The Relationship between Metal Exposure and Chronic Obstructive Pulmonary Disease in the General US Population: NHANES 2015–2016
Abstract
:1. Introduction
2. Materials and Methods
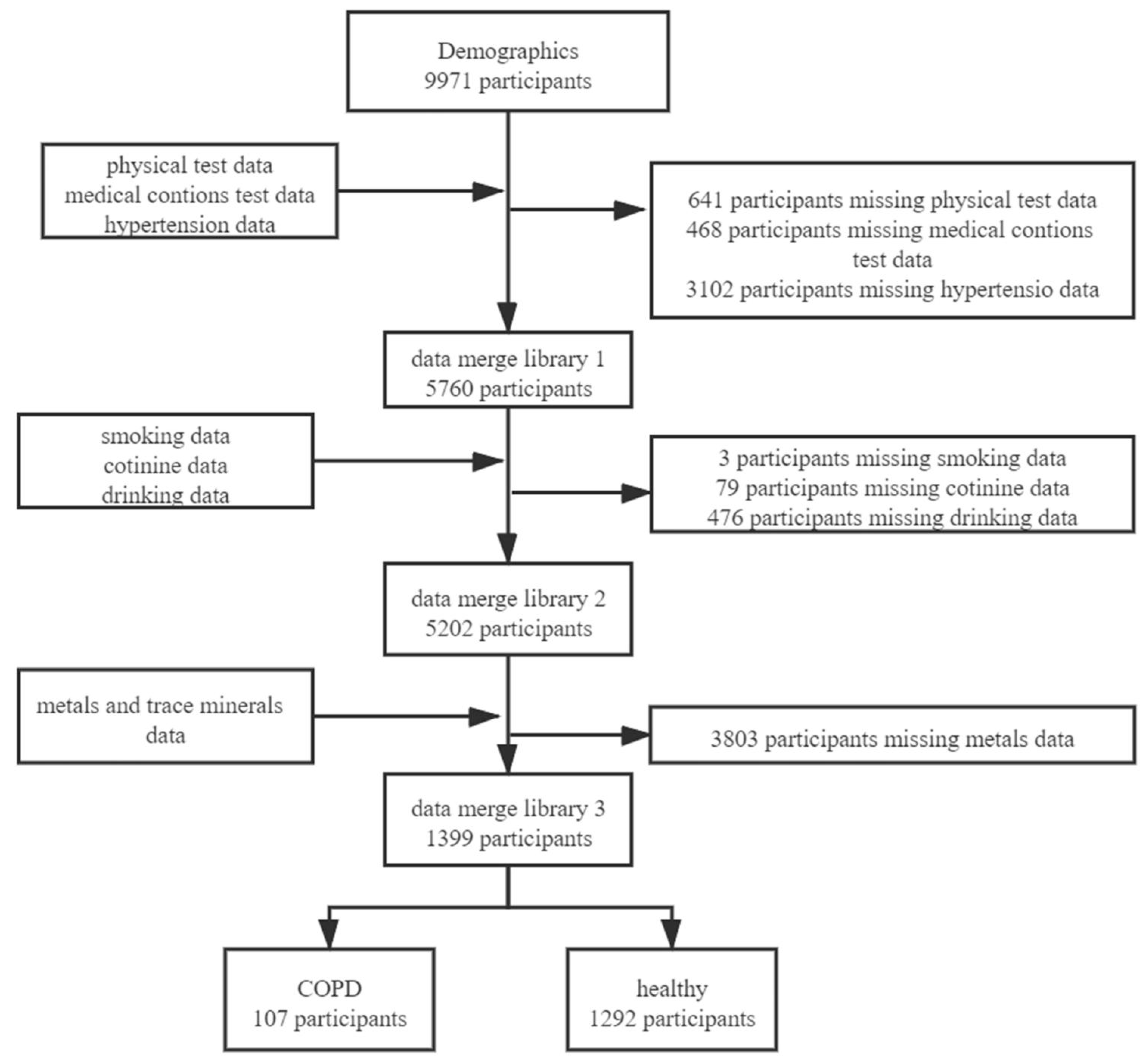
2.1. Study Population
2.2. Metal and Trace Mineral Measurements
2.3. COPD
2.4. Smoking and Secondhand Smoke Exposure
2.5. Drinking
2.6. Covariates
2.7. Statistical Analysis
3. Results
3.1. Demographic Characteristics
