Effects of Healthcare Policies and Reforms at the Primary Level in China: From the Evidence of Shenzhen Primary Care Reforms from 2018 to 2019
Abstract
:1. Introduction
2. Literature View
2.1. Evaluation of the Outcomes of China’s Healthcare Reform
2.2. Exploration of the Factors Affecting the Effectiveness of Healthcare Reform
3. Research Backgrounds and Research Design
3.1. Research Backgrounds
3.2. Research Framework and Hypothesis
3.3. Data Collection and Collation
4. Analysis Results
4.1. Characteristics of the Development of Shenzhen Primary Care Center
4.2. Comparative Analysis of the Development of the Two Types of Primary Care Centers in Shenzhen
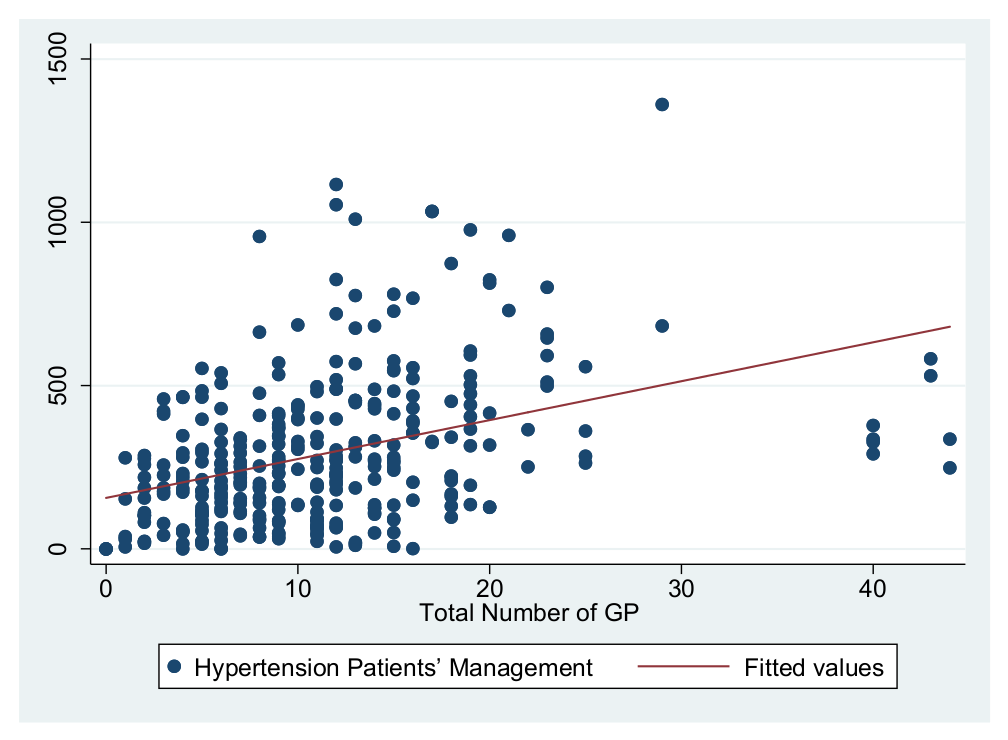
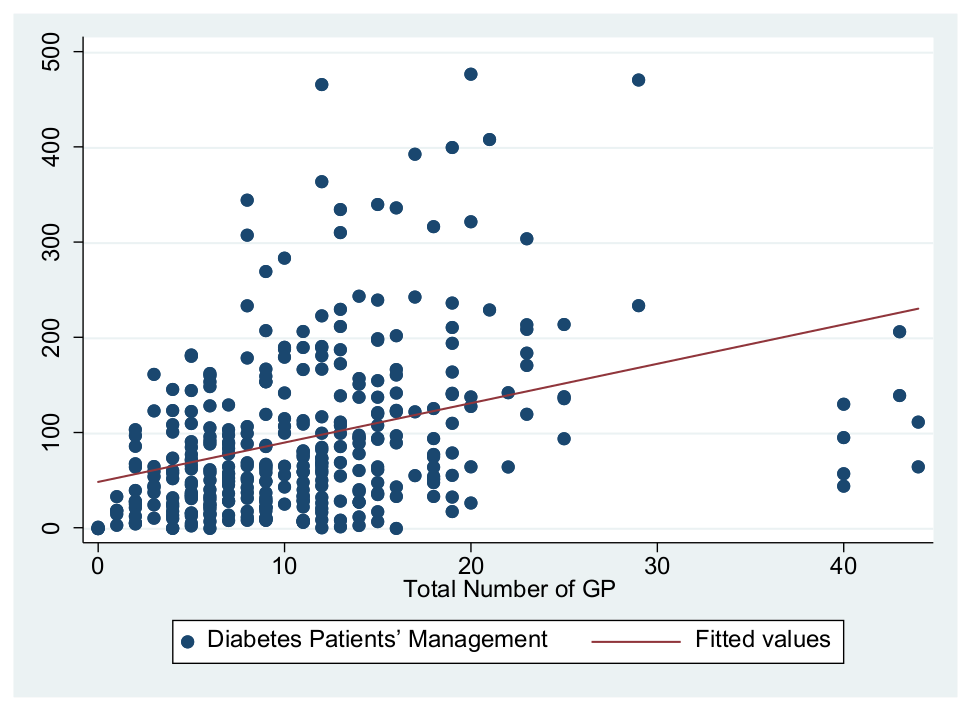
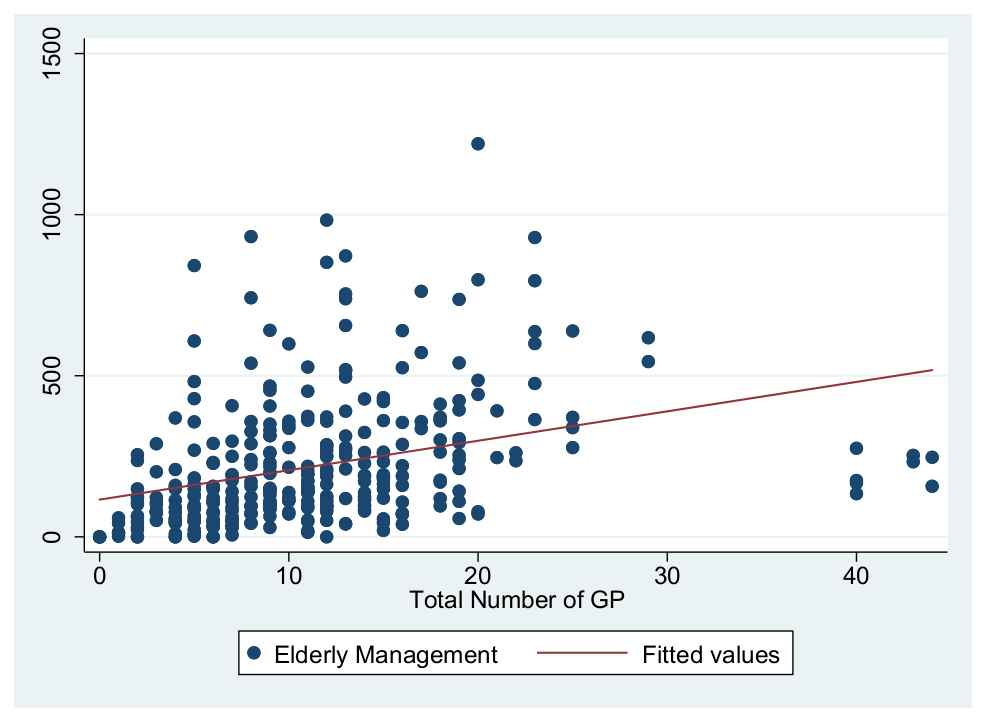
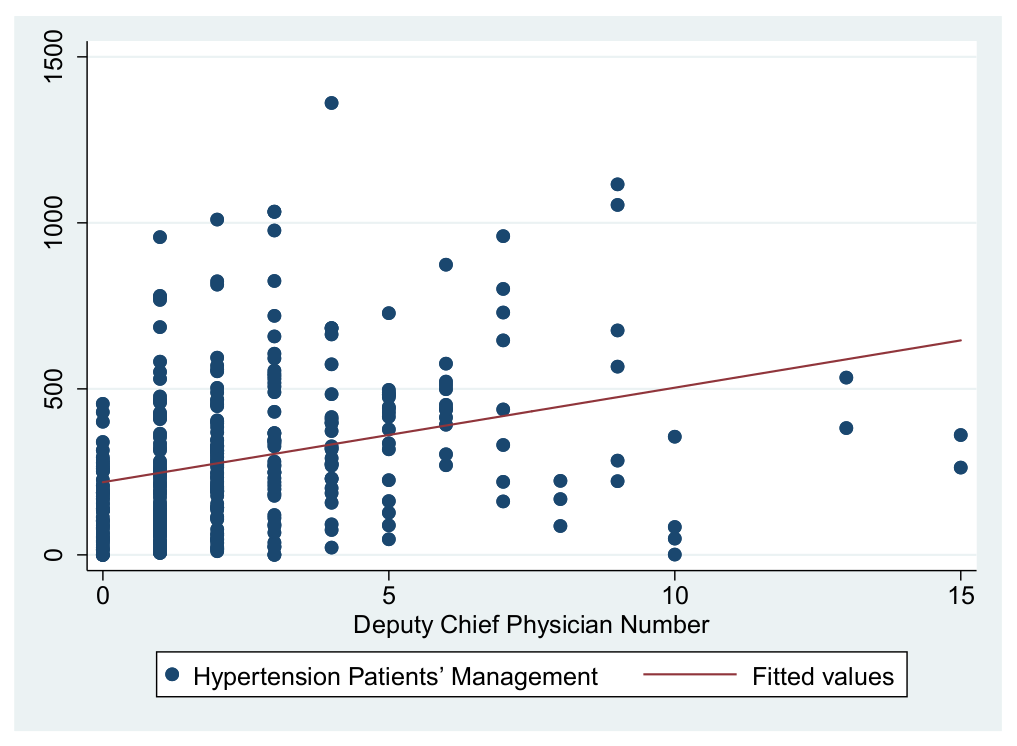
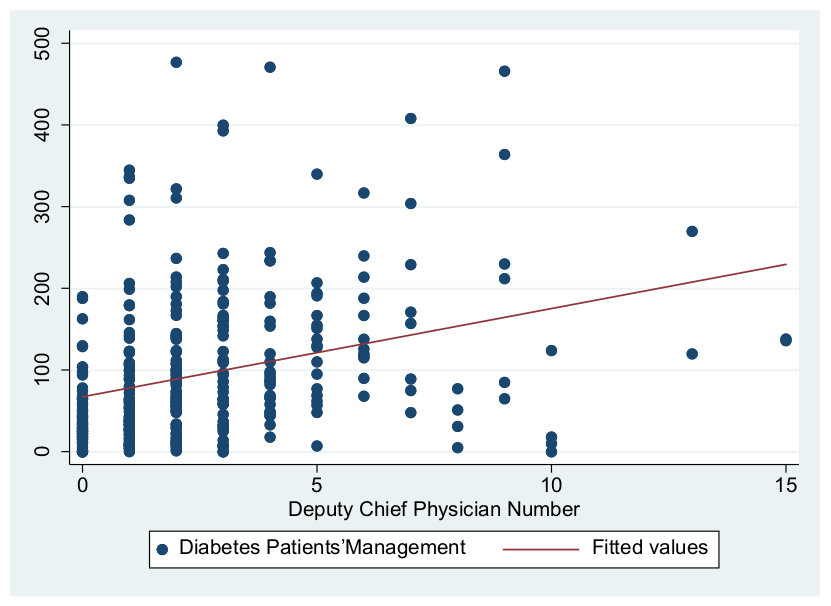
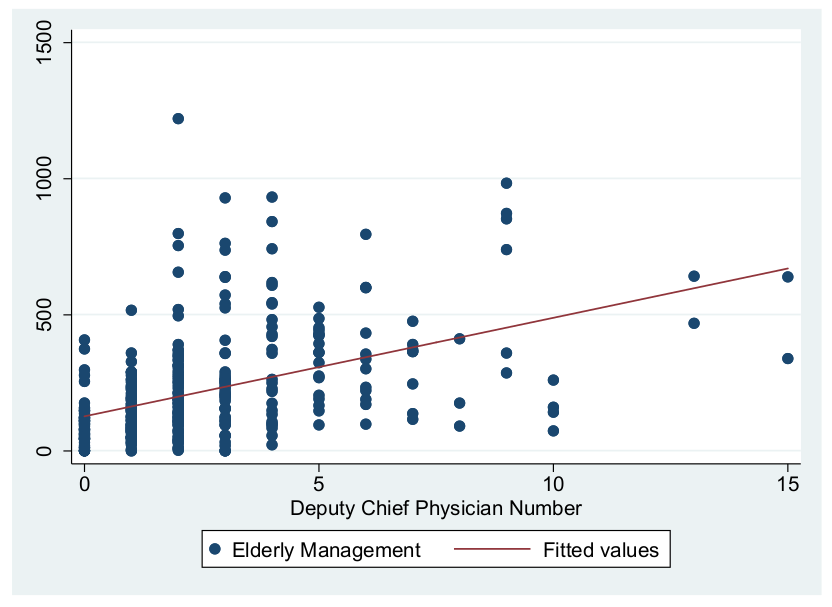
4.3. Correlation Analysis
4.4. Results of the Model 1–Model 3 Regression Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huang, J.L.; Zhu, Q.; Guo, J. Can Health Disparity Be Eliminated? The Role of Family Doctor Played in Shanghai, China. Int. J. Environ. Res. Public Health 2020, 17, 5548. [Google Scholar] [CrossRef] [PubMed]
- Song, X.Q.; Wei, Y.P.; Deng, W.; Zhang, S.Y.; Zhou, P.; Liu, Y.; Wan, J.L. Spatio-Temporal Distribution, Spillover Effects and Influences of China’s Two Levels of Public Healthcare Resources. Int. J. Environ. Res. Public Health 2019, 16, 582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, S.H.; Yuan, B.B.; Zhang, L.Y.; Cheng, G.; Zhu, W.M.; Hou, Z.Y.; He, L.; Ma, X.C.; Meng, Q.Y. Increased Inequalities in Health Resource and Access to Healthcare in Rural China. Int. J. Environ. Res. Public Health 2019, 16, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, J.; Rozelle, S.; Xu, Q.; Yu, N.; Zhou, T.S. Social Engagement and Elderly Health in China: Evidence from the China Health and Retirement Longitudinal Survey (CHARLS). Int. J. Environ. Res. Public Health 2019, 16, 278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yip, W.N.; Fu, H.Q.; Chen, A.T.; Zhai, T.M.; Jian, W.Y.; Xu, R.M.; Pan, J.; Hu, M.; Zhou, Z.L.; Chen, Q.L.; et al. 10 years of health-care reform in China: Progress and gaps in Universal Health Coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [CrossRef]
- Shu, Z.; Liu, Y.; Li, M.; Li, J. The effects of health system reform on medical services utilization and expenditures in China in 2004–2015. Int. Health 2021, 13, 640–647. [Google Scholar] [CrossRef]
- Ran, Y.F.; Gao, H.X.; Han, D.; Hou, G.L.; Chen, Y.C.; Zhang, Y. Comparison of inpatient distribution amongst different medical alliances in a county: A longitudinal study on a healthcare reform in rural China. Int. J. Equity Health 2020, 19, 1–9. [Google Scholar] [CrossRef]
