Attention-Deficit/Hyperactivity Disorder Symptoms, Sensation-Seeking, and Sensory Modulation Dysfunction in Substance Use Disorder: A Cross Sectional Two-Group Comparative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Assessments
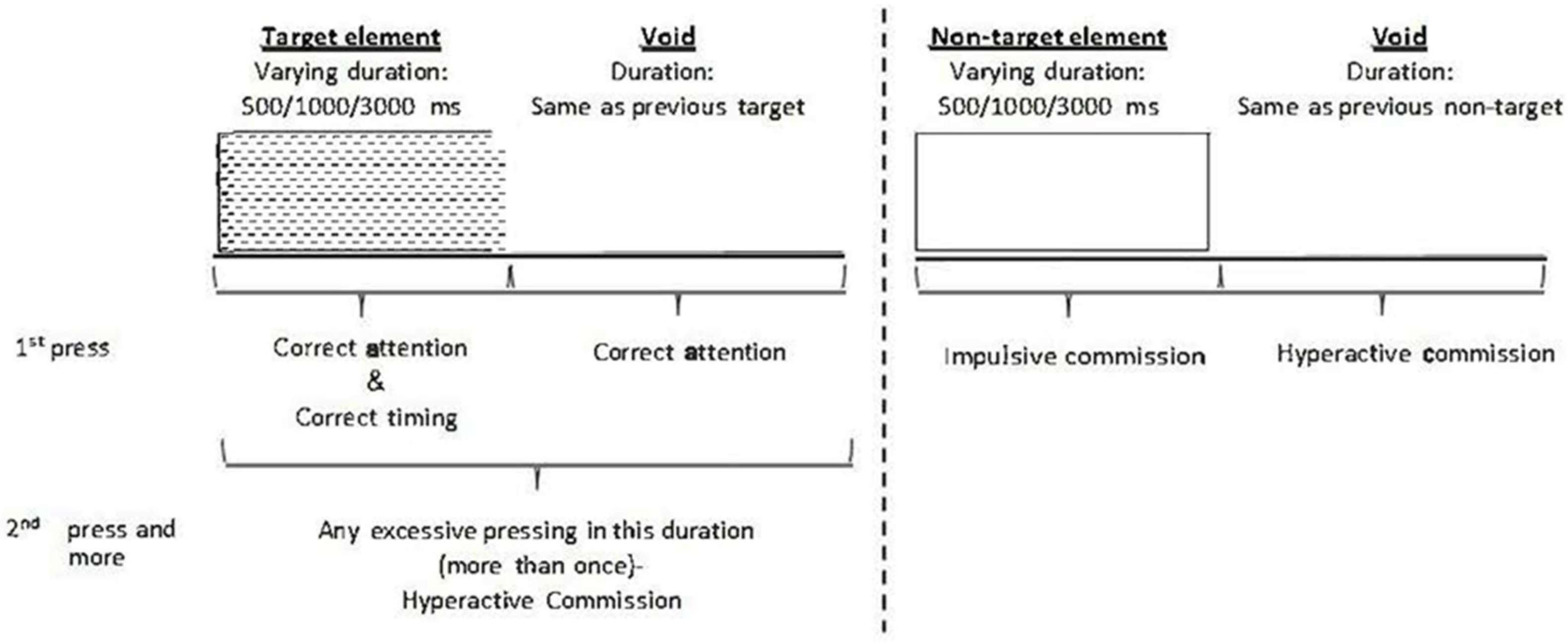
2.3.1. Performance Testing
2.3.2. Self-Report Questionnaires
2.4. Procedures
2.5. Data Analysis
3. Results
3.1. Demographic Characteristics
3.2. Substance Use Consumption in the Study Group
3.3. Group Differences in the MOXO-CPT Indexes
3.4. Group Differences in the BSSS Dimensions
3.5. SMD Distribution in the Study and Comparison Groups
3.6. SMD, MOXO-CPT, and Sensation-Seeking as Risk Factors for SUD
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilens, T.E.; Kaminski, T.A. The Co-Occurrence of ADHD and Substance Use Disorders. Psychiatr. Ann. 2018, 48, 328–332. [Google Scholar] [CrossRef]
- van de Glind, G.; Konstenius, M.; Koeter, M.W.J.; van Emmerik-van Oortmerssen, K.; Carpentier, P.J.; Kaye, S.; Degenhardt, L.; Skutle, A.; Franck, J.; Bu, E.T.; et al. Variability in the Prevalence of Adult ADHD in Treatment Seeking Substance Use Disorder Patients: Results from an International Multi-Center Study Exploring DSM-IV and DSM-5 Criteria. Drug Alcohol Depend. 2014, 134, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Zulauf, C.A.; Sprich, S.E.; Safren, S.A.; Wilens, T.E. The Complicated Relationship between Attention Deficit/Hyperactivity Disorder and Substance Use Disorders. Curr. Psychiatry Rep. 2014, 16, 436. [Google Scholar] [CrossRef] [PubMed]
- Fluyau, D.; Revadigar, N.; Pierre, C.G. Systematic Review and Meta-Analysis: Treatment of Substance Use Disorder in Attention Deficit Hyperactivity Disorder. Am. J. Addict. 2021, 30, 110–121. [Google Scholar] [CrossRef]
- Yule, A.M.; Martelon, M.; Faraone, S.V.; Carrellas, N.; Wilens, T.E.; Biederman, J. Examining the Association between Attention de Fi Cit Hyperactivity Disorder and Substance Use Disorders: A Familial Risk Analysis. J. Psychiatr. Res. 2017, 85, 49–55. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Fayyad, J.; Sampson, N.A.; Hwang, I.; Adamowski, T.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Andrade, L.H.; Borges, G.; de Girolamo, G.; Florescu, S. The Descriptive Epidemiology of DSM-IV Adult ADHD in the World Health Organization World Mental Health Surveys. Atten. Defic. Hyperact. 2017, 9, 47–65. [Google Scholar] [CrossRef]
- Kuriyan, A.B.; Pelham, W.E.; Gnagy, E.M.; Sibley, M.H.; Babinski, D.E.; Walther, C.; Cheong, J.; Yu, J.; Kent, K.M. Young Adult Educational and Vocational Outcomes of Children Diagnosed with ADHD. J. Abnorm. Child Psychol. 2013, 41, 27–41. [Google Scholar] [CrossRef]
- Scheres, A.; Solanto, M.V. Do Adhd Symptoms, Executive Function, and Study Strategies Predict Temporal Reward Discounting in College Students with Varying Levels of Adhd Symptoms? A Pilot Study. Brain Sci. 2021, 11, 181. [Google Scholar] [CrossRef]
