Pilot Feasibility Study of a Hospital-Based Post-Natal Educational Intervention on New Mothers in a BFHI-Compliant Tertiary Referral Center for Neonatal Care
Abstract
:1. Background
2. Materials and Methods
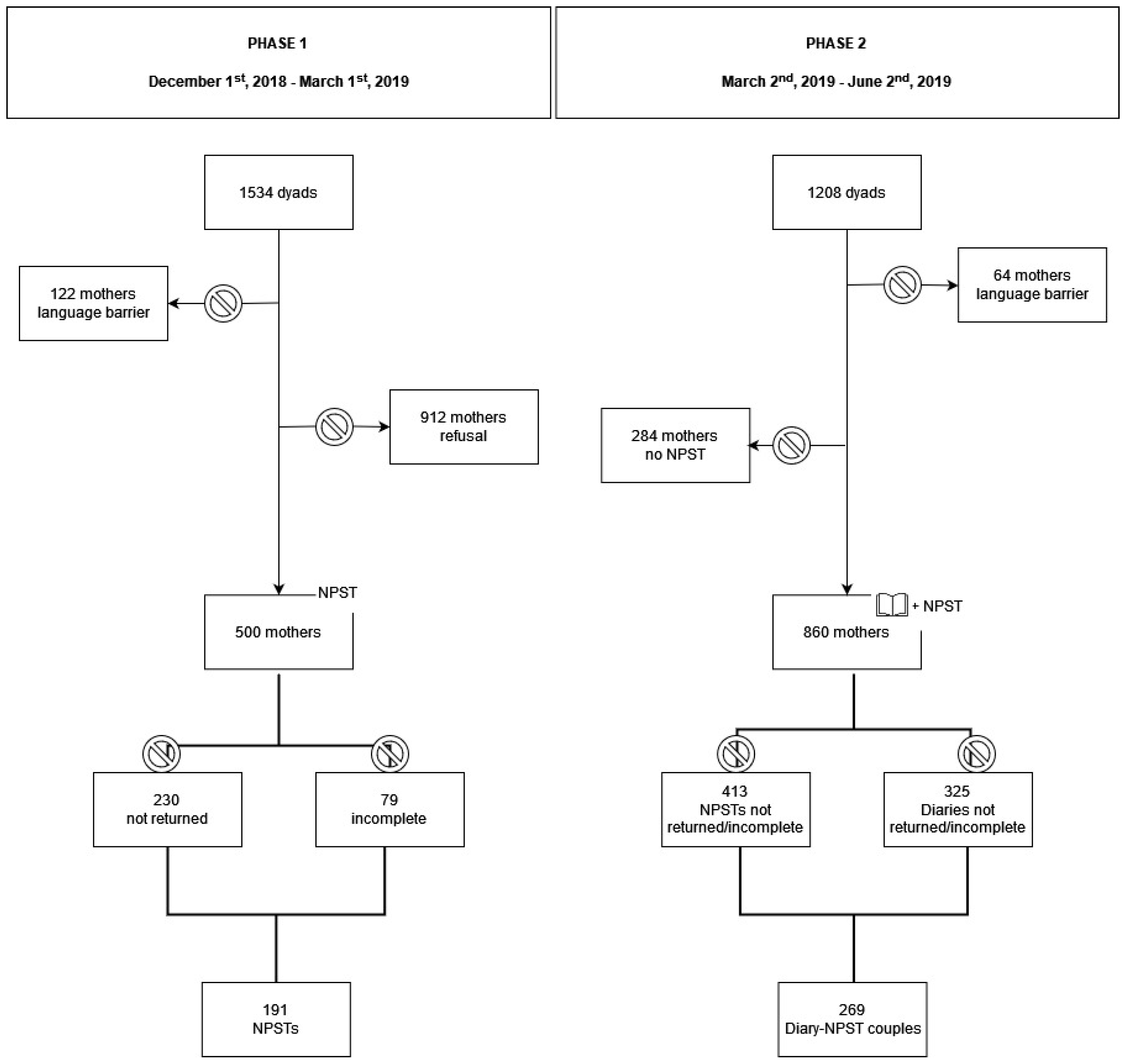
2.1. Study Design and Setting
2.2. Study Sample
2.3. Instruments
2.3.1. Post-Natal Educational Intervention
2.3.2. The Nurse–Parent Support Tool
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. The Diary
3.2. Breastfeeding Outcomes
4. The NPST
5. Discussion
6. Conclusions
Take-Home Messages
- The Diary was generally well accepted by mothers, who described the information received through it on breastfeeding and newborn care as clear and comprehensive. Such results prompted us to include the Diary as part of the perinatal assistance routinely offered at our post-natal unit;
- No difference in maternal perception of support from healthcare professionals during hospital stay emerged between the two phases. We consider this a positive result, since it suggests consistency in the assistance offered at our post-natal unit by our healthcare personnel, who strictly follows the BFHI indications, and which is therefore independent of the use of the Diary. The Diary should indeed be intended as an additional element of post-natal assistance, and not its core;
- Exclusive breastfeeding rates at discharge resulted in being higher in the mothers who did not receive the educational intervention (Phase 1). However, mothers in Phase 2 were older, more frequently Italian and recovering from a cesarean section than mothers in Phase 1. This, given the known lower exclusive breastfeeding rates reported in these populations, may be considered at least partly responsible for our results. More importantly, said difference in exclusive breastfeeding rates between the two phases lost statistical significance at 48 h. Therefore, a potential effect of the educational intervention in the long term cannot be excluded, also keeping in mind that the Diary consists of written material that mothers can reference once they get back home, usually far from healthcare professionals. Further studies, with a greater sample size and longer follow-up, are needed to confirm our hypothesis on a possible impact of the Diary on the duration of exclusive breastfeeding.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BFHI | Baby-Friendly Hospital Initiative |
