Healthy Dwelling: Design of Biophilic Interior Environments Fostering Self-Care Practices for People Living with Migraines, Chronic Pain, and Depression
Abstract
:1. Introduction
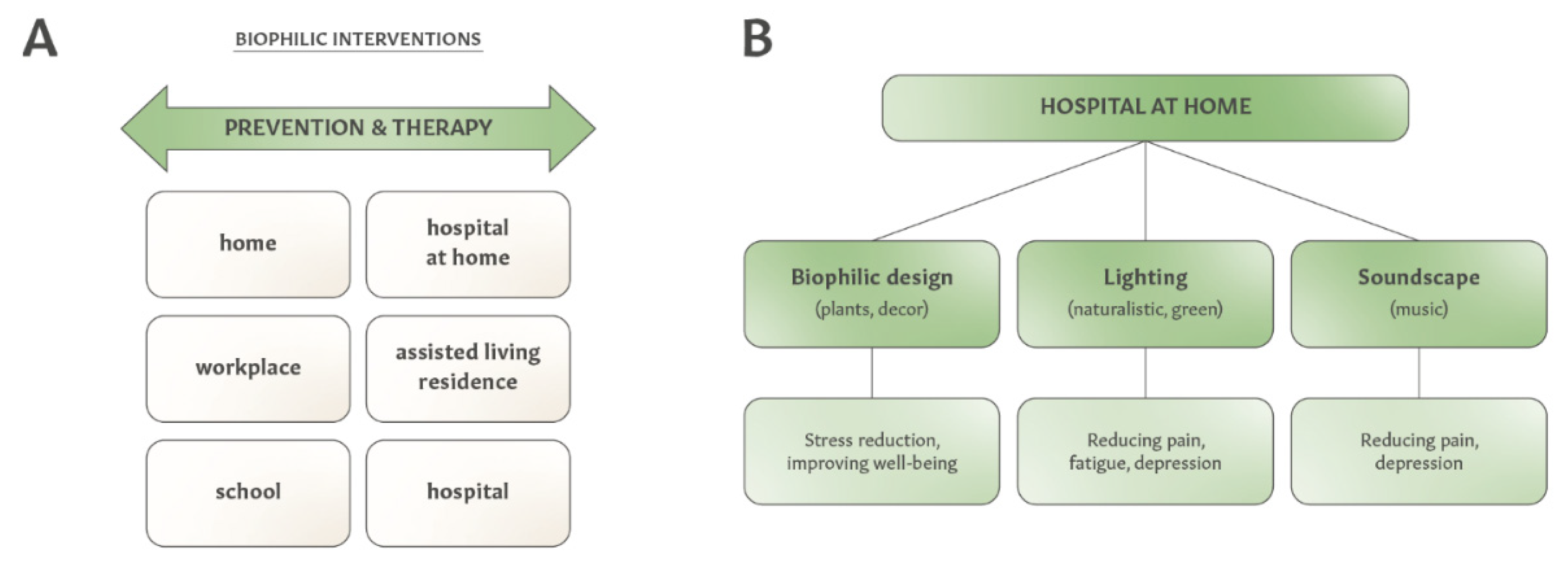
2. Integrating Biophilic Design and Self-Care to Create Therapeutic Interior Environments
3. Therapeutic Interior Design for People with Chronic Diseases
3.1. Designing Therapeutic Interior Environments for People with Migraines
| Modality | Studies Supporting Interior Landscapes Integrating Biophilic Interventions and Self-Care |
|---|---|
| Exposure to nature | |
| Green LED light |
|
| Aromatherapy | |
| Relaxation and mindfulness meditation | |
| Yoga |
|
| Sleep hygiene |
|
| Nutrition |
|
3.2. Designing Therapeutic Interior Environments for People with Chronic Pain
| Modality | Studies Supporting Interior Landscapes Integrating Biophilic Interventions and Self-Care |
|---|---|
| Exposure to nature | |
| Lighting | |
| Music |
|
| Physical activity, yoga and breathing exercises | |
| Mindfulness meditation | |
| Sleep hygiene | |
| Combination of modalities |
3.3. Designing Therapeutic Interior Environments for People with Depression
| Modality | Studies Supporting Interior Landscapes Integrating Biophilic Interventions and Self-Care |
|---|---|
| Exposure to nature | |
| Lighting |
|
| Music | |
| Physical activity and yoga |
|
| Mindfulness meditation | |
| Breathing exercises |
|
| Aromatherapy |
|
| Sleep hygiene | |
| Nutrition |
|
4. Expanding Interior Design Elements for Therapeutic Purposes
5. Advancing Therapeutic Interior Design to Improve Healthcare Outcomes
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [Green Version]
- Feigin, V.L.; Vos, T.; Nichols, E.; Owolabi, O.M.; Carroll, W.M.; Dichgans, M.; Deuschl, G.; Parmar, P.; Brainin, M.; Murray, C. The global burden of neurological disorders: Translating evidence into policy. Lancet Neurol. 2019, 19, 255–265. [Google Scholar] [CrossRef]
- Booth, F.W.; Roberts, C.K.; Thyfault, J.P.; Ruegsegger, G.N.; Toedebusch, R.G. Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms. Physiol. Rev. 2017, 97, 1351–1402. [Google Scholar] [CrossRef]
- Brasche, S.; Bischof, W. Daily time spent indoors in German homes—Baseline data for the assessment of indoor exposure of German occupants. Int. J. Hyg. Environ. Health 2005, 208, 247–253. [Google Scholar] [CrossRef]
- Pears, M.; Kola-Palmer, S.; De Azevedo, L.B. The impact of sitting time and physical activity on mental health during COVID-19 lockdown. Sport Sci. Health 2021, 1–13. [Google Scholar] [CrossRef]
- Manger, S. Lifestyle interventions for mental health. Aust. J. Gen. Pr. 2019, 48, 670–673. [Google Scholar] [CrossRef]
- Dean, E.; Söderlund, A. What is the role of lifestyle behaviour change associated with non-communicable disease risk in managing musculoskeletal health conditions with special reference to chronic pain? BMC Musculoskelet. Disord. 2015, 16, 1–7. [Google Scholar] [CrossRef]
- Bulaj, G.; Clark, J.; Ebrahimi, M.; Bald, E. From Precision Metapharmacology to Patient Empowerment: Delivery of Self-Care Practices for Epilepsy, Pain, Depression and Cancer Using Digital Health Technologies. Front. Pharmacol. 2021, 12. [Google Scholar] [CrossRef]
- Yassein, G.; Ebrahiem, S. Biophilic Design in the Built Environment to Improve Well-Being: A Systematic Review of Practices. J. Urban Res. 2018, 30, 128–146. [Google Scholar] [CrossRef]
- Wilson, E.O. Biophilia; Harvard University Press: Cambridge, MA, USA, 1984. [Google Scholar]
- Kellert, S.R.; Calabrese, E.F. The Practice of Biophilic Design; Terrapin Bright LLC: London, UK, 2015; Available online: https://www.biophilic-design.com/ (accessed on 12 February 2022).
