Healthcare Professionals’ Perceptions of Promoting Healthy Lifestyle Behaviors in Pregnant Migrant Women and the Potential of a Digital Support Tool—A Qualitative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Informants and Recruitment
2.3. Ethics
2.4. Data Collection
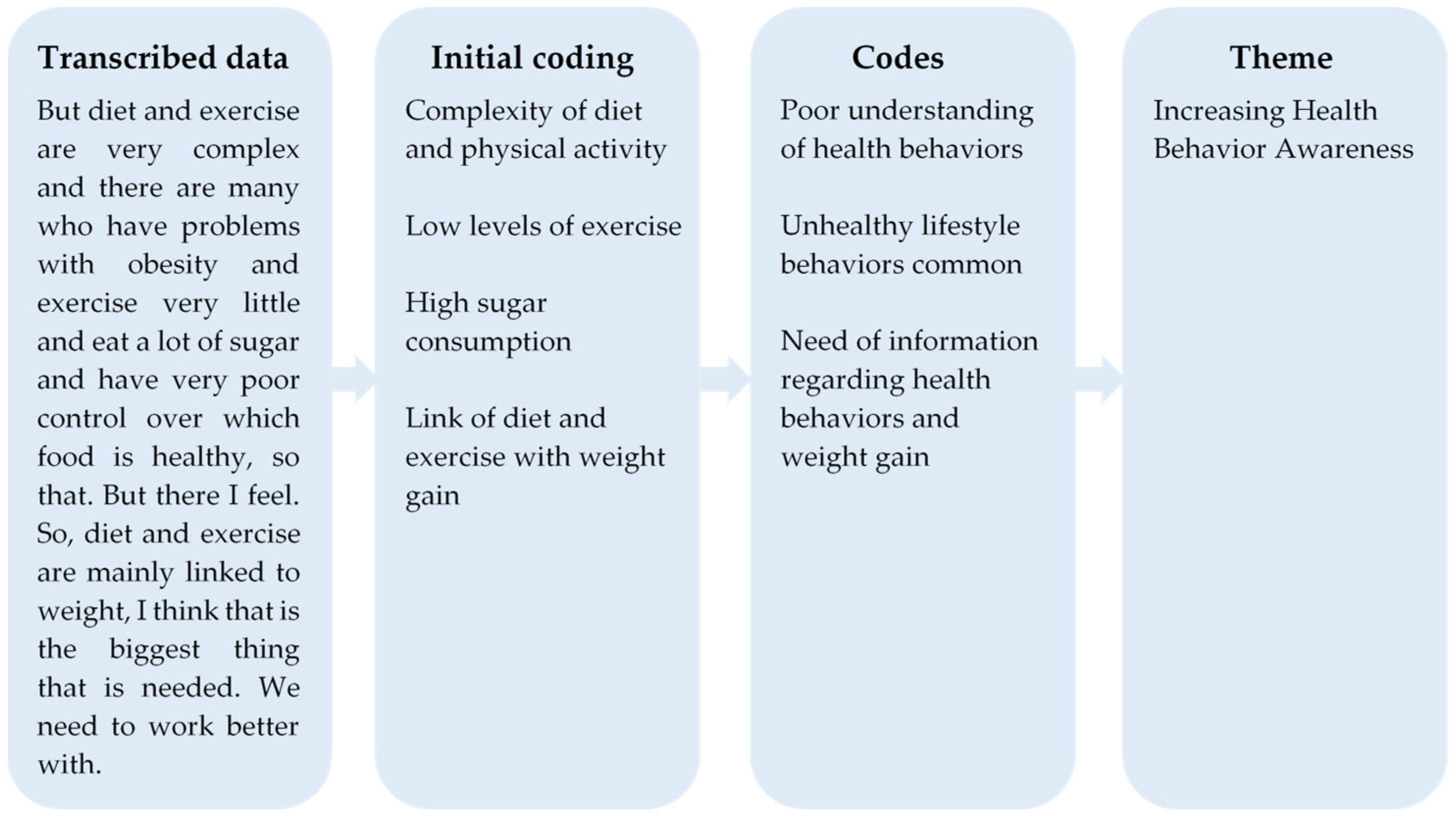
2.5. Data Analysis
3. Results
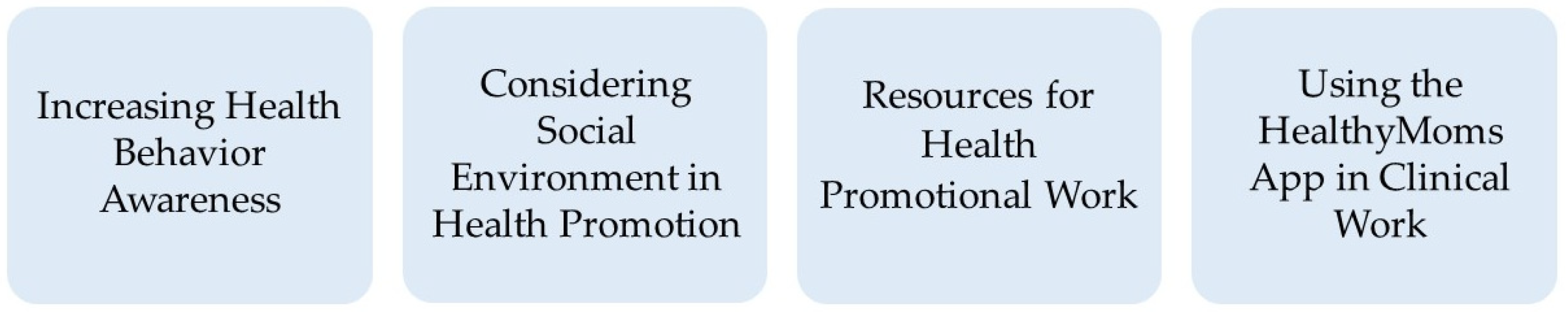
3.1. Increasing Health Behavior Awareness
“I am very unsure if they are aware of… I think, for example, the National Food Administration has certain recommendations for pregnant women. I do not know if they are aware of them. If they have information about them and if they think they are relevant.”(Midwife, delivery ward, interview 10)
“I can imagine that those who come from a country and have not come here voluntarily, may have come here as a refugee or have had to flee from their country, they do not really focus on things like this [lifestyle habits] that I think that they sometimes experience as a bit trivial. They have many other major issues in their lives that they need to solve. Maybe ‘can I stay at all?’, ‘Can my children come here?’, ‘Can my husband come here?’”(Midwife, maternity care, interview 12)
“I think you often can see that they do not care as much about how much weight they gain during a pregnancy and you can often see that the weight increases quite quickly and do not absorb the same information about healthy weight gain and healthy lifestyle habits. I think you can see a big difference there.”(Midwife, maternity care, interview 6)
3.2. Considering Social Environment in Health Promotion
“That you [migrant women] value experiences from previous generations higher than we do. […] It is important to convince the partner but also the women in the surrounding environment such as sisters, mothers, mother-in-law, that in some cases can play an important role. Possibly that we [healthcare professionals] should broaden our views there as well and also aim to direct the information to the women in the surrounding environment.”(Midwife, delivery ward, interview 10)
“You [the women] sleep poorly, you eat poorly, you move too little, you have pretty much none, or almost no, hour of the day where you are alone. Without having to be present and available with your womb, with your body, with your household chores, with your breasts for the children.”(Midwife, maternity care, interview 9)
“But if the woman understands, it is still the woman who fixes the food at home… If the woman herself understands, it is a gain for the whole family, in fact. Both children and husband.”(Physician, endocrinological clinic, interview 8)
3.3. Resources for Health Promotional Work
”To rest on the experience, how it [cultural foods] usually is. And maybe go into details a little. […] So you need to have dug a lot more into the food culture to know what everything means here.”(Dietician, endocrinological clinic, interview 3)
