Risk Assessment of Indoor Air Quality and Its Association with Subjective Symptoms among Office Workers in Korea
Abstract
1. Introduction
2. Materials and Methods
2.1. Target Office Buildings
2.2. Indoor and Outdoor Air Quality Measurements
2.3. Questionnaire and Checklist
2.4. Health Risk Assessment
2.5. Statistical Analysis
3. Results
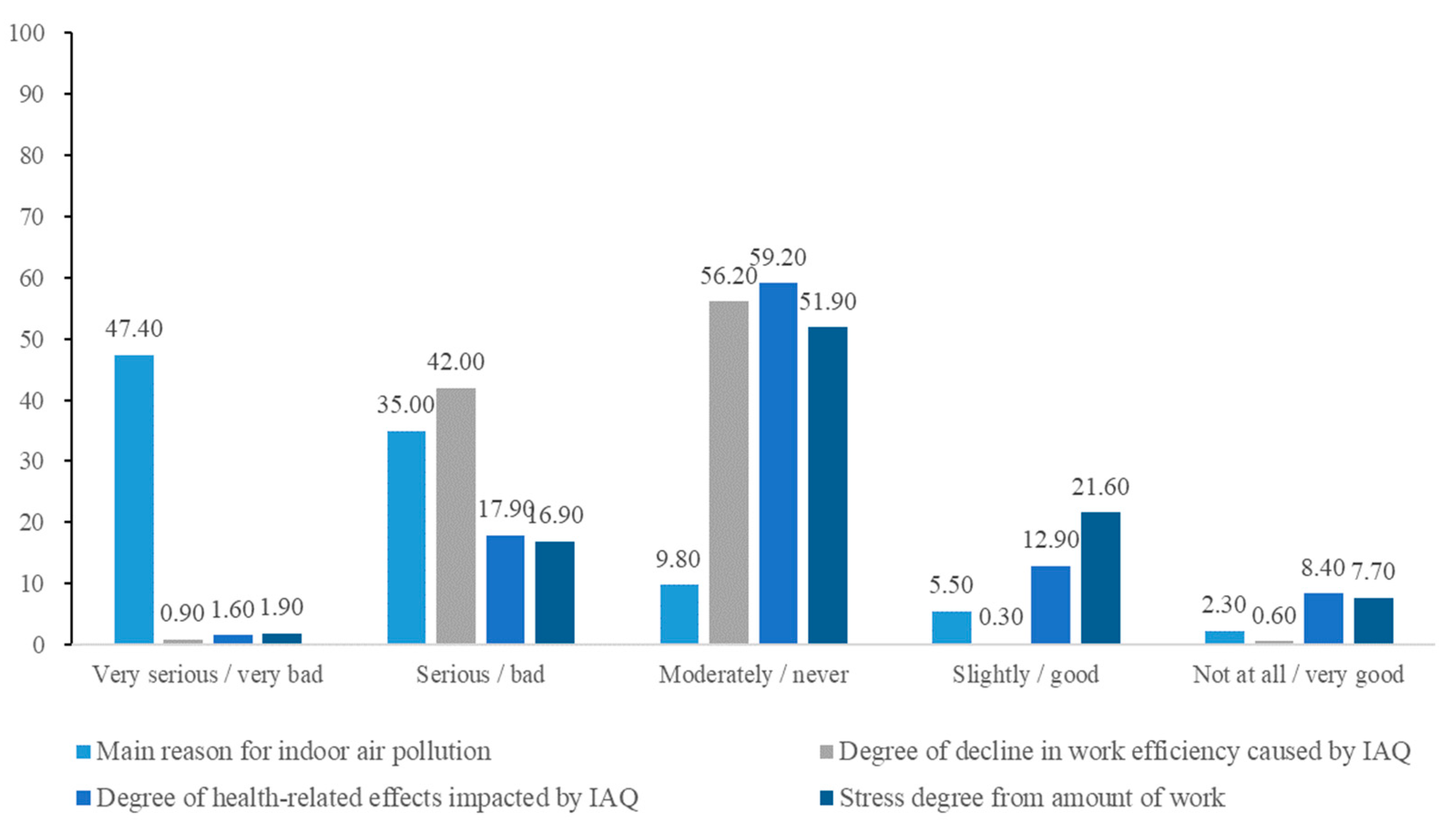
3.1. Questionnaire and Checklist for Office Workers
3.1.1. Office Characteristics
3.1.2. Association between Subjective Symptoms and Environmental Factors
3.2. Indoor and Outdoor Air Pollutant Concentrations
3.3. Health Risk Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, W.; Lee, K.; Yoon, C.; Yu, S.; Park, K.; Choi, W. Determinants of residential indoor air transportation activity times in Korea. J. Expo. Sci. Environ. Epidemiol. 2011, 21, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.; Shuai, J.F.; Kim, T.; Seo, J.; Jung, D.; Ryu, H.; Yang, W. Micro-environmental time activity patterns of weekday and weekend on Korean adults. J. Odor. Indoor. Environ. 2017, 16, 182–186. [Google Scholar] [CrossRef]
- Korean Statistical Information Services. Employment Trend by Occupation. 2019. Available online: https://www.nypi.re.kr/archive/board?menuId=MENU00303&siteId=null (accessed on 11 December 2021).