- van Emmerik-van Oortmerssen, K.; van de Glind, G.; van den Brink, W.; Smit, F.; Crunelle, C.L.; Swets, M.; Schoevers, R.A. Prevalence of Attention-Deficit Hyperactivity Disorder in Substance Use Disorder Patients: A Meta-Analysis and Meta-Regression Analysis. Drug Alcohol Depend. 2012, 122, 11–19. [Google Scholar] [CrossRef]
- Levy, S.; Katusic, S.K.; Colligan, R.C.; Weaver, A.L.; Killian, J.M.; Voigt, R.G.; Barbaresi, W.J. Childhood ADHD and Risk for Substance Dependence in Adulthood: A Longitudinal, Population-Based Study. PLoS ONE 2014, 9, e105640. [Google Scholar] [CrossRef]
- Wilens, T.E.; Martelon, M.; Gagan, J.; Bateman, C.; Ronna, F.; Petty, C.; Biederman, J. Does ADHD Predict Substance-Use of Young Adults with ADHD. JAAC 2011, 50, 543–553. [Google Scholar] [CrossRef]
- Wiklund, J.; Yu, W.; Tucker, R.; Marino, L.D. ADHD, impulsivity and entrepreneurship. J. Bus. Ventur. 2017, 32, 627–656. [Google Scholar] [CrossRef]
- Jensen, M.; Chassin, L.; Gonzales, N.A. Neighborhood Moderation of Sensation Seeking Effects on Adolescent Substance Use Initiation. J. Youth Adolesc. 2017, 1953–1967. [Google Scholar] [CrossRef]
- Zuckerman, M. Behavioral Expressions and Biosocial Bases of Sensation Seeking; Cambridge University Press: New York, NY, USA; Cambridge University Press: Cambridge, UK, 1994. [Google Scholar]
- Vreeker, A.; van der Burg, B.G.; van Laar, M.; Brunt, T.M. Characterizing Users of New Psychoactive Substances Using Psychometric Scales for Risk-Related Behavior. Addict. Behav. 2017, 70, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Hoyle, R.H.; Stephenson, M.T.; Palmgreen, P.; Pugzles, E.; Donohew, R.L. Reliability and Validity of a Brief Measure of Sensation Seeking. Personal. Individ. Differ. 2002, 32, 401–414. [Google Scholar] [CrossRef]
- Malmberg, M.; Overbeek, G.; Monshouwer, K.; Lammers, J.; Vollebergh, W.A.; Engels, R.C. Substance Use Risk Profiles and Associations with Early Substance Use in Adolescence. J. Behav. Med. 2010, 33, 474–485. [Google Scholar] [CrossRef] [PubMed]
- Moggi, F.; Schorno, D.; Soravia, L.M.; Mohler-Kuo, M.; Estévez-Lamorte, N.; Studer, J.; Gmel, G. Screened Attention Deficit/Hyperactivity Disorder as a Predictor of Substance Use Initiation and Escalation in Early Adulthood and the Role of Self-Reported Conduct Disorder and Sensation Seeking: A 5-Year Longitudinal Study with Young Adult Swiss Men. Eur. Addict. Res. 2020, 26, 233–244. [Google Scholar] [CrossRef]
- Kalig-Amir, M.; Berger, I.; Rigbi, A.; Bar-shalita, T. An Exploratory Study of Parent—Child Association in Sensory Modulation Disorder Involving ADHD-Related Symptoms. Pediatr. Res. 2019, 86, 221–226. [Google Scholar] [CrossRef]