“And then, there is very low trust in us. They do not trust us. And then they have a very hard time following our recommendations. […] Their trust in us is not very strong, so if we recommend medical treatment, it takes time until they understand or accept, so those are challenges.”(Physician, endocrinological clinic, interview 5)
”As I said before, this that you often feel like you could put more energy into these topics [health behaviors] if we had the time, which we do not have room for.”(Midwife, maternity care, interview 13)
“It can be difficult to reach through to them [the women] in a good way when using an interpreter. […] Difficult to get through with tools or tips that suit them and their culture or lifestyle. It may be difficult to motivate them.”(Midwife, maternity care, interview 6)
3.4. Using the HealthyMoms Application in Clinical Work
“Yes, I think that our job automatically becomes easier when the woman has a higher level of knowledge and maybe a bit more compliance to good diet and exercise habits through this [the app]. It will feel easier for us to communicate about this. And hopefully that it then leads to that if we are really lucky, or what you say, and it works then the pregnant woman should gain less [weight], have lower risk of gestational diabetes and then that means less work for us, yes, like that. If one is to think about all the benefits.”(Midwife, maternity care, interview 2)
“I still think we need to keep it [the health promotion work] a bit in the profession and bring in effective aids. But it cannot be replaced with just an IT solution, you must have both. I feel that. So I feel that there is a risk that it will only be digitized. I think that’s a shame. You must have aids, but still need the skills of midwives and be able to talk about these things. I think that is important from a public health perspective.”(Physician, maternity care, interview 14)
“But the starting point must be in their own context. What are their lifestyles? What knowledge have they gained from growing up? How should we think now? What was good, what was not good?”(Midwife, maternity care, interview 12)
4. Discussion
4.1. Main Findings
4.2. Comparison with Previous Work
4.3. Strengths and Limitations
4.4. Implications and Clinical Relevance
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Voerman, E.; Santos, S.; Inskip, H.; Amiano, P.; Barros, H.; Charles, M.A.; Chatzi, L.; Chrousos, G.P.; Corpeleijn, E.; Crozier, S.; et al. Association of gestational weight gain with adverse maternal and infant outcomes. JAMA 2019, 321, 1702–1715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.; Boyle, J.A.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; Rode, L.; et al. Association of gestational weight gain with maternal and infant outcomes: A systematic review and meta-analysis. JAMA 2017, 317, 2207–2225. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.; Voerman, E.; Amiano, P.; Barros, H.; Beilin, L.J.; Bergström, A.; Charles, M.A.; Chatzi, L.; Chevrier, C.; Chrousos, G.P.; et al. Impact of maternal body mass index and gestational weight gain on pregnancy complications: An individual participant data meta-analysis of European, North American and Australian cohorts. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 984–995. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, R.F.; Abell, S.K.; Ranasinha, S.; Misso, M.L.; Boyle, J.A.; Harrison, C.L.; Black, M.H.; Li, N.; Hu, G.; Corrado, F.; et al. Gestational weight gain across continents and ethnicity: Systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Med. 2018, 16, 153. [Google Scholar] [CrossRef] [PubMed]
- Han, Z.; Lutsiv, O.; Mulla, S.; Rosen, A.; Beyene, J.; McDonald, S.D. Low gestational weight gain and the risk of preterm birth and low birthweight: A systematic review and meta-analyses. Acta Obstet. Gynecol. Scand. 2011, 90, 935–954. [Google Scholar] [CrossRef]
- Henriksson, P.; Sandborg, J.; Blomberg, M.; Nowicka, P.; Petersson, K.; Bendtsen, M.; Rosell, M.; Löf, M. Body mass index and gestational weight gain in migrant women by birth regions compared with Swedish-born women: A registry linkage study of 0.5 million pregnancies. PLoS ONE 2020, 15, e0241319. [Google Scholar] [CrossRef]
- Heslehurst, N.; Brown, H.; Pemu, A.; Coleman, H.; Rankin, J. Perinatal health outcomes and care among asylum seekers and refugees: A systematic review of systematic reviews. BMC Med. 2018, 16, 89. [Google Scholar] [CrossRef]
- Behboudi-Gandevani, S.; Parajuli, R.; Vaismoradi, M. A systematic review of the prevalence of gestational diabetes in Norway. Int. J. Environ. Res. Public Health 2021, 18, 1423. [Google Scholar] [CrossRef]
- Song, C.; Lyu, Y.; Li, C.; Liu, P.; Li, J.; Ma, R.C.; Yang, X. Long-term risk of diabetes in women at varying durations after gestational diabetes: A systematic review and meta-analysis with more than 2 million women. Obes. Rev. 2018, 19, 421–429. [Google Scholar] [CrossRef]
- Kramer, C.K.; Campbell, S.; Retnakaran, R. Gestational diabetes and the risk of cardiovascular disease in women: A systematic review and meta-analysis. Diabetologia 2019, 62, 905–914. [Google Scholar] [CrossRef] [Green Version]
- Muktabhant, B.; Lawrie, T.A.; Lumbiganon, P.; Laopaiboon, M. Diet or exercise, or both, for preventing excessive weight gain in pregnancy. Cochrane Database Syst. Rev. 2015, 15, CD007145. [Google Scholar] [CrossRef]
- O’Brien, O.A.; McCarthy, M.; Gibney, E.R.; McAuliffe, F.M. Technology-supported dietary and lifestyle interventions in healthy pregnant women: A systematic review. Eur. J. Clin. Nutr. 2014, 68, 760–766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The World Health Organization. mHealth: Use of Appropriate Digital Technologies for Public Health: Report by the Director-General. Available online: https://apps.who.int/iris/handle/10665/274134 (accessed on 11 January 2022).