- Wang, Y.L.; Li, H.W.; Yu, S.X.; Zhang, P. The development course and prospect of China’s medical and health policy in the 100 years under the perspective of policy tools. Sci. Technol. Rev. 2021, 39, 82–89. [Google Scholar]
- Meng, Q.; Fang, H.; Liu, X.; Yuan, B.; Xu, J. Consolidating the social health insurance schemes in China: Towards an equitable and efficient health system. Lancet 2015, 386, 1484–1492. [Google Scholar] [CrossRef]
- Liu, G.G.; Vortherms, S.A.; Hong, X. China’s Health Reform Update. Annu. Rev. Public Health 2017, 38, 431–448. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Fu, H. China’s health care system reform: Progress and prospects. Int. J. Health Plann. Manage. 2017, 32, 240–253. [Google Scholar] [CrossRef] [PubMed]
- Miao, J.; Wu, X.; Sun, X. Neighborhood, social cohesion, and the Elderly’s depression in Shanghai. Soc. Sci. Med. 2018, 229, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Ocasio, W. Attention to attention. Organ. Sci. 2011, 22, 1286–1296. [Google Scholar] [CrossRef] [Green Version]
- Simon, H.A. Administrative Behavior: A Study of Decision-Making Processes in Administrative Organization; Macmillan: New York, NY, USA, 1947. [Google Scholar]
- Cohen, M.D.; March, J.G.; Olsen, J.P. A Garbage Can Model of Organizational Choice. Adm. Sci. Q. 1972, 17, 1. [Google Scholar] [CrossRef] [Green Version]
- Weick, K.E.; Kiesler, C.A. The Social Psychology of Organizing; Random House: New York, NY, USA, 1979. [Google Scholar]
- Husain, L.; Bloom, G.; Xiao, Y. Building policy capacity for managing rapid, complex change in China’s health system. Policy Soc. 2021, 40, 1–12. [Google Scholar] [CrossRef]
- World Bank. World Development Report 1993: Investing in Health. Popul. Dev. Rev. 1994, 16, 129–131. [Google Scholar]
- Ma, B.B.; Du, P. How the Health Services Accessibility to Influence People’s Public Medical Fairness-Based on the Analysis of the Questionnaire in the 7 Provinces and Cities. J. Gansu Adm. Inst. 2019, 1, 56–63. [Google Scholar]
- Zhao, D.Y. The Value Conflict in the Process of Policy-making: The Experiences Reaped from China’s Reform of Medical and Health Work. Manag. World 2008, 10, 41–52. [Google Scholar]
- Chen, J.Q.; Xu, S.; Gao, J. The Mixed Effect of China’s New Health Care Reform on Health Insurance Coverage and the Efficiency of Health Service Utilisation: A Longitudinal Approach. Int. J. Environ. Res. Public Health 2020, 17, 1782. [Google Scholar] [CrossRef] [Green Version]
- Zhao, D.Y.; Liang, H. Behavior Model of Stakeholder and Rules incremental Adjusting during Policy Process-From Shanghai Experience of Reconstructing Urban New Medical Service System. J. Public Manag. 2009, 6, 50–58. [Google Scholar]
