Evaluating Teaching Effectiveness of Medical Humanities in an Integrated Clerkship Program by a Novel Prospective Propensity Score Matching Framework
Abstract
1. Introduction
2. Materials and Methods
2.1. The Integrated Clinical Clerkship Program
2.2. The Conventional Clerkships in Medicine and Surgery
2.3. Enrollment of Participants and Sample Size Calculation
2.4. Study Design
2.5. Self-Report Instruments
2.6. Objective Assessment of Clinical Performance
2.7. Clinical Grades
2.8. Evaluation of Humanities Education
2.9. Statistics Analysis
3. Results
4. Discussion
4.1. Main Findings
4.2. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cooke, M.; Irby, D.M.; Sullivan, W.; Ludmerer, K.M. American medical education 100 years after the Flexner report. N. Engl. J. Med. 2006, 355, 1339–1344. [Google Scholar] [CrossRef]
- Obermeyer, Z.; Lee, T.H. Lost in Thought—The Limits of the Human Mind and the Future of Medicine. N. Engl. J. Med. 2017, 377, 1209–1211. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.H.; Asch, S.M. Machine Learning and Prediction in Medicine—Beyond the Peak of Inflated Expectations. N. Engl. J. Med. 2017, 376, 2507–2509. [Google Scholar] [CrossRef] [PubMed]
- Ogur, B.; Hirsh, D.; Krupat, E.; Bor, D. The Harvard Medical School-Cambridge integrated clerkship: An innovative model of clinical education. Acad. Med. 2007, 82, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Hirsh, D.; Gaufberg, E.; Ogur, B.; Cohen, P.; Krupat, E.; Cox, M.; Pelletier, S.; Bor, D. Educational outcomes of the Harvard Medical School-Cambridge integrated clerkship: A way forward for medical education. Acad. Med. 2012, 87, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Hauer, K.E.; Hirsh, D.; Ma, I.; Hansen, L.; Ogur, B.; Poncelet, A.N.; Alexander, E.K.; O’Brien, B.C. The role of role: Learning in longitudinal integrated and traditional block clerkships. Med. Educ. 2012, 46, 698–710. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, B.C.; Poncelet, A.N.; Hansen, L.; Hirsh, D.A.; Ogur, B.; Alexander, E.K.; Krupat, E.; Hauer, K.E. Students’ workplace learning in two clerkship models: A multi-site observational study. Med. Educ. 2012, 46, 613–624. [Google Scholar] [CrossRef]