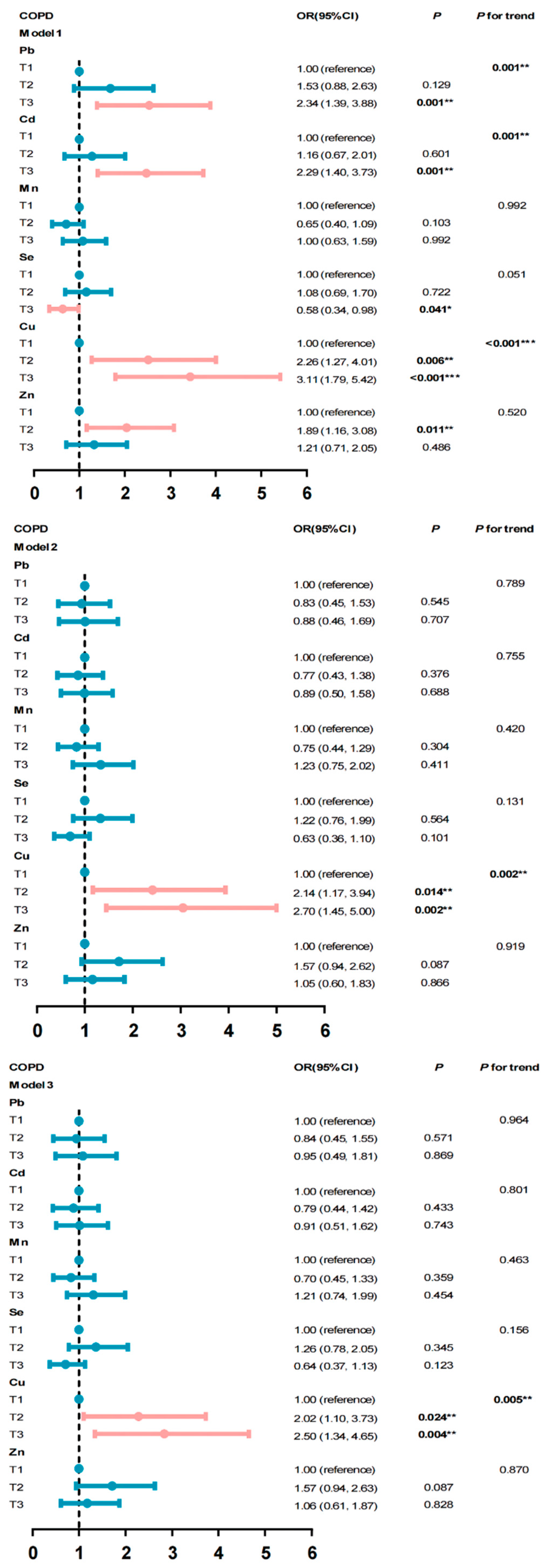
3.2. The Association between Metals, Trace Mineral Exposure, and the Risk of COPD
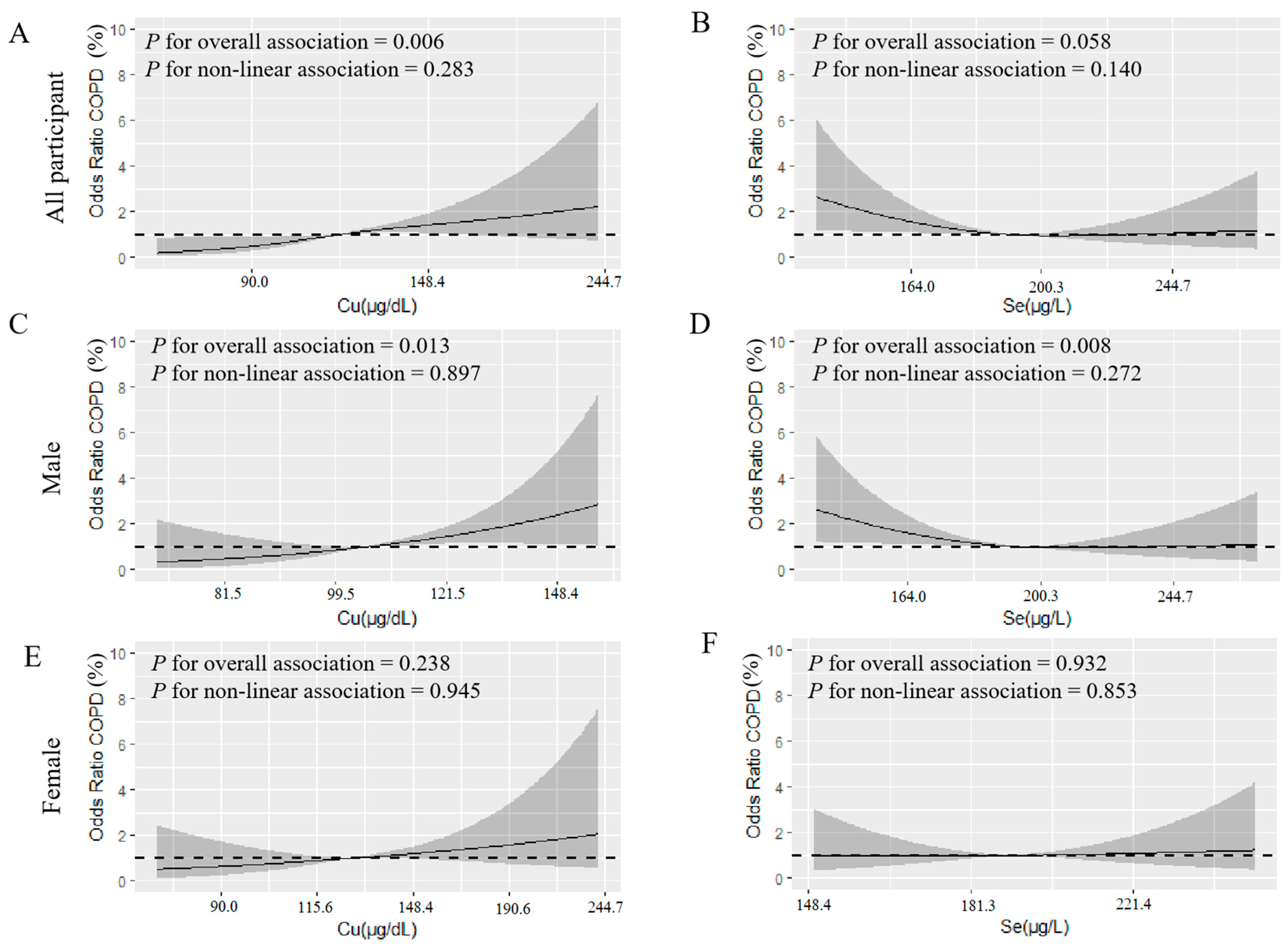
3.3. Dose–Response Relationship between Metals and the Risk of COPD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ibrahimou, B.; Azim, S.I.; Sun, N. Interaction between blood lead level and chronic obstructive pulmonary disease (COPD) on risk of heart attack or stroke: USA NHANES, 2013–2014. Pulm. Pharmacol. Ther. 2019, 58, 101805. [Google Scholar] [CrossRef]
- Vogelmeier, C.F.; Criner, G.J.; Martinez, F.J.; Anzueto, A.; Barnes, P.J.; Bourbeau, J.; Celli, B.R.; Chen, R.; Decramer, M.; Fabbri, L.M.; et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am. J. Respir. Crit. Care Med. 2017, 195, 557–582. [Google Scholar] [CrossRef]
- Global Status of COPD. Available online: https://www.who.int/respiratory/copd/burden/zh/ (accessed on 2 October 2021).
