How to Educate the Public about Dental Trauma—A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Methodological Framework
2.2. Framing Research Questions
2.3. Inclusion and Exclusion Criteria
2.4. Information Sources and Search Strategy
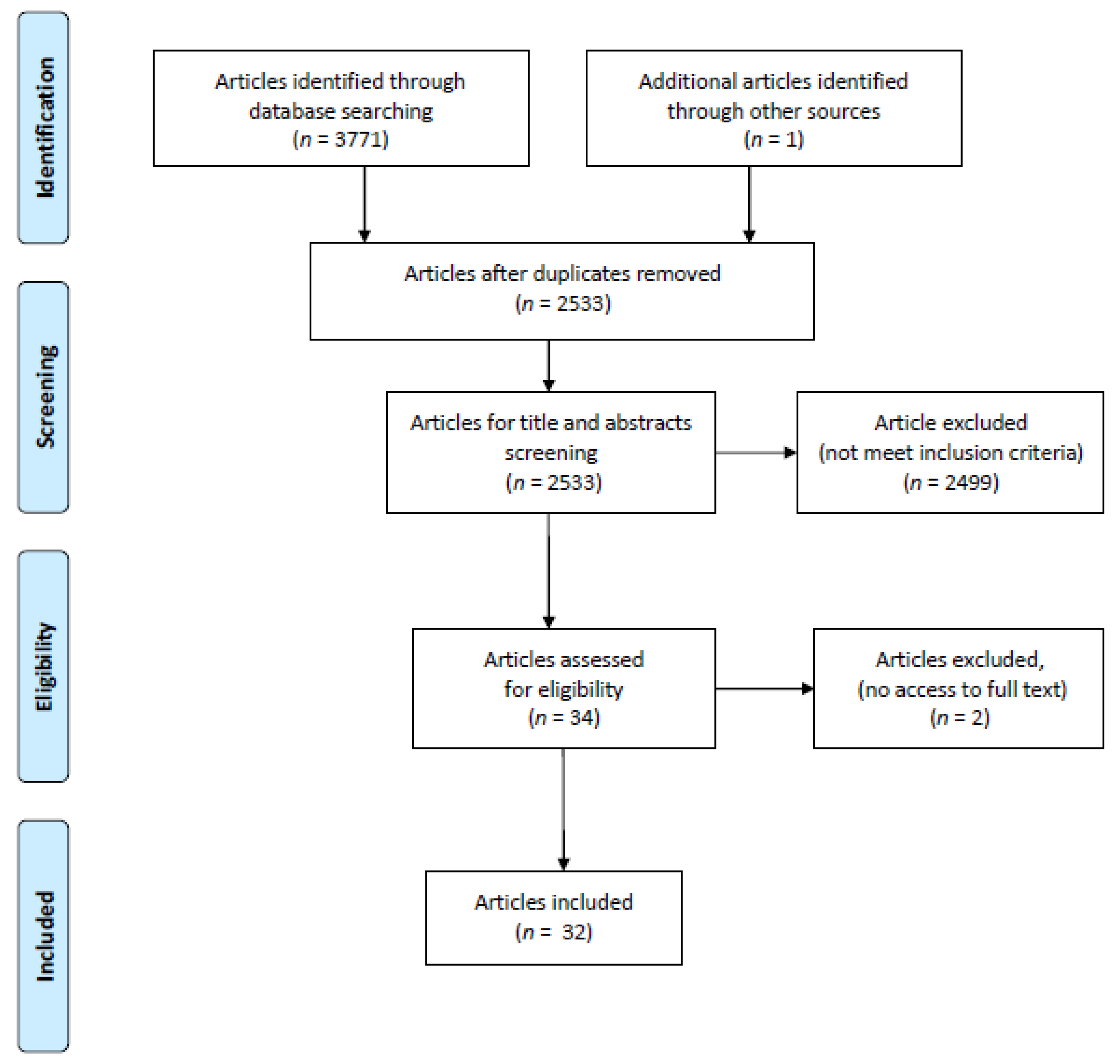
2.5. Study Selection
2.6. Data Extraction
3. Results
3.1. Geographical Distribution
3.2. Subjects
3.3. Intervention
3.4. Knowledge Gain Assessment
3.5. Term of Observation
3.6. Key Findings
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andreasen, J.O.; Lauridsen, E.; Daugaard-Jensen, J. Dental traumatology: An orphan in pediatric dentistry? Pediatr. Dent. 2009, 31, 153–163. [Google Scholar] [PubMed]
- Antunes, L.A.A.; Lemos, H.M.; Milani, A.J.; Guimarães, L.S.; Küchler, K.C.; Antunes, L.S. Does traumatic dental injury impact oral health-related to quality of life of children and adolescents? Systematic review and meta-analysis. Int. J. Dent. Hyg. 2020, 18, 142–162. [Google Scholar] [CrossRef] [PubMed]
- Lopez, D.; Waidyatillake, N.; Zaror, C.; Mariño, R. Impact of uncomplicated traumatic dental injuries on the quality of life of children and adolescents: A systematic review and meta-analysis. BMC Oral Health 2019, 19, 224. [Google Scholar] [CrossRef] [PubMed]
- Glendor, U. Has the education of professional caregivers and lay people in dental trauma care failed? Dent. Traumatol. 2005, 29, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, F.A.; Hill, F.J.; Mackie, I.C. Investigation of lay knowledge of the management of avulsed permanent incisors. Endod. Dent. Traumatol. 1997, 13, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Levin, L.; Zadik, Y. Education on and prevention of dental trauma: It’s time to act! Dent. Traumatol. 2012, 28, 49–54. [Google Scholar] [CrossRef]
- Yeng, T.; O’Sullivan, A.J.; Shulruf, B. Medical doctors’ knowledge of dental trauma management: A review. Dent. Traumatol. 2020, 36, 100. [Google Scholar] [CrossRef]
- Traebert, J.; Traiano, M.L.; Armênio, R.; Barbieri, D.B.; De Lacerda, J.T.; Marcenes, W. Knowledge of lay people and dentists in emergency management of dental trauma. Dent. Traumatol. 2009, 25, 277–283. [Google Scholar] [CrossRef]
- Tewari, N.; Johnson, R.M.; Mathur, V.P.; Rahul, M.; Goel, S.; Ritwik, P.; Bansal, K.; Atif, M. Global status of knowledge for prevention and emergency management of traumatic dental injuries in sports persons and coaches: A systematic review. Dent. Traumatol. 2021, 37, 196–207. [Google Scholar] [CrossRef]
- Tewari, N.; Sultan, F.; Mathur, V.P.; Rahul, M.; Goel, S.; Bansal, K.; Chawla, A.; Haldar, P.; Pandey, R.M. Global status of knowledge for prevention and emergency management of traumatic dental injuries in dental professionals: A systematic review and meta-analysis. Dent. Traumatol. 2021, 37, 161–176. [Google Scholar]
- Tewari, N.; Goel, S.; Rahul, M.; Mathur, V.P.; Ritwik, P.; Haldar, P.; Priya, H.; Pandey, R.M. Global status of knowledge for prevention and emergency management of traumatic dental injuries among school teachers: A systematic review and meta-analysis. Dent. Traumatol. 2020, 36, 568–583. [Google Scholar] [CrossRef] [PubMed]