| IBCLC | International Board-Certified Lactation Consultant |
| NICU | Neonatal Intensive Care Unit |
| NPST | Nurse–Parent Support Tool |
| UNICEF | United Nations Children Fund |
| WHO | World Health Organization |
References
- Benitz, W.E.; Committee on Fetus and Newborn, American Academy of Pediatrics. Hospital Stay for Healthy Term Newborn Infants. Pediatrics 2015, 135, 948–953. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). Exclusive Breastfeeding for Optimal Growth, Development and Health of Infants. Available online: http://www.who.int/elena/titles/exclusive_breastfeeding/en/ (accessed on 25 May 2019).
- Fewtrell, M.S.; Mohd Shukri, N.H.; Wells, J.C.K. “Optimising” Breastfeeding: What Can We Learn from Evolutionary, Comparative and Anthropological Aspects of Lactation? BMC Med. 2020, 18, 4. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.Y.; Ip, W.Y.; Choi, K.C. The Effect of a Self-Efficacy-Based Educational Programme on Maternal Breast Feeding Self-Efficacy, Breast Feeding Duration and Exclusive Breast Feeding Rates: A Longitudinal Study. Midwifery 2016, 36, 92–98. [Google Scholar] [CrossRef]
- Ortiz-Félix, R.E.; Cárdenas-Villarreal, V.M.; Miranda-Félix, P.E.; Guevara-Valtier, M.C. Impact of a Prenatal Education Intervention in Pregnant Women to Prevent Overweight in Infants. Gac. Med. Mex. 2021, 157, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Buchko, B.L.; Gutshall, C.H.; Jordan, E.T. Improving Quality and Efficiency of Postpartum Hospital Education. J. Perinat. Educ. 2012, 21, 238–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aksu, H.; Küçük, M.; Düzgün, G. The Effect of Postnatal Breastfeeding Education/Support Offered at Home 3 Days after Delivery on Breastfeeding Duration and Knowledge: A Randomized Trial. Available online: https://pubmed.ncbi.nlm.nih.gov/20608806/ (accessed on 8 February 2021).