- Mazor-Karsenty, T.; Parush, S.; Bonneh, Y.; Shalev, L. Research in Developmental Disabilities Comparing the Executive Attention of Adult Females with ADHD to That of Females with Sensory Modulation Disorder (SMD) under Aversive and Non-Aversive Auditory Conditions. Res. Dev. Disabil. 2015, 37, 17–30. [Google Scholar] [CrossRef]
- Miller, L.J.; Nielsen, D.M.; Schoen, S.A. Attention Deficit Hyperactivity Disorder and Sensory Modulation Disorder: A Comparison of Behavior and Physiology. Res. Dev. Disabil. 2012, 33, 804–818. [Google Scholar] [CrossRef]
- Delgado-Lobete, L.; Pértega-Díaz, S.; Santos-del-Riego, S.; Montes-Montes, R. Sensory Processing Patterns in Developmental Coordination Disorder, Attention Deficit Hyperactivity Disorder and Typical Development. Res. Dev. Disabil. 2020, 100, 103608. [Google Scholar] [CrossRef] [PubMed]
- Interdisciplinary Council on Developmental and Learning Disorders (ICDL). Diagnostic Manual for Infancy and Early Childhood; ICDL: Bethesda, MD, USA, 2005. [Google Scholar]
- Miller, L.J.; Anzalone, M.E.; Lane, S.J.; Cermak, S.A.; Osten, E.T. Concept Evolution in Sensory Integration: A Proposed Nosology for Diagnosis. Am. J. Occup. Ther. 2007, 61, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Zero to Three. Diagnostic Classification: 0-3R: Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood; National Center for Clinical: Washington, DC, USA, 2005. [Google Scholar]
- Kinnealey, M.; Oliver, B.; Wilbarger, P. A Phenomenological Study of Sensory Defensiveness in Adults. Am. J. Occup. Ther. 1995, 49, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Bar-Shalita, T.; Deutsch, L.; Honigman, L.; Weissman-Fogel, I. Ecological Aspects of Pain in Sensory Modulation Disorder. Res. Dev. Disabil. 2015, 45–46, 157–167. [Google Scholar] [CrossRef] [PubMed]
- Weissman-Fogel, I.; Granovsky, Y.; Bar-Shalita, T. Sensory Over-Responsiveness among Healthy Subjects Is Associated with a Pronociceptive State. Pain Pract. 2018, 18, 473–486. [Google Scholar] [CrossRef]
- Ryu, J.; Bar-Shalita, T.; Granovsky, Y.; Weissman-Fogel, I.; Torres, E.B. Personalized Biometrics of Physical Pain Agree with Psychophysics by Participants with Sensory over Responsivity. J. Pers. Med. 2021, 11, 93. [Google Scholar] [CrossRef]
- Yalachkov, Y.; Kaiser, J.; Naumer, M.J. Sensory and Motor Aspects of Addiction. Behav. Brain Res. 2010, 207, 215–222. [Google Scholar] [CrossRef]
- Assayag, N.; Bonneh, Y.; Parush, S.; Mell, H.; Neeman Kaplan, R.; Bar-Shalita, T. Perceived Sensitivity to Pain and Responsiveness to Non-Noxious Sensation in Substance Use Disorder. Pain Med. 2019, 21, 1902–1912. [Google Scholar] [CrossRef]
- Bashapoor, S.; Hosseini-kiasari, S.T.; Daneshvar, S.; Kazemi-Taskooh, Z. Comparing Sensory Information Processing and Alexithymia between People with Substance Dependency and Normal. Addict. Health 2015, 7, 174. [Google Scholar]