- López-Campos, J.L.; Tan, W.; Soriano, J.B. Global burden of COPD. Respirology 2016, 21, 14–23. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Fernandes, L.; Mesquita, A. Biomass smoke exposure is the main risk factor for COPD in non smoking women in a developing country. Eur. Respir. J. 2013, 42, 2008. [Google Scholar]
- Matheson, M.C.; Benke, G.; Raven, J.; Sim, M.R.; Kromhout, H.; Vermeulen, R.; Johns, D.P.; Walters, E.H.; Abramson, M.J. Biological dust exposure in the workplace is a risk factor for chronic obstructive pulmonary disease. Thorax 2005, 60, 645–651. [Google Scholar] [CrossRef] [Green Version]
- De Marco, R.; Accordini, S.; Marcon, A.; Cerveri, I.; Antó, J.M.; Gislason, T.; Heinrich, J.; Janson, C.; Jarvis, D.; Kuenzli, N.; et al. Risk factors for chronic obstructive pulmonary disease in a European cohort of young adults. Am. J. Respir. Crit. Care Med. 2011, 183, 891–897. [Google Scholar] [CrossRef]
- Sparrow, D.; Silbert, J.E.; Weiss, S.T. The relationship of pulmonary function to copper concentrations in drinking water. Am. Rev. Respir. Dis. 1982, 126, 312–315. [Google Scholar]
- Xiao, L.; Zhou, Y.; Cui, X.; Huang, X.; Yuan, J.; Chen, W. Association of urinary metals and lung function in general Chinese population of Wuhan. Zhonghua Yu Fang Yi Xue Za Zhi 2016, 50, 680–688. [Google Scholar]
- Pappas, R.S.; Fresquez, M.R.; Martone, N.; Watson, C.H. Toxic metal concentrations in mainstream smoke from cigarettes available in the USA. J. Anal. Toxicol. 2014, 38, 204–211. [Google Scholar] [CrossRef] [Green Version]
- Piadé, J.J.; Jaccard, G.; Dolka, C.; Belushkin, M.; Wajrock, S. Differences in cadmium transfer from tobacco to cigarette smoke, compared to arsenic or lead. Toxicol. Rep. 2015, 2, 12–26. [Google Scholar] [CrossRef] [Green Version]
- Richter, P.; Faroon, O.; Pappas, R.S. Cadmium and cadmium/zinc ratios and tobacco-related morbidities. Int. J. Environ. Res. Public Health 2017, 14, 1154. [Google Scholar] [CrossRef] [Green Version]
- Manca, D.; Ricard, A.C.; Trottier, B.; Chevalier, G. Studies on lipid peroxidation in rat tissues following administration of low and moderate doses of cadmium chloride. Toxicology 1991, 67, 303–323. [Google Scholar] [CrossRef]
- Faroon, O.; Ashizawa, A.; Wright, S.; Tucker, P.; Jenkins, K.; Ingerman, L.; Rudisill, C. Agency for Toxic Substances and Disease Registry (ATSDR) Toxicological Profiles. In Toxicological Profile for Cadmium; Agency for Toxic Substances and Disease Registry (US): Atlanta, GA, USA, 2012. [Google Scholar]
- Anetor, J.; Ajose, F.; Anetor, G.; Iyanda, A.; Babalola, B.; Adeniyi, F. High cadmium/zinc ratio in cigarette smokers: Potential implications as a biomarker of risk of prostate cancer. Niger. J. Physiol. Sci. 2008, 23, 41–49. [Google Scholar] [CrossRef] [Green Version]
- Ibs, K.H.; Rink, L. Zinc-altered immune function. J. Nutr. 2003, 133, 1452S–1456S. [Google Scholar] [CrossRef]
- Rink, L.; Kirchner, H. Zinc-altered immune function and cytokine production. J. Nutr. 2000, 130, 1407S–1411S. [Google Scholar] [CrossRef] [Green Version]
- Meydani, S.N.; Barnett, J.B.; Dallal, G.E.; Fine, B.C.; Jacques, P.F.; Leka, L.S.; Hamer, D.H. Serum zinc and pneumonia in nursing home elderly. Am. J. Clin. Nutr. 2007, 86, 1167–1173. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.S.; Caffrey, J.L.; Chang, M.H.; Dowling, N.; Lin, J.W. Cigarette smoking, cadmium exposure, and zinc intake on obstructive lung disorder. Respir. Res. 2010, 11, 53. [Google Scholar] [CrossRef] [Green Version]
- Rahman, I.; Kilty, I. Antioxidant therapeutic targets in COPD. Curr. Drug Targets 2006, 7, 707–720. [Google Scholar] [CrossRef]
- Hassan, F.; Xu, X.; Nuovo, G.; Killilea, D.W.; Tyrrell, J.; Da Tan, C.; Tarran, R.; Diaz, P.; Jee, J.; Knoell, D.; et al. Accumulation of metals in GOLD4 COPD lungs is associated with decreased CFTR levels. Respir. Res. 2014, 15, 69. [Google Scholar] [CrossRef] [Green Version]
- Rokadia, H.K.; Agarwal, S. Serum heavy metals and obstructive lung disease: Results from the National Health and Nutrition Examination Survey. Chest 2013, 143, 388–397. [Google Scholar] [CrossRef]
- Thomas, R. Practical Guide to ICP-MS: A Tutorial for Beginners; CRC Press: Boca Raton, FL, USA, 2008. [Google Scholar]