- Teherani, A.; Irby, D.M.; Loeser, H. Outcomes of different clerkship models: Longitudinal integrated, hybrid, and block. Acad. Med. 2013, 88, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Speer, A.J.; Stagnaro-Green, A.; Elnicki, D.M. Interdisciplinary clerkships: Educational models of the future? Am. J. Med. 1995, 99, 451–453. [Google Scholar] [CrossRef]
- Parry, J.; Mathers, J.; Al-Fares, A.; Mohammad, M.; Nandakumar, M.; Tsivos, D. Hostile teaching hospitals and friendly district general hospitals: Final year students’ views on clinical attachment locations. Med. Educ. 2002, 36, 1131–1141. [Google Scholar] [CrossRef] [PubMed]
- Thistlethwaite, J.E.; Bartle, E.; Chong, A.A.; Dick, M.L.; King, D.; Mahoney, S.; Papinczak, T.; Tucker, G. A review of longitudinal community and hospital placements in medical education: BEME Guide No. 26. Med. Teach. 2013, 35, e1340–e1364. [Google Scholar] [CrossRef] [PubMed]
- de Villiers, M.; van Schalkwyk, S.; Blitz, J.; Couper, I.; Moodley, K.; Talib, Z.; Young, T. Decentralised training for medical students: A scoping review. BMC Med. Educ. 2017, 17, 196. [Google Scholar] [CrossRef]
- Schauer, R.W.; Schieve, D. Performance of medical students in a nontraditional rural clinical program, 1998–1999 through 2003-04. Acad. Med. 2006, 81, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, T.C.; Smith, H., Jr.; Blackburn, B.; Silverman, B.; Schroeder, B.; Reitman, D.; Ambroz, A. A method for assessing the quality of a randomized control trial. Control. Clin. Trials 1981, 2, 31–49. [Google Scholar] [CrossRef]
- Wang, Y.A.; Chen, C.F.; Chen, C.H.; Wang, G.L.; Huang, A.T. A clinical clerkship collaborative program in Taiwan: Acquiring core clinical competencies through patient care responsibility. J. Formos. Med. Assoc. 2016, 115, 418–425. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lai, C.-W. Experiences of accreditation of medical education in Taiwan. J. Educ. Eval. Health Prof. 2009, 6, 2–4. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudi, S.; Jafari, E.; Nasrabadi, H.A.; Liaghatdar, M.J. Holistic education: An approach for 21 century. Int. Educ. Stud. 2012, 5, 178–186. [Google Scholar] [CrossRef]
- Wang, X.; Shih, J.; Kuo, F.-J.; Ho, M.-J. A scoping review of medical professionalism research published in the Chinese language. BMC Med. Educ. 2016, 16, 300. [Google Scholar] [CrossRef] [PubMed]
