot Study. Am. J. Health Educ. 2013, 44, 1–8. [Google Scholar] [CrossRef]
- Ames, C. Achievement goals, motivational climate, and motivational processes. In Motivation in Sport and Exercise; Roberts, G.C., Ed.; Human Kinetics Publishers: Champaign, IL, USA, 1992; pp. 161–176. [Google Scholar]
- Ames, C. Classroom: Goals, structures, and student motivation. J. Educ. Psychol. 1992, 84, 409–414. [Google Scholar] [CrossRef]
- Ames, C.; Archer, J. Achievement of goals in the classroom: Students’ learning strategies and motivation process. J. Educ. Psychol. 1988, 80, 260–267. [Google Scholar] [CrossRef]
- Epstein, J. Family structure and students’ motivation: A development perspective. In Research on Motivation in Education; Ames, C., Ames, R., Eds.; Academic Press: New York, NY, USA, 1989; Volume 3, pp. 259–295. [Google Scholar]
- Valentini, N.C.; Rudisill, M.E. An inclusive mastery climate intervention and the motor skill development of children with and without disability. Adapt. Phys. Act. Q. 2004, 21, 330–347. [Google Scholar] [CrossRef]
- Valentini, N.C.; Rudisill, M.E. Motivational climate, motor-skill development, and perceived competence: Two studies of developmentally delayed kindergarten children. J. Teach. Phys. Educ. 2004, 23, 216–234. [Google Scholar] [CrossRef]
- Valentini, N.C.; Rudisill, M.E.; Goodway, J.D. Incorporating a mastery climate into elementary physical education: It’s developmentally appropriate. J. Phys. Educ. Recreat. Danc. 1999, 70, 28–32. [Google Scholar] [CrossRef]
- Hastie, P.A.; Rudisill, M.E.; Boyd, K. An ecological analysis of a preschool mastery climate physical education programme. Phys. Educ. Sport Pedagog. 2016, 21, 217–232. [Google Scholar] [CrossRef]
- WHO—World Health Organization: Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneve, Switzerland, 2006.
- Ulrich, D. Test of Gross Motor Development; Prod-Ed: Austin, TX, USA, 2000. [Google Scholar]
- Serrano, J.; Neto, C. As rotinas de vida diária das crianças com idades compreendidas entre os 7 e os 10 anos nos meios rural e urbano. In O Jogo e o Desenvolvimento da Criança; Neto, C., Ed.; Edições FMH: Lisboa, Portugal, 1997; pp. 207–226. [Google Scholar]
- Brauner, L.; Valentini, N.C.; de Souza, M.S.; Zanella, L.W.; Berleze, A. A influência de um programa de iniciação esportiva no desempenho motor e na rotina de atividades de crianças. Braz. J. Phys. Educ. Sports 2019, 33, 569–586. [Google Scholar]
- Harter, S.; Pike, R. The Pictorial Scale of Perceived Competence and Social Acceptance—PSPCSA; University of Denver Press: Denver, CO, USA, 1981. [Google Scholar]
- Valentini, N.C.; Bandeira, P.F.R.; Rudisill, M.E. Validity and Reliability of the Pictorial Scale of Perceived Competence and Social Acceptance for Brazilian. Braz. J. Phys. Educ. Sports 2020, 34, 331–344. [Google Scholar]
- Valentini, N.C. Validity and Reliability of the TGMD-2 for Brazilian Children. J. Mot. Behav. 2012, 44, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Rink, J.E. Effective instruction in physical education. In Student Learning in Physical Education: Applying Research to Enhance Instruction; Silverman, S.J., Ennis, C.D., Eds.; Human Kinetics: Champaign, IL, USA, 1996; pp. 171–198. [Google Scholar]
- Rafaelli, M.; Koller, S.H.; Reppold, C.T.; Kuschick, M.B.; Krum, F.B.; Bandeira, D.R.; Simões, C. Gender differences in Brazilian street youth’s family circumstances and experiences on the street. Child Abus. Negl. 2000, 24, 1431–1441. [Google Scholar] [CrossRef] [Green Version]
- Valentini, N.C.; Clark, J.E.; Whitall, J. Developmental co-ordination disorder in socially disadvantaged Brazilian children. Child Care Health Dev. 2015, 41, 970–979. [Google Scholar] [CrossRef]