- Tanner, S.D.; Baranov, V.I. Theory, design, and operation of a dynamic reaction cell for ICP-MS. At. Spectrosc. Norwalk Conn. 1999, 20, 45–52. [Google Scholar]
- Tanner, S.D.; Baranov, V.I.; Bandura, D.R. Reaction cells and collision cells for ICP-MS: A tutorial review. Spectrochim. Acta Part B At. Spectrosc. 2002, 57, 1361–1452. [Google Scholar] [CrossRef]
- Navaneethan, S.D.; Mandayam, S.; Arrigain, S.; Rahman, M.; Winkelmayer, W.C.; Schold, J.D. Obstructive and restrictive lung function measures and CKD: National Health and nutrition examination survey (NHANES) 2007–2012. Am. J. Kidney Dis. 2016, 68, 414–421. [Google Scholar] [CrossRef] [Green Version]
- Dong, X.; Li, S.; Sun, J.; Zhang, D. Association of Coffee, Decaffeinated Coffee and Caffeine Intake from Coffee with Cognitive Performance in Older Adults: National Health and Nutrition Examination Survey (NHANES) 2011–2014. Nutrients 2020, 12, 840. [Google Scholar] [CrossRef] [Green Version]
- Madrigal, J.M.; Persky, V.; Pappalardo, A.; Argos, M. Association of heavy metals with measures of pulmonary function in children and youth: Results from the National Health and Nutrition Examination Survey (NHANES). Environ. Int. 2018, 121, 871–878. [Google Scholar] [CrossRef]
- Desquilbet, L.; Mariotti, F. Dose-response analyses using restricted cubic spline functions in public health research. Stat. Med. 2010, 29, 1037–1057. [Google Scholar] [CrossRef]
- Wen, X.; Liu, Y.; Bai, Y.; Li, M.; Fu, Q.; Zheng, Y. LOXL2, a copper-dependent monoamine oxidase, activates lung fibroblasts through the TGF-β/Smad pathway. Int. J. Mol. Med. 2018, 42, 3530–3541. [Google Scholar] [CrossRef] [Green Version]
- Baldari, S.; Di Rocco, G.; Toietta, G. Current biomedical use of copper chelation therapy. Int. J. Mol. Sci. 2020, 21, 1069. [Google Scholar] [CrossRef] [Green Version]
- Janssen, R.; de Brouwer, B.; Jan, H.; Wouters, E.F. Copper as the most likely pathogenic divergence factor between lung fibrosis and emphysema. Med. Hypotheses 2018, 120, 49–54. [Google Scholar] [CrossRef]
- Bastola, M.M.; Locatis, C.; Maisiak, R.; Fontelo, P. Selenium, copper, zinc and hypertension: An analysis of the National Health and Nutrition Examination Survey (2011–2016). BMC Cardiovasc. Disord. 2020, 20, 45. [Google Scholar] [CrossRef] [Green Version]
- Suadicani, P.; Hein, H.O.; Gyntelberg, F. Serum selenium level and risk of lung cancer mortality: A 16-year follow-up of the Copenhagen Male Study. Eur. Respir. J. 2012, 39, 1443–1448. [Google Scholar] [CrossRef] [Green Version]
- Salmonowicz, B.; Krzystek-Korpacka, M.; Noczynska, A. Trace elements, magnesium, and the efficacy of antioxidant systems in children with type 1 diabetes mellitus and in their siblings. Adv. Clin. Exp. Med. 2014, 23, 259–268. [Google Scholar] [CrossRef] [Green Version]
- Alkan, F.A.; Karis, D.; Cakmak, G.; Ercan, A.M. Analysis of the relationship between hemorheologic parameters, aluminum, manganese, and selenium in smokers. Biol. Trace Elem. Res. 2019, 187, 22–31. [Google Scholar] [CrossRef]
- Brune, D.; Nordberg, G.; Wester, P.O. Distribution of 23 elements in the kidney, liver and lungs of workers from a smeltery and refinery in North Sweden exposed to a number of elements and of a control group. Sci. Total Environ. 1980, 16, 13–35. [Google Scholar] [CrossRef]
- Barceloux, D.G.; Barceloux, D. Copper. J. Toxicol. Clin. Toxicol. 1999, 37, 217–230. [Google Scholar] [CrossRef]
- Weissman, S.H.; Cuddihy, R.G.; Medinsky, M.A. Absorption, distribution, and retention of inhaled selenious acid and selenium metal aerosols in beagle dogs. Toxicol. Appl. Pharmacol. 1983, 67, 331–337. [Google Scholar] [CrossRef]
- Li, S.; Sun, W.; Zhang, D. Association of zinc, iron, copper, and selenium intakes with low cognitive performance in older adults: A cross-sectional study from National Health and Nutrition Examination Survey (NHANES). J. Alzheimer’s Dis. 2019, 72, 1145–1157. [Google Scholar] [CrossRef]
- Kies, C. Food sources of dietary copper. Copper bioavailability and metabolism. Adv. Exp. Med. Biol. 1989, 258, 1–20. [Google Scholar]
- U.S. Copper Intake. Available online: https://ods.od.nih.gov/factsheets/Copper-HealthProfessional/ (accessed on 2 October 2021).