- Sandborg, J.; Söderström, E.; Henriksson, P.; Bendtsen, M.; Henström, M.; Leppänen, M.H.; Maddison, R.; Migueles, J.H.; Blomberg, M.; Löf, M. Effectiveness of a Smartphone App to Promote Healthy Weight Gain, Diet, and Physical Activity During Pregnancy (HealthyMoms): Randomized Controlled Trial. JMIR mHealth uHealth 2021, 9, e26091. [Google Scholar] [CrossRef] [PubMed]
- Sandborg, J.; Henriksson, P.; Larsen, E.; Lindqvist, A.-K.; Rutberg, S.; Söderström, E.; Maddison, R.; Löf, M. Participants’ Engagement and Satisfaction with a Smartphone App Intended to Support Healthy Weight Gain, Diet, and Physical Activity During Pregnancy: Qualitative Study Within the HealthyMoms Trial. JMIR mHealth uHealth 2021, 9, e26159. [Google Scholar] [CrossRef] [PubMed]
- Shieh, C.; Cullen, D.L.; Pike, C.; Pressler, S.J. Intervention strategies for preventing excessive gestational weight gain: Systematic review and meta-analysis. Obes. Rev. 2018, 19, 1093–1109. [Google Scholar] [CrossRef] [Green Version]
- Hughson, J.P.; Daly, J.O.; Woodward-Kron, R.; Hajek, J.; Story, D. The rise of pregnancy apps and the implications for culturally and linguistically diverse women: Narrative review. JMIR mHealth uHealth 2018, 6, e189. [Google Scholar] [CrossRef] [Green Version]
- Statistics Sweden. Number of Migrations and Migrants during the Period 2010–2019 by Country of Birth and Number of Migrations. Available online: https://www.scb.se/en/finding-statistics/statistics-by-subject-area/population/population-composition/population-statistics/ (accessed on 11 January 2022).
- Bendtsen, M.; Bendtsen, P.; Henriksson, H.; Henriksson, P.; Müssener, U.; Thomas, K.; Löf, M. The mobile health multiple lifestyle behavior interventions across the Lifespan (MoBILE) research program: Protocol for development, evaluation, and implementation. J. Med. Internet Res. 2020, 22, e14894. [Google Scholar] [CrossRef]
- Patton, M.Q. Qualitative Research & Evaluation Methods, 4th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2015. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [Green Version]
- Ngongalah, L.; Rankin, J.; Rapley, T.; Odeniyi, A.; Akhter, Z.; Heslehurst, N. Dietary and physical activity behaviours in African migrant women living in high income countries: A systematic review and framework synthesis. Nutrients 2018, 10, 1017. [Google Scholar] [CrossRef] [Green Version]
- Persson, G.; Mahmud, A.J.; Hansson, E.E.; Strandberg, E.L. Somali women’s view of physical activity—A focus group study. BMC Womens Health 2014, 14, 129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodwin, L.; Hunter, B.; Jones, A. The midwife–woman relationship in a South Wales community: Experiences of midwives and migrant Pakistani women in early pregnancy. Health Expect. 2018, 21, 347–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tankwanchi, A.S.; Bowman, B.; Garrison, M.; Larson, H.; Wiysonge, C.S. Vaccine hesitancy in migrant communities: A rapid review of latest evidence. Curr. Opin. Immunol. 2021, 71, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Merry, L.; Villadsen, S.F.; Sicard, V.; Lewis-Hibbert, N. Transnationalism and care of migrant families during pregnancy, postpartum and early-childhood: An integrative review. BMC Health Serv. Res. 2020, 20, 778. [Google Scholar] [CrossRef] [PubMed]
- Kasper, A.; Mohwinkel, L.; Nowak, A.C.; Kolip, P. Maternal health care for refugee women—A qualitative review. Midwifery 2022, 104, 103157. [Google Scholar] [CrossRef]