- Wilson, E.A.; Makoul, G.; Bojarski, E.A.; Bailey, S.C.; Waite, K.R.; Rapp, D.N.; Baker, D.W.; Wolf, M.S. Comparative analysis of print and multimedia health materials: A review of the literature. Patient Educ. Couns. 2012, 89, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Vallance, J.K.; Taylor, L.M.; Lavallee, C. Suitability and readability assessment of educational print resources related to physical activity: Implications and recommendations for practice. Patient Educ. Couns. 2008, 72, 342–349. [Google Scholar] [CrossRef] [PubMed]
- Al-Sane, M.; Bourisly, N.; Almulla, T.; Andersson, L. Laypeoples’ preferred sources of health information on the emergency management of tooth avulsion. Dent. Traumatol. 2011, 27, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Kahabuka, F.K.; van’t Hof, M.; Willemsen, W.; Burgersdijk, R. Influence of seminar and mailed guidelines on knowledge of school teachers regarding emergency treatment for dental injuries. East Afr. Med. J. 2003, 80, 105–109. [Google Scholar]
- McIntyre, J.D.; Lee, J.Y.; Trope, M.; Vann, W.F., Jr. Effectiveness of dental trauma education for elementary school staff. Dent. Traumatol. 2008, 24, 146–150. [Google Scholar] [CrossRef]
- Holan, G.; Cohenca, N.; Brin, I.; Sgan-Cohen, H. An oral health promotion program for the prevention of complications following avulsion: The effect on knowledge of physical education teachers. Dent. Traumatol. 2006, 22, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Al-Asfour, A.; Andersson, L.; Al-Jame, Q. School teachers’ knowledge of tooth avulsion and dental first aid before and after receiving information about avulsed teeth and replantation. Dent. Traumatol. 2008, 24, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Al-Asfour, A.; Andersson, L. The effect of a leaflet given to parents for first aid measures after tooth avulsion. Dent. Traumatol. 2008, 24, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Lieger, O.; Graf, C.; El-Maaytah, M.; von Arx, T. Impact of educational posters on the lay knowledge of school teachers regarding emergency management of dental injuries. Dent. Traumatol. 2009, 25, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Frujeri, M.L.V.; Costa, E.D., Jr. Effect of a single dental health education on the management of permanent avulsed teeth by different groups of professionals. Dent. Traumatol. 2009, 25, 262–271. [Google Scholar] [CrossRef]
- Levin, L.; Jeffet, U.; Zadik, Y. The effect of short dental trauma lecture on knowledge of high-risk population: An intervention study of 336 young adults. Dent. Traumatol. 2010, 26, 86–89. [Google Scholar] [CrossRef]
- Karande, N.; Shah, P.; Bhatia, M.; Lakade, L.; Bijle, M.N.; Arora, N.; Bhalla, M. Assessment of awareness amongst school teachers regarding prevention and emergency management of dentoalveolar traumatic injuries in school children in Pune City, before and 3 months after dental educational program. J. Contemp. Dent. Pract. 2012, 13, 873–877. [Google Scholar] [CrossRef]
