Influence of “Face-to-Face Contact” and “Non-Face-to-Face Contact” on the Subsequent Decline in Self-Rated Health and Mental Health Status of Young, Middle-Aged, and Older Japanese Adults: A Two-Year Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
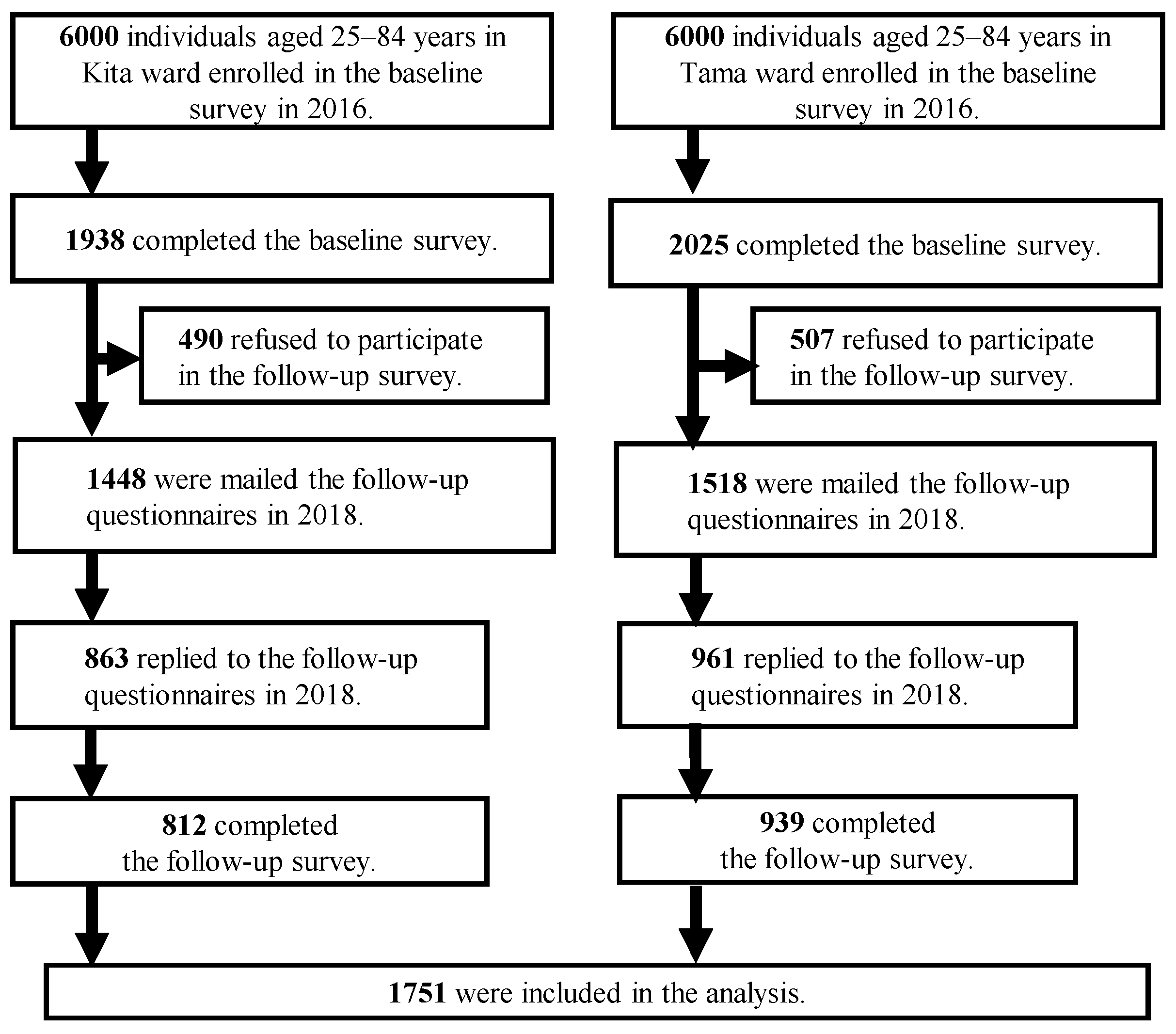
2.1. Study Area and Participants
2.2. Measures and Analysis Strategy
2.3. Statistical Methods
3. Results
4. Discussion
4.1. Cross-Sectional and Longitudinal Association of Social Contact with Self-Rated Health
4.2. Cross-Sectional and Longitudinal Association of Social Contact with Mental Health
4.3. Limitations and Strength
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef] [PubMed]
- McDonald, M. In Japan, Lonely Deaths in Society’s Margins. The New York Times. 5 March 2012. Available online: https://rendezvous.blogs.nytimes.com/2012/03/25/in-japan-lonely-deaths-in-societys-margins/ (accessed on 12 January 2022).