- Kellert, S.R.; Heerwagen, J.; Mador, M. Biophilic Design: The Theory, Science, and Practice of Bringing Buildings to Life; Wiley & Sons: New York, NY, USA; Hoboken, NJ, USA, 2008. [Google Scholar]
- Gillis, K.; Gatersleben, B. A Review of Psychological Literature on the Health and Wellbeing Benefits of Biophilic Design. Buildings 2015, 5, 948–963. [Google Scholar] [CrossRef] [Green Version]
- Taylor, R. The Potential of Biophilic Fractal Designs to Promote Health and Performance: A Review of Experiments and Applications. Sustainability 2021, 13, 823. [Google Scholar] [CrossRef]
- Zhong, W.; Schröder, T.; Bekkering, J. Biophilic design in architecture and its contributions to health, well-being, and sustainability: A critical review. Front. Arch. Res. 2021. [Google Scholar] [CrossRef]
- Thomas, C.; Xing, Y. To What Extent Is Biophilia Implemented in the Built Environment to Improve Health and Wellbeing?—State-of-the-Art Review and a Holistic Biophilic Design Framework. Emerg. Res. Sustain. Energy Build. A Low-Carbon Future 2021, 227–247. [Google Scholar] [CrossRef]
- Hung, S.-H.; Chang, C.-Y. Health benefits of evidence-based biophilic-designed environments: A review. J. People Plants Environ. 2021, 24, 1–16. [Google Scholar] [CrossRef]
- Barbiero, G.; Berto, R. Biophilia as Evolutionary Adaptation: An Onto- and Phylogenetic Framework for Biophilic Design. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef]
- McSweeney, J.; Rainham, D.; Johnson, S.A.; Sherry, S.B.; Singleton, J. Indoor nature exposure (INE): A health-promotion framework. Health Promot. Int. 2014, 30, 126–139. [Google Scholar] [CrossRef] [Green Version]
- Yin, J.; Yuan, J.; Arfaei, N.; Catalano, P.J.; Allen, J.G.; Spengler, J.D. Effects of biophilic indoor environment on stress and anxiety recovery: A between-subjects experiment in virtual reality. Environ. Int. 2019, 136, 105427. [Google Scholar] [CrossRef]
- McSweeney, J.; Johnson, S.; Sherry, S.; Singleton, J.; Rainham, D. Indoor nature exposure and influence on physiological stress markers. Int. J. Environ. Health Res. 2019, 1–15. [Google Scholar] [CrossRef]
- McGee, B.; Marshall-Baker, A. Loving Nature From the Inside Out. HERD Health Environ. Res. Des. J. 2015, 8, 115–130. [Google Scholar] [CrossRef]
- Gray, T.; Birrell, C. Are Biophilic-Designed Site Office Buildings Linked to Health Benefits and High Performing Occupants? Int. J. Environ. Res. Public Health 2014, 11, 12204–12222. [Google Scholar] [CrossRef] [Green Version]
- Khanehshenas, F.; Habibi, P.; Zakerian, S.A. The Effect of Biophilic Design Patterns on Employee’s Health and Well-being: A Systematic Review. J. Ergon. 2020, 7, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Peters, T.; Verderber, S. Biophilic Design Strategies in Long-Term Residential Care Environments for Persons with Dementia. J. Aging Environ. 2021, 1–29. [Google Scholar] [CrossRef]
- Nuamah, J.; Rodriguez-Paras, C.; Sasangohar, F. Veteran-Centered Investigation of Architectural and Space Design Considerations for Post-Traumatic Stress Disorder (PTSD). HERD: Heal. Environ. Res. Des. J. 2020, 14, 164–173. [Google Scholar] [CrossRef]
- Norouzi, N.; Garza, C.M. Architecture for Children With Autism Spectrum Disorder and Their Therapists. HERD Health Environ. Res. Des. J. 2021, 14, 147–156. [Google Scholar] [CrossRef]
- Lattacher, S.L.; Wohofsky, L.; Scharf, P.; Krainer, D. A Customized Smart Home and Interior Design Concept Co-Designed with and for People with Autism Spectrum Disorder. In Navigating Healthcare through Challenging Times; IOS Press: Amsterdam, The Netherlands, 2021; Volume 279, pp. 36–37. [Google Scholar] [CrossRef]
- Shin, J.-H.; Dennis, J.S.; Mohammed, H. Mental Health Outcome Measures in Environmental Design Research: A Critical Review. HERD: Health Environ. Res. Des. J. 2021, 14, 331–357. [Google Scholar] [CrossRef]
- Engineer, A.; Sternberg, E.M.; Najafi, B. Designing Interiors to Mitigate Physical and Cognitive Deficits Related to Aging and to Promote Longevity in Older Adults: A Review. Gerontology 2018, 64, 612–622. [Google Scholar] [CrossRef]
- Lee, Y.; Park, J.; Jang, M. Perceived effects of home renovation on independence of physically disabled Koreans living at home. Disabil. Rehabil. 2017, 40, 2380–2387. [Google Scholar] [CrossRef]
- Capasso, L.; D’Alessandro, D. Housing and health: Here we go again. Int. J. Environ. Res. Public Health 2021, 18, 12060. [Google Scholar] [CrossRef]
- Besedovsky, L.; Lange, T.; Haack, M. The Sleep-Immune Crosstalk in Health and Disease. Physiol. Rev. 2019, 99, 1325–1380. [Google Scholar] [CrossRef] [Green Version]
- Goldstein, A.N.; Walker, M.P. The Role of Sleep in Emotional Brain Function. Annu. Rev. Clin. Psychol. 2014, 10, 679–708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tiseo, C.; Vacca, A.; Felbush, A.; Filimonova, T.; Gai, A.; Glazyrina, T.; Hubalek, I.A.; Marchenko, Y.; Overeem, L.H.; Piroso, S.; et al. Migraine and sleep disorders: A systematic review. J. Headache Pain 2020, 21, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Jin, X.; Shan, Z.; Li, S.; Huang, H.; Li, P.; Peng, X.; Peng, Z.; Yu, K.; Bao, W.; et al. Relationship of Sleep Duration With All-Cause Mortality and Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. J. Am. Heart Assoc. 2017, 6, e005947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leubner, D.; Hinterberger, T. Reviewing the Effectiveness of Music Interventions in Treating Depression. Front. Psychol. 2017, 8, 1109. [Google Scholar] [CrossRef] [Green Version]