- Arikan, V.; Sönmez, H. Knowledge level of primary school teachers regarding traumatic dental injuries and their emergency management before and after receiving an informative leaflet. Dent. Traumatol. 2012, 28, 101–107. [Google Scholar] [CrossRef]
- Skapetis, T.; Gerzina, T.; Hu, W. Managing dental emergencies: A descriptive study of the effects of a multimodal educational intervention for primary care providers at six months. BMC Med. Educ. 2012, 30, 103. [Google Scholar] [CrossRef]
- Baginska, J.; Wilczynska-Borawska, M. Knowledge of nurses working at schools in Bialystok, Poland, of tooth avulsion and its management. Dent. Traumatol. 2012, 28, 314–319. [Google Scholar] [CrossRef]
- Emerich, K.; Wlodarczyk, P.; Ziolkowski, A. Education of Sport University students regarding first-aid procedures after dental trauma. Eur. J. Paediatr Dent. 2013, 14, 37–41. [Google Scholar] [PubMed]
- Soubra, B.N.; Debs, N.N. Impact of audiovisual method in educating children facing dental avulsion. Dent. Traumatol. 2014, 30, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Ghaderi, F.; Adl, A.; Ranjbar, Z. Effect of a leaflet given to parents on knowledge of tooth avulsion. Eur. J. Paediatr. Dent. 2012, 14, 13–16. [Google Scholar]
- Nuvvula, S.; Shilpa, G.; Nirmala, S.; Yamini, V.; Pujita, C. Informative promotional outcome on school teachers′ knowledge about emergency management of dental trauma. J. Conserv. Dent. 2013, 16, 21–27. [Google Scholar] [CrossRef]
- Young, C.; Wong, K.Y.; Cheung, L.K. Effectiveness of educational poster on knowledge of emergency management of dental trauma—Part 1. Cluster randomised controlled trial for primary and secondary school teachers. PLoS ONE 2013, 8, e74833. [Google Scholar] [CrossRef]
- Young, C.; Wong, K.Y.; Cheung, L.K. Effectiveness of educational poster on knowledge of emergency management of dental trauma—Part 2: Cluster randomised controlled trial for secondary school students. PLoS ONE 2014, 9, e101972. [Google Scholar] [CrossRef]
- Raoof, M.; Shokouhinejad, N.; Izadi, A.; Nourzadeh, M.; Afkham, A.; Forghani, F.-R.; Tavallaie, M.; Mohammadalizadeh, S. Long-term effect of an educational intervention regarding dental trauma first aid: A phase II study. Dent. Traumatol. 2014, 30, 296–301. [Google Scholar] [CrossRef]
- Ghadimi, S.; Seraj, B.; Keshavarz, H.; Shamshiri, A.R.; Abiri, R. The effect of using an educational poster on elementary school health teachers’ knowledge of emergency management of traumatic dental injuries. J. Dent. Tehran 2014, 11, 620–628. [Google Scholar]
- Grewal, N.; Shangdiar, G.D.; Samita, G. Efficacy of a comprehensive dental education program regarding management of avulsed permanent teeth as a valid indicator of increased success rate of treatment of avulsion in a North Indian population. Contemp. Clin. Dent. 2015, 6, 477–482. [Google Scholar] [CrossRef]
- Perazzo, M.F.; Cruz da Silva, B.R.; Neves, É.T.B.; Firmino, R.T.; Ribeiro, G.L.; Granville-Garcia, A.F. Effect of dental health education on the management of avulsed teeth by firefighters. J. Public Health 2015, 23, 49–55. [Google Scholar] [CrossRef]