- Kato, T.A.; Kanba, S.; Teo, A.R. Hikikomori: Multidimensional understanding, assessment, and future international perspectives. Psychiatry Clin. Neurosci. 2019, 73, 427–440. [Google Scholar] [CrossRef] [PubMed]
- Japan Cabinet Office. Wakamono no Seikatsu ni Kansuru Chousa-Houkokusho. Investigation on Life of Youth. 2016. Available online: https://www8.cao.go.jp/youth/kenkyu/hikikomori/h27/pdf/teigi.pdf (accessed on 12 January 2022). (In Japanese)
- Hämmig, O. Health risks associated with social isolation in general and in young, middle and old age. PLoS ONE 2019, 14, e0219663. [Google Scholar] [CrossRef] [Green Version]
- Berkman, L.F.; Melchior, M.; Chastang, J.F.; Niedhammer, I.; Leclerc, A.; Goldberg, M. Social integration and mortality: A prospective study of French employees of Electricity of France-Gas of France: The GAZEL Cohort. Am. J. Epidemiol. 2004, 159, 167–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horsten, M.; Mittleman, M.A.; Wamala, S.P.; Schenck-Gustafsson, K.; Orth-Gome’r, K. Depressive symptoms and lack of social integration in relation to prognosis of CHD in middle-aged women. The Stockholm Female Coronary Risk Study. Eur. Heart J. 2000, 21, 1072–1080. [Google Scholar] [CrossRef]
- Townsend, P. The Family Life of Old People: An Inquiry in East London; Oxford University Press: Oxford, UK, 1963; pp. 188–205. [Google Scholar]
- Saito, M.; Fujiwara, Y.; Kobayashi, E.; Fukaya, T.; Nishi, M.; Shinkai, S. Prevalence and characteristics of social isolation in the elderly in a dormitory suburb according to household composition. Nihon Koshu Eisei Zasshi 2010, 57, 785–795. [Google Scholar] [PubMed]
- Saito, M.; Kondo, K.; Ojima, T.; Hirai, H.; JAGES Group. Criteria for social isolation based on associations with health indicators among older people-A 10-year follow-up of the Aichi Gerontological Evaluation Study. Nihon Koshu Eisei Zasshi 2015, 62, 95–105. [Google Scholar] [CrossRef]
- Fujiwara, Y.; Nishi, M.; Fukaya, T.; Hasebe, M.; Nonaka, K.; Koike, T.; Suzuki, H.; Murayama, Y.; Saito, M.; Kobayashi, E. Synergistic or independent impacts of low frequency of going outside the home and social isolation on functional decline: A 4-year prospective study of urban Japanese older adults. Geriatr. Gerontol. Int. 2017, 17, 500–508. [Google Scholar] [CrossRef]
- Sakurai, R.; Yasunaga, M.; Nishi, M.; Fukaya, T.; Hasebe, M.; Murayama, Y.; Koike, T.; Matsunaga, H.; Nonaka, K.; Suzuki, H.; et al. Co-existence of social isolation and homebound status increase the risk of all-cause mortality. Int. Psychogeriatr. 2019, 31, 703–711. [Google Scholar] [CrossRef]
- Saito, M.; Aida, J.; Cable, N.; Zaninotto, P.; Ikeda, T.; Tsuji, T.; Koyama, S.; Noguchi, T.; Osaka, K.; Kondo, K. Cross-national comparison of social isolation and mortality among older adults: A 10-year follow-up study in Japan and England. Geriatr. Gerontol. Int. 2021, 21, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Noguchi, T.; Saito, M.; Aida, J.; Cable, N.; Tsuji, T.; Koyama, S.; Ikeda, T.; Osaka, K.; Kondo, K. Association between social isolation and depression onset among older adults: A cross-national longitudinal study in England and Japan. BMJ Open 2021, 11, e045834. [Google Scholar] [CrossRef] [PubMed]