- Tang, Q.; Huang, Z.; Zhou, H.; Ye, P. Effects of music therapy on depression: A meta-analysis of randomized controlled trials. PLoS ONE 2020, 15, e0240862. [Google Scholar] [CrossRef]
- Garza-Villarreal, A.E.; Pando, V.; Vuust, P.; Parsons, C. Music-Induced Analgesia in Chronic Pain Conditions: A Systematic Review and Meta-Analysis. Pain Physician 2017, 20, 597–610. [Google Scholar] [CrossRef] [PubMed]
- Martin-Saavedra, J.S.; Vergara-Mendez, L.D.; Pradilla, I.; Vélez-Van-Meerbeke, A.; Talero-Gutiérrez, C. Standardizing music characteristics for the management of pain: A systematic review and meta-analysis of clinical trials. Complement. Ther. Med. 2018, 41, 81–89. [Google Scholar] [CrossRef]
- Sahlin, E.; Ahlborg, J.G.; Tenenbaum, A.; Grahn, P. Using Nature-Based Rehabilitation to Restart a Stalled Process of Rehabilitation in Individuals with Stress-Related Mental Illness. Int. J. Environ. Res. Public Health 2015, 12, 1928–1951. [Google Scholar] [CrossRef] [Green Version]
- Kang, B.; Kim, T.; Kim, M.J.; Lee, K.H.; Choi, S.; Lee, N.H.; Kim, H.R.; Jun, B.; Park, S.Y.; Lee, S.J.; et al. Relief of Chronic Posterior Neck Pain Depending on the Type of Forest Therapy: Comparison of the Therapeutic Effect of Forest Bathing Alone Versus Forest Bathing With Exercise. Ann. Rehabil. Med. 2015, 39, 957–963. [Google Scholar] [CrossRef] [Green Version]
- Park, S.-H.; Mattson, R.H. Ornamental Indoor Plants in Hospital Rooms Enhanced Health Outcomes of Patients Recovering from Surgery. J. Altern. Complement. Med. 2009, 15, 975–980. [Google Scholar] [CrossRef]
- Yavne, Y.; Kabaha, A.; Rosen, T.; Avisar, I.; Orbach, H.; Amital, D.; Amital, H. The Powers of Flowers: Evaluating the Impact of Floral Therapy on Pain and Psychiatric Symptoms in Fibromyalgia. Israel Med. Assoc. J. IMAJ 2019, 21, 449–453. [Google Scholar]
- Kim, H.; Kim, J.; Ju, H.J.; Jang, B.J.; Wang, T.K.; Kim, Y.I. Effect of Forest Therapy for Menopausal Women with Insomnia. Int. J. Environ. Res. Public Health 2020, 17, 6548. [Google Scholar] [CrossRef]
- Shin, J.C.; Parab, K.V.; An, R.; Grigsby-Toussaint, D.S. Greenspace exposure and sleep: A systematic review. Environ. Res. 2019, 182, 109081. [Google Scholar] [CrossRef] [PubMed]
- Kakar, E.; Venema, E.; Jeekel, J.; Klimek, M.; van der Jagt, M. Music intervention for sleep quality in critically ill and surgical patients: A meta-analysis. BMJ Open 2021, 11, e042510. [Google Scholar] [CrossRef] [PubMed]
- Feng, F.; Zhang, Y.; Hou, J.; Cai, J.; Jiang, Q.; Li, X.; Zhao, Q.; Li, B.-A. Can music improve sleep quality in adults with primary insomnia? A systematic review and network meta-analysis. Int. J. Nurs. Stud. 2018, 77, 189–196. [Google Scholar] [CrossRef]
- Han, J.-W.; Choi, H.; Jeon, Y.-H.; Yoon, C.-H.; Woo, J.-M.; Kim, W. The Effects of Forest Therapy on Coping with Chronic Widespread Pain: Physiological and Psychological Differences between Participants in a Forest Therapy Program and a Control Group. Int. J. Environ. Res. Public Health 2016, 13, 255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chanda, M.L.; Levitin, D.J. The neurochemistry of music. Trends Cogn. Sci. 2013, 17, 179–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deng, L.; Deng, Q. The basic roles of indoor plants in human health and comfort. Environ. Sci. Pollut. Res. 2018, 25, 36087–36101. [Google Scholar] [CrossRef]
- Dijkstra, K.; Pieterse, M.; Pruyn, A. Stress-reducing effects of indoor plants in the built healthcare environment: The mediating role of perceived attractiveness. Prev. Med. 2008, 47, 279–283. [Google Scholar] [CrossRef]
- Jiang, S.; Deng, L.; Luo, H.; Li, X.; Guo, B.; Jiang, M.; Jia, Y.; Ma, J.; Sun, L.; Huang, Z. Effect of Fragrant Primula Flowers on Physiology and Psychology in Female College Students: An Empirical Study. Front. Psychol. 2021, 12, 437. [Google Scholar] [CrossRef]
- Song, C.; Igarashi, M.; Ikei, H.; Miyazaki, Y. Physiological effects of viewing fresh red roses. Complement. Ther. Med. 2017, 35, 78–84. [Google Scholar] [CrossRef]
- Ikei, H.; Komatsu, M.; Song, C.; Himoro, E.; Miyazaki, Y. The physiological and psychological relaxing effects of viewing rose flowers in office workers. J. Physiol. Anthr. 2014, 33, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mochizuki-Kawai, H.; Matsuda, I.; Mochizuki, S. Viewing a flower image provides automatic recovery effects after psychological stress. J. Environ. Psychol. 2020, 70, 101445. [Google Scholar] [CrossRef]
- Jo, H.; Song, C.; Miyazaki, Y. Physiological Benefits of Viewing Nature: A Systematic Review of Indoor Experiments. Int. J. Environ. Res. Public Health 2019, 16, 4739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, J.; Arfaei, N.; Macnaughton, P.; Catalano, P.J.; Allen, J.G.; Spengler, J.D. Effects of biophilic interventions in office on stress reaction and cognitive function: A randomized crossover study in virtual reality. Indoor Air 2019, 29, 1028–1039. [Google Scholar] [CrossRef] [PubMed]
- Ikei, H.; Song, C.; Miyazaki, Y. Physiological Effects of Touching Wood. Int. J. Environ. Res. Public Health. 2017, 14, 801. [Google Scholar] [CrossRef]