- Iskander, M.; Lou, J.; Wells, M.; Scarbecz, M. A poster and a mobile healthcare application as information tools for dental trauma management. Dent. Traumatol. 2016, 32, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Cruz-da-Silva, B.R.; Perazzo, M.F.; Neves, É.T.B.; Firmino, R.T.; Granville-Garcia, A.F. Effect of an educational programme on the knowledge level among an emergency service medical team regarding tooth avulsion. Oral Health Prev. Dent. 2016, 14, 259–266. [Google Scholar] [PubMed]
- Senaikarasi, R.M.; Taranath, M.; Manchanda, K. Assessment of knowledge and attitude before and after a health education program in East Madurai primary school teachers with regard to emergency management of avulsed teeth. J. Indian Soc. Pedod. Prev. Dent. 2017, 35, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Al-Musawi, A.; Al-Sane, M.; Andersson, L. Smartphone App as an aid in the emergency management of avulsed teeth. Dent. Traumatol. 2017, 33, 13–18. [Google Scholar] [CrossRef]
- Yordi, C.W.; Badr, S.B.Y.; Shokry, M. Effectiveness of dental traumatic injuries’ educational message on school teachers in Beirut-cluster randomized field trial. Egypt. Dent. J. 2017, 63, 269–285. [Google Scholar] [CrossRef][Green Version]
- Al Sari, S.; Kowash, M.; Hussein, I.; Al-Halabi, M. An educational initiative for Dubai School nurses and physical education teachers on the management of traumatic dental injuries. J. Sch. Nurs. 2019, 35, 359–366. [Google Scholar] [CrossRef]
- Nagata, J.Y.; Góis, V.L.D.A.; Munchow, E.A.; Albuquerque, M.T.P. Dental trauma education intervention as a positive influence among undergraduate students. Eur. J. Dent. 2018, 21, 502–507. [Google Scholar] [CrossRef]
- Jain, M.; Bansal, A.; Tyagi, P.; Jain, A.; Tiwari, U.; Nashine, N. Comparison and evaluation of attitude and knowledge towards the management of dental injury in school teachers before and after oral health education. Int. J. Clin. Pediatr. Dent. 2018, 11, 425–429. [Google Scholar] [CrossRef]
- Niviethitha, S.; Bhawarlal, C.; Ramkumar, H.; Dhakshanamoorthy, S.; Shanmugam, H. Effectiveness of an audio-visual aid on the knowledge of school teachers regarding the emergency management of dental injuries. Dent. Traumatol. 2018, 34, 290–296. [Google Scholar] [CrossRef]
- Razeghi, S.; Mohebbi, S.Z.; Gholami, M.; Mashayekhi, M.; Maraghehpour, B.; Rahnama, E. Effect of two educational interventions on primary school teachers’ knowledge and self-reported practice regarding emergency management of traumatic dental injuries. BMC Oral Health 2019, 19, 130. [Google Scholar] [CrossRef]
- Custers, E.J.F.M. Long-term retention of basic science knowledge: A review study. Adv. Health Sci. Educ. Theory Pract. 2010, 15, 109–128. [Google Scholar] [CrossRef]
- Health Development Agency. The Effectiveness of Public Health Campaigns. HDA Briefing. 2004. Available online: http://www.prevencionbasadaenlaevidencia.net/uploads/PDF/RP_campaignsEffectivenes.pdf (accessed on 20 January 2020).