- Borges, J.M.; Antonio, J.; Marzo, J.C. Relationship Between Sensory Processing, Relationship between Sensory Processing, Resilience, Attitudes and Drug use in Portuguese Adults. Paidéia (Ribeirão Preto) 2017, 27, 255–262. [Google Scholar] [CrossRef]
- Engel-Yeger, B. Sensory Processing Disorders among Substance Dependents. Cad. Bras. Ter. Ocup. 2014, 22, 111–118. [Google Scholar] [CrossRef]
- Kelly, J.; Meredith, P.J.; Taylor, M.; Morphett, A.; Wilson, H. Substances and Your Senses: The Sensory Patterns of Young People within an Alcohol and Drug Treatment Service. Subst. Abus. 2021, 42, 998–1006. [Google Scholar] [CrossRef] [PubMed]
- Yochman, A.; Alon-Beery, O.; Sribman, A.; Parush, S. Differential Diagnosis of Sensory Modulation Disorder (SMD) and Attention Deficit Hyperactivity Disorder (ADHD): Participation, Sensation, and Attention. Front. Hum. Neurosci. 2013, 7, 862. [Google Scholar] [CrossRef]
- Bar-Shalita, T.; Vatine, J.J.; Parush, S. Sensory Modulation Disorder: A Risk Factor for Participation in Daily Life Activities. Dev. Med. Child Neurol. 2008, 50, 932–937. [Google Scholar] [CrossRef] [PubMed]
- Dunn, W.; Little, L.; Dean, E.; Robertson, S.; Evans, B. The State of the Science on Sensory Factors and Their Impact on Daily Life for Children: A Scoping Review. Particip. Health 2016, 6 (Suppl. 2), 3S–26S. [Google Scholar] [CrossRef] [PubMed]
- Kinnealey, M.; Koenig, K.P.; Smith, S. Relationships between Sensory Modulation and Social Supports and Health-Related Quality of Life. Am. J. Occup. Ther. 2011, 65, 320–327. [Google Scholar] [CrossRef]
- Bunt, G.C.; Muehlbach, B.; Moed, C.O. The Therapeutic Community: An International Perspective. Subst. Abus. 2008, 29, 81–87. [Google Scholar] [CrossRef]
- Verdejo-García, A.; Pérez-García, M. Profile of Executive Deficits in Cocaine and Heroin Polysubstance Users: Common and Differential Effects on Separate Executive Components. Psychopharmacology 2007, 190, 517–530. [Google Scholar] [CrossRef]
- Dickerson, A.E. Securing sample for effective research across research designs. In Research in Occupational Therapy: Methods of Inquiry for Enhancing Practice; Kielhofner, G., Ed.; Davis Company: Philadelphia, PA, USA, 2006; pp. 515–529. [Google Scholar]
- Berger, I.; Goldzweig, G. Objective Measures of Attention-Deficit/Hyperactivity Disorder: A Pilot Study. Isr. Med. Assoc. J. 2010, 12, 531–535. [Google Scholar]
- Berger, I.; Cassuto, H. The Effect of Environmental Distractors Incorporation into a CPT on Sustained Attention and ADHD Diagnosis among Adolescents. J. Neurosci. Methods 2014, 222, 62–68. [Google Scholar] [CrossRef]
