User Experience and Sustainability of 3D Printing in Dentistry
Abstract
:1. Introduction
2. Method
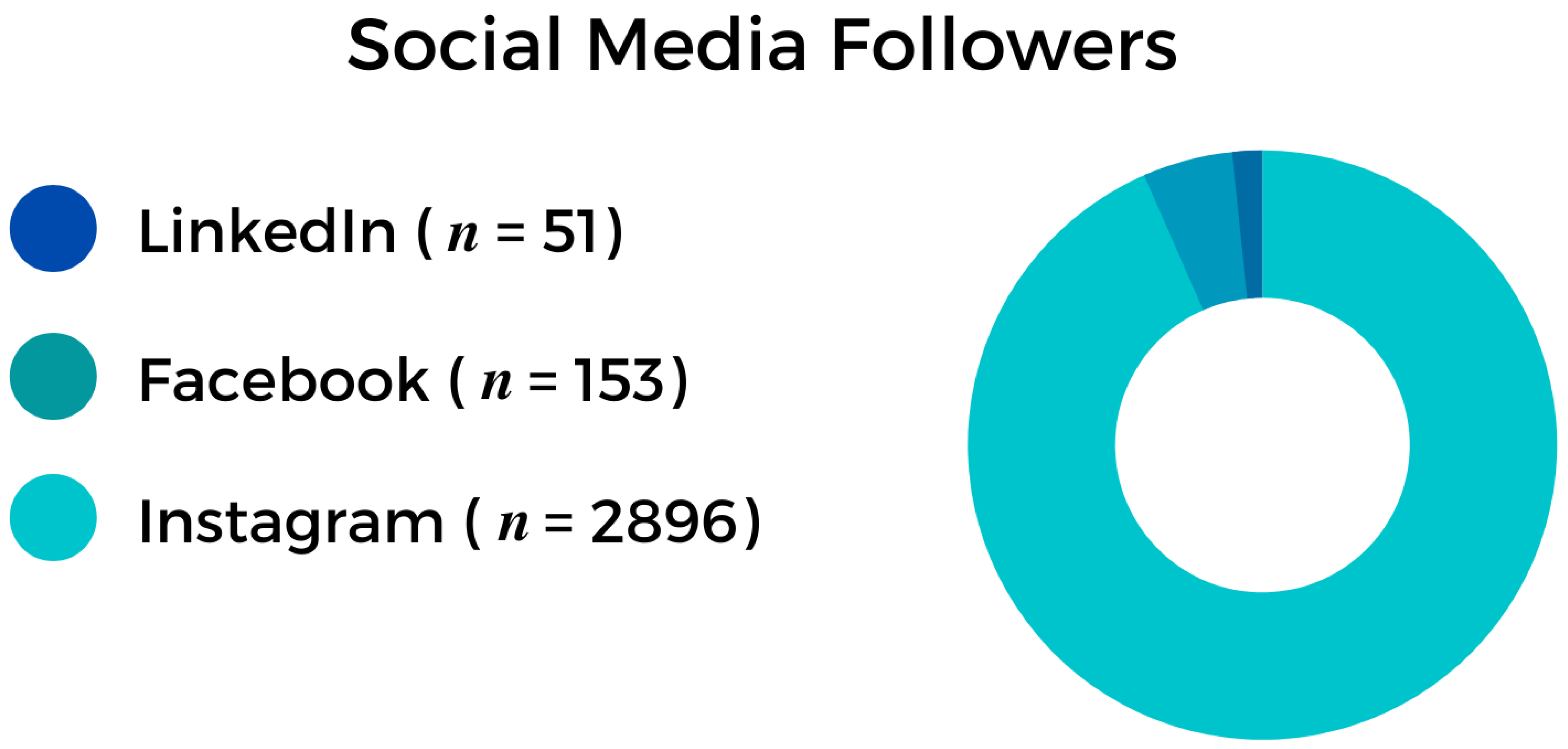
2.1. Online Survey
2.2. Data Collection and Outcome Measures
2.3. Statistical Analysis and Visualization
3. Results
- Semmelweis University Summer School 2020;
- Semmelweis University Congress for Ph.D. Students 2020;
- Semmelweis University Postgraduate Course—Faculty of Dentistry 2021;
- Semmelweis University Career Day 2021.