- Yen-Ju Lin, B.; Liu, P.-C.; Ku, K.-T.; Lee, C.-C. Adaptation of medical students during clinical training: Effects of holistic preclinical education on clerkship performance. Teach. Learn. Med. 2019, 31, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Zarifsanaiey, N.; Mosalanejad, L.; Ebrahimi, A.-M. A holistic approach to teaching medical ethics: A new trend to accountability in medical education. Pak. J. Med. Health Sci. 2019, 12, 1829–1836. [Google Scholar]
- Thompson, E.R. Development and validation of an International English Big-Five Mini-Markers. Personal. Individ. Differ. 2008, 45, 542–548. [Google Scholar] [CrossRef]
- Deng, J.Y.; Tseng, S.M.; Li, Y.Z.; Yu, C.S. International English Big-Five Mini-Markers: Development of the Traditional Chinese version. J. Manag. Bus. Res. 2011, 28, 579–600. [Google Scholar]
- Schigelone, A.; White, C.; Krupat, E. Medical Students’ Attitudes toward the Doctor-Patient Relationship: A Cross-Sectional Study; Association of American Medical Colleges Central Group on Educational Affairs: Madison, WI, USA, 2005. [Google Scholar]
- Hojat, M. Empathy in Patient Care: Antecedents, Development, Measurement, and Outcomes; Springer: Philadelphia, PA, USA, 2007. [Google Scholar]
- Krupat, E.; Hiam, C.M.; Fleming, M.Z.; Freeman, P. Patient-centeredness and its correlates among first year medical students. Int. J. Psychiatry Med. 1999, 29, 347–356. [Google Scholar] [CrossRef]
- Krupat, E.; Rosenkranz, S.L.; Yeager, C.M.; Barnard, K.; Putnam, S.M.; Inui, T.S. The practice orientations of physicians and patients: The effect of doctor-patient congruence on satisfaction. Patient Educ. Couns. 2000, 39, 49–59. [Google Scholar] [CrossRef]
- Cook, D.A.; Beckman, T.J. Reflections on experimental research in medical education. Adv. Health Sci. Educ. Theory Pract. 2010, 15, 455–464. [Google Scholar] [CrossRef]
- Quaintance, J.L.; Arnold, L.; Thompson, G.S. Development of an instrument to measure the climate of professionalism in a clinical teaching environment. Acad. Med. 2008, 83 (Suppl. S10), S5–S8. [Google Scholar] [CrossRef]
- SAS Institute. Base SAS 9.4 Procedures Guide: Statistical Procedures; SAS Institute: Cary, NC, USA, 2017. [Google Scholar]
- Gracey, C.F.; Haidet, P.; Branch, W.T.; Weissmann, P.; Kern, D.E.; Mitchell, G.; Frankel, R.; Inui, T. Precepting humanism: Strategies for fostering the human dimensions of care in ambulatory settings. Acad. Med. 2005, 80, 21–28. [Google Scholar] [CrossRef]