- Ikei, H.; Song, C.; Miyazaki, Y. Physiological Effects of Touching Coated Wood. Int. J. Environ. Res. Public Health 2017, 14, 773. [Google Scholar] [CrossRef] [Green Version]
- Walch, J.M.; Rabin, B.S.; Day, R.; Williams, J.N.; Choi, K.; Kang, J.D. The Effect of Sunlight on Postoperative Analgesic Medication Use: A Prospective Study of Patients Undergoing Spinal Surgery. Psychosom. Med. 2005, 67, 156–163. [Google Scholar] [CrossRef]
- Peroutka, S.J. What Turns on a Migraine? A Systematic Review of Migraine Precipitating Factors. Curr. Pain Headache Rep. 2014, 18, 1–6. [Google Scholar] [CrossRef]
- Probyn, K.; Bowers, H.; Mistry, D.; Caldwell, F.; Underwood, M.; Patel, S.; Sandhu, H.K.; Matharu, M.; Pincus, T.; On Behalf of the CHESS Team. Non-pharmacological self-management for people living with migraine or tension-type headache: A systematic review including analysis of intervention components. BMJ Open 2017, 7, e016670. [Google Scholar] [CrossRef] [Green Version]
- Robblee, J.; Starling, A.J. SEEDS for success: Lifestyle management in migraine. Clevel. Clin. J. Med. 2019, 86, 741–749. [Google Scholar] [CrossRef]
- Martin, L.F.; Patwardhan, A.M.; Jain, S.V.; Salloum, M.M.; Freeman, J.; Khanna, R.; Gannala, P.; Goel, V.; Jones-MacFarland, F.N.; Killgore, W.D.; et al. Evaluation of green light exposure on headache frequency and quality of life in migraine patients: A preliminary one-way cross-over clinical trial. Cephalalgia 2020, 41, 135–147. [Google Scholar] [CrossRef] [PubMed]
- Yuan, R.; Zhang, D.; Yang, J.; Wu, Z.; Luo, C.; Han, L.; Yang, F.; Lin, J.; Yang, M. Review of aromatherapy essential oils and their mechanism of action against migraines. J. Ethnopharmacol. 2020, 265, 113326. [Google Scholar] [CrossRef] [PubMed]
- Toda, M.; Matsuse, R. Endocrinological effect of lavender aromatherapy on stressful visual stimuli. Contemp. Clin. Trials Commun. 2020, 17, 100547. [Google Scholar] [CrossRef] [PubMed]
- Donelli, D.; Antonelli, M.; Bellinazzi, C.; Gensini, G.F.; Firenzuoli, F. Effects of lavender on anxiety: A systematic review and meta-analysis. Phytomedicine 2019, 65, 153099. [Google Scholar] [CrossRef]
- López, V.; Nielsen, B.; Solas, M.; Ramírez, M.J.; Jäger, A.K. Exploring Pharmacological Mechanisms of Lavender (Lavandula angustifolia) Essential Oil on Central Nervous System Targets. Front. Pharmacol. 2017, 8, 280. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, M.; Barbieri, G.; Donelli, D. Effects of forest bathing (shinrin-yoku) on levels of cortisol as a stress biomarker: A systematic review and meta-analysis. Int. J. Biometeorol. 2019, 63, 1117–1134. [Google Scholar] [CrossRef]
- Stier-Jarmer, M.; Throner, V.; Kirschneck, M.; Immich, G.; Frisch, D.; Schuh, A. The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses. Int. J. Environ. Res. Public Health 2021, 18, 1770. [Google Scholar] [CrossRef]
- Stigsdotter, U.K.; Corazon, S.S.; Sidenius, U.; Nyed, P.K.; Larsen, H.B.; Fjorback, L.O. Efficacy of nature-based therapy for individuals with stress-related illnesses: Randomised controlled trial. Br. J. Psychiatry 2018, 213, 404–411. [Google Scholar] [CrossRef]
- Shuda, Q.; Bougoulias, M.E.; Kass, R. Effect of nature exposure on perceived and physiologic stress: A systematic review. Complement. Ther. Med. 2020, 53, 102514. [Google Scholar] [CrossRef]
- Sasannejad, P.; Saeedi, M.; Shoeibi, A.; Gorji, A.; Abbasi, M.; Foroughipour, M. Lavender Essential Oil in the Treatment of Migraine Headache: A Placebo-Controlled Clinical Trial. Eur. Neurol. 2012, 67, 288–291. [Google Scholar] [CrossRef]
- Hasanpour-Dehkordi, A.; Rafieian-Kopaei, M.; Lorigooini, Z.; Deris, F.; Solati, K.; Mahdiyeh, F. Comparing the effect of intranasal lidocaine 4% with peppermint essential oil drop 1.5% on migraine attacks: A double-blind clinical trial. Int. J. Prev. Med. 2019, 10, 121. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, P.J.; Lumley, M.A.; Kraft, C.A.; Dooley, J.A. Relaxation Training and Written Emotional Disclosure for Tension or Migraine Headaches: A Randomized, Controlled Trial. Ann. Behav. Med. 2008, 36, 21–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wells, R.E.; O’Connell, N.; Pierce, C.R.; Estave, P.; Penzien, D.B.; Loder, E.; Zeidan, F.; Houle, T.T. Effectiveness of Mindfulness Meditation vs Headache Education for Adults With Migraine. JAMA Intern. Med. 2021, 181, 317–328. [Google Scholar] [CrossRef] [PubMed]
- Wells, R.E.; Seng, E.K.; Edwards, R.R.; Victorson, D.E.; Pierce, C.R.; Rosenberg, L.; Napadow, V.; Schuman-Olivier, Z. Mindfulness in migraine: A narrative review. Expert Rev. Neurother. 2020, 20, 207–225. [Google Scholar] [CrossRef] [PubMed]
- Ha, H.; Gonzalez, A. Migraine headache prophylaxis. Am. Fam. Physician 2019, 99, 17–24. [Google Scholar] [PubMed]
- Kumar, A.; Bhatia, R.; Sharma, G.; Dhanlika, D.; Vishnubhatla, S.; Singh, R.K.; Dash, D.; Tripathi, M.; Srivastava, M.P. Effect of yoga as add-on therapy in migraine (CONTAIN). Neurology 2020, 94, e2203–e2212. [Google Scholar] [CrossRef]
- Rains, J.C. Sleep and Migraine: Assessment and Treatment of Comorbid Sleep Disorders. Headache J. Head Face Pain 2018, 58, 1074–1091. [Google Scholar] [CrossRef]