- Topp, C.; Østergaard, S.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Awata, S.; Bech, P.; Koizumi, Y.; Seki, T.; Kuriyama, S.; Hozawa, A.; Ohmori, K.; Nakaya, N.; Matsuoka, H.; Tsuji, I. Validity and utility of the Japanese version of the WHO-Five Well-Being Index in the context of detecting suicidal ideation in elderly community residents. Int. Psychogeriatr. 2007, 19, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, E.; Fujiwara, Y.; Fukaya, T.; Nishi, M.; Saito, M.; Shinkai, S. Social support availability and psychological well-being among the socially isolated elderly. Differences by living arrangement and gender. Nihon Koshu Eisei Zasshi 2011, 58, 446–456. [Google Scholar]
- Hunter, R.F.; de la Haye, K.; Murray, J.M.; Badham, J.; Valente, T.W.; Clarke, M.; Kee, F. Social network interventions for health behaviours and outcomes: A systematic review and meta-analysis. PLoS Med. 2019, 16, e1002890. [Google Scholar] [CrossRef] [Green Version]
- Kawachi, I.; Berkman, L. Social cohesion, social capital, and health. In Social Epidemiology; Berkman, L., Kawachi, I., Eds.; Oxford University Press: Oxford, UK, 2014; pp. 174–190. [Google Scholar]
- Seino, S.; Kitamura, A.; Nishi, M.; Tomine, Y.; Tanaka, I.; Taniguchi, Y.; Yokoyama, Y.; Amano, H.; Narita, M.; Ikeuchi, T.; et al. Individual- and community-level neighbor relationships and physical activity among older Japanese adults living in a metropolitan area: A cross-sectional multilevel analysis. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 46. [Google Scholar] [CrossRef]
- Larsen, B.A.; Strong, D.; Linke, S.E. The association between family and friend integration and physical activity: Results from the NHIS. Int. J. Behav. Med. 2014, 21, 529–536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sander, J.; Schupp, J.; Richter, D. Getting together: Social contact frequency across the life span. Dev. Psychol. 2017, 53, 1571–1588. [Google Scholar] [CrossRef]
- House, J.S.; Landis, K.R.; Umberson, D. Social relationships and health. Science 1988, 241, 540–545. [Google Scholar] [CrossRef]
- Pinquart, M.; Sörensen, S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: A meta-analysis. Psychol. Aging 2000, 15, 187–224. [Google Scholar] [CrossRef] [PubMed]
- Levula, A.; Harré, M.; Wilson, A. Social network factors as mediators of mental health and psychological distress. Int. J. Soc. Psychiatry 2017, 63, 235–243. [Google Scholar] [CrossRef]
- Tsutsui, T. Implementation process and challenges for the community-based integrated care system in Japan. Int. J. Integr. Care 2014, 14, e002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- OECD. Lack of Social Support. 2020. Available online: https://data.oecd.org/healthrisk/lack-of-social-support.htm (accessed on 12 January 2022).
- Ministry of Health, Labour, and Welfare. Chapter 1: Current situation of suicide: Section 3, Change in the Number of Suicides by Age Group. In White Paper on Suicide Prevention in Japan; Cabinet Office: Tokyo, Japan, 2020; pp. 6–10. [Google Scholar]
- Ellison, N.B.; Steinfield, C.; Lampe, C. The benefits of Facebook “Friends:” social capital and college students’ use of online social network sites. J. Comput. Mediat. Commun. 2007, 12, 1143–1168. [Google Scholar] [CrossRef] [Green Version]