- Kang, G.; Zhang, H. China’s Health Care System: Something is Wrong and How We Can Fix It. Am. J. Med. 2020, 133, e58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lai, Y.; Chen, S.; Li, M.; Ung, C.O.L.; Hu, H. Policy Interventions, Development Trends, and Service Innovations of Internet Hospitals in China: Documentary Analysis and Qualitative Interview Study. J. Med. Int. Res. 2021, 23, e22330. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Zhang, J.; Xu, Z.; Cong, X.; Zhu, Z. The efficiency of provincial government healthcare expenditure after China’s new healthcare reform. PLoS ONE 2021, 16, e0258274. [Google Scholar] [CrossRef]
- Mao, W.; Tang, Y.; Tran, T.; Pender, M.; Khanh, P.N.; Tang, S. Advancing universal health coverage in China and Vietnam: Lessons for other countries. BMC Public Health 2020, 20, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Yan, C.W. Changes and logics of medical and health policies during the 70 years since the foundation of new China. Adm. Trib. 2019, 26, 31–37. [Google Scholar]
- Guo, Q.; Luo, K.; Hu, R. The Spatial Correlations of Health Resource Agglomeration Capacities and Their Influencing Factors: Evidence from China. Int. J. Environ. Res. Public Health 2020, 17, 8075. [Google Scholar] [CrossRef]
- Zhou, W.; Yu, Y.; Zhao, X.; Xiao, S.; Chen, L. Evaluating China’s mental health policy on local-level promotion and implementation: A case study of Liuyang Municipality. BMC Public Health 2019, 19, 24. [Google Scholar] [CrossRef] [Green Version]
- Yue, J.L.; Huang, B.H. The Healthy China Strategy and China’s Social Policy Innovation. Zhongshan Da Xue Xue Bao (Soc. Sci. Ed.) 2020, 60, 179–187. [Google Scholar]
- Karasiewicz, M.; Chawlowska, E.; Lipiak, A.; Wieckowska, B. A Step towards Understanding and Tackling Health Inequalities: The Use of Secondary Prevention Services and the Need for Health Promotion in a Rural Setting. Int. J. Environ. Res. Public Health 2021, 18, 8492. [Google Scholar] [CrossRef]
- Islam, M.R.; Rahman, M.S.; Rahman, M.M.; Nomura, S.; De Silva, A.; Lanerolle, P.; Rahman, M.M. Reducing childhood malnutrition in Bangladesh: The importance of addressing socio-economic inequalities. Public Health Nutr. 2019, 23, 72–82. [Google Scholar] [CrossRef]
- Ali, B.; Chauhan, S. Inequalities in the utilisation of maternal health Care in Rural India: Evidence from National Family Health Survey III & IV. BMC Public Health 2021, 20, 1027. [Google Scholar]
- Hosokawa, R.; Ojima, T.; Myojin, T.; Aida, J.; Kondo, K.; Kondo, N. Associations between Healthcare Resources and Healthy Life Expectancy: A Descriptive Study across Secondary Medical Areas in Japan (vol 17, 6301, 2020). Int. J. Environ. Res. Public Health 2020, 17, 6301. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Zhou, Z.L.; Si, Y.F.; Xu, Y.J.; Shen, C.; Wang, Y.Y.; Wang, X. Unequal distribution of health human resource in mainland China: What are the determinants from a comprehensive perspective? Int. J. Equity Health 2018, 17, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friel, S.; Marmot, M.G. Action on the Social Determinants of Health and Health Inequities Goes Global. Annu. Rev. Public Health 2011, 32, 225–236. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.Q.; Zheng, J.; Xu, L.Z.; Wu, H.T. Equity of Health Services Utilisation and Expenditure among Urban and Rural Residents under Universal Health Coverage. Int. J. Environ. Res. Public Health 2021, 18, 593. [Google Scholar] [CrossRef]