- Seyyedi, N.; Rahmatnezhad, L.; Mesgarzadeh, M.; Khalkhali, H.; Seyyedi, N.; Rahimi, B. Effectiveness of a Smartphone-Based Educational Intervention to Improve Breastfeeding. Int. Breastfeed. J. 2021, 16, 70. [Google Scholar] [CrossRef]
- Cauble, J.S.; Herman, A.; Wick, J.; Goetz, J.; Daley, C.M.; Sullivan, D.K.; Hull, H.R. A Prenatal Group Based Phone Counseling Intervention to Improve Breastfeeding Rates and Complementary Feeding: A Randomized, Controlled Pilot and Feasibility Trial. BMC Pregnancy Childbirth 2021, 21, 521. [Google Scholar] [CrossRef]
- Wong, M.S.; Mou, H.; Chien, W.T. Effectiveness of Educational and Supportive Intervention for Primiparous Women on Breastfeeding Related Outcomes and Breastfeeding Self-Efficacy: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2021, 117, 103874. [Google Scholar] [CrossRef]
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO). Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services: The Revised Baby-Friendly Hospital Initiative; UNICEF: New York, NY, USA; World Health Organization (WHO): Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization (WHO). Ten Steps to Successful Breastfeeding (Revised 2018). Available online: http://www.who.int/nutrition/bfhi/ten-steps/en/ (accessed on 25 May 2019).
- World Health Organization (WHO); Department of Maternal, Newborn, Child and Adolescent Health. WHO Recommendations on Postnatal Care of the Mother and Newborn; World Health Organization (WHO): Geneva, Switzerland, 2013; ISBN 978-92-4-150664-9. [Google Scholar]
- World Health Organization (WHO). WHO Recommendations on Newborn Health; World Health Organization (WHO): Geneva, Switzerland, 2017. [Google Scholar]
- United Nations Children’s Fund (UNICEF). Guida all’Applicazione dei Passi; United Nations Children’s Fund (UNICEF): New York, NY, USA, 2016. [Google Scholar]
- Pregnancy, Childbirth, Postpartum and Newborn Care A Guide for Essential Practice; World Health Organization (WHO): Geneva, Switzerland, 2016; ISBN 978-92-4-154935-6.
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO). Manuale del Partecipante del Corso di 20 Ore per il Personale della Maternità; United Nations Children’s Fund (UNICEF): New York, NY, USA; World Health Organization (WHO): Geneva, Switzerland, 2009. [Google Scholar]
- Ministero della Salute. Allattare al Seno: Un Investimento per La Vita; Ministero della Salute: Rome, Italy, 2018.
- United Nations Children’s Fund (UNICEF). UK Assessment of Breastmilk Expression; United Nations Children’s Fund (UNICEF): New York, NY, USA, 2017. [Google Scholar]
- United Nations Children’s Fund (UNICEF). UK Baby Friendly Initiative Breastfeeding Checklist for Mothers; United Nations Children’s Fund (UNICEF): New York, NY, USA, 2016. [Google Scholar]
- Miles, M.S.; Carlson, J.; Brunssen, S. The nurse parent support tool. J. Pediatr. Nurs. 1999, 14, 44–50. [Google Scholar] [CrossRef]
- Montirosso, R.; Provenzi, L.; Calciolari, G.; Borgatti, R.; NEO-ACQUA Study Group. Measuring Maternal Stress and Perceived Support in 25 Italian NICUs. Acta Paediatr. 2012, 101, 136–142. [Google Scholar] [CrossRef]
- Colombo, L.; Crippa, B.L.; Consonni, D.; Bettinelli, M.E.; Agosti, V.; Mangino, G.; Bezze, E.N.; Mauri, P.A.; Zanotta, L.; Roggero, P.; et al. Breastfeeding Determinants in Healthy Term Newborns. Nutrients 2018, 10, 48. [Google Scholar] [CrossRef] [Green Version]