- Kessler, R.C.; Adler, L.; Ames, M.; Demler, O.; Faraone, S.; Hiripi, E.V.A.; Howes, M.J.; Jin, R.; Secnik, K.; Spencer, T. The World Health Organization Adult ADHD Self-Report Scale (ASRS): A Short Screening Scale for Use in the General Population. Psychol. Med. 2005, 35, 245–256. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Adler, L.A.; Gruber, M.J.; Sarawate, C.A.; Spencer, T.; Brunt, D.L.V.A.N. Validity of the World Health Organization Adult ADHD Self-Report Scale (ASRS) Screener in a Representative Sample of Health Plan Members. Int. J. Methods Psychiatr. Res. 2007, 16, 52–65. [Google Scholar] [CrossRef]
- Van De Glind, G.; Van Emmerik-van Oortmerssen, K.; Carpentier, P.J.; Levin, F.R.; Koeter, M.W.; Barta, C.; Kaye, S.; Skutle, A.; Franck, J.; Konstenius, M. The International ADHD in Substance Use Disorders Prevalence (IASP) Study: Background, Methods and Study Population. Int. J. Methods Psychiatr. Res. 2013, 22, 232–244. [Google Scholar] [CrossRef] [PubMed]
- Ustun, B.; Adler, L.A.; Rudin, C.; Faraone, S.V.; Spencer, T.J.; Berglund, P.; Gruber, M.J.; Kessler, R.C. The World Health Organization Adult Attention-Deficit/Hyperactivity Disorder Self-Report Screening Scale for DSM-5. JAMA Psychiatry 2017, 74, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Adler, L.A.; Spencer, T.; Stephen, F.; Kessler, R.C.; Howes, M.J.; Biederman, J.; Secnik, K. Validity of Pilot Adult ADHD Self-Report Scale (ASRS) to Rate Adult ADHD Symptoms. Ann. Clin. Psychiatry 2006, 18, 145–148. [Google Scholar] [CrossRef]
- Matza, L.S.; Van Brunt, D.L.; Cates, C.; Murray, L.T. Test—Retest Reliability of Two Patient-Report Measures for Use in Adults With ADHD. J. Atten. Disord. 2011, 15, 557–563. [Google Scholar] [CrossRef]
- Bar-Shalita, T.; Seltzer, Z.; Vatine, J.; Yochman, A.; Parush, S. Development and Psychometric Properties of the Sensory Responsiveness Questionnaire (SRQ). Disabil. Rehabil. 2009, 31, 189–201. [Google Scholar] [CrossRef]
- Shlosberg, D.; Amit, B.H.; Zalsman, G.; Krivoy, A.; Mell, H.; Lev-Ran, S.; Shoval, G. Cognitive Impairments in Abstinent Male Residents of a Therapeutic Community for Substance-Use Disorders: A Five-Year Retrospective Study. Subst. Use Misuse 2019, 54, 538–548. [Google Scholar] [CrossRef]
- Van De Glind, G.; Brynte, C.; Skutle, A.; Kaye, S.; Konstenius, M.; Levin, F.; Mathys, F.; Demetrovics, Z.; Moggi, F.; Ramos-Quiroga, J.A.; et al. The International Collaboration on ADHD and Substance Abuse (ICASA): Mission, Results, and Future Activities. Eur. Addict. Res. 2020, 26, 173–178. [Google Scholar] [CrossRef]
- Hagen, E.; Erga, A.H.; Nesvåg, S.M.; Mckay, J.R.; Lundervold, A.J. One-Year Abstinence Improves ADHD Symptoms among Patients with Polysubstance Use Disorder. Addict. Behav. Rep. 2017, 6, 96–101. [Google Scholar] [CrossRef]
- Farhoodi, F.; Rostami, R.; Abdolmanafi, A.; Amiri, M. A Study and Comparison of the Symptoms of Attention Deficit Hyperactivity Disorder (ADHD) among Patients with Substance Use Disorder and Normal People. Procedia Soc. Behav. Sci. 2010, 5, 892–895. [Google Scholar] [CrossRef][Green Version]