- Jiang, C.; Wu, B.; Xue, M.; Lin, J.; Hu, Z.; Nie, X.; Cai, G. Inflammation accelerates copper-mediated cytotoxicity through induction of six-transmembrane epithelial antigens of prostate 4 expression. Immunol. Cell Biol. 2021, 99, 392–402. [Google Scholar] [CrossRef]
- Pearson, P.; Britton, J.; McKeever, T.; Lewis, S.; Weiss, S.; Pavord, I.; Fogarty, A. Lung function and blood levels of copper, selenium, vitamin C and vitamin E in the general population. Eur. J. Clin. Nutr. 2005, 59, 1043–1048. [Google Scholar] [CrossRef]
- Tofovic, S.P.; Zhang, X.; Jackson, E.K.; Zhu, H.; Petrusevska, G. 2-methoxyestradiol attenuates bleomycin-induced pulmonary hypertension and fibrosis in estrogen-deficient rats. Vasc. Pharmacol. 2009, 51, 190–197. [Google Scholar] [CrossRef] [Green Version]
- Sathish, V.; Martin, Y.N.; Prakash, Y. Sex steroid signaling: Implications for lung diseases. Pharmacol. Ther. 2015, 150, 94–108. [Google Scholar] [CrossRef] [Green Version]
- U.S. Selenium Intake. Available online: https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/ (accessed on 2 October 2021).
- Bailey, R.L.; Gahche, J.J.; Lentino, C.V.; Dwyer, J.T.; Engel, J.S.; Thomas, P.R.; Betz, J.M.; Sempos, C.T.; Picciano, M.F. Dietary supplement use in the United States, 2003–2006. J. Nutr. 2011, 141, 261–266. [Google Scholar] [CrossRef] [Green Version]
- Feng, W.; Huang, X.; Zhang, C.; Liu, C.; Cui, X.; Zhou, Y.; Sun, H.; Qiu, G.; Guo, H.; He, M.; et al. The dose–response association of urinary metals with altered pulmonary function and risks of restrictive and obstructive lung diseases: A population-based study in China. BMJ Open 2015, 5, e007643. [Google Scholar] [CrossRef]
- Isbaniah, F.; Wiyono, W.H.; Yunus, F.; Setiawati, A.; Totzke, U.; Verbruggen, M. Echinacea purpurea along with zinc, selenium and vitamin C to alleviate exacerbations of chronic obstructive pulmonary disease: Results from a randomized controlled trial. J. Clin. Pharm. Ther. 2011, 36, 568–576. [Google Scholar] [CrossRef]
| Variables | Healthy | COPD | p-Value |
|---|---|---|---|
| (N = 1292) | (N = 107) | ||
| Age | 48.81 ± 17.43 a | 58.53 ± 16.19 a | <0.001 *** |
| Sex | 0.828 | ||
| Male | 642 (49.69) | 52 (48.60) | |
| Female | 650 (50.31) | 55 (51.40) | |
| Race | <0.001 *** | ||
| Mexican American | 233 (18.03) | 8 (7.48) | |
| Other Hispanic | 167 (12.93) | 20 (78.69) | |
| Non-Hispanic White | 442 (34.21) | 60 (56.07) | |
| Non-Hispanic Black | 252 (19.50) | 16 (14.95) | |
| Other Race | 198 (15.33) | 3 (2.80) | |
| BMI (kg/m2) | 0.019 * | ||
| <18.5 | 18 (1.39) | 1 (0.93) | |
| 18.5–25 | 325 (25.15) | 16 (14.95) | |
| 25-30 | 437 (33.82) | 32 (29.91) | |
| ≥30 | 512 (39.63) | 58 (54.21) | |
| Education | 0.025 * | ||