- Gomez-Pomar, E.; Blubaugh, R. The Baby Friendly Hospital Initiative and the Ten Steps for Successful Breastfeeding. A Critical Review of the Literature. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2018, 38, 623–632. [Google Scholar] [CrossRef]
- Gao, L.; Xie, W.; Yang, X.; Chan, S.W. Effects of an Interpersonal-Psychotherapy-Oriented Postnatal Programme for Chinese First-Time Mothers: A Randomized Controlled Trial. Int. J. Nurs. Stud. 2015, 52, 22–29. [Google Scholar] [CrossRef]
- Bryanton, J.; Beck, C.T.; Montelpare, W. Postnatal Parental Education for Optimizing Infant General Health and Parent-Infant Relationships. Cochrane Database Syst. Rev. 2013, 28, CD004068. [Google Scholar] [CrossRef] [PubMed]
- Morniroli, D.; Consales, A.; Riverso, L.; Colombo, L.; Bezze, E.N.; Sannino, P.; Zanotta, L.; Marchisio, P.; Mosca, F.; Plevani, L.; et al. Post-Partum Hospital Stay and Mothers’ Choices on Breastfeeding and Vaccines: A Chance We Should Not Miss. Front. Public Health 2021, 9, 662. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.K.; Edelman, A.; Jensen, J. Patient Satisfaction and the Impact of Written Material about Postpartum Contraceptive Decisions. Am. J. Obstet. Gynecol. 2003, 188, 1202–1204. [Google Scholar] [CrossRef] [PubMed]
- McKellar, L.; Pincombe, J.; Henderson, A. ‘Coming Ready or Not!’ Preparing Parents for Parenthood. Br. J. Midwifery 2009, 17, 160–167. [Google Scholar] [CrossRef]
- Currò, V.; Lanni, R.; Scipione, F.; Grimaldi, V.; Mastroiacovo, P. Randomised Controlled Trial Assessing the Effectiveness of a Booklet on the Duration of Breast Feeding. Arch. Dis. Child. 1997, 76, 500–503; Discussion 503–504. [Google Scholar] [CrossRef]
- Kronborg, H.; Vaeth, M.; Olsen, J.; Iversen, L.; Harder, I. Effect of Early Postnatal Breastfeeding Support: A Cluster-Randomized Community Based Trial. Acta Paediatr. 2007, 96, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Meedya, S.; Fernandez, R.; Fahy, K. Effect of Educational and Support Interventions on Long-Term Breastfeeding Rates in Primiparous Women: A Systematic Review and Meta-Analysis. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 2307–2332. [Google Scholar] [CrossRef]
- Araban, M.; Karimian, Z.; Karimian Kakolaki, Z.; McQueen, K.A.; Dennis, C.-L. Randomized Controlled Trial of a Prenatal Breastfeeding Self-Efficacy Intervention in Primiparous Women in Iran. J. Obstet. Gynecol. Neonatal Nurs. 2018, 47, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Osaki, K.; Hattori, T.; Toda, A.; Mulati, E.; Hermawan, L.; Pritasari, K.; Bardosono, S.; Kosen, S. Maternal and Child Health Handbook Use for Maternal and Child Care: A Cluster Randomized Controlled Study in Rural Java, Indonesia. J. Public Health 2019, 41, 170–182. [Google Scholar] [CrossRef] [PubMed]
- Mercer, R.T. Nursing Support of the Process of Becoming a Mother. J. Obstet. Gynecol. Neonatal Nurs. 2006, 35, 649–651. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.L.; Prinz, R.J. Potential Roles of Parental Self-Efficacy in Parent and Child Adjustment: A Review. Clin. Psychol. Rev. 2005, 25, 341–363. [Google Scholar] [CrossRef]
- Bernier, A.; Carlson, S.M.; Whipple, N. From External Regulation to Self-Regulation: Early Parenting Precursors of Young Children’s Executive Functioning. Child Dev. 2010, 81, 326–339. [Google Scholar] [CrossRef]
- Prior, E.; Santhakumaran, S.; Gale, C.; Philipps, L.H.; Modi, N.; Hyde, M.J. Breastfeeding after Cesarean Delivery: A Systematic Review and Meta-Analysis of World Literature. Am. J. Clin. Nutr. 2012, 95, 1113–1135. [Google Scholar] [CrossRef] [Green Version]