- Indoor Air Quality Management Group. Guidance Notes for the Management of Indoor Air Quality in Offices and Public Places. 2019. Available online: https://www.iaq.gov.hk/media/82253/gn_officeandpublicplace_eng-2019.pdf (accessed on 11 December 2021).
- Olesen, B.W.; Seelen, J. Criteria for a comfortable indoor environment in buildings. J. Therm. Biol. 1993, 18, 545–549. [Google Scholar] [CrossRef]
- Wolkoff, P.; Skov, P.; Franck, C.; Petersen, L.N. Eye irritation and environmental factors in the office environment hypotheses, causes and a physiological model. Scand. J. Work Environ. Health 2003, 29, 411–430. [Google Scholar] [CrossRef] [PubMed]
- Fisk, W.J. Review of health and productivity gains from better IEQ. Proc. Healthy Build. 2000, 4, 23–34. [Google Scholar]
- Bako Biro, Z.; Wargocki, P.; Weschler, C.J.; Fanger, P.O. Effect of pollution from personal computers on perceived air quality, SBS symptoms and productivity in offices. Indoor Air 2004, 14, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Al Horr, Y.; Arif, M.; Kaushik, A.; Mazroei, A.; Katafygiotou, M.; Elsarrag, E. Occupant productivity and office indoor environment quality: A review of the literature. Build Environ. 2016, 105, 369–389. [Google Scholar] [CrossRef]
- Becchio, C.; Bottero, M.C.; Corgnati, S.P.; Dell’Anna, F.; Fabi, V.; Lingua, C.; Prendin, L.; Ranieri, M. The effects of indoor and outdoor air pollutants on workers’ productivity in office building. E3S Web Conf. 2019, 111, 7. [Google Scholar] [CrossRef]
- Burge, P. Sick building syndrome. Occup. Environ. Med. 2004, 61, 185–190. [Google Scholar] [CrossRef]
- Chang, C.C.; Ruhl, R.A.; Halpern, G.M.; Gershwin, M.E. The sick building syndrome. I. Definition and epidemiological considerations. J. Asthma 1993, 30, 285–295. [Google Scholar] [CrossRef]
- WHO. Indoor Air Pollutants Exposure and Health Effects. Cph. EURO Rep. Stud. 1983, 78, 23–26. [Google Scholar]
- Abdul-Wahab, S.A.; En, S.C.F.; Elkamel, A.; Ahmadi, L.; Yetilmezsoy, K. A review of standards and guidelines set by international bodies for the parameters of indoor air quality. Atmos Pollut. Res. 2015, 6, 751–767. [Google Scholar] [CrossRef]
- Weekes, D., Jr.; Lapotaire, J.P.; Persily, A.; Siegel, J.; Stephens, B.; Walker, I.; Wargocki, P.; White, B. ASHRAE Position Document on Indoor Air Quality. 2020. Available online: https://www.ashrae.org/file%20library/about/position%20documents/pd_indoor-air-quality-2020-07-01.pdf (accessed on 12 December 2021).