- Bujnowska-Fedak, M.M. Trends in the use of the Internet for health purposes in Poland. BMC Public Health 2015, 15, 194. [Google Scholar] [CrossRef] [PubMed]
- Bardaweel, S.A.; Dashash, M. E-learning or educational leaflet: Does it make a difference in oral health promotion? A clustered randomized trial. BMC Oral Health 2018, 18, 81. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, W.; Amuta, O.A.; Jeon, K.C. Health information seeking in the digital age: An analysis of health information seeking behaviour among US adults. Cogent Soc. Sci. 2017, 3, 1302785. [Google Scholar] [CrossRef]
- Hutchison, C.M.D.; Cave, V.; Walshaw, E.G.; Burns, B.; Park, C. YouTube™ as a source for patient education about the management of dental avulsion injuries. Dent. Traumatol. 2020, 36, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Abu-Ghazaleh, S.; Hassona, Y.; Hattar, S. Dental trauma in social media-Analysis of Facebook content and public engagement. Dent. Traumatol. 2018, 34, 394–400. [Google Scholar] [CrossRef]
- Traebert, J.; Peres, M.A.; Blank, V.; Böell, R.D.S.; Pietruza, J.A. Prevalence of traumatic dental injury and associated factors among 12-year-old school children in Florianópolis, Brazil. Dent. Traumatol. 2013, 19, 15–18. [Google Scholar] [CrossRef]
- Pham, T.M.; Rajić, A.; Greig, J.D.; Sargeant, J.M.; Papadopoulos, A.; McEwen, S.A. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res. Synth. Methods 2014, 5, 371–385. [Google Scholar] [CrossRef]
- Sedlaceck, P.; Poi, W.R.; Amaral, M.F.; Castilho, L.R.; Panzarini, S.R.; Saito, C.T.M.H.; Brandini, D.A. Educational impact of notebook covers on the knowledge of sixth-grade primary pupils about tooth avulsion and replantation: A randomized trial. Health Educ. Behav. 2021. [Google Scholar] [CrossRef]
- Lima, J.; Caldarelli, P.G.; Rocha, J.S.; Fagundes Tomazinho, F.S.; Fariniuk, L.F.; Baratto-Filho, F.; Leão Gabardo, M.C. Educational approaches for assessing knowledge about and actions of educators in response to dental avulsion. J. Indian Soc. Pedod. Prev. Dent. 2021, 39, 138–146. [Google Scholar]
| Authors | Year | Country | Modality | Sample | Term of Observation |
|---|---|---|---|---|---|
| Kahabuka et al. [19] | 2003 | Tanzania | a seminar vs. a guidelines sent by email | teachers | 6 months |
| McIntyre et al. [20] | 2006 | USA | a pamphlet vs. a pamphlet and a 10-min lecture | public elementary school teachers, teacher’s assistants, nurses | 3 months |
| Holan et al. [21] | 2006 | Israel | a seminar | physical education teachers | 10 months |
| Al-Asfor et al. [22] | 2008 | Kuwait | a lecture | teachers | after intervention |
| Al-Asfor, Andersson [23] | 2008 | Kuwait | a leaflet | parents | 1 week |
| Lieger et al. [24] | 2009 | Switzerland | a poster | teachers | 5 years |
| Frujeri, Costa [25] | 2009 | Brazil | a lecture | different professionals | 2 months |
| Levin et al. [26] | 2010 | Israel | a lecture | 18-year-old men military recruits | after intervention |
| Karande et al. [27] | 2012 | India | a lecture | teachers | 3 months |
| Arikan, Sȍnmez [28] | 2012 | Turkey | a leaflet | teachers | 1 month |
| Skapetis et al. [29] | 2012 | Australia | an interactive and multimodal workshop | physicians, nurse practitioners, medical students | 6 months |
| Baginska, Wilczynska -Borawska [30] | 2012 | Poalnd | a lecture | school nurses | 2 years |