- Kitano, N.; Nomura, K.; Kido, M.; Murakami, K.; Ohkubo, T.; Ueno, M.; Sugimoto, M. Combined Effects of Maternal Age and Parity on Successful Initiation of Exclusive Breastfeeding. Prev. Med. Rep. 2015, 3, 121–126. [Google Scholar] [CrossRef] [Green Version]
- Istituto Nazionale di Statistica Gravidanza. Parto e Allattamento al Seno; Istituto Nazionale di Statistica Gravidanza: Milano, Italy, 2014. [Google Scholar]
- Smith, L.J. Impact of Birthing Practices on the Breastfeeding Dyad. J. Midwifery Womens Health 2007, 52, 621–630. [Google Scholar] [CrossRef]
- Dong, D.; Ru, X.; Huang, X.; Sang, T.; Li, S.; Wang, Y.; Feng, Q. A Prospective Cohort Study on Lactation Status and Breastfeeding Challenges in Mothers Giving Birth to Preterm Infants. Int. Breastfeed. J. 2022, 17, 6. [Google Scholar] [CrossRef]
- de Jager, E.; Skouteris, H.; Broadbent, J.; Amir, L.; Mellor, K. Psychosocial Correlates of Exclusive Breastfeeding: A Systematic Review. Midwifery 2013, 29, 506–518. [Google Scholar] [CrossRef]
- Piro, S.S.; Ahmed, H.M. Impacts of Antenatal Nursing Interventions on Mothers’ Breastfeeding Self-Efficacy: An Experimental Study. BMC Pregnancy Childbirth 2020, 20, 19. [Google Scholar] [CrossRef] [PubMed]
| Domain of Support | Items |
|---|---|
| Informational support | NPST 2, NPST 3, NPST 6, NPST 7, NPST 8, NPST 9, NPST 10, NPST 14, NPST 16 |
| Emotional support | NPST 1, NPST 12, NPST 13 |
| Parental esteem support | NPST 4, NPST 5, NPST 11, NPST 18 |
| Caregiving support | NPST 15, NPST 17, NPST 19, NPST 20, NPST 21 |
| Variable | Total Population (n = 460) | Phase 1 (n = 191) | Phase 2 (n = 269) | p |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Age (years) | 34 (31–37) | 34 (30–37) | 35 (32–38) | 0.01 |
| Foreign origin (%) | 52 (11.3) | 28 (14.7) | 24 (8.9) | 0.05 |
| University degree/PhD (%) | 309 (67.2) | 124 (64.9) | 185 (68.8) | 0.38 |
| Single parent (%) | 18 (3.9) | 7 (3.7) | 11 (4.1) | 0.81 |
| Clinical characteristics | ||||
| Primiparity (%) | 249 (54.1) | 106 (55.5) | 143 (53.2) | 0.62 |
| Cesarean section (%) | 161 (35) | 61 (31.9) | 100 (37.2) | 0.0005 |
| Neonatal characteristics | ||||
| Male sex (%) | 244 (53) | 106 (55.5) | 138 (51.3) | 0.37 |
| Gestational age (weeks) | 39 (38–40) | 39 (38–40) | 39 (38–40) | 0.56 |
| Birth weight (g) | 3305 (3060–3570) | 3350 (3050–3590) | 3300 (3080–3550) | 0.62 |
| % | |
| Diary Delivery | |
| Delivery room | 51.72 |
| Post-natal unit | 48.28 |
| Skin-to-Skin Contact | |
| Yes | 93.53 |
| No | 6.47 |
| Beginning | |
| Within 5 min of birth | 64.85 |
| Between 3 and 60 min from birth | 22.53 |
| After 60 min from birth | 12.63 |
| Duration | |
| ≥60 min | 76.12 |
| <60 min | 23.88 |
| Quality of the information received | |
| Clear and comprehensive | 94.01 |
| Need more information | 4.93 |
| Newborn’s Feeding Cues | |
| Quality of the information received | |
| Clear and comprehensive | 94.93 |
| Need more information | 4.35 |
| Continuous Rooming-In | |
| Yes | 64.75 |
| No | 35.25 |
| Reasons for interruption of rooming-in | |
| Newborn’s clinical reasons | 43.08 |
| Maternal rest | 49.74 |
| Both | 7.18 |
| Quality of the information received | |
| Clear and comprehensive | 91.74 |
| Need more information | 7.02 |
| Bowel Movements and Diuresis | |
| Quality of the information received | |
| Clear and comprehensive | 92.9 |