- Slobodin, O.; Blankers, M.; Kapitány-Fövény, M.; Kaye, S.; Berger, I.; Johnson, B.; Demetrovics, Z.; Van Den Brink, W.; Van De Glind, G. Differential Diagnosis in Patients with Substance Use Disorder and/or Attention-Deficit/Hyperactivity Disorder Using Continuous Performance Test. Eur. Addict. Res. 2020, 26, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Berger, I.; Slobodin, O.; Cassuto, H. Usefulness and Validity of Continuous Performance Tests in the Diagnosis of Attention-De Fi Cit Hyperactivity Disorder Children. Arch. Clin. Neuropsychol. 2017, 32, 81–93. [Google Scholar] [CrossRef]
- Loree, A.M.; Lundahl, L.H.; Ledgerwood, D.M. Impulsivity as a Predictor of Treatment Outcome in Substance Use Disorders: Review and Synthesis. Drug Alcohol Rev. 2015, 34, 119–134. [Google Scholar] [CrossRef] [PubMed]
- Stevens, L.; Verdejo-garcía, A.; Goudriaan, A.E.; Roeyers, H.; Dom, G.; Vanderplasschen, W. Impulsivity as a Vulnerability Factor for Poor Addiction Treatment Outcomes: A Review of Neurocognitive Fi Ndings among Individuals with Substance Use Disorders. J. Subst. Abuse Treat. 2014, 47, 58–72. [Google Scholar] [CrossRef] [PubMed]
- Verdejo-Garcı, A.; Lawrence, A.J.; Clark, L. Impulsivity as a Vulnerability Marker for Substance-Use Disorders: Review of Findings from High-Risk Research, Problem Gamblers and Genetic Association Studies. Neurosci. Biobehav. Rev. 2008, 32, 777–810. [Google Scholar] [CrossRef] [PubMed]
- Young, J.T.; Bellgrove, M.A.; Arunogiri, S. Assessment of Attention-Deficit Hyperactivity Disorder in People with Substance Use Disorder: Another Case of What Gets Measured Gets Done. Aust. N. Z. J. Psychiatry 2021, 55, 744–746. [Google Scholar] [CrossRef]
- Kaynak, Ö.; Meyers, K.; Caldeira, K.M.; Vincent, K.B.; Winters, K.C.; Arria, A.M. Addictive Behaviors Relationships among Parental Monitoring and Sensation Seeking on the Development of Substance Use Disorder among College Students. Addict. Behav. 2013, 38, 1457–1463. [Google Scholar] [CrossRef][Green Version]
- Bardo, M.T.; Donohew, R.L.; Harrington, N.G. Psychobiiology of Novelty Seeking and Drug Seeking Behavior. Behav. Brain Res. 1996, 77, 23–43. [Google Scholar] [CrossRef]
- Granovsky, Y.; Weissman-Fogel, I.; Bar-Shalita, T. Resting-State EEG in Individuals with Sensory over-Responsivity: An Exploratory Study. Am. J. Occup. Ther. 2018, 73. [Google Scholar] [CrossRef]
- Chandrasekaran, C. ScienceDirect Computational Principles and Models of Multisensory Integration. Curr. Opin. Neurobiol. 2017, 43, 25–34. [Google Scholar] [CrossRef]
- Warner, E.; Koomar, J.; Lary, B.; Cook, A. Can the Body Change the Score? Application of Sensory Modulation Principles in the Treatment of Traumatized Adolescents in Residential Settings. J. Fam. Violence 2013, 28, 729–738. [Google Scholar] [CrossRef]