- Moyer, C.A.; Arnold, L.; Quaintance, J.; Braddock, C.; Spickard, A., 3rd; Wilson, D.; Rominski, S.; Stern, D.T. What factors create a humanistic doctor? A nationwide survey of fourth-year medical students. Acad. Med. 2010, 85, 1800–1807. [Google Scholar] [CrossRef]
- Lee, W.K.; Harris, C.C.D.; Mortensen, K.A.; Long, L.M.; Sugimoto-Matsuda, J. Enhancing student perspectives of humanism in medicine: Reflections from the Kalaupapa service learning project. BMC Med. Educ. 2016, 16, 137. [Google Scholar] [CrossRef] [PubMed]
- Thrush, C.R.; Spollen, J.J.; Tariq, S.G.; Williams, D.K.; Li, J.M. Evidence for validity of a survey to measure the learning environment for professionalism. Med. Teach. 2011, 33, e683–e688. [Google Scholar] [CrossRef]
- Li, H.; Ding, N.; Zhang, Y.; Liu, Y.; Wen, D. Assessing medical professionalism: A systematic review of instruments and their measurement properties. PLoS ONE 2017, 12, e0177321. [Google Scholar] [CrossRef]
- Birden, H.; Glass, N.; Wilson, I.; Harrison, M.; Usherwood, T.; Nass, D. Teaching professionalism in medical education: A Best Evidence Medical Education (BEME) systematic review. BEME Guide No. 25. Med. Teach. 2013, 35, e1252–e1266. [Google Scholar] [CrossRef] [PubMed]
- Kruger, J.; Dunning, D. Unskilled and unaware of it: How difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J. Pers. Soc. Psychol. 1999, 77, 1121–1134. [Google Scholar] [CrossRef] [PubMed]
- Hochberg, M.; Berman, R.; Ogilvie, J.; Yingling, S.; Lee, S.; Pusic, M.; Pachter, H.L. Midclerkship feedback in the surgical clerkship: The “Professionalism, Reporting, Interpreting, Managing, Educating, and Procedural Skills” application utilizing learner self-assessment. Am. J. Surg. 2017, 213, 212–216. [Google Scholar] [CrossRef]
- Joint Commission of Taiwan Rigorous and Equable Professional Accreditation. 2021. Available online: https://www.jct.org.tw/cp-1127-1106-22fc4-2.html (accessed on 14 January 2022).
- Wilkinson, T.J.; Wade, W.B.; Knock, L.D. A blueprint to assess professionalism: Results of a systematic review. Acad. Med. 2009, 84, 551–558. [Google Scholar] [CrossRef] [PubMed]


| Variable | Overall N = 207 | C Hospital N = 69 | B Hospital N = 138 | p-Value |
|---|---|---|---|---|
| Age | 22.6 ± 1.1 | 22.7 ± 1.5 | 22.5 ± 0.9 | 0.2298 |