| Need more information | 7.1 |
| Breastfeeding Observation | |
| Maternal general conditions | |
| Relaxed and at ease | 89.78 |
| Tense and uncomfortable | 9.49 |
| Mixed feelings | 0.73 |
| Neonatal general conditions | |
| Wellbeing | 90.53 |
| Uneasiness | 1.40 |
| A combination of the two | 8.07 |
| Newborn’s position | |
| Adequate | 79.42 |
| Not adequate | 2.88 |
| Not sure | 17.70 |
| Latch-on | |
| Adequate | 75.45 |
| Not adequate | 7.59 |
| Not sure | 16.96 |
| Suction | |
| Adequate | 58.55 |
| Not adequate | 3.85 |
| Not sure | 37.61 |
| Breast Examination | |
| Breast conditions | |
| No change observed | 34.44 |
| Normal changes observed | 49.79 |
| Abnormal changes observed | 15.77 |
| Nipple pain | |
| Yes | 60.17 |
| No | 39.83 |
| Nipple redness | |
| No | 60.58 |
| Faded | 25.73 |
| Marked | 13.69 |
| Variable | Total Population (n = 460) | Phase 1 (n = 191) | Phase 2 (n = 269) | p |
|---|---|---|---|---|
| Exclusive breastfeeding at discharge, n (%) | 349 (75.9%) | 154 (80.6%) | 195 (72.5%) | 0.04 |
| Exclusive breastfeeding at 48 h post-discharge, n (%) | 347 (75.4%) | 149 (78%) | 198 (73.6%) | 0.28 |
| NPST | Total Population (n = 460) | Phase 1 (n = 191) | Phase 2 (n = 269) | p |
|---|---|---|---|---|
| Total score | 4.05 (3.52–4.48) | 4.05 (3.57–4.48) | 4.05 (3.48–4.48) | 0.78 |
| Informational support | 4 (3.33–4.44) | 4 (3.44–4.44) | 4 (3.33–4.44) | 0.86 |
| Emotional support | 3.67 (3–4.33) | 3.67 (3–4.33) | 3.67 (3–4.33) | 0.49 |
| Appraisal/parental esteem support | 4 (3.25–4.5) | 4 (3.25–4.75) | 4 (3.25–4.5) | 0.75 |
| Caregiving support | 4.4 (3.8–4.8) | 4.4 (3.8–4.8) | 4.4 (3.8–4.8) | 0.49 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Consales, A.; Colombo, L.; Zanotta, L.; Morniroli, D.; Sannino, P.; Rampini, S.; Piccoli, G.; Donghi, M.; Marchisio, P.; Mosca, F.; et al. Pilot Feasibility Study of a Hospital-Based Post-Natal Educational Intervention on New Mothers in a BFHI-Compliant Tertiary Referral Center for Neonatal Care. Int. J. Environ. Res. Public Health 2022, 19, 2020. https://doi.org/10.3390/ijerph19042020
Consales A, Colombo L, Zanotta L, Morniroli D, Sannino P, Rampini S, Piccoli G, Donghi M, Marchisio P, Mosca F, et al. Pilot Feasibility Study of a Hospital-Based Post-Natal Educational Intervention on New Mothers in a BFHI-Compliant Tertiary Referral Center for Neonatal Care. International Journal of Environmental Research and Public Health. 2022; 19(4):2020. https://doi.org/10.3390/ijerph19042020
Chicago/Turabian StyleConsales, Alessandra, Lorenzo Colombo, Lidia Zanotta, Daniela Morniroli, Patrizio Sannino, Serena Rampini, Giulia Piccoli, Michaela Donghi, Paola Marchisio, Fabio Mosca, and et al. 2022. "Pilot Feasibility Study of a Hospital-Based Post-Natal Educational Intervention on New Mothers in a BFHI-Compliant Tertiary Referral Center for Neonatal Care" International Journal of Environmental Research and Public Health 19, no. 4: 2020. https://doi.org/10.3390/ijerph19042020
APA StyleConsales, A., Colombo, L., Zanotta, L., Morniroli, D., Sannino, P., Rampini, S., Piccoli, G., Donghi, M., Marchisio, P., Mosca, F., Plevani, L., & Giannì, M. L. (2022). Pilot Feasibility Study of a Hospital-Based Post-Natal Educational Intervention on New Mothers in a BFHI-Compliant Tertiary Referral Center for Neonatal Care. International Journal of Environmental Research and Public Health, 19(4), 2020. https://doi.org/10.3390/ijerph19042020