- Smitherman, T.A.; Walters, A.B.; Davis, R.E.; Ambrose, C.E.; Roland, M.; Houle, T.; Rains, J.C. Randomized Controlled Pilot Trial of Behavioral Insomnia Treatment for Chronic Migraine With Comorbid Insomnia. Headache J. Head Face Pain 2016, 56, 276–291. [Google Scholar] [CrossRef]
- Calhoun, A.H.; Ford, S. Behavioral Sleep Modification May Revert Transformed Migraine to Episodic Migraine. Headache J. Head Face Pain 2007, 47, 1178–1183. [Google Scholar] [CrossRef]
- Von Luckner, A.; Riederer, F. Magnesium in Migraine Prophylaxis-Is There an Evidence-Based Rationale? A Systematic Review. Headache J. Head Face Pain 2017, 58, 199–209. [Google Scholar] [CrossRef]
- Kirkland, A.; Sarlo, G.L.; Holton, K.F. The Role of Magnesium in Neurological Disorders. Nutrients 2018, 10, 730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maghbooli, M.; Golipour, F.; Esfandabadi, A.M.; Yousefi, M. Comparison Between the Efficacy of Ginger and Sumatriptan in the Ablative Treatment of the Common Migraine. Phytotherapy Res. 2013, 28, 412–415. [Google Scholar] [CrossRef] [PubMed]
- Haviland-Jones, J.; Rosario, H.H.; Wilson, P.; McGuire, T.R. An Environmental Approach to Positive Emotion: Flowers. Evol. Psychol. 2005, 3. [Google Scholar] [CrossRef]
- Micheletti, J.K.; Bláfoss, R.; Sundstrup, E.; Bay, H.; Pastre, C.M.; Andersen, L.L. Association between lifestyle and musculoskeletal pain: Cross-sectional study among 10,000 adults from the general working population. BMC Musculoskelet. Disord. 2019, 20, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshimoto, T.; Ochiai, H.; Shirasawa, T.; Nagahama, S.; Uehara, A.; Muramatsu, J.; Kokaze, A. Clustering of Lifestyle Factors and Its Association with Low Back Pain: A Cross-Sectional Study of Over 400,000 Japanese Adults. J. Pain Res. 2020, 13, 1411–1419. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Wilt, T.J.; McLean, R.M.; Forciea, M.A.; for the Clinical Guidelines Committee of the American College of Physicians. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline from the American College of Physicians. Ann. Intern. Med. 2017, 166, 514–530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, V.X.; Oomens, P.; Klimek, M.; Verhofstad, M.H.J.; Jeekel, J. The Effect of Perioperative Music on Medication Requirement and Hospital Length of Stay. Ann. Surg. 2019, 272, 961–972. [Google Scholar] [CrossRef]
- Hole, J.; Hirsch, M.; Ball, E.; Meads, C. Music as an aid for postoperative recovery in adults: A systematic review and meta-analysis. Lancet 2015, 386, 1659–1671. [Google Scholar] [CrossRef]
- Stanhope, J.; Breed, M.F.; Weinstein, P. Exposure to greenspaces could reduce the high global burden of pain. Environ. Res. 2020, 187, 109641. [Google Scholar] [CrossRef]
- Burns, J.W.; Gerhart, J.; Rizvydeen, M.; Kimura, M.; Burgess, H.J. Morning Bright Light Treatment for Chronic Low Back Pain: Potential Impact on the Volatility of Pain, Mood, Function, and Sleep. Pain Med. 2019, 21, 1153–1161. [Google Scholar] [CrossRef]
- Burgess, H.J.; Rizvydeen, M.; Kimura, M.; Pollack, M.H.; Hobfoll, E.S.; Rajan, K.B.; Burns, J.W. An Open Trial of Morning Bright Light Treatment Among US Military Veterans with Chronic Low Back Pain: A Pilot Study. Pain Med. 2018, 20, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Burgess, H.J.; Park, M.; Ong, J.C.; Shakoor, N.; Williams, D.A.; Burns, J. Morning Versus Evening Bright Light Treatment at Home to Improve Function and Pain Sensitivity for Women with Fibromyalgia: A Pilot Study. Pain Med. 2016, 18, 116–123. [Google Scholar] [CrossRef] [Green Version]
- Martin, L.; Porreca, F.; Mata, E.I.; Salloum, M.; Goel, V.; Gunnala, P.; Killgore, W.D.S.; Jain, S.; Jones-MacFarland, F.N.; Khanna, R.; et al. Green Light Exposure Improves Pain and Quality of Life in Fibromyalgia Patients: A Preliminary One-Way Crossover Clinical Trial. Pain Med. 2021, 22, 118–130. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Hwang, S.; Jiang, P.; Hsiung, N. Effect of Music Therapy on Pain After Orthopedic Surgery—A Systematic Review and Meta-Analysis. Pain Pr. 2020, 20, 422–436. [Google Scholar] [CrossRef] [PubMed]
- Garza-Villarreal, E.A.; Wilson, A.D.; Vase, L.; Brattico, E.; Barrios, F.A.; Jensen, T.S.T.; Romero-Romo, J.I.; Vuust, P. Music reduces pain and increases functional mobility in fibromyalgia. Front. Psychol. 2014, 5, 90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, B.E.; Bliven, K.C.H. The Use of Breathing Exercises in the Treatment of Chronic, Nonspecific Low Back Pain. J. Sport Rehabil. 2017, 26, 452–458. [Google Scholar] [CrossRef]
- Hilton, L.; Hempel, S.; Ewing, B.A.; Apaydin, E.; Xenakis, L.; Newberry, S.; Colaiaco, B.; Maher, A.R.; Shanman, R.M.; Sorbero, M.E.; et al. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Ann. Behav. Med. 2016, 51, 199–213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeidan, F.; Vago, D. Mindfulness meditation-based pain relief: A mechanistic account. Ann. N. Y. Acad. Sci. 2016, 1373, 114–127. [Google Scholar] [CrossRef]
- Gerhart, J.I.; Burns, J.W.; Post, K.M.; Smith, D.A.; Porter, L.S.; Burgess, H.J.; Schuster, E.; Buvanendran, A.; Fras, A.M.; Keefe, F.J. Relationships Between Sleep Quality and Pain-Related Factors for People with Chronic Low Back Pain: Tests of Reciprocal and Time of Day Effects. Ann. Behav. Med. 2016, 51, 365–375. [Google Scholar] [CrossRef]