| Less than 9th grade | 134 (10.37) | 17 (15.89) | |
| 9–11 grade | 142 (10.99) | 15 (14.02) | |
| High school graduate | 293 (22.68) | 26 (24.30) | |
| Some college/AA degree | 379 (29.33) | 35 (32.71) | |
| College graduate | 344 (26.63) | 14 (13.08) | |
| Ratio of Family Income to Poverty | 0.001 ** | ||
| Under standard level | 1071 (82.89) | 102 (95.33) | |
| Above standard level | 221 (17.11) | 5 (4.67) | |
| Smoking | <0.001 *** | ||
| Current smoking | 751 (58.13) | 31 (28.97) | |
| Non-smoking | 234 (18.11) | 38 (35.51) | |
| Former smoking | 307 (23.76) | 38 (35.51) | |
| Secondhand smoke exposure | 0.013 ** | ||
| Yes | 947 (75.39) | 69 (64.49) | |
| No | 318 (24.61) | 38 (35.51) | |
| Serum cotinine (ng/mL) | 0.03 (0.01, 4.08) b | 0.18 (0.01, 227) b | <0.001 *** |
| Drinking | 0.052 | ||
| Yes | 899 (69.58) | 84 (78.50) | |
| No | 393 (30.42) | 23 (21.50) | |
| Hypertension | <0.001 *** | ||
| Yes | 428 (33.13) | 67 (62.62) | |
| No | 864 (66.87) | 40 (37.38) | |
| Diabetes | <0.001 * | ||
| Yes | 198 (15.33) | 35 (32.71) | |
| No | 1094 (84.67) | 72 (67.29) | |
| Blood Pb (µg/dL) | 0.93 (0.59, 1.49) b | 1.20 (0.75, 2.02) b | <0.001 *** |
| Tertile 1 (0.05–0.71) | 445 (34.44) | 23 (21.50) | |
| Tertile 2 (0.72–1.32) | 431 (33.36) | 34 (31.78) | |
| Tertile 3 (1.33–23.51) | 416 (32.20) | 50 (46.73) | |
| Blood Cd (µg/L) | 0.29 (0.18, 0.50) b | 0.41 (0.23, 0.93) b | <0.001 *** |
| Tertile 1 (0.07–0.22) | 458 (35.45) | 26 (24.30) | |
| Tertile 2 (0.23–0.42) | 426 (32.97) | 28 (26.17) | |
| Tertile 3 (0.43–6.37) | 408 (31.58) | 53 (49.53) | |
| Blood Mn (µg/L) | 9.52 (7.72, 11.91) b | 9.72 (7.61, 11.83) b | 0.862 |
| Tertile 1 (2.31–8.30) | 427 (33.05) | 40 (37.38) | |
| Tertile 2 (8.31–10.96) | 439 (33.98) | 27 (25.23) | |
| Tertile 3 (10.97–56.56) | 426 (32.97) | 40 (37.38) | |
| Blood Se (µg/L) | 192.75 (178.99, 207.38) b | 189.26 (176.96, 201.26) b | 0.070 |
| Tertile 1 (119.87–183.22) | 427 (33.05) | 40 (37.38) | |
| Tertile 2 (183.23–201.75) | 423 (32.74) | 43 (40.19) | |
| Tertile 3 (201.76–318.33) | 442 (34.21) | 24 (22.43) | |
| Serum Cu (µg/dL) | 114.25 (99.15, 133.10) b | 124.30 (110.40, 145.00) b | <0.001 *** |
| Tertile 1 (52.90–105.00) | 454 (35.14) | 18 (16.82) | |
| Tertile 2 (105.01–126.60) | 425 (32.89) | 38 (35.51) | |
| Tertile 3 (126.61–306.60) | 413 (31.97) | 51 (47.66) | |
| Serum Zn (µg/dL) | 79.90 (69.80, 89.90) b | 80. 90 (72.50, 91.10) b | 0.408 |
| Tertile 1 (31.40–73.70) | 442 (34.21) | 27 (25.23) | |
| Tertile 2 (73.71–86.40) | 416 (32.20) | 48 (44.86) | |
| Tertile 3 (86.41–139.10) | 434 (33.59) | 32 (29.91) |
| variables | Male | Female | ||||
|---|---|---|---|---|---|---|
| OR | p | 95% CI | OR | p | 95% CI | |
| Pb | ||||||