- McKernan, L.C.; Nash, M.R.; Gottdiener, W.H.; Anderson, S.E.; Lambert, W.E.; Carr, E.R. Further Evidence of Self-Medication: Personality Factors Influencing Drug Choice in Substance Use Disorders. Psychiatry 2015, 43, 243–275. [Google Scholar] [CrossRef] [PubMed]
- Alexander, A.C.; Ward, K.D. Understanding Postdisaster Substance Use and Psychological Distress Using Concepts from the Self-Medication Hypothesis and Social Cognitive Theory. J. Psychoact. Drugs 2018, 50, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Khantzian, E.J. Understanding Addictive Vulnerability: An Evolving Psychodynamic Perspective. Neuropsychoanalysis 2003, 5, 5–21. [Google Scholar] [CrossRef]
- Bar-shalita, T.; Granovsky, Y.; Parush, S.; Weissman-fogel, I. Sensory Modulation Disorder (SMD) and Pain: A New Perspective. Front. Integr. Neurosci. 2019, 13, 27. [Google Scholar] [CrossRef]
- Meredith, P.J.; Andrews, N.E.; Thackeray, J.; Bowen, S.; Poll, C.; Strong, J. Can Sensory- and Attachment-Informed Approaches Modify the Perception of Pain? An Experimental Study. Pain Res. Manag. 2021, 2021, 5527261. [Google Scholar] [CrossRef]
- Bart, O.; Bar-Shalita, T.; Mansour, H.; Dar, R. Relationships among Sensory Responsiveness, Anxiety, and Ritual Behaviors in Children with and without Atypical Sensory Responsiveness. Phys. Occup. Ther. Pediatr. 2017, 37, 322–331. [Google Scholar] [CrossRef]
- Engel-Yeger, B.; Dunn, W. The Relationship between Sensory Processing Difficulties and Anxiety Level of Healthy Adults. Br. J. Occup. Ther. 2011, 74, 210–216. [Google Scholar] [CrossRef]
- Bar-Shalita, T.; Cermak, S.A. Atypical Sensory Modulation and Psychological Distress in the General Population. Am. J. Occup. Ther. 2016, 70, 7004250010p1–7004250010p9. [Google Scholar] [CrossRef]
- Engel-Yeger, B.; Dunn, W. Exploring the Relationship between Affect and Sensory Processing Patterns in Adults. Br. J. Occup. Ther. 2011, 74, 456–464. [Google Scholar] [CrossRef]
- Bar-shalita, T.; Livshitz, A.; Levin-meltz, Y.; Rand, D.; Deutsch, L.; Vatine, J. Sensory Modulation Dysfunction Is Associated with Complex Regional Pain Syndrome. PLoS ONE 2018, 13, e0201354. [Google Scholar] [CrossRef] [PubMed]
- Granovsky, Y.; Shor, M.; Shifrin, A.; Sprecher, E.; Yarnitsky, D.; Bar-Shalita, T. Assessment of Responsiveness to Everyday Non-Noxious Stimuli in Pain-Free Migraineurs with versus without Aura. J. Pain 2018, 8, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Vergara-Moragues, E.; Verdejo-García, A.; Lozano, O.M.; Santiago-Ramajo, S.; González-Saiz, F.; Betanzos Espinosa, P.; Pérez García, M. Association between Executive Function and Outcome Measure of Treatment in Therapeutic Community among Cocaine Dependent Individuals. J. Subst. Abuse Treat. 2017, 78, 48–55. [Google Scholar] [CrossRef]

| Charactristics | Study Group n = 58 | Comparison Group n = 62 |
|---|---|---|
| Gender | ||
| Male | 91.4% (n = 53) | 87.1% (n = 54) |