- Burgess, H.J.; Burns, J.W.; Buvanendran, A.; Gupta, R.; Chont, M.; Kennedy, M.; Bruehl, S. Associations Between Sleep Disturbance and Chronic Pain Intensity and Function. Clin. J. Pain 2019, 35, 569–576. [Google Scholar] [CrossRef]
- Serrat, M.; Almirall, M.; Musté, M.; Sanabria-Mazo, J.P.; Feliu-Soler, A.; Méndez-Ulrich, J.L.; Luciano, J.V.; Sanz, A. Effectiveness of a multicomponent treatment for fibromyalgia based on pain neuroscience education, exercise therapy, psychological support, and nature exposure (nat-fm): A pragmatic randomized controlled trial. J. Clin. Med. 2020, 9, 3348. [Google Scholar] [CrossRef] [PubMed]
- Verkaik, R.; Busch, M.; Koeneman, T.; Berg, R.V.D.; Spreeuwenberg, P.; Francke, A.L. Guided imagery in people with fibromyalgia: A randomized controlled trial of effects on pain, functional status and self-efficacy. J. Health Psychol. 2013, 19, 678–688. [Google Scholar] [CrossRef] [PubMed]
- Torres, E.; Pedersen, I.N.; Pérez-Fernández, I.J. Randomized Trial of a Group Music and Imagery Method (GrpMI) for Women with Fibromyalgia. J. Music Ther. 2018, 55, 186–220. [Google Scholar] [CrossRef] [PubMed]
- Polaski, A.M.; Phelps, A.L.; Smith, T.J.; Helm, E.R.; Morone, E.N.; Szucs, A.K.; Kostek, M.C.; Kolber, B.J. Integrated Meditation and Exercise Therapy: A Randomized Controlled Pilot of a Combined Nonpharmacological Intervention Focused on Reducing Disability and Pain in Patients with Chronic Low Back Pain. Pain Med. 2021, 22, 444–458. [Google Scholar] [CrossRef]
- Kahn, P.H., Jr.; Friedman, B.; Gill, B.; Hagman, J.; Severson, R.L.; Freier, N.G.; Feldman, E.N.; Carrère, S.; Stolyar, A. A plasma display window?—The shifting baseline problem in a technologically mediated natural world. J. Environ. Psychol. 2008, 28, 192–199. [Google Scholar] [CrossRef]
- Craighead, W.E.; Dunlop, B.W. Combination Psychotherapy and Antidepressant Medication Treatment for Depression: For Whom, When, and How. Annu. Rev. Psychol. 2014, 65, 267–300. [Google Scholar] [CrossRef]
- Hawton, K.; i Comabella, C.C.; Haw, C.; Saunders, K. Risk factors for suicide in individuals with depression: A systematic review. J. Affect. Disord. 2013, 147, 17–28. [Google Scholar] [CrossRef]
- Alexopoulos, G.S. Depression in the elderly. Lancet 2005, 365, 1961–1970. [Google Scholar] [CrossRef]
- Sarris, J.; O’Neil, A.; Coulson, C.E.; Schweitzer, I.; Berk, M. Lifestyle medicine for depression. BMC Psychiatry 2014, 14, 107. [Google Scholar] [CrossRef] [Green Version]
- Zhang, R.; Zhang, C.-Q.; Rhodes, R.E. The pathways linking objectively-measured greenspace exposure and mental health: A systematic review of observational studies. Environ. Res. 2021, 198, 111233. [Google Scholar] [CrossRef]
- Oh, B.; Lee, K.J.; Zaslawski, C.; Yeung, A.; Rosenthal, D.; Larkey, L.; Back, M. Health and well-being benefits of spending time in forests: Systematic review. Environ. Health Prev. Med. 2017, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bratman, G.N.; Hamilton, J.P.; Daily, G.C. The impacts of nature experience on human cognitive function and mental health. Ann. N. Y. Acad. Sci. 2012, 1249, 118–136. [Google Scholar] [CrossRef] [PubMed]
- Hirakawa, H.; Terao, T.; Muronaga, M.; Ishii, N. Adjunctive bright light therapy for treating bipolar depression: A systematic review and meta-analysis of randomized controlled trials. Brain Behav. 2020, 10, e01876. [Google Scholar] [CrossRef]
- Braçe, O.; Garrido-Cumbrera, M.; Foley, R.; Correa-Fernández, J.; Suárez-Cáceres, G.; Lafortezza, R. Is a View of Green Spaces from Home Associated with a Lower Risk of Anxiety and Depression? Int. J. Environ. Res. Public Health 2020, 17, 7014. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, M.; Wendel-Vos, W.; van Poppel, M.; Kemper, H.; van Mechelen, W.; Maas, J. Health benefits of green spaces in the living environment: A systematic review of epidemiological studies. Urban For. Urban Greening 2015, 14, 806–816. [Google Scholar] [CrossRef]
- Yao, W.; Chen, F.; Wang, S.; Zhang, X. Impact of Exposure to Natural and Built Environments on Positive and Negative Affect: A Systematic Review and Meta-Analysis. Front. Public Health. 2021, 9. [Google Scholar] [CrossRef]
- Mcmahan, E.A.; Estes, D. The effect of contact with natural environments on positive and negative affect: A meta-analysis. J. Posit. Psychol. 2015, 10, 507–519. [Google Scholar] [CrossRef]
- Perera, S.; Eisen, R.; Bhatt, M.; Bhatnagar, N.; de Souza, R.; Thabane, L.; Samaan, Z. Light therapy for non-seasonal depression: Systematic review and meta-analysis. BJPsych Open 2016, 2, 116–126. [Google Scholar] [CrossRef] [Green Version]
- Tao, L.; Jiang, R.; Zhang, K.; Qian, Z.; Chen, P.; Lv, Y.; Yao, Y. Light therapy in non-seasonal depression: An update meta-analysis. Psychiatry Res. 2020, 291, 113247. [Google Scholar] [CrossRef]
- Lam, R.W. Morning light therapy for winter depression: Predictors of response. Acta Psychiatr. Scand. 1994, 89, 97–101. [Google Scholar] [CrossRef]