- Mårtensson, L.; Lytsy, P.; Westerling, R.; Wångdahl, J. Experiences and needs concerning health related information for newly arrived refugees in Sweden. BMC Public Health 2020, 20, 1044. [Google Scholar] [CrossRef]
- Henriksson, H.; Alexandrou, C.; Henriksson, P.; Henström, M.; Bendtsen, M.; Thomas, K.; Müssener, U.; Nilsen, P.; Löf, M. MINISTOP 2.0: A smartphone app integrated in primary child health care to promote healthy diet and physical activity behaviours and prevent obesity in preschool-aged children: Protocol for a hybrid design effectiveness-implementation study. BMC Public Health 2020, 20, 1756. [Google Scholar] [CrossRef]
- Alexandrou, C.; Müssener, U.; Thomas, K.; Henriksson, H.; Löf, M. Adapting a parental support app to promote healthy diet and physical activity behaviors (MINISTOP) for a multi-ethnic setting: A qualitative study on the needs and preferences of parents and nurses within Swedish child health care. Nutrients 2021, 13, 2190. [Google Scholar] [CrossRef]
- Moser, A.; Korstjens, I. Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. Eur. J. Gen. Pract. 2018, 24, 9–18. [Google Scholar] [CrossRef] [Green Version]
- Korstjens, I.; Moser, A. Series: Practical guidance to qualitative research. Part 4: Trustworthiness and Series: Practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur. J. Gen. Pract. 2018, 24, 120–124. [Google Scholar] [CrossRef] [Green Version]
- The World Health Organization. Diagnostic Criteria and Classification of Hyperglycaemia First Detected in Pregnancy. Available online: https://www.who.int/publications/i/item/WHO-NMH-MND-13.2 (accessed on 12 January 2022).
- Statistics Sweden. ICT Usage in Households and by Individuals 2020. Available online: https://www.scb.se/en/finding-statistics/statistics-by-subject-area/living-conditions/living-conditions/ict-usage-in-households-and-by-individuals/pong/publications/ict-usage-in-households-and-by-individuals-2020/ (accessed on 7 February 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Söderström, E.; Müssener, U.; Löfgren, M.; Sandell, L.; Thomas, K.; Löf, M. Healthcare Professionals’ Perceptions of Promoting Healthy Lifestyle Behaviors in Pregnant Migrant Women and the Potential of a Digital Support Tool—A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 2328. https://doi.org/10.3390/ijerph19042328
Söderström E, Müssener U, Löfgren M, Sandell L, Thomas K, Löf M. Healthcare Professionals’ Perceptions of Promoting Healthy Lifestyle Behaviors in Pregnant Migrant Women and the Potential of a Digital Support Tool—A Qualitative Study. International Journal of Environmental Research and Public Health. 2022; 19(4):2328. https://doi.org/10.3390/ijerph19042328
Chicago/Turabian StyleSöderström, Emmie, Ulrika Müssener, Mikaela Löfgren, Linnea Sandell, Kristin Thomas, and Marie Löf. 2022. "Healthcare Professionals’ Perceptions of Promoting Healthy Lifestyle Behaviors in Pregnant Migrant Women and the Potential of a Digital Support Tool—A Qualitative Study" International Journal of Environmental Research and Public Health 19, no. 4: 2328. https://doi.org/10.3390/ijerph19042328
APA StyleSöderström, E., Müssener, U., Löfgren, M., Sandell, L., Thomas, K., & Löf, M. (2022). Healthcare Professionals’ Perceptions of Promoting Healthy Lifestyle Behaviors in Pregnant Migrant Women and the Potential of a Digital Support Tool—A Qualitative Study. International Journal of Environmental Research and Public Health, 19(4), 2328. https://doi.org/10.3390/ijerph19042328