- Lu, C.Y.; Lin, J.M.; Chen, Y.Y.; Chen, Y.C. Building-related symptoms among office employees associated with indoor carbon dioxide and total volatile organic compounds. Int. J. Environ. Res. Public Health 2015, 12, 5833–5845. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, Y.; Nishimura, H. A badge-type personal sampler for measurement of personal exposure to NO2 and NO in ambient air. Environ. Int. 1982, 8, 235–242. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency Integrated Risk Information System (US EPA IRIS). Available online: https://www.epa.gov/iris (accessed on 13 July 2021).
- National Institute of Environmental Research. Korean Exposure Factors Handbook; National Institute of Environmental Research: Incheon, Korea, 2019.
- Zhang, R.; Hong, T. Modeling of HVAC operational faults in building performance simulation. Appl. Energy 2017, 202, 178–188. [Google Scholar] [CrossRef]
- Dascalaki, E.G.; Lagoudi, A.; Balaras, C.A.; Gaglia, A.G. Air quality in hospital operating rooms. Build Environ. 2008, 43, 1945–1952. [Google Scholar] [CrossRef]
- Villanueva, F.; Tapia, A.; Lara, S.; Amo-Salas, M. Indoor and outdoor air concentrations of volatile organic compounds and NO2 in schools of urban, industrial and rural areas in Central-Southern Spain. Sci. Total Environ. 2018, 622, 222–235. [Google Scholar] [CrossRef]
- Massolo, L.; Rehwagen, M.; Porta, A.; Ronco, A.; Herbarth, O.; Mueller, A. Indoor-outdoor distribution and risk assessment of volatile organic compounds in the atmosphere of industrial and urban area. Environ. Toxicol. 2009, 25, 339–349. [Google Scholar] [CrossRef]
- Assanov, D.; Zapasnyi, V. and Kerimray, A. Air quality and industrial emissions in the cities of Kazakhstan 2021. Atmos 2021, 12, 314. [Google Scholar] [CrossRef]
- Kim, D.H.; Son, Y.S.; Lee, T.J.; Jo, Y.M. Particulate matter and influencing factors in domestic elementary schools. J. Korean Soc. Atmos. Environ. 2020, 36, 153–170. [Google Scholar] [CrossRef][Green Version]
- Destaillats, H.; Maddalena, R.L.; Singer, B.C.; Hodgson, A.T.; McKone, T.E. Indoor pollutants emitted by office equipment: A review of reported data and information needs. Atmos Environ. 2008, 42, 1371–1388. [Google Scholar] [CrossRef]
- Kowalska, J.; Szewczyńska, M.; Pośniak, M. Measurements of chlorinated volatile organic compounds emitted from office printers and photocopiers. Environ. Sci. Pollut. Res. 2015, 22, 5241–5252. [Google Scholar] [CrossRef] [PubMed]
- Lai, D.; Karava, P.; Chen, Q. Study of outdoor ozone penetration into buildings through ventilation and infiltration. Build Environ. 2015, 93, 112–118. [Google Scholar] [CrossRef]
- Dimakopoulou, K.; Grivas, G.; Samoli, E.; Rodopoulou, S.; Spyratos, D.; Papakosta, D.; Karakatsani, A.; Chaloulakou, A.; Katsouyanni, K. Determinants of personal exposure to ozone in school children. Results from a panel study in Greece. Environ. Res. 2017, 154, 66–72. [Google Scholar] [CrossRef]
- Salonen, H.; Salthammer, T.; Morawska, L. Human exposure to NO2 in school and office indoor environments. Environ. Int. 2019, 130, 104–887. [Google Scholar] [CrossRef]