- ExoCad (exocad GmbH, Darmstadt, Germany) (n = 41);
- MeshMixer (AutoDesk Inc., San Rafael, CA, USA) (n = 29);
- 3Shape (3Shape A/S, Copenhagen, Denmark) (n = 21);
- Rayware (SprintRay Inc., Los Angeles, CA, USA) (n = 11);
- Chitubox (Shenzhen CBD Technology Co., Ltd., Shenzhen, China) (n = 8);
- Blue Sky Plan (Blue Sky Bio, LLC, Libertyville, IL, USA) (n = 7);
- Blender (The Blender Foundation, Amsterdam, The Netherlands) (n = 1);
- Dental Wings (Dental Wings Inc., Montréal, QC, Canada) (n = 1);
- SolidWorks (Dassault Systèmes SolidWorks Corp., Waltham, MA, USA) (n = 1) software.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 3D | 3 Dimensional |
| 3DP | 3-Dimensional Printing |
| ABS | Acrylonitrile Butadiene Styrene |
| AM | Additive Manufacturing |
| CAD/CAM | Computer-Aided Design/Computer-Aided Manufacturing |
| DiCOM | Digital Imaging and Communications in Medicine |
| DLP | Digital Light Processing |
| FDM | Fused Deposition Modeling |
| HEPA | High-Efficiency Particulate Air |
| IPA | Isopropyl Alcohol |
| LFS | Low Force Stereolithography |
| PBF | Powder Bed Fusion |
| SLA | Stereolithography Apparatus |
| STL | Standard Triangle Language |
| UFP | Ultra Fine Particles |
| VOC | Volatile Organic Compounds |
References
- Liaw, C.-Y.; Guvendiren, M. Current and emerging applications of 3D printing in medicine. Biofabrication 2017, 9, 024102. [Google Scholar] [CrossRef] [PubMed]
- Methani, M.M.; Revilla-Leon, M.; Zandinejad, A. The potential of additive manufacturing technologies and their processing parameters for the fabrication of all-ceramic crowns: A review. J. Esthet. Restor. Dent. 2020, 32, 182–192. [Google Scholar] [CrossRef] [PubMed]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. Online 2016, 15, 115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dang, W.; Ma, B.; Li, B.; Huan, Z.; Ma, N.; Zhu, H.; Chang, J.; Xiao, Y.; Wu, C. 3D printing of metal-organic framework nanosheets-structured scaffolds with tumor therapy and bone construction. Biofabrication 2020, 12, 025005. [Google Scholar] [CrossRef]
- Jiang, Y.; Pan, X.; Yao, M.; Han, L.; Zhang, X.; Jia, Z.; Weng, J.; Chen, W.; Fang, L.; Wang, X.; et al. Bioinspired adhesive and tumor microenvironment responsive nanoMOFs assembled 3D-printed scaffold for anti-tumor therapy and bone regeneration. Nano Today 2021, 39, 101182. [Google Scholar] [CrossRef]
- Wang, X.; Xue, J.; Ma, B.; Wu, J.; Chang, J.; Gelinsky, M.; Wu, C. Black Bioceramics: Combining Regeneration with Therapy. Adv. Mater. 2020, 32, e2005140. [Google Scholar] [CrossRef]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Javaid, M.; Haleem, A. Current status and applications of additive manufacturing in dentistry: A literature-based review. J. Oral Biol. Craniofac. Res. 2019, 9, 179–185. [Google Scholar] [CrossRef]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G.; Kamposiora, P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020, 20, 343. [Google Scholar] [CrossRef]
- Revilla-Leon, M.; Ozcan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef] [Green Version]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Cousley, R.R. Introducing 3D printing in your orthodontic practice. J. Orthod. 2020, 47, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Etajuri, E.A.; Suliman, E.; Mahmood, W.A.A.; Ibrahim, N.; Buzayan, M.; Mohd, N.R. Deviation of dental implants placed using a novel 3D-printed surgical guide: An in vitro study. Dent. Med. Probl. 2020, 57, 359–362. [Google Scholar] [CrossRef]
- Maroulakos, M.; Kamperos, G.; Tayebi, L.; Halazonetis, D.; Ren, Y. Applications of 3D printing on craniofacial bone repair: A systematic review. J. Dent. 2019, 80, 1–14. [Google Scholar] [CrossRef]
- Tu, C.C.; Tsai, P.-I.; Chen, S.-Y.; Kuo, M.Y.-P.; Sun, J.-S.; Chang, J.Z.-C. 3D laser-printed porous Ti6Al4V dental implants for compromised bone support. J. Formos. Med Assoc. 2020, 119, 420–429. [Google Scholar]