- Sosa Díaz, M.J. Emergency Remote Education, Family Support and the Digital Divide in the Context of the COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2021, 18, 7956. [Google Scholar] [CrossRef]
- Wang, Y.; Qian, D.F.; Cao, J.L.; Zhao, P.P.; Wang, M.N. Knowledge and Evaluation of Hierarchical Diagnosis and Treatment System among Outpatients. Chin. Gen. Pract. 2019, 22, 1106–1111. [Google Scholar]
- Tang, S.L.; Li, P.; Wang, H.; Tang, K.A. Optimization Research on Hierarchical Diagnosis System under the Background of Medical Alliance Construction: Based on SD Causal Loop Diagram. Chin. Health Econ. 2019, 38, 20–23. [Google Scholar]
- Sutarsa, I.N.; Kasim, R.; Slimings, C.; Bain-Donohue, S.; Barnard, A. Effects of employing primary care doctors in hospital to improve the quality of care and health outcomes of rural patients: A systematic scoping review. Aust. J. Rural Health 2021, 29, 492–501. [Google Scholar] [CrossRef]
- Wang, X.; Yang, H.; Duan, Z.; Pan, J. Spatial accessibility of primary healthcare in China: A case study in Sichuan Province. Soc. Sci. Med. 2018, 209, 14–24. [Google Scholar] [CrossRef]
- Myint, C.Y.; Pavlova, M.; Thein, K.N.; Groot, W. A systematic review of the health-financing mechanisms in the Association of Southeast Asian Nations countries and the People’s Republic of China: Lessons for the move towards universal health coverage. PLoS One 2019, 14, e0217278. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.Y.; Shaw, I. The impact of out-of-pocket payments on healthcare inequity: The case of national health insurance in South Korea. Int. J. Environ. Res. Public Health 2014, 7, 7304–7318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, H.P.; Chai, X.Y.; Sheng, J.Y.; Wu, X.Y. Research on the precision service model combining big data medical care and smart elderly care under the Regional Medical Cluster model. Chin. Hosp. 2021, 25, 1–3. [Google Scholar]
- Zhang, X.H. Influence of ‘Chang ting Model’ of Primary Healthcare Reform on the Development of Township Health Hospital —A Case Study of Chang ting County. Fujian Agric. For. Univ. 2020, 5. [Google Scholar] [CrossRef]
- Van Panhuis, W.G.; Paul, P.; Emerson, C.; Grefenstette, J.; Wilder, R.; Herbst, A.J.; Heymann, D.; Burke, D.S. A systematic review of barriers to data sharing in public health. BMC Public Health 2014, 14, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, J.J.; Liu, Y.; Ren, Q.Q. Application of Digital Information Technology in General Practice. Chin. Gen. Pract. 2015, 18, 1488–1492. [Google Scholar]