- Sun, Y.; Hou, J.; Cheng, R.; Sheng, Y.; Zhang, X.; Sundell, J. Indoor air quality, ventilation and their associations with sick building syndrome in Chinese homes. Energy Build 2019, 197, 112–119. [Google Scholar] [CrossRef]
- Mentese, S.; Mirici, N.A.; Elbir, T.; Palaz, E.; Mumcuoğlu, D.T.; Cotuker, O.; Bakar, C.; Oymak, S.; Otkun, M.T. A long-term multi-parametric monitoring study: Indoor air quality (IAQ) and the sources of the pollutants, prevalence of sick building syndrome (SBS) symptoms, and respiratory health indicators. Atmos. Pollut. Res. 2020, 11, 2270–2281. [Google Scholar] [CrossRef]
- Zainal, Z.A.; Hashim, Z.; Jalaludin, J.; Lee, L.F.; Hashim, J.H. Sick building syndrome among office workers in relation to office environment and indoor air pollutant air at an academic institution, Malaysis. Malaysian. J. Med. Health Sci. 2019, 15, 126–134. [Google Scholar]
- Sundell, J. On the association between building ventilation characteristics, some indoor environmental exposures, some allergic manifestations and subjective symptom reports. Indoor Air 1994, 4, 7–49. [Google Scholar] [CrossRef]
- Mendell, M.J. Non-specific symptoms in office workers: A review and summary of the epidemiological literature. Indoor Air 1993, 3, 227–236. [Google Scholar] [CrossRef]
- Bjurnsson, E.; Janson, C.; Norbäck, D.; Boman, G. Symptoms related to the sick building syndrome in a general population sample: Associations with atopy, bronchial hyper-responsiveness and anxiety. Int. J. Tuberc. Lung Dis. 1998, 2, 1023–1028. [Google Scholar]
- Jafari, M.J.; Khajevandi, A.A.; Najarkola, S.A.M.; Yekaninejad, M.S.; Pourhoseingholi, M.A.; Omidi, L.; Kalantary, S. Association of sick building syndrome with indoor air parameters. Tanaffos 2015, 14, 55–62. [Google Scholar] [PubMed]
- Baik, J.J.; Cho, S.H.; Park, B.J.; Kang, D.H. Sick building syndrome and the related factors in office workers. J. Prev. Med. Public Health 1997, 30, 157–170. [Google Scholar]
- Yang, J.Y.; Lee, J.H.; Lim, Y.W.; Park, S.E.; Hong, C.S.; Kim, C.S.; Shin, D.C. Factors related to aldehydes exposure and symptoms in residential indoor air. Environ. Toxicol. 2007, 22, 37–47. [Google Scholar]
- Kim, J.C.; Kim, Y.S.; Roh, Y.M.; Hong, S.C.; Lee, C.M.; Jun, H.J. Health risk assessment of indoor HAPs in new apartments. Environ. Health 2007, 33, 1–10. [Google Scholar]
- Janssen, N.A.; Hoek, G.; Brunekreef, B.; Harssema, H.; Mensink, I.; Zuidhof, A. Personal sampling of particles in adults: Relation among personal, indoor, and outdoor air concentrations. Am. J. Epidemiol. 1998, 147, 537–547. [Google Scholar] [CrossRef] [PubMed]

| Pollutants | Sampling Method and Time | Analytical Method | LOD * | Standards ** |
|---|---|---|---|---|
| CO ** | NDIR (Non-dispersive infrared absorption) Sampling time: 30 min, 2 times (30 min before and after working) | Direct-reading instrument | 0.01 ppm | 10 ppm |
| CO2 ** | 1000 ppm | |||