- Herber, V.; Okutan, B.; Antonoglou, G.; Sommer, N.; Payer, M. Bioresorbable Magnesium-Based Alloys as Novel Biomaterials in Oral Bone Regeneration: General Review and Clinical Perspectives. J. Clin. Med. 2021, 10, 1842. [Google Scholar] [CrossRef] [PubMed]
- Thayer, P.; Martinez, H.; Gatenholm, E. History and trends of 3D bioprinting. Methods Mol. Biol. 2020, 2140, 3–18. [Google Scholar]
- Smith, P.B.; Perry, J.; Elza, W. Economic and clinical impact of digitally produced dentures. J. Prosthodont. 2021, 30 (Suppl. 2), 108–112. [Google Scholar] [CrossRef]
- Kamio, T.; Suzuki, M.; Asaumi, R.; Kawai, T. Dicom segmentation and stl creation for 3D printing: A process and software package comparison for osseous anatomy. 3D Print Med. 2020, 6, 17. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D printing in dentistry-state of the art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Topolovec-Vranic, J.; Natarajan, K. The use of social media in recruitment for medical research studies: A scoping review. J. Med. Internet Res. 2016, 18, e286. [Google Scholar] [CrossRef]
- Rolls, K.; Hansen, M.; Jackson, D.; Elliott, D. How health care professionals use social media to create virtual communities: An integrative review. J. Med. Internet Res. 2016, 18, e166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Regenberg, A. Science and social media. Stem Cells Transl. Med. 2019, 8, 1226–1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Powell, R.A.; Single, H.M.; Lloyd, K.R. Focus groups in mental health research: Enhancing the validity of user and provider questionnaires. Int. J. Soc. Psychiatry 1996, 42, 193–206. [Google Scholar] [CrossRef]
- Zohrabi, M. Mixed Method Research: Instruments, Validity, Reliability and Reporting Findings. Theory Pr. Lang. Stud. 2013, 3, 254–262. [Google Scholar] [CrossRef]
- Gao, H.; Yang, Z.; Lin, W.S.; Tan, J.; Chen, L. The effect of build orientation on the dimensional accuracy of 3D-printed mandibular complete dentures manufactured with a multijet 3D printer. J. Prosthodont. 2021, 30, 684–689. [Google Scholar] [CrossRef]
- Rungrojwittayakul, O.; Kan, J.Y.; Shiozaki, K.; Swamidass, R.S.; Goodacre, B.J.; Goodacre, C.J.; Lozada, J.L. Accuracy of 3D printed models created by two technologies of printers with different designs of model base. J. Prosthodont. 2020, 29, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Unkovskiy, A.; Schmidt, F.; Beuer, F.; Li, P.; Spintzyk, S.; Kraemer Fernandez, P. Stereolithography vs. Direct light processing for rapid manufacturing of complete denture bases: An in vitro accuracy analysis. J. Clin. Med. 2021, 10, 1070. [Google Scholar] [CrossRef]
- Yoo, S.Y.; Kim, S.K.; Heo, S.J.; Koak, J.Y.; Kim, J.G. Dimensional accuracy of dental models for three-unit prostheses fabricated by various 3D printing technologies. Materials 2021, 14, 1550. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ronsivalle, V.; Rustico, L.; Aboulazm, K.; Isola, G.; Palazzo, G. Evaluation of the accuracy of orthodontic models prototyped with entry-level lcd-based 3D printers: A study using surface-based superimposition and deviation analysis. Clin. Oral Investig. 2021, 26, 303–312. [Google Scholar] [CrossRef]
- Khosravani, M.R.; Reinicke, T. On the environmental impacts of 3D printing technology. Appl. Mater. Today 2020, 20, 100689. [Google Scholar] [CrossRef]
- Shuaib, M.; Haleem, A.; Kumar, S.; Javaid, M. Impact of 3D printing on the environment: A literature-based study. Sustain. Oper. Comput. 2021, 2, 57–63. [Google Scholar] [CrossRef]
- How Sustainable is Industrial 3D Printing? 2020. Available online: https://amfg.ai/2020/03/10/how-sustainable-is-industrial-3D-printing/ (accessed on 15 December 2021).