| Sex | 0.4912 | |||
| Male | 100 (48%) | 31 (45%) | 69 (50%) | |
| Female | 107 (52%) | 38 (55%) | 69 (50%) | |
| Admission route | 0.6898 | |||
| Interview | 105 (51%) | 37 (54%) | 68 (48%) | |
| Recommendation | 28 (14%) | 7 (10%) | 21 (15%) | |
| Examination | 73 (35%) | 24 (35%) | 49 (36%) | |
| Study Loan | 0.4624 | |||
| No | 149 (72%) | 50 (72%) | 99 (72%) | |
| Yes | 58 (28%) | 19 (28%) | 39 (28%) | |
| Part-time job | 0.6580 | |||
| No | 126 (61%) | 41 (60%) | 85 (62%) | |
| Yes | 80 (39%) | 27 (40%) | 53 (38%) | |
| Personalities 1,2 | ||||
| Extraversion 1,2 | 40.9 ± 12.0 | 39.9 ± 12.4 | 41.4 ± 11.8 | 0.3978 |
| Agreeableness 1,2 | 52.6 ± 7.5 | 52.5 ± 7.5 | 52.6 ± 7.5 | 0.9116 |
| Conscientiousness 1,2 | 34.1 ± 10.2 | 34.3 ± 10.4 | 34.0 ± 10.2 | 0.8783 |
| Neuroticism 1,2 | 47.7 ± 7.9 | 47.5 ± 8.4 | 47.9 ± 7.6 | 0.7552 |
| Openness 1,2 | 48.6 ± 8.0 | 48.4 ± 8.0 | 48.7 ± 8.0 | 0.8301 |
| At Baseline | Overall N = 207 | C Hospital N = 69 | B Hospital N = 138 | p-Value | Non-Inferiority Test |
|---|---|---|---|---|---|
| At baseline 1,2 | |||||
| TOMS | |||||
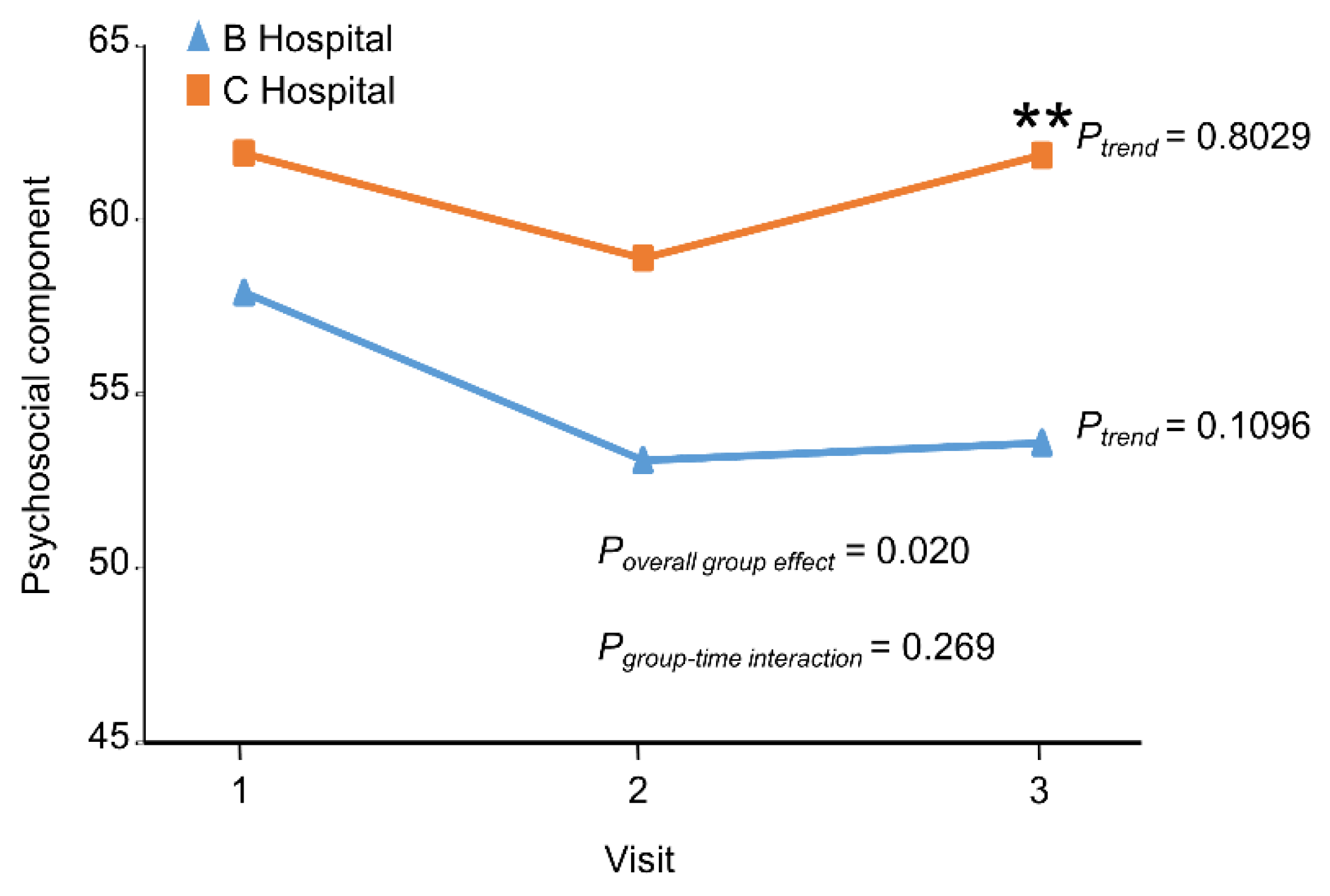
| Psychosocial | 59.3 ± 18.3 | 61.9 ± 17.7 | 57.9 ± 8.5 | 0.1439 | |
| JSPE | |||||
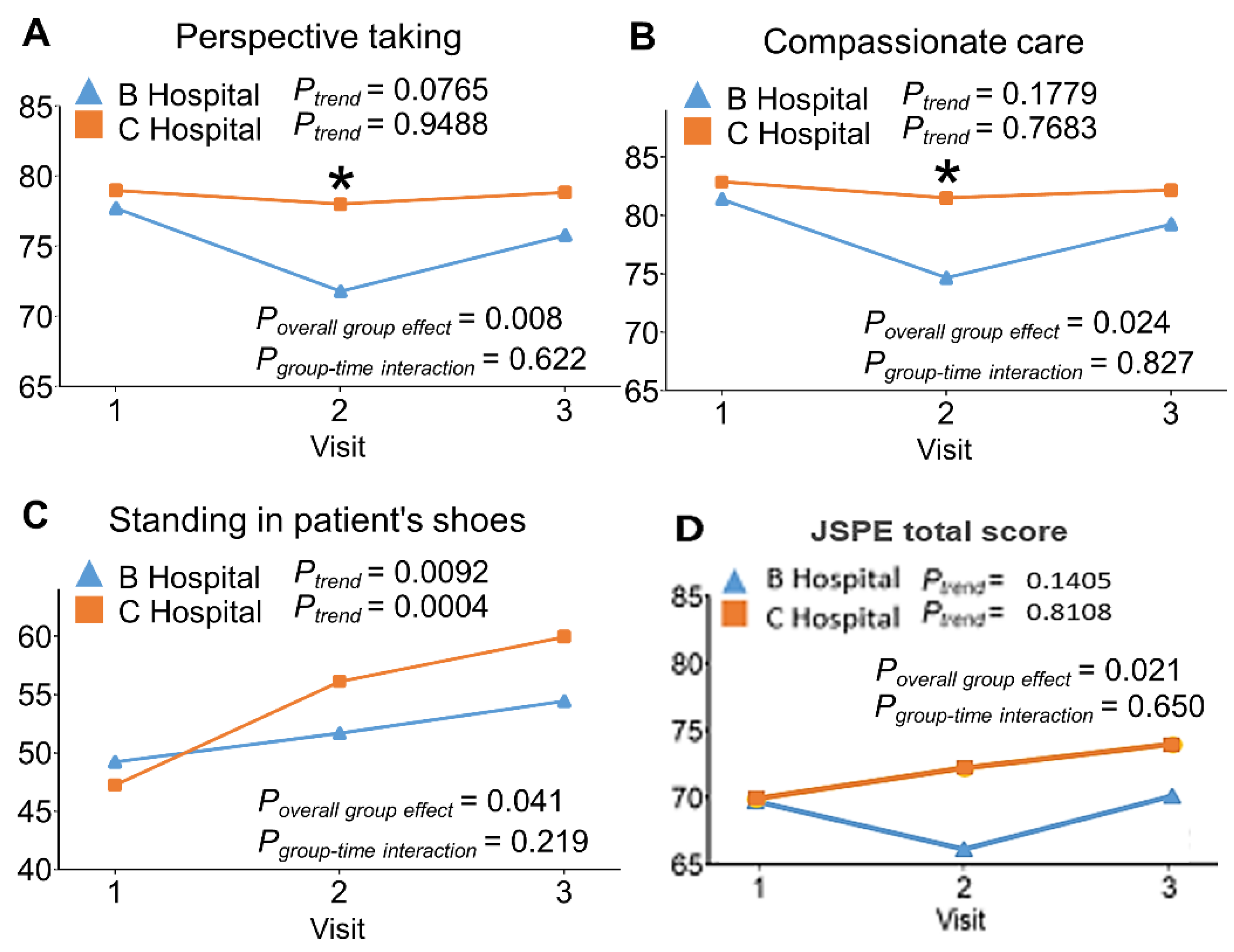
| Perspective taking | 78.1 ± 11.1 | 79.0 ± 11.9 | 77.7 ± 10.7 | 0.4413 | |
| Compassionate care | 81.9 ± 11.8 | 82.9 ± 11.4 | 81.4 ± 12.0 | 0.4000 | |
| Standing in patient’s shoes | 48.6 ± 24.8 | 47.2 ± 26.1 | 49.2 ± 24.2 | 0.5873 | |
| PPOS | |||||
| Sharing | 61.1 ± 10.0 | 62.7 ± 10.1 | 60.3 ± 9.8 | 0.1000 | |
| Caring | 61.8 ± 8.1 | 62.4 ± 7.7 | 61.5 ± 8.2 | 0.4368 | |
| At the end of programs 1,2 | |||||
| TOMS | |||||
| Psychosocial | 56.4 ± 21.0 | 61.9 ± 18.1 | 53.6 ± 21.9 | 0.0091 | <0.0001 |
| JSPE | |||||
| Perspective taking | 76.8 ± 12.6 | 78.8 ± 15.5 | 75.8 ± 10.8 | 0.1483 | 0.0001 |
| Compassionate care | 80.2 ± 15.1 | 82.2 ± 19.1 | 79.3 ± 12.6 | 0.2558 | 0.0201 |
| Standing in patient’s shoes | 56.3 ± 24.7 | 59.9 ± 26.8 | 54.4 ± 23.5 | 0.1333 | <0.0001 |
| Combined * | 69.5 ± 11.5 | 69.7 ± 11.9 | 69.4 ± 11.3 | 0.8840 | 0.0010 |
| PPOS | |||||
| Sharing | 59.3 ± 11.1 | 64.5 ± 11.0 | 56.6 ± 10.3 | <0.0001 | |
| Caring | 61.6 ± 7.5 | 63.6 ± 7.5 | 60.6 ± 7.4 | 0.0063 | <0.0001 |
| PCI | |||||
| Peers | 60.8 ± 9.3 | 62.7 ± 10.5 | 59.8 ± 8.6 | 0.0490 | <0.0001 |