| HCHO **, Acetaldehyde ** | 2,4-DNPH Cartridge (0.5–1.0 L/m) Sampling time: 1 h ※ EPA Method TO-11 (Formaldehyde in ambient air) | HPLC (High performance liquid chromatography) | 0.07 µg/m3 0.05 µg/m3 | 120 µg/m3 (HCHO) (or 0.1 ppm) |
| TVOCs ** | Tenax-tube (50–100 mL/m) Sampling time: 1 h ※ EPA Method TO-17 (Volatile organic compounds in ambient air) | GC-MS (Gas chromatography) | Benzene: 0.04 µg/m3 Toluene: 0.12 µg/m3 Xylene: 0.02 µg/m3 Ethylbenzene: 0.03 µg/m3 | 500 µg/m3 |
| O3 *** | Coated glass filter preloaded in cassettes, nitrite impregnated (passive sampler) sampling time: 6 h | IC (Ion chromatography) | 3 ppb | N.A. ***** |
| NO2 **** | Badge-type diffusive sampler (passive sampler) Sampling time: 1 h | UV-VIS Spectro-photometer | 6 ppb | 0.1 ppm |
| Category | Symptom Group (Mean ± SD) | Non-Symptom Group (Mean ± SD) | p-Value | ||
|---|---|---|---|---|---|
| Dry eye | Gender | Men (n = 199) | 58.10% (n = 126) | 83.90% (n = 73) | 0.00 |
| Women (n = 105) | 41.90% (n = 91) | 16.10% (n = 14) | |||
| Age | 37.85 ± 9.32 | 39.21 ± 10.04 | 0.27 | ||
| Hours spent indoors (h) | 8.48 ± 2.71 | 7.51 ± 3.17 | 0.01 | ||
| Ophthalmitis | Gender | Men (n = 199) | 62.40% (n = 148) | 76.10% (n = 51) | 0.04 |
| Women (n = 105) | 37.60% (n = 89) | 23.90%(n = 16) | |||
| Age | 38.00 ± 9.37 | 39.07 ± 10.13 | 0.42 | ||
| Hours spent indoors (h) | 8.54 ± 2.76 | 7.01 ± 2.97 | 0.00 | ||
| Nasal stuffiness & rhinits | Gender | Men (n = 199) | 61.00% (n = 111) | 72.10% (n = 88) | 0.05 |
| Women (n = 105) | 39.00% (n = 71) | 27.90% (n = 34) | |||
| Age | 37.69 ± 9.38 | 39.07 ± 9.74 | 0.22 | ||
| Hours spent indoors (h) | 8.45 ± 2.82 | 7.84 ± 2.92 | 0.07 | ||
| Headache | Gender | Men (n = 199) | 61.30% (n = 114) | 72.00% (n = 85) | 0.06 |
| Women (n = 105) | 38.70% (n = 72) | 28.00% (n = 33) | |||
| Age | 37.26 ± 8.85 | 39.79 ± 10.39 | 0.02 | ||
| Hours spent indoors (h) | 8.72 ± 2.61 | 7.40 ± 3.10 | 0.00 | ||
| Category | Indoor Air Pollutant | Response to Symptoms | p-Value | |
|---|---|---|---|---|
| Symptom Group (Mean ± SD) | Non Symptom Group (Mean ± SD) | |||
| Dry eye | Benzene | 4.23 ± 3.76 | 3.37 ± 3.36 | 0.05 |
| Ophthalmitis | Benzene | 4.30 ± 3.74 | 2.87 ± 3.12 | 0.02 |
| Ethylbenzene | 13.14 ± 8.52 | 10.87 ± 8.91 | 0.05 | |
| Acetaldehyde | 13.50 ± 12.01 | 11.03 ± 8.14 | 0.05 | |
| Headache | Benzene | 4.28 ± 3.76 | 3.52 ± 8.14 | 0.07 |
| Category | Variable | Linear Regression | R2 | p-Value |
|---|---|---|---|---|
| Benzene | X1: Outdoor concentration of HCHO | y = 0.088X1 + 0.040X2 + 0.081X3 + 0.020X4 –1.191 | 0.626 | 0.01 |
| X2: The number of photo copiers | 0.05 | |||
| X3: Outdoor concentration of Benzene | 0.02 | |||
| X4: Outdoor humidity | 0.05 | |||
| TVOCs | X1: The number of printers | y = 22.105x + 29.732 | 0.144 | 0.04 |
| Toluene | X1: The number of photo copiers | y = 0.070x + 4.133 | 0.243 | 0.01 |
| Ethylbenzene | X1: The number of photo copiers | y = 0.063x + 2.068 | 0.189 | 0.02 |
| m, p-xylene | X1: The number of photo copiers | y = 0.052x + 1.776 | 0.172 | 0.02 |
| o-xylene | X1: Outdoor concentration of HCHO | y = 0.093x + 1.020 | 0.187 | 0.02 |