- Pjrek, E.; Friedrich, M.-E.; Cambioli, L.; Dold, M.; Jäger, F.; Komorowski, A.; Lanzenberger, R.; Kasper, S.; Winkler, D. The Efficacy of Light Therapy in the Treatment of Seasonal Affective Disorder: A Meta-Analysis of Randomized Controlled Trials. Psychother. Psychosom. 2019, 89, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Srisurapanont, K.; Samakarn, Y.; Kamklong, B.; Siratrairat, P.; Bumiputra, A.; Jaikwang, M.; Srisurapanont, M. Blue-wavelength light therapy for post-traumatic brain injury sleepiness, sleep disturbance, depression, and fatigue: A systematic review and network meta-analysis. PLoS ONE 2021, 16, e0246172. [Google Scholar] [CrossRef] [PubMed]
- Cooney, G.M.; Dwan, K.; Greig, C.; Lawlor, A.D.; Rimer, J.; Waugh, F.R.; McMurdo, M.; Mead, E.G. Exercise for depression. Cochrane Database Syst. Rev. 2013, CD004366. [Google Scholar] [CrossRef]
- Gujral, S.; Aizenstein, H.; Reynolds, C.F., III; Butters, M.A.; Erickson, K.I. Exercise effects on depression: Possible neural mechanisms. Gen. Hosp. Psychiatry 2017, 49, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Kandola, A.; Ashdown-Franks, G.; Hendrikse, J.; Sabiston, C.M.; Stubbs, B. Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neurosci. Biobehav. Rev. 2019, 107, 525–539. [Google Scholar] [CrossRef] [PubMed]
- Brinsley, J.; Schuch, F.; Lederman, O.; Girard, D.; Smout, M.; Immink, A.M.; Stubbs, B.; Firth, J.; Davison, K.; Rosenbaum, S. Effects of yoga on depressive symptoms in people with mental disorders: A systematic review and meta-analysis. Br. J. Sports Med. 2020, 55, 992–1000. [Google Scholar] [CrossRef]
- Long, J.; Briggs, M.; Astin, F. Overview of Systematic Reviews of Mindfulness Meditation-based Interventions for People With Long-term Conditions. Adv. Mind-Body Med. 2018, 31, 26–36. [Google Scholar]
- Alsaraireh, F.A.; Aloush, S.M. Mindfulness Meditation Versus Physical Exercise in the Management of Depression Among Nursing Students. J. Nurs. Educ. 2017, 56, 599–604. [Google Scholar] [CrossRef]
- Sharma, A.; Barrett, M.S.; Cucchiara, A.J.; Gooneratne, N.S.; Thase, M.E. A Breathing-Based Meditation Intervention for Patients With Major Depressive Disorder Following Inadequate Response to Antidepressants. J. Clin. Psychiatry 2016, 78, e59–e63. [Google Scholar] [CrossRef] [Green Version]
- Zaccaro, A.; Piarulli, A.; Laurino, M.; Garbella, E.; Menicucci, D.; Neri, B.; Gemignani, A. How Breath-Control Can Change Your Life: A Systematic Review on Psycho-Physiological Correlates of Slow Breathing. Front. Hum. Neurosci. 2018, 12, 353. [Google Scholar] [CrossRef] [Green Version]
- Srivastava, A.; Kuppili, P.P.; Gupta, T.; Nebhinani, N.; Chandani, A. Kriya Yoga in Patients with Depressive Disorders: A Pilot Study. J. Neurosci. Rural Pr. 2021, 12, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Vidaña, D.I.; Ngai, S.P.; He, W.; Chow, J.K.-W.; Lau, B.W.-M.; Tsang, H.W. The Effectiveness of Aromatherapy for Depressive Symptoms: A Systematic Review. Evid.-Based Complement. Altern. Med. 2017, 2017, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Baglioni, C.; Battagliese, G.; Feige, B.; Spiegelhalder, K.; Nissen, C.; Voderholzer, U.; Lombardo, C.; Riemann, D. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011, 135, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Monteleone, P.; Martiadis, V.; Maj, M. Circadian rhythms and treatment implications in depression. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2011, 35, 1569–1574. [Google Scholar] [CrossRef]
- Ng, Q.X.; Venkatanarayanan, N.; Ho, C.Y.X. Clinical use of Hypericum perforatum (St John’s wort) in depression: A meta-analysis. J. Affect. Disord. 2017, 210, 211–221. [Google Scholar] [CrossRef]
- Apaydin, E.A.; Maher, A.R.; Shanman, R.; Booth, M.S.; Miles, J.N.V.; Sorbero, M.E.; Hempel, S. A systematic review of St. John’s wort for major depressive disorder. Syst. Rev. 2016, 5, 148. [Google Scholar] [CrossRef] [Green Version]
- Psaltopoulou, T.; Sergentanis, T.N.; Panagiotakos, D.B.; Sergentanis, I.N.; Kosti, R.; Scarmeas, N. Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann. Neurol. 2013, 74, 580–591. [Google Scholar] [CrossRef]
- Klainin-Yobas, P.; Oo, W.N.; Yew, P.Y.S.; Lau, Y. Effects of relaxation interventions on depression and anxiety among older adults: A systematic review. Aging Ment. Health 2015, 19, 1043–1055. [Google Scholar] [CrossRef]
- Xiao, P.; Ding, S.; Duan, Y.; Li, L.; Zhou, Y.; Luo, X.; Xie, J.; Cheng, A.S. Effect of Light Therapy on Cancer-Related Fatigue: A Systematic Review and Meta-Analysis. J. Pain Symptom Manag. 2021, 63, e188–e202. [Google Scholar] [CrossRef]
- Lindskov, F.O.; Iversen, H.K.; West, A.S. Clinical outcomes of light therapy in hospitalized patients—A systematic review. Chrono.-Int. 2021, 39, 299–310. [Google Scholar] [CrossRef]
- Cheng, K.; Martin, L.F.; Slepian, M.J.; Patwardhan, A.M.; Ibrahim, M.M. Mechanisms and Pathways of Pain Photobiomodulation: A Narrative Review. J. Pain 2021, 22, 763–777. [Google Scholar] [CrossRef] [PubMed]
- Connolly, L.J.; Ponsford, J.L.; Rajaratnam, S.M.W.; Lockley, S.W. Development of a Home-Based Light Therapy for Fatigue Following Traumatic Brain Injury: Two Case Studies. Front. Neurol. 2021, 12, 1559. [Google Scholar] [CrossRef] [PubMed]