- Borhese, M.M.; Tremblay, M.S.; Katzmarzyk, P.T.; Tudor-Locke, C.; Schuna, J.M., Jr.; Leduc, G.; Boyer, C.; LeBlanc, A.G.; Chaput, J.-P. Mediating role of television time, diet patterns, physical activity and sleep duration in the association between television in the bedroom and adiposity in 10-year-old children. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 2–10. [Google Scholar]
- AAP—American Academy of Pediatrics. Council on Communications and Media. Media use in school-aged children and adolescents. Pediatrics 2016, 138, e20162592. [Google Scholar] [CrossRef]
- Campbell, K.J.; Lioret, S.; McNaughton, S.A.; Crawford, D.A.; Salmon, J.; Ball, K.; McCallum, Z.; Gerner, B.E.; Spence, A.C.; Cameron, A.J.; et al. A parent-focused intervention to reduce infant obesity risk behaviors: A randomized trial. Pediatrics 2013, 131, 652–660. [Google Scholar] [CrossRef] [Green Version]
- French, S.A.; Sherwood, N.E.; Jaka, M.M.; Haapala, J.L.; Ebbeling, C.B.; Ludwig, D.S. Physical changes in the home environment to reduce television viewing and sugar-sweetened beverage consumption among 5- to 12-year-old children: A randomized pilot study. Pediatric Obes. 2016, 11, 12–15. [Google Scholar] [CrossRef] [Green Version]
- Brauner, L.M.; Valentini, N.C.; de Souza, M.S. Youth sports program influences children’s perceived competence? Psico-USF 2017, 22, 527–539. [Google Scholar] [CrossRef] [Green Version]
- Kemp, C.; Pienaar, A.E. The effect of a physical activity, diet and behaviour modification intervention on the self-perception of 9 to 12 year old overweight and obese children: Physical activity and health. Afr. J. Phys. Health Educ. Recreat. Danc. 2010, 16, 101–116. [Google Scholar] [CrossRef]
- Nobre, G.C.; Bandeira, P.F.R.; Ramalho, M.H.S.; Nobre, F.S.S.; Valentini, N.C. Self-perceptions of competence in children from socially vulnerable contexts, assisted and unassisted by social sports projects. J. Hum. Growth Dev. 2014, 25, 271–276. [Google Scholar] [CrossRef] [Green Version]
- Kaiser, L.; Smith, K.A.; Heleski, C.R.; Spence, L.J. Effects of a therapeutic riding program on at-risk and special education children. J. Am. Vet. Med. Assoc. 2006, 228, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Pless, M.; Carlsson, M.; Sundelin, C.; Persson, K. Pre-school children with developmental co-ordination disorder: Self-perceived competence and group motor skill intervention. Acta Paediatr. 2001, 90, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Valentini, N.C.; Pierosan, L.; Rudisill, M.E.; Hastie, P.A. Mastery and exercise play interventions: Motor skill development and verbal recall of children with and without disabilities. Phys. Educ. Sport Pedagog. 2016, 22, 349–363. [Google Scholar] [CrossRef]
- Robinson, L.E.; Rudisill, M.E.; Goodway, J.D. Instructional climates in preschool children who are at-risk. Part II: Perceived physical competence. Res. Q. Exerc. Sport 2009, 80, 543–551. [Google Scholar] [CrossRef]
- Zask, A.; Adams, J.K.; Brooks, L.O.; Hughes, D.F. Tooty Fruity Vegie: An obesity prevention intervention evaluation in Australian preschools. Health Promot. J. Aust. 2012, 23, 10–15. [Google Scholar] [CrossRef]
- Maia, E.G.; Dos Passos, C.M.; Levy, R.B.; Martins, A.P.B.; Mais, L.A.; Claro, R.M. What to expect from the price of healthy and unhealthy foods over time? The case from Brazil. Public Health Nutr. 2020, 23, 579–588. [Google Scholar] [CrossRef] [Green Version]
- Cohen, K.E.; Morgan, P.J.; Plotnikoff, R.C.; Callister, R.; Lubans, D.R. Physical Activity and Skills Intervention: SCORES: Cluster Randomized Controlled Trial. Med. Sci. Sports Exerc. 2015, 47, 765–774. [Google Scholar] [CrossRef]
- Zanella, L.W.; de Sousa, M.S.; Bandeira, P.F.R.; Nobre, G.C.; Valentini, N.C. Overweight and obesity: Motor intervention and influences on motor behavior. Motricidade 2016, 12, 42–53. [Google Scholar]
- Pífero, C.M.; Valentini, N.C. Tennis specialized skills: A beginning sport intervention study with school children. Braz. J. Phys. Educ. Sport 2010, 24, 149–163. [Google Scholar]