- Nabi, R.L.; Prestin, A.; So, J. Facebook friends with (Health) benefits? Exploring social network site use and perceptions of social support, stress, and well-being. Cyberpsychol. Behav. Soc. Netw. 2013, 16, 721–727. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fox, J.; Moreland, J.J. The dark side of social networking sites: An exploration of the relational and psychological stressors associated with Facebook use and affordances. Comput. Hum. Behav. 2015, 45, 168–176. [Google Scholar] [CrossRef]
- Vidal, C.; Lhaksampa, T.; Miller, L.; Platt, R. Social media use and depression in adolescents: A scoping review. Int. Rev. Psychiatry 2020, 32, 235–253. [Google Scholar] [CrossRef]
- Sakurai, R.; Nemoto, Y.; Mastunaga, H.; Fujiwara, Y. Who is mentally healthy? Mental health profiles of Japanese social networking service users with a focus on LINE, Facebook, Twitter, and Instagram. PLoS ONE 2021, 16, e0246090. [Google Scholar] [CrossRef]
- Fujiwara, Y.; Shinkai, S.; Kumagai, S.; Amano, H.; Yoshida, Y.; Yoshida, H.; Kim, H.; Suzuki, T.; Ishizaki, T.; Watanabe, S.; et al. Changes in TMIG-Index of Competence by subscale in Japanese urban and rural community older populations: Six-years prospective study. Geriatr. Gerontol. Int. 2003, 3, S63–S68. [Google Scholar] [CrossRef]
- Cohen, S.; Gottlieb, B.H.; Underwood, L.G. Social relationships and health. In Measuring and Intervening in Social Support; Cohen, S., Underwood, L.G., Gottlieb, B.H., Eds.; Oxford University Press: New York, NY, USA, 2000; pp. 3–25. [Google Scholar]
| (1) Group O: 65–84 Years | (2) Group M: 50–64 Years | (3) Group Y: 25–49 Years | Total | p a | Multiple Comparison Procedure | ||||
|---|---|---|---|---|---|---|---|---|---|
| n = 649 | n = 533 | n = 569 | n = 1751 | (1) vs. (2) | (2) vs. (3) | (3) vs. (1) | |||
| Age | Mean (SD) | 72.4 (5.3) | 57.2 (4.4) | 39.4 (6.7) | 57.0 (14.8) | <0.001 | <0.001 | <0.001 | <0.001 |
| Field | Tama ward | 54.1% | 54.2% | 52.5% | 53.6% | 0.820 | - | - | - |
| Gender | female | 54.4% | 63.4% | 67.7% | 61.5% | <0.001 | 0.002 | 0.145 | <0.001 |
| Social contact status b | NC | 26.1% | 37.3% | 37.9% | 33.4% | <0.001 | <0.001 | 0.792 | <0.001 |
| NFFC | 18.2% | 27.0% | 28.2% | 24.2% | |||||
| FFC | 55.7% | 35.8% | 33.9% | 42.4% | |||||
| WHO-5 c (range: 0–25) | poor (<13) | 25.4% | 32.8% | 33.6% | 30.3% | 0.003 | 0.006 | 0.798 | 0.002 |
| Self-rated health d | poor | 15.5% | 16.4% | 11.5% | 14.5% | 0.043 | 0.688 | 0.018 | 0.044 |
| Number of history of chronic conditions | ≥1 | 34.9% | 16.7% | 7.2% | 20.4% | <0.001 | <0.001 | <0.001 | <0.001 |
| Years of education | <13 | 58.4% | 30.5% | 17.3% | 36.5% | <0.001 | <0.001 | <0.001 | <0.001 |
| Living arrangement | living alone | 22.7% | 10.6% | 18.1% | 17.5% | <0.001 | <0.001 | 0.001 | 0.058 |
| Subjective financial Situation e | not so good | 21.2% | 25.1% | 22.8% | 22.9% | 0.282 | - | - | - |
| Poor Self-Rated Health a | Reference | Category | (1) Group O: 65–84 Years | (2) Group M: 50–64 Years | (3) Group Y: 25–49 Years | ||||||
| OR | 95% C.I. | p | OR | 95% C.I. | p | OR | 95% C.I. | p | |||
| Field | Kita ward | Tama ward | 0.94 | 0.74–1.19 | 0.594 | 1.13 | 0.88–1.46 | 0.327 | 1.08 | 0.81–1.43 | 0.619 |
| Gender | male | female | 1.65 | 0.98–2.78 | 0.061 | 1.83 | 1.01–3.30 | 0.045 | 1.18 | 0.63–2.20 | 0.608 |