| T1 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| T2 | 1.20 | 0.752 | 0.38–3.79 | 0.78 | 0.522 | 0.36–1.68 |
| T3 | 1.70 | 0.362 | 0.54–5.31 | 0.68 | 0.384 | 0.28–1.63 |
| p for trend | 0.279 | 0.388 | ||||
| Cd | ||||||
| T1 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| T2 | 0.65 | 0.378 | 0.26–1.68 | 0.80 | 0.576 | 0.37–1.74 |
| T3 | 1.64 | 0.235 | 0.73–3.69 | 0.48 | 0.110 | 0.19–1.18 |
| p for trend | 0.160 | 0.109 | ||||
| Mn | ||||||
| T1 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| T2 | 0.90 | 0.796 | 0.41–1.99 | 0.66 | 0.278 | 0.31–1.40 |
| T3 | 1.74 | 0.122 | 0.86–3.50 | 0.85 | 0.654 | 0.41–1.74 |
| p for trend | 0.147 | 0.696 | ||||
| Se | ||||||
| T1 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| T2 | 0.86 | 0.683 | 0.43–1.75 | 1.79 | 0.092 | 0.91–3.53 |
| T3 | 0.48 | 0.078 | 0.22–1.08 | 0.83 | 0.633 | 0.38–1.81 |
| p for trend | 0.081 | 0.806 | ||||
| Cu | ||||||
| T1 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| T2 | 1.65 | 0.200 | 0.77–3.52 | 2.53 | 0.113 | 0.80–7.96 |
| T3 | 3.31 | 0.004 ** | 1.47–7.44 | 2.38 | 0.128 | 0.78–7.28 |
| p for trend | 0.004 ** | 0.247 | ||||
| Zn | ||||||
| T1 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| T2 | 1.43 | 0.332 | 0.69–2.96 | 1.81 | 0.124 | 0.85–3.86 |
| T3 | 0.72 | 0.423 | 0.32–1.62 | 1.70 | 0.195 | 0.76–3.80 |
| p for trend | 0.420 | 0.212 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fei, Q.; Weng, X.; Liu, K.; Liu, S.; Chen, J.; Guo, X.; Jing, C. The Relationship between Metal Exposure and Chronic Obstructive Pulmonary Disease in the General US Population: NHANES 2015–2016. Int. J. Environ. Res. Public Health 2022, 19, 2085. https://doi.org/10.3390/ijerph19042085
Fei Q, Weng X, Liu K, Liu S, Chen J, Guo X, Jing C. The Relationship between Metal Exposure and Chronic Obstructive Pulmonary Disease in the General US Population: NHANES 2015–2016. International Journal of Environmental Research and Public Health. 2022; 19(4):2085. https://doi.org/10.3390/ijerph19042085
Chicago/Turabian StyleFei, Qiaoyuan, Xueqiong Weng, Kun Liu, Shan Liu, Jingmin Chen, Xinrong Guo, and Chunxia Jing. 2022. "The Relationship between Metal Exposure and Chronic Obstructive Pulmonary Disease in the General US Population: NHANES 2015–2016" International Journal of Environmental Research and Public Health 19, no. 4: 2085. https://doi.org/10.3390/ijerph19042085
APA StyleFei, Q., Weng, X., Liu, K., Liu, S., Chen, J., Guo, X., & Jing, C. (2022). The Relationship between Metal Exposure and Chronic Obstructive Pulmonary Disease in the General US Population: NHANES 2015–2016. International Journal of Environmental Research and Public Health, 19(4), 2085. https://doi.org/10.3390/ijerph19042085