- Li, L.Q.; Li, J.; Lin, J. Thought of Exerting Regional Function of the Hospital Under the Background of Hierarchical Diagnosis and Treatment. Chin. Hosp. Manag. 2016, 36, 8–9. [Google Scholar]
- Kong, Y.W.; Cao, J.; Zheng, Y.F.; Chen, L.S.; Zhang, M.J.; Zou, Z.H.; Lin, E. “Down-referral Being Difficult” Phenomenon in the Two-way Referral Based on Stakeholder Theory. Chin. Gen. Pract. 2017, 20, 1173–1176. [Google Scholar]
- Mao, Y.; Luo, X.; Chen, X.; Xie, T.; Zhang, Z.R. Current situation and countermeasures of two-way referral between wound healing department and community health system. Chin. J. Burn. 2012, 28, 455–457. [Google Scholar]
- Li, X.; Krumholz, H.M.; Yip, W.; Cheng, K.K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Li, C.; Lu, J.; Su, M.; et al. Quality of primary healthcare in China: Challenges and recommendations. Lancet 2020, 395, 1802–1812. [Google Scholar] [CrossRef]
| Dimension | Category | Code |
|---|---|---|
| Primary Care Service Effects | Management number of hypertension patients | Number of hypertension patients managed |
| Management number of diabetic patients | Number of health management of diabetes patients | |
| Management number of the elderly | Number of elderly health management | |
| Service Levels | Performance appraisal | Compensation Evaluation mechanism |
| Medical revenue | Annual outpatient expenses, Annual gross medical income | |
| Infrastructure | Debt resolving, Infrastructure Construction, Telemedicine Construction | |
| Pharmaceuticals management | Pharmaceuticals price quality management, pharmaceuticals regulatory, pharmaceutical consumables, drug circulation, the catalogue of medicine | |
| Medical Level | Number of GP practitioners | Establishment general practitioners’ management, local rural talent, general practitioners, the establishment of a general practitioner training mechanism, general practitioner management, general practitioner ad hoc posts, general practitioner titles |
| Medical education | Health education, medical teaching coordination, enrollment structure | |
| Talent Level | Deputy Chief Physician of the Center | Innovative scientific research management mechanism, coordinate the allocation of high-level personnel training funds |
| Information Sharing | Information technology | Internet medical care, Two-way referral |
| Dimensions | Primary Care Service Effects | Service Levels | Medical Level | Talent Level | Information Sharing | Total |
|---|---|---|---|---|---|---|
| Frequency | 75 | 71 | 33 | 5 | 8 | 192 |
| Proportion | 39.06% | 36.98% | 17.18% | 2.61% | 4.17% | 100.00% |
| Dimensions | Indexes |
|---|---|
| Medical Level | Number of GP practitioners |
| Talent Level | Deputy Chief Physician of the Center |
| Service Levels | Annual outpatient expenses and annual gross medical income |