- Sampaio, D.F.; Valentini, N.C. Gymnastics rhythmic’ youth sport: Traditional approach and mastery motivational climate approach. J. Phys. Educ. 2015, 26, 1–10. [Google Scholar]
- Rudisill, M.E.; Johnson, J.L. Mastery Motivational Climates in Early Childhood Physical Education: What Have We Learned over the Years? J. Phys. Educ. Rec. Danc. 2018, 89, 26–32. [Google Scholar] [CrossRef]



| Children with Obesity/Overweight N (%) | Children with Adequate Weight N (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Children Activities at Home | MCG | CG | MCG | CG | |||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | ||
| Mobility to school | Bus | 14 (51.9) | 12 (44.4) | 4 (21.1) | 4 (21.1) | 3 (27.3) | 2 (18.2) | 4 (23.5) | 4 (23.5) |
| Walking/biking | 13 (48.1) | 15 (55.6) | 15 (78.9) | 15 (78.9) | 8 (72.7) | 9 (81.8) | 13 (76.5) | 13 (76.5) | |
| Space to play | Park/Backyard | 19 (70.4) | 19 (70.4) | 15 (78.9) | 15 (78.9) | 7 (63.6) | 7 (63.6) | 15 (88.2) | 15 (88.2) |
| Inside home | 8 (29.6) | 8 (29.6) | 4 (21.1) | 4 (21.1) | 4 (36.4) | 4 (36.4) | 2 (11.8) | 2 (11.8) | |
| House’ chores | Usually | 10 (37) | 15 (55.6) | 10 (52.6) | 13 (68.4) | 6 (54.5) | 8 (72.7) | 10 (58.8) | 10 (58.8) |
| Never | 17 (63.0) | 12 (44.4) | 9 (47.4) | 6 (31.6) | 5 (45.5) | 3 (27.3) | 7 (41.2) | 7 (41.2) | |
| Run | 2/3 times/week | 14 (52.9) | 25 (92.6) * | 4 (21.1) | 9 (47.4) * | 5 (45.5) | 9 (81.8) * | 8 (47.1) | 10 (58.8) |
| None | 13 (48.1) | 2 (7.4) | 15 (78.9) | 10 (52.6) | 6 (54.5) | 2 (18.2) | 9 (52.9) | 7 (41.2) | |
| Play ball | 2/3 times/week | 17 (63) | 26 (96.3) * | 14 (73.7) | 17 (89.5) | 9 (81.8) | 11 (100) | 16 (94.1) | 16 (94.1) |
| None | 10 (37.0) | 1 (3.7) | 5 (26.3) | 2 (10.5) | 2 (18.2) | 0 | 1 (5.9) | 1 (5.9) | |
| Dance and Circle Sing Games | 2/3 times/week | 4 (14.8) | 6 (22.2) | 6 (31.6) | 6 (31.6) | 5 (45.5) | 6 (54.5) | 8 (47.1) | 9 (52.9) |
| None | 23 (85.2) | 21 (77.8) | 13 (68.4) | 13 (68.4) | 6 (54.5) | 5 (45.5) | 9 (52.9) | 8 (47.10 | |
| Jump rope | 2/3 times/week | 9 (33.3) | 24 (88.9) * | 5 (26.3) | 5 (26.3) | 3 (27.3) | 8 (72.8) * | 3 (17.6) | 4 (23.5) |
| None | 18 (66.7) | 3 (11.1) | 14 (73.7) | 14 (73.7) | 8 (72.7) | 3 (27.5) | 14 (82.4) | 13 (76.5) | |
| Ride Bike | 2/3 times/week | 20 (74.1) | 26 (96.3) * | 12 (63.2) | 13 (68.4) | 8 (72.7) | 8 (72.8) | 13 (76.5) | 13 (76.5) |
| None | 7 (25.9) | 1 (3.7) | 7 (36.8) | 6 (31.6) | 3 (27.3) | 3 (27.3) | 4 (23.5) | 4 (23.5) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berleze, A.; Valentini, N.C. Intervention for Children with Obesity and Overweight and Motor Delays from Low-Income Families: Fostering Engagement, Motor Development, Self-Perceptions, and Playtime. Int. J. Environ. Res. Public Health 2022, 19, 2545. https://doi.org/10.3390/ijerph19052545
Berleze A, Valentini NC. Intervention for Children with Obesity and Overweight and Motor Delays from Low-Income Families: Fostering Engagement, Motor Development, Self-Perceptions, and Playtime. International Journal of Environmental Research and Public Health. 2022; 19(5):2545. https://doi.org/10.3390/ijerph19052545
Chicago/Turabian StyleBerleze, Adriana, and Nadia Cristina Valentini. 2022. "Intervention for Children with Obesity and Overweight and Motor Delays from Low-Income Families: Fostering Engagement, Motor Development, Self-Perceptions, and Playtime" International Journal of Environmental Research and Public Health 19, no. 5: 2545. https://doi.org/10.3390/ijerph19052545
APA StyleBerleze, A., & Valentini, N. C. (2022). Intervention for Children with Obesity and Overweight and Motor Delays from Low-Income Families: Fostering Engagement, Motor Development, Self-Perceptions, and Playtime. International Journal of Environmental Research and Public Health, 19(5), 2545. https://doi.org/10.3390/ijerph19052545