| Formaldehyde | X1: Use of air purifier | y = −1.784x + 3.576 | 0.341 | 0.00 |
| Acetaldehyde | X1: Use of air purifier | y = −1.048x + 2.421 | 0.191 | 0.03 |
| Air Pollutant | Cancer Risk | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Point Estimate | Probabilistic | |||||||||
| CTE * | Mean | Max | Min | Percentiles | ||||||
| 25 | 50 | 75 | 90 | 95 | ||||||
| Carcinogen | Benzene | 2.9 × 10−6 | 2.91 × 10−6 | 9.10 × 10−6 | 0 | 1.08 × 10−6 | 1.99 × 10−6 | 3.62 × 10−6 | 6.14 × 10−6 | 8.45 × 10−6 |
| Formaldehyde | 4.8 × 10−5 | 4.77 × 10−5 | 2.1 × 10−3 | 0 | 1.41 × 10−5 | 2.86 × 10−5 | 5.70 × 10−5 | 1.0 × 10−4 | 1.5 × 10−4 | |
| Acetaldehyde | 2.7 × 10−6 | 2.70 × 10−6 | 4.94 × 10−5 | 0 | 1.17 × 10−6 | 2.01 × 10−6 | 3.42 × 10−6 | 5.46 × 10−6 | 7.20 × 10−6 | |
| Non- carcinogen | Toluene | 2.4 × 10−2 | 2.4 × 10−2 | 6.5 × 10−1 | 5.2 × 10−4 | 9.5 × 10−3 | 1.6 × 10−2 | 3.0 × 10−2 | 5.0 × 10−2 | 6.8 × 10−2 |
| Ethylbenzene | 1.3 × 10−2 | 1.3 × 10−2 | 1.7 × 10−1 | 6.1 × 10−4 | 7.2 × 10−3 | 1.1 × 10−2 | 1.6 × 10−2 | 2.4 × 10−2 | 3.1 × 10−2 | |
| m, p-xylene | 9.2 × 10−2 | 9.2 × 10−2 | 9.2 × 10−1 | 6.7 × 10−3 | 5.2 × 10−2 | 7.2 × 10−2 | 1.1 × 10−1 | 1.6 × 10−1 | 2.0 × 10−1 | |
| o-xylene | 6.4 × 10−2 | 6.4 × 10−2 | 6.0 × 10−1 | 3.4 × 10−3 | 3.6 × 10−2 | 5.3 × 10−2 | 8.0 × 10−2 | 1.1 × 10−1 | 1.4 × 10−1 | |
| NO2 | 5.0 × 10−4 | 6.1 × 10−4 | 2.1 × 10−3 | 1.0 × 10−4 | 3.8 × 10−4 | 4.8 × 10−4 | 6.0 × 10−4 | 7.3 × 10−4 | 8.3 × 10−4 | |
| O3 | 4.9 × 10−4 | 4.9 × 10−4 | 1.8 × 10−3 | 1.0 × 10−4 | 3.7 × 10−4 | 4.6 × 10−4 | 5.8 × 10−4 | 7.1 × 10−4 | 8.1 × 10−4 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, D.; Choe, Y.; Shin, J.; Kim, E.; Min, G.; Kim, D.; Cho, M.; Lee, C.; Choi, K.; Woo, B.L.; et al. Risk Assessment of Indoor Air Quality and Its Association with Subjective Symptoms among Office Workers in Korea. Int. J. Environ. Res. Public Health 2022, 19, 2446. https://doi.org/10.3390/ijerph19042446
Jung D, Choe Y, Shin J, Kim E, Min G, Kim D, Cho M, Lee C, Choi K, Woo BL, et al. Risk Assessment of Indoor Air Quality and Its Association with Subjective Symptoms among Office Workers in Korea. International Journal of Environmental Research and Public Health. 2022; 19(4):2446. https://doi.org/10.3390/ijerph19042446
Chicago/Turabian StyleJung, Dayoung, Youngtae Choe, Jihun Shin, Eunche Kim, Gihong Min, Dongjun Kim, Mansu Cho, Chaekwan Lee, Kilyong Choi, Byung Lyul Woo, and et al. 2022. "Risk Assessment of Indoor Air Quality and Its Association with Subjective Symptoms among Office Workers in Korea" International Journal of Environmental Research and Public Health 19, no. 4: 2446. https://doi.org/10.3390/ijerph19042446
APA StyleJung, D., Choe, Y., Shin, J., Kim, E., Min, G., Kim, D., Cho, M., Lee, C., Choi, K., Woo, B. L., & Yang, W. (2022). Risk Assessment of Indoor Air Quality and Its Association with Subjective Symptoms among Office Workers in Korea. International Journal of Environmental Research and Public Health, 19(4), 2446. https://doi.org/10.3390/ijerph19042446