| Information Sharing | Two-way referral |
| Primary Care Service Effects | Management number of hypertension patients Management number of diabetic patients Management number of the elderly |
| Variables | Indicators | Index Description | |
|---|---|---|---|
| Dependent Variables | Primary Care Service Effects | Management number of hypertension patients | Number of hypertension patients managed as specification |
| Management number of diabetic patients | Number of health management of diabetes patients as required | ||
| Management number of the elderly | Number of elderly health management according to specifications | ||
| Independent Variables | Medical Level | Number of GP practitioners | Number of GP practitioners |
| Talent Level | Number of Deputy Chief Physician of the Center | Number of Deputy Chief Physician of the Center | |
| Control variables | Service Levels | Annual outpatient expenses | |
| Annual gross medical income | Including the fiscal revenue | ||
| Information Sharing | Annual number of two-way referrals | Number of Trans cases |
| Variable Type | Variable Name | Observation Value | Mean | Standard Difference | Minimum Value | Maximum Value |
|---|---|---|---|---|---|---|
| Primary Care Service Effects | Hypertension standard management number | 336 | 290.58 | 228.62 | 0.00 | 1361.00 |
| Diabetes Management | 339 | 94.55 | 87.92 | 0.00 | 477.00 | |
| Standardized management number of the elderly | 338 | 218.35 | 199.31 | 0.00 | 1220.00 | |
| Medical Level | Number of GP practitioners | 348 | 11.08 | 7.38 | 0.00 | 44.00 |
| Talent Level | Number of doctors, deputy chief physician of the center | 346 | 2.52 | 2.53 | 0.00 | 15.00 |
| Service Levels | Outpatient expenses | 338 | 318,182.90 | 228,592.80 | 0.00 | 983,300.00 |
| Total medical income | 338 | 407,174.30 | 249,310.30 | 0.00 | 991,972.00 | |
| Number of outpatients | 338 | 50,384.45 | 37,408.76 | 4.00 | 226,443.00 | |
| Information Sharing | Number of bidirectional referrals | 319 | 4092.84 | 4677.66 | 1.00 | 44,310.00 |
| Area | Pingshan District | Bao’an District | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | Maximum Value | Minimum Value | N | Mean | Maximum Value | Minimum Value | N | |
| Number of general practitioners | 13.31 | 44.00 | 2.00 | 70 | 10.52 | 40.00 | 0.00 | 278 |
| Number of deputy chief physician of the center | 1.43 | 8.00 | 0.00 | 70 | 2.80 | 15.00 | 0.00 | 276 |
| Outpatient expenses | 285,159.70 | 983,300 | 300.39 | 67 | 326,347.40 | 974,599.00 | 0.00 | 271 |
| Total medical income | 357,312.30 | 989,180 | 449.75 | 67 | 419,501.80 | 991,972.00 | 0.00 | 271 |
| Number of two-way referrals | 3032.18 | 14,255.00 | 1.00 | 61 | 4343.61 | 44,310.00 | 1.00 | 258 |
| Management number of hypertension patients | 157.26 | 582.00 | 6.00 | 65 | 322.56 | 1361.00 | 0.00 | 271 |