| Age | 1 year crement | 1.04 | 1.00–1.09 | 0.072 | 0.99 | 0.94–1.05 | 0.775 | 1.01 | 0.97–1.06 | 0.575 | |
| Social contact status c | NC | NFFC | 1.04 | 0.52–2.06 | 0.923 | 0.87 | 0.47–1.63 | 0.662 | 1.02 | 0.53–1.97 | 0.963 |
| FFC | 0.68 | 0.38–1.22 | 0.197 | 0.50 | 0.26–0.94 | 0.031 | 0.40 | 0.19–0.83 | 0.014 | ||
| Number of history of chronic conditions | 0 | ≥1 | 5.42 | 3.29–8.93 | 0.000 | 4.39 | 2.49–7.73 | 0.000 | 6.56 | 3.03–14.18 | 0.000 |
| Years of education | <13 | ≥13 | 0.77 | 0.45–1.29 | 0.314 | 0.85 | 0.50–1.44 | 0.542 | 0.70 | 0.35–1.40 | 0.317 |
| Living arrangement | living with someone | living alone | 1.18 | 0.68–2.05 | 0.563 | 2.01 | 0.99–4.10 | 0.055 | 1.32 | 0.64–2.72 | 0.453 |
| Subjective financial situation d | good | poor | 2.22 | 1.29–3.83 | 0.004 | 2.29 | 1.35–3.88 | 0.002 | 3.19 | 1.77–5.73 | 0.000 |
| Poor WHO-5 b (<13 scores) | Reference | Category | Group O: 65–84 years | Group M: 50–64 years | Group Y: 25–49 years | ||||||
| OR | 95% C.I. | p | OR | 95% C.I. | p | OR | 95% C.I. | p | |||
| Field | Kita ward | Tama ward | 0.83 | 0.67–1.02 | 0.072 | 1.12 | 0.92–1.36 | 0.270 | 0.90 | 0.75–1.08 | 0.249 |
| Gender | male | female | 1.15 | 0.73–1.80 | 0.547 | 0.95 | 0.62–1.46 | 0.812 | 1.03 | 0.69–1.53 | 0.901 |
| Age | 1 year crement | 0.97 | 0.93–1.00 | 0.075 | 0.96 | 0.92–1.00 | 0.075 | 1.01 | 0.98–1.04 | 0.405 | |
| Social contact status c | NC | NFFC | 0.55 | 0.31–0.96 | 0.036 | 0.56 | 0.34–0.93 | 0.025 | 0.63 | 0.41–0.99 | 0.043 |
| FFC | 0.21 | 0.13–0.35 | 0.000 | 0.50 | 0.31–0.81 | 0.005 | 0.30 | 0.19–0.47 | 0.000 | ||
| Number of history of chronic conditions | 0 | ≥1 | 1.38 | 0.90–2.11 | 0.143 | 1.54 | 0.92–2.60 | 0.103 | 0.84 | 0.40–1.76 | 0.635 |
| Years of education | <13 | ≥13 | 0.60 | 0.38–0.93 | 0.023 | 0.70 | 0.46–1.07 | 0.102 | 1.26 | 0.76–2.08 | 0.378 |
| Living arrangement | living with someone | living alone | 1.19 | 0.73–1.92 | 0.491 | 1.54 | 0.83–2.87 | 0.171 | 1.55 | 0.97–2.49 | 0.068 |
| Subjective financial situation d | good | poor | 2.48 | 1.56–3.94 | 0.000 | 2.10 | 1.36–3.26 | 0.001 | 1.93 | 1.26–2.96 | 0.003 |
| Decline in Self-Rated Health a | Reference | Category | Group O: 65–84 Years | Group M: 50–64 Years | Group Y: 25–49 Years | ||||||
| OR | 95% C.I. | p | OR | 95% C.I. | p | OR | 95% C.I. | p | |||
| Field | Kita-ward | Tama-ward | 0.71 | 0.36–1.37 | 0.304 | 0.42 | 0.18–0.99 | 0.048 | 0.68 | 0.31–1.53 | 0.351 |
| Gender | male | female | 0.78 | 0.38–1.58 | 0.485 | 0.79 | 0.33–1.88 | 0.587 | 0.45 | 0.20–1.02 | 0.057 |
| Age | 1 year crement | 1.02 | 0.96–1.09 | 0.473 | 1.06 | 0.96–1.17 | 0.259 | 0.87 | 0.82–0.93 | 0.000 | |
| Social contact status c | NC | NFFC | 0.53 | 0.19–1.46 | 0.221 | 0.47 | 0.17–1.34 | 0.159 | 0.75 | 0.28–2.02 | 0.573 |
| FFC | 0.64 | 0.30–1.36 | 0.240 | 0.28 | 0.10–0.80 | 0.017 | 0.79 | 0.31–2.01 | 0.624 | ||
| Number of history of chronic conditions | 0 | ≥1 | 2.71 | 1.37–5.34 | 0.004 | 2.43 | 0.93–6.39 | 0.071 | 3.01 | 0.60–15.26 | 0.183 |
| Years of education | <13 | ≥13 | 0.67 | 0.33–1.35 | 0.258 | 0.38 | 0.17–0.87 | 0.021 | 0.28 | 0.11–0.75 | 0.011 |
| Living arrangement | living with someone | living alone | 0.96 | 0.43–2.14 | 0.911 | 0.17 | 0.02–1.44 | 0.104 | 0.84 | 0.31–2.31 | 0.739 |
| Subjective financial situation d | good | poor | 2.86 | 1.38–5.91 | 0.005 | 3.21 | 1.39–7.38 | 0.006 | 1.79 | 0.76–4.20 | 0.181 |