| Residents | 58.3 ± 10.5 | 64.2 ± 11.2 | 55.4 ± 8.8 | <0.0001 | |
| Attending | 60.0 ± 10.8 | 65.7 ± 11.3 | 57.1 ± 9.4 | <0.0001 | |
| Faculty | 69.6 ± 16.0 | 77.0 ± 14.9 | 65.8 ± 15.2 | <0.0001 | |
| OSCE | |||||
| Medicine | 87.2 ± 6.5 | 87.2 ± 5.8 | 87.2 ± 6.9 | 0.9761 | 0.0010 |
| Surgery | 89.7 ± 3.3 | 90.0 ± 3.0 | 89.6 ± 3.4 | 0.3181 | 0.0012 |
| Combined * | 87.4 ± 5.1 | 87.4 ± 5.4 | 87.4 ± 5.0 | 0.9830 | 0.0421 |
| 6th year Internship grade (N = 152) | 91.1 ± 1.9 | 91.0 ± 2.2 | 91.1 ± 1.7 | 0.7762 | 0.0529 |
| 7th year Internship grade (N = 97) | 92.9 ± 1.4 | 93.0 ± 1.4 | 92.9 ± 1.3 | 0.6464 | 0.0296 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-H.; Wang, S.-J.; Yeh, W.-Y.; Wu, C.-L.; Wang, Y.A.; Chen, C.-F.; Yang, Y.-Y.; Huang, W.J.; Chan, K.-Y.; Lai, C.-W.; et al. Evaluating Teaching Effectiveness of Medical Humanities in an Integrated Clerkship Program by a Novel Prospective Propensity Score Matching Framework. Int. J. Environ. Res. Public Health 2022, 19, 1882. https://doi.org/10.3390/ijerph19031882
Chen C-H, Wang S-J, Yeh W-Y, Wu C-L, Wang YA, Chen C-F, Yang Y-Y, Huang WJ, Chan K-Y, Lai C-W, et al. Evaluating Teaching Effectiveness of Medical Humanities in an Integrated Clerkship Program by a Novel Prospective Propensity Score Matching Framework. International Journal of Environmental Research and Public Health. 2022; 19(3):1882. https://doi.org/10.3390/ijerph19031882
Chicago/Turabian StyleChen, Chen-Huan, Shuu-Jiun Wang, Wan-Yu Yeh, Chung-Li Wu, Yong A. Wang, Cheng-Feng Chen, Ying-Ying Yang, William J. Huang, Kwan-Yee Chan, Chi-Wan Lai, and et al. 2022. "Evaluating Teaching Effectiveness of Medical Humanities in an Integrated Clerkship Program by a Novel Prospective Propensity Score Matching Framework" International Journal of Environmental Research and Public Health 19, no. 3: 1882. https://doi.org/10.3390/ijerph19031882
APA StyleChen, C.-H., Wang, S.-J., Yeh, W.-Y., Wu, C.-L., Wang, Y. A., Chen, C.-F., Yang, Y.-Y., Huang, W. J., Chan, K.-Y., Lai, C.-W., Wang, G.-L., & Cheng, H.-M. (2022). Evaluating Teaching Effectiveness of Medical Humanities in an Integrated Clerkship Program by a Novel Prospective Propensity Score Matching Framework. International Journal of Environmental Research and Public Health, 19(3), 1882. https://doi.org/10.3390/ijerph19031882