| Management number of diabetic patients | 49.54 | 206.00 | 0.00 | 65 | 105.23 | 477.00 | 0.00 | 274 |
| Management number of the elderly | 115.72 | 412.00 | 0.00 | 65 | 242.78 | 1220.00 | 0.00 | 273 |
| Total Number of GP | Deputy Chief Physician Number | Hospital Type | Outpatient Expenses | Hospital Gross Income | Two-Way Referral Number | |
|---|---|---|---|---|---|---|
| Total number of GP | 1.00 | |||||
| Deputy chief physician number | 0.32 | 1.00 | ||||
| Hospital type | −0.16 | 0.23 | 1.00 | |||
| Outpatient expenses | 0.29 | 0.27 | 0.18 | 1.00 | ||
| Hospital gross income | 0.09 | -0.04 | 0.14 | 0.24 | 1.00 | |
| Two-way referral number | 0.31 | 0.16 | 0.11 | 0.25 | 0.08 | 1.00 |
| Variable | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1a | Model 1b | Model 1c | Model 2a | Model 2b | Model 2c | Model 3a | Model 3b | Model 3c | |
| Hypertension Patients’ Management | Diabetes Patients’ Management | Elderly Management | Hypertension Patients’ Management | Diabetes Patients’ Management | Elderly Management | Hypertension Patients’ Management | Diabetes Patients’ Management | Elderly Management | |
| Total number of GP | 8.02 *** | 2.59 *** | 7.62 *** | 6.92 *** | 2.03 *** | 4.83 *** | |||
| (1.48) | (0.61) | (1.47) | (1.56) | (0.63) | (1.48) | ||||
| Deputy chief physician number | 15.80 *** | 6.67 *** | 28.13*** | 9.47 ** | 4.81 *** | 23.71 *** | |||
| (4.24) | (1.71) | (3.97) | (4.36) | (1.79) | (4.14) | ||||
| Hospital type | 156.50 *** | 51.51 *** | 133.54 *** | 98.75 *** | 30.84 *** | 62.29 ** | 138.84 *** | 42.59 *** | 90.28 *** |
| (26.74) | (11.03) | (26.53) | (27.09) | (10.96) | (25.38) | (27.8) | (11.42) | (26.42) | |
| Outpatient expenses | 43.47 *** | 19.72 *** | 56.04 *** | 50.21 *** | 20.70 *** | 52.18 *** | 38.87 *** | 17.37 *** | 44.26*** |
| (13.61) | (5.62) | (13.50) | (13.88) | (5.62) | (13.01) | (13.72) | (5.64) | (13.04) | |
| Hospital gross income | −3.14 | −1.07 | −13.61 | 7.86 | 3.21 | 3.20 | 1.62 | 1.38 | −1.16 |
| (14.17) | (5.84) | (14.06) | (14.64) | (5.928) | (13.72) | (14.29) | (5.87) | (13.58) | |
| Two-way referral number | 0.02 *** | 0.01 *** | 0.003 | 0.02 *** | 0.007 *** | 0.005 ** | 0.02 *** | 0.01 *** | 0.003 |
| (0.002) | (0.001) | (0.002) | (0.002) | (0.0009) | (0.002) | (0.002) | (0.0009) | (0.002) | |
| Constant | −487.65 ** | −227.87 ** | −504.99 ** | −624.00 *** | −268.21 *** | −604.30 *** | −488.74 ** | −228.55 *** | −509.87 ** |
| (215.00) | (88.68) | (213.28) | (218.16) | (88.30) | (204.43) | (213.99) | (87.93) | (203.37) | |
| Observations | 317 | 317 | 317 | 316 | 316 | 316 | 316 | 316 | 316 |
| R2 | 0.412 | 0.335 | 0.251 | 0.384 | 0.329 | 0.299 | 0.421 | 0.351 | 0.323 |
| Variable | Model 4 | Model 5 | Model 6 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 4a | Model 4b | Model 4c | Model 5a | Model 5b | Model 5c | Model 6a | Model 6b | Model 6c | |