| Female | 8.6% (n = 5) | 12.9% (n = 8) |
| Age (years), Mean (SD) | 27.4 (9.94) | 26.0 (5.83) |
| Years of education, Mean (SD) | 11.4 (1.30) | 13.9 (2.27) |
| Substance use distribution * | ||
| Cannabis | 22.4% (n = 13) | |
| Opioids | 22.4% (n = 13) | |
| Stimulants | 8.6% (n = 5) | |
| Synthetic cannabinoid | 31% (n = 18) | |
| Alcohol | 15.5% (n = 9) | |
| Initial age for drug use, Mean (SD) | 16.4 (3.78) |
| Study Variables | Study Group (n = 58) | Comparison Group (n = 62) |
|---|---|---|
| SMD | 53.6 (30) | 14.5 (9) |
| SMD-SUR | 14.3 (8) | 6.5 (4) |
| SMD-SOR | 48.2 (27) | 8/1 (5) |
| BSSS-Total score | 3.5 (0.73) | 2.8 (0.75) |
| Experience-Seeking | 3.6 (1.00) | 3.4 (1.03) |
| Boredom Susceptibility | 3.1 (0.74) | 2.5 (0.90) |
| Thrill- and Adventure-Seeking | 3.6 (1.19) | 2.7 (0.98) |
| MOXO-CPT * | ||
| Disinhibition | 3.7(1.09) | 2.5 (1.09) |
| Attention | 265.1 (9.55) | 269.6 (2.61) |
| Timing | 232.9 (25.27) | 233.4 (24.31) |
| Hyperactivity | 9.4 (11.96) | 3.2 (2.79) |
| Impulsivity | 17.7 (13.53) | 9.7 (6.95) |
| Variable | OR | Lower 95% CI | Upper 95% CI | Pr > ChiSq |
|---|---|---|---|---|
| SMD-SOR (Yes/No) | 26.889 | 5.965 | 121.216 | <0.0001 |
| MOXO-CPT Impulsivity Index | 1.136 | 1.056 | 1.222 | 0.0006 |
| BSSS-Total score | 2.877 | 2.877 | 6.455 | 0.0103 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assayag, N.; Berger, I.; Parush, S.; Mell, H.; Bar-Shalita, T. Attention-Deficit/Hyperactivity Disorder Symptoms, Sensation-Seeking, and Sensory Modulation Dysfunction in Substance Use Disorder: A Cross Sectional Two-Group Comparative Study. Int. J. Environ. Res. Public Health 2022, 19, 2541. https://doi.org/10.3390/ijerph19052541
Assayag N, Berger I, Parush S, Mell H, Bar-Shalita T. Attention-Deficit/Hyperactivity Disorder Symptoms, Sensation-Seeking, and Sensory Modulation Dysfunction in Substance Use Disorder: A Cross Sectional Two-Group Comparative Study. International Journal of Environmental Research and Public Health. 2022; 19(5):2541. https://doi.org/10.3390/ijerph19052541
Chicago/Turabian StyleAssayag, Naama, Itai Berger, Shula Parush, Haim Mell, and Tami Bar-Shalita. 2022. "Attention-Deficit/Hyperactivity Disorder Symptoms, Sensation-Seeking, and Sensory Modulation Dysfunction in Substance Use Disorder: A Cross Sectional Two-Group Comparative Study" International Journal of Environmental Research and Public Health 19, no. 5: 2541. https://doi.org/10.3390/ijerph19052541
APA StyleAssayag, N., Berger, I., Parush, S., Mell, H., & Bar-Shalita, T. (2022). Attention-Deficit/Hyperactivity Disorder Symptoms, Sensation-Seeking, and Sensory Modulation Dysfunction in Substance Use Disorder: A Cross Sectional Two-Group Comparative Study. International Journal of Environmental Research and Public Health, 19(5), 2541. https://doi.org/10.3390/ijerph19052541