- Rejeski, D.; Zhao, F.; Huang, Y. Research needs and recommendations on environmental implications of additive manufacturing. Addit. Manuf. 2018, 19, 21–28. [Google Scholar] [CrossRef] [Green Version]
- The Environmental Impact of 3D Printing. 2017. Available online: https://3Dinsider.com/environmental-impact-3D-printing/ (accessed on 15 December 2021).
- Xu, Y.; Xepapadeas, A.B.; Koos, B.; Geis-Gerstorfer, J.; Li, P.; Spintzyk, S. Effect of post-rinsing time on the mechanical strength and cytotoxicity of a 3D printed orthodontic splint material. Dent. Mater. 2021, 37, e314–e327. [Google Scholar] [CrossRef] [PubMed]
- Recycling IPA for 3D Printing. 2020. Available online: https://formlabs.com/blog/recycling-ipa/ (accessed on 15 December 2021).
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef] [PubMed]


| Company | Satisfaction | Price | Material Price | Speed | Support | Overall |
|---|---|---|---|---|---|---|
| Asiga | 5.0 (n = 24) | 3.9 (n = 24) | 3.7 (n = 24) | 4.4 (n = 24) | 4.7 (n = 24) | 4.3 (n = 24) |
| Nextdent | 4.9 (n = 25) | 4.4 (n = 25) | 4.4 (n = 25) | 5.0 (n = 25) | 4.6 (n = 25) | 4.7 (n = 25) |
| Formlabs | 4.4 (n = 35) | 4.4(n = 35) | 4.3 (n = 35) | 2.6 (n = 35) | 4.2 (n = 35) | 4.0 (n = 35) |
| Anycubic | 4.5 (n = 15) | 4.8 (n = 15) | 4.5 (n = 15) | 4.0 (n = 15) | 4.3 (n = 15) | 4.4 (n = 15) |
| Sprintray | 4.3 (n = 10) | 4.3 (n = 10) | 4.3 (n = 10) | 4.0 (n = 10) | 4.0 (n = 10) | 4.2 (n = 10) |
| Phrozen | 3.7 (n = 11) | 5.0 (n = 11) | 4.0 (n = 11) | 4.0 (n = 11) | 3.0 (n = 11) | 3.9 (n = 11) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hegedus, T.; Kreuter, P.; Kismarczi-Antalffy, A.A.; Demeter, T.; Banyai, D.; Vegh, A.; Geczi, Z.; Hermann, P.; Payer, M.; Zsembery, A.; et al. User Experience and Sustainability of 3D Printing in Dentistry. Int. J. Environ. Res. Public Health 2022, 19, 1921. https://doi.org/10.3390/ijerph19041921
Hegedus T, Kreuter P, Kismarczi-Antalffy AA, Demeter T, Banyai D, Vegh A, Geczi Z, Hermann P, Payer M, Zsembery A, et al. User Experience and Sustainability of 3D Printing in Dentistry. International Journal of Environmental Research and Public Health. 2022; 19(4):1921. https://doi.org/10.3390/ijerph19041921
Chicago/Turabian StyleHegedus, Tamas, Patrik Kreuter, Aron Attila Kismarczi-Antalffy, Tamas Demeter, Dorottya Banyai, Adam Vegh, Zoltan Geczi, Peter Hermann, Michael Payer, Akos Zsembery, and et al. 2022. "User Experience and Sustainability of 3D Printing in Dentistry" International Journal of Environmental Research and Public Health 19, no. 4: 1921. https://doi.org/10.3390/ijerph19041921
APA StyleHegedus, T., Kreuter, P., Kismarczi-Antalffy, A. A., Demeter, T., Banyai, D., Vegh, A., Geczi, Z., Hermann, P., Payer, M., Zsembery, A., Al-Hassiny, A., Mukaddam, K., Herber, V., Jakse, N., & Vegh, D. (2022). User Experience and Sustainability of 3D Printing in Dentistry. International Journal of Environmental Research and Public Health, 19(4), 1921. https://doi.org/10.3390/ijerph19041921