| Hypertension Patients’ Management | Diabetes Patients’ Management | Elderly Management | Hypertension Patients’ Management | Diabetes Patients’ Management | Elderly Management | Hypertension Patients’ Management | Diabetes Patients’ Management | Elderly Management | |
| Total number of GP | 6.62 *** | 2.13 *** | 5.56 *** | 5.72 *** | 1.70 *** | 3.30 ** | |||
| (1.40) | (0.57) | (1.41) | (1.43) | (0.59) | (1.38) | ||||
| Deputy chief physician number | 14.93 *** | 6.30 *** | 28.55 *** | 10.72 ** | 5.04 *** | 26.12 *** | |||
| (4.15) | (1.68) | (3.93) | (4.19) | (1.72) | (4.03) | ||||
| Hospital type × Two-way referral number | 0.02 *** | 0.008 *** | 0.009 *** | 0.02 *** | 0.008 *** | 0.007 *** | 0.02 *** | 0.007 *** | 0.007 *** |
| (0.002) | (0.0009) | (0.002) | (0.002) | (0.0008) | (0.002) | (0.002) | (0.0009) | (0.002) | |
| Outpatient expenses | 64.17 *** | 26.54 *** | 68.03 *** | 67.41 *** | 26.32 *** | 57.00 *** | 57.38 *** | 23.33 *** | 51.22 *** |
| (13.22) | (5.43) | (13.39) | (13.47) | (5.45) | (12.73) | (13.40) | (5.48) | (12.86) | |
| Hospital gross income | −2.65 | −1.04 | −9.20 | 4.49 | 1.90 | 3.98 | 1.86 | 1.12 | 2.47 |
| (14.09) | (5.79) | (14.27) | (14.43) | (5.84) | (13.64) | (14.11) | (5.78) | (13.55) | |
| Constant | −615.15 *** | −268.56 *** | −596.67 *** | −708.92 *** | −294.43 *** | −630.50 *** | −602.41 *** | −262.76 *** | −569.11 *** |
| (212.80) | (87.36) | (215.43) | (214.50) | (86.76) | (202.74) | (211.21) | (86.44) | (202.84) | |
| Observations | 317 | 317 | 317 | 316 | 316 | 316 | 316 | 316 | 316 |
| R2 | 0.412 | 0.341 | 0.22 | 0.395 | 0.342 | 0.3 | 0.424 | 0.359 | 0.312 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wen, M.; Liao, L.; Wang, Y.; Zhou, X. Effects of Healthcare Policies and Reforms at the Primary Level in China: From the Evidence of Shenzhen Primary Care Reforms from 2018 to 2019. Int. J. Environ. Res. Public Health 2022, 19, 1945. https://doi.org/10.3390/ijerph19041945
Wen M, Liao L, Wang Y, Zhou X. Effects of Healthcare Policies and Reforms at the Primary Level in China: From the Evidence of Shenzhen Primary Care Reforms from 2018 to 2019. International Journal of Environmental Research and Public Health. 2022; 19(4):1945. https://doi.org/10.3390/ijerph19041945
Chicago/Turabian StyleWen, Mingyue, Liao Liao, Yilin Wang, and Xunzhi Zhou. 2022. "Effects of Healthcare Policies and Reforms at the Primary Level in China: From the Evidence of Shenzhen Primary Care Reforms from 2018 to 2019" International Journal of Environmental Research and Public Health 19, no. 4: 1945. https://doi.org/10.3390/ijerph19041945
APA StyleWen, M., Liao, L., Wang, Y., & Zhou, X. (2022). Effects of Healthcare Policies and Reforms at the Primary Level in China: From the Evidence of Shenzhen Primary Care Reforms from 2018 to 2019. International Journal of Environmental Research and Public Health, 19(4), 1945. https://doi.org/10.3390/ijerph19041945