| Emerich et al. [31] | 2013 | Poland | a lecture + an additional task | physical education students | 1 year |
| Soubra, Debs [32] | 2013 | Lebanon | audio and visual methods | pupils (8–11 years old) | 3 months, after intervention |
| Ghaderi et al. [33] | 2013 | Iran | a leaflet | parents | 1 week |
| Pujita et al. [34] | 2013 | India | a lecture | teachers | 3 months |
| Young et al. [35] | 2013 | Hong Kong | a poster | teachers | up to 1 week |
| Young et al. [36] | 2013 | Hong Kong | a poster | pupils (11–20 years) | up to 1 week |
| Raoof et al. [37] | 2014 | Iran | a multimodal educational intervention (lecture + poster) | health teachers | 3 years |
| Ghadimi et al. [38] | 2014 | Iran | a poster | school health teachers | 1 month |
| Grewal et al. [39] | 2015 | India | a multimodal educational intervention (flip cards + a poster + interactive sessions and a lecture) | school teachers/sport coaches, pupils (7–12 years old), parents | 6 months |
| Perazzo et al. [40] | 2015 | Brazil | a lecture | firefighters | 6 months |
| Iskander et al. [41] | 2016 | USA | a mobile application vs. a poster | parents | after intervention |
| Cruz-da-Silva et al. [42] | 2016 | Brazil | a multimodal educational intervention (a lecture + a pamphlet) | non-dental health professional involved in the emergency care | 6 months |
| Taranath et al. [43] | 2017 | India | a Power Point presentation | school teachers | 1 month |
| Al-Musawi et al. [44] | 2017 | Kuwait | a lecture vs. a lecture + access to the Dental Trauma App vs. access to the Dental Trauma App | female teacher | after intervention |
| Yordi et al. [45] | 2017 | Labanon | a multimodal educational intervention (a PowerPoint presentation + a brochure + a poster) | teachers | 6 months |
| Al Sari et al. [46] | 2018 | United Arab Emirates | a multimodal educational intervention (a workshop + a poster) | school nurses and physical education teachers | 3 months |
| Nagata et al. [47] | 2018 | Brazil | a lecture | health courses’ students | after intervention |
| Nashine et al. [48] | 2018 | India | audio vs. audio-visual aids (not specified) | teachers | after intervention |
| Niviethitha et al. [49] | 2018 | India | an interactive educational DVD video | teachers | after intervention |
| Razeghi et al. [50] | 2019 | Iran | a leaflet vs. a lecture | teachers | 6 months |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nowosielska, M.; Bagińska, J.; Kobus, A.; Kierklo, A. How to Educate the Public about Dental Trauma—A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 2479. https://doi.org/10.3390/ijerph19042479
Nowosielska M, Bagińska J, Kobus A, Kierklo A. How to Educate the Public about Dental Trauma—A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(4):2479. https://doi.org/10.3390/ijerph19042479
Chicago/Turabian StyleNowosielska, Magdalena, Joanna Bagińska, Agnieszka Kobus, and Anna Kierklo. 2022. "How to Educate the Public about Dental Trauma—A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 4: 2479. https://doi.org/10.3390/ijerph19042479
APA StyleNowosielska, M., Bagińska, J., Kobus, A., & Kierklo, A. (2022). How to Educate the Public about Dental Trauma—A Scoping Review. International Journal of Environmental Research and Public Health, 19(4), 2479. https://doi.org/10.3390/ijerph19042479