- Connolly, L.J.; Rajaratnam, S.M.W.; Murray, J.M.; Spitz, G.; Lockley, S.W.; Ponsford, J.L. Home-based light therapy for fatigue following acquired brain injury: A pilot randomized controlled trial. BMC Neurol. 2021, 21, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Tähkämö, L.; Partonen, T.; Pesonen, A.-K. Systematic review of light exposure impact on human circadian rhythm. Chronobiol. Int. 2019, 36, 151–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shechter, A.; Kim, E.W.; St-Onge, M.-P.; Westwood, A.J. Blocking nocturnal blue light for insomnia: A randomized controlled trial. J. Psychiatr. Res. 2017, 96, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Baglioni, C.; Nanovska, S.; Regen, W.; Spiegelhalder, K.; Feige, B.; Nissen, C.; Reynolds, C.F.; Riemann, D. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol. Bull. 2016, 142, 969–990. [Google Scholar] [CrossRef]
- Leff, B. Defining and disseminating the hospital-at-home model. Can. Med Assoc. J. 2009, 180, 156–157. [Google Scholar] [CrossRef] [Green Version]
- Martin, K.; Nanu, L.; Kwon, W.-S.; Martin, D. Small Garden, Big Impact: Emotional and Behavioral Responses of Visitors to a Rooftop Atrium in a Major Hospital. HERD: Heal. Environ. Res. Des. J. 2021, 14, 274–287. [Google Scholar] [CrossRef]
- Totaforti, S. Applying the benefits of biophilic theory to hospital design. City Territ. Arch. 2018, 5, 1. [Google Scholar] [CrossRef]
- Abdelaal, M.S.; Soebarto, V. Biophilia and Salutogenesis as restorative design approaches in healthcare architecture. Arch. Sci. Rev. 2019, 62, 195–205. [Google Scholar] [CrossRef]
- Ibrahim, T.; Gabr, H.; Khodeir, L.; Aboubakr, D. Synergetic approach for biophilic healing interior design for paediatric cancer. J. Eng. Appl. 2020, 67, 1435–1453. [Google Scholar]
- Miller, E.; Burton, L.O. Redesigning aged care with a biophilic lens: A call to action. Cities Health 2020, 1–13. [Google Scholar] [CrossRef]
- Taylor, S.P.; Golding, L. Economic Considerations for Hospital at Home Programs: Beyond the Pandemic. J. Gen. Intern. Med. 2021, 36, 3861–3864. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.M.; Ouchi, K.; Blanchfield, B.; Saenz, A.; Burke, K.; Paz, M.; Diamond, K.; Pu, C.T.; Schnipper, J.L. Hospital-Level Care at Home for Acutely Ill Adults. Ann. Intern. Med. 2019, 172, 77. [Google Scholar] [CrossRef] [PubMed]
- McGee, B.; Park, N.; Portillo, M.; Bosch, S.; Swisher, M. Diy Biophilia: Development of the Biophilic Interior Design Matrix as a Design Tool. J. Inter. Des. 2019, 44, 201–221. [Google Scholar] [CrossRef]
- McGee, B.; Park, N.-K. Colour, Light, and Materiality: Biophilic Interior Design Presence in Research and Practice. Interiority 2022, 5, 27–52. [Google Scholar] [CrossRef]
- Noser, E.A.; Klages, K.L.; Gamwell, K.L.; Brammer, C.N.; Hommel, A.K.; Ramsey, R.R. A systematic evaluation of primary headache management apps leveraging behavior change techniques. Cephalalgia 2021. [Google Scholar] [CrossRef]
- Hommel, K.A.; Carmody, J.; Hershey, A.D.; Holbein, C.; Kabbouche-Samaha, M.; Peugh, J.; Powers, S. Digital Therapeutic Self-Management Intervention in Adolescents With Migraine: Feasibility and Preliminary Efficacy of “Migraine Manager”. Headache: J. Head Face Pain 2020, 60, 1103–1110. [Google Scholar] [CrossRef]
- Rubin, R. Virtual Reality Device Is Authorized to Relieve Back Pain. JAMA 2021, 326, 2354. [Google Scholar] [CrossRef]
- Garcia, L.M.; Birckhead, B.J.; Krishnamurthy, P.; Sackman, J.; Mackey, I.G.; Louis, R.G.; Salmasi, V.; Maddox, T.; Darnall, B.D. An 8-Week Self-Administered At-Home Behavioral Skills-Based Virtual Reality Program for Chronic Low Back Pain: Double-Blind, Randomized, Placebo-Controlled Trial Conducted During COVID-19. J. Med. Internet Res. 2021, 23, e26292. [Google Scholar] [CrossRef]
- Moshe, I.; Terhorst, Y.; Philippi, P.; Domhardt, M.; Cuijpers, P.; Cristea, I.; Pulkki-Råback, L.; Baumeister, H.; Sander, L.B. Digital interventions for the treatment of depression: A meta-analytic review. Psychol. Bull. 2021, 147, 749–786. [Google Scholar] [CrossRef] [PubMed]
- Moberg, C.; Niles, A.; Beermann, D. Guided Self-Help Works: Randomized Waitlist Controlled Trial of Pacifica, a Mobile App Integrating Cognitive Behavioral Therapy and Mindfulness for Stress, Anxiety, and Depression. J. Med. Internet Res. 2019, 21, e12556. [Google Scholar] [CrossRef] [PubMed] [Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huntsman, D.D.; Bulaj, G. Healthy Dwelling: Design of Biophilic Interior Environments Fostering Self-Care Practices for People Living with Migraines, Chronic Pain, and Depression. Int. J. Environ. Res. Public Health 2022, 19, 2248. https://doi.org/10.3390/ijerph19042248
Huntsman DD, Bulaj G. Healthy Dwelling: Design of Biophilic Interior Environments Fostering Self-Care Practices for People Living with Migraines, Chronic Pain, and Depression. International Journal of Environmental Research and Public Health. 2022; 19(4):2248. https://doi.org/10.3390/ijerph19042248
Chicago/Turabian StyleHuntsman, Dorothy Day, and Grzegorz Bulaj. 2022. "Healthy Dwelling: Design of Biophilic Interior Environments Fostering Self-Care Practices for People Living with Migraines, Chronic Pain, and Depression" International Journal of Environmental Research and Public Health 19, no. 4: 2248. https://doi.org/10.3390/ijerph19042248
APA StyleHuntsman, D. D., & Bulaj, G. (2022). Healthy Dwelling: Design of Biophilic Interior Environments Fostering Self-Care Practices for People Living with Migraines, Chronic Pain, and Depression. International Journal of Environmental Research and Public Health, 19(4), 2248. https://doi.org/10.3390/ijerph19042248