| Poor WHO-5 b (<13 scores) | Reference | Category | Group O: 65–84 years | Group M: 50–64 years | Group Y: 25–49 years | ||||||
| OR | 95% C.I. | p | OR | 95% C.I. | p | OR | 95% C.I. | p | |||
| Field | Kita-ward | Tama-ward | 0.53 | 0.31–0.90 | 0.019 | 1.21 | 0.71–2.06 | 0.487 | 0.88 | 0.54–1.44 | 0.613 |
| Gender | male | female | 0.53 | 0.29–0.96 | 0.037 | 1.46 | 0.80–2.69 | 0.220 | 0.65 | 0.39–1.09 | 0.100 |
| Age | 1 year crement | 1.00 | 0.95–1.05 | 0.908 | 1.00 | 0.94–1.07 | 0.914 | 0.99 | 0.96–1.03 | 0.756 | |
| Social contact status c | NC | NFFC | 0.45 | 0.21–0.97 | 0.043 | 0.81 | 0.42–1.57 | 0.536 | 0.47 | 0.25–0.88 | 0.019 |
| FFC | 0.27 | 0.14–0.51 | 0.000 | 0.66 | 0.34–1.30 | 0.227 | 0.42 | 0.23–0.74 | 0.003 | ||
| Number of history of chronic conditions | 0 | ≥1 | 1.29 | 0.73–2.27 | 0.384 | 1.39 | 0.67–2.85 | 0.376 | 3.13 | 1.35–7.25 | 0.008 |
| Years of education | <13 | ≥13 | 0.75 | 0.43–1.30 | 0.298 | 0.83 | 0.46–1.50 | 0.541 | 0.95 | 0.50–1.82 | 0.880 |
| Living arrangement | living with someone | living alone | 0.72 | 0.37–1.39 | 0.325 | 2.36 | 1.03–5.39 | 0.043 | 1.38 | 0.73–2.62 | 0.324 |
| Subjective financial situation d | good | poor | 2.76 | 1.48–5.12 | 0.001 | 1.42 | 0.74–2.71 | 0.295 | 2.37 | 1.33–4.20 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujiwara, Y.; Nonaka, K.; Kuraoka, M.; Murayama, Y.; Murayama, S.; Nemoto, Y.; Tanaka, M.; Matsunaga, H.; Fujita, K.; Murayama, H.; et al. Influence of “Face-to-Face Contact” and “Non-Face-to-Face Contact” on the Subsequent Decline in Self-Rated Health and Mental Health Status of Young, Middle-Aged, and Older Japanese Adults: A Two-Year Prospective Study. Int. J. Environ. Res. Public Health 2022, 19, 2218. https://doi.org/10.3390/ijerph19042218
Fujiwara Y, Nonaka K, Kuraoka M, Murayama Y, Murayama S, Nemoto Y, Tanaka M, Matsunaga H, Fujita K, Murayama H, et al. Influence of “Face-to-Face Contact” and “Non-Face-to-Face Contact” on the Subsequent Decline in Self-Rated Health and Mental Health Status of Young, Middle-Aged, and Older Japanese Adults: A Two-Year Prospective Study. International Journal of Environmental Research and Public Health. 2022; 19(4):2218. https://doi.org/10.3390/ijerph19042218
Chicago/Turabian StyleFujiwara, Yoshinori, Kumiko Nonaka, Masataka Kuraoka, Yoh Murayama, Sachiko Murayama, Yuta Nemoto, Motoki Tanaka, Hiroko Matsunaga, Koji Fujita, Hiroshi Murayama, and et al. 2022. "Influence of “Face-to-Face Contact” and “Non-Face-to-Face Contact” on the Subsequent Decline in Self-Rated Health and Mental Health Status of Young, Middle-Aged, and Older Japanese Adults: A Two-Year Prospective Study" International Journal of Environmental Research and Public Health 19, no. 4: 2218. https://doi.org/10.3390/ijerph19042218
APA StyleFujiwara, Y., Nonaka, K., Kuraoka, M., Murayama, Y., Murayama, S., Nemoto, Y., Tanaka, M., Matsunaga, H., Fujita, K., Murayama, H., & Kobayashi, E. (2022). Influence of “Face-to-Face Contact” and “Non-Face-to-Face Contact” on the Subsequent Decline in Self-Rated Health and Mental Health Status of Young, Middle-Aged, and Older Japanese Adults: A Two-Year Prospective Study. International Journal of Environmental Research and Public Health, 19(4), 2218. https://doi.org/10.3390/ijerph19042218







