Reliability Study of the Items of the Alberta Infant Motor Scale (AIMS) Using Kappa Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Infant Subjects
2.2. Raters
2.3. Evaluation Tool (AIMS)
2.4. Interrater and Intrarater Reliability Analysis
2.5. Data Analysis
3. Results
3.1. Interrater and Intrarater Reliability of AIMS for Each Item
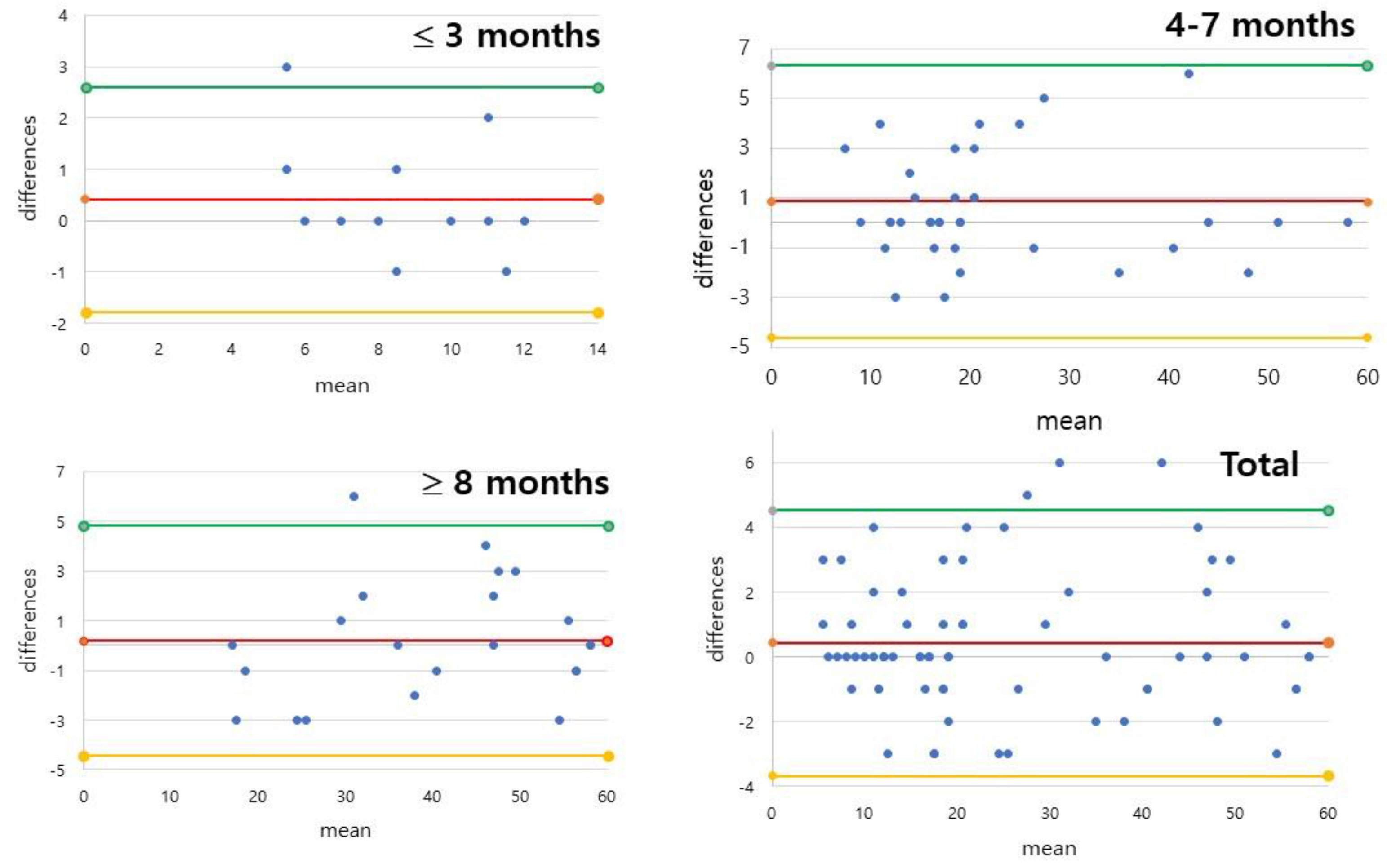
3.2. Interrater and Intrarater Reliability of AIMS for Subtotal and Total Scores
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Silva, L.P.; Maia, P.C.; Lopes, M.M.; Cardoso, M.V. Intraclass reliability of the Alberta Infant Motor Scale in the Brazilian version. Rev. Esc. Enferm. USP 2013, 47, 1046–1051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loeb, D.F.; Imgrund, C.M.; Lee, J.; Barlow, S.M. Language, Motor, and Cognitive Outcomes of Toddlers Who Were Born Preterm. Am. J. Speech Lang Pathol. 2020, 29, 625–637. [Google Scholar] [CrossRef] [PubMed]
- Bos, A.F.; Van Braeckel, K.N.; Hitzert, M.M.; Tanis, J.C.; Roze, E. Development of fine motor skills in preterm infants. Dev. Med. Child Neurol. 2013, 55 (Suppl. 4), 1–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- George, J.M.; Boyd, R.N.; Colditz, P.B.; Rose, S.E.; Pannek, K.; Fripp, J.; Lingwood, B.E.; Lai, M.M.; Kong, A.H.; Ware, R.S.; et al. PPREMO: A prospective cohort study of preterm infant brain structure and function to predict neurodevelopmental outcome. BMC Pediatrics 2015, 15, 123. [Google Scholar] [CrossRef]
- Sweeney, J.K.; Gutierrez, T. Musculoskeletal Implications of Preterm Infant Positioning in the NICU. J. Perinat. Neonatal Nurs. 2002, 16, 58–70. [Google Scholar] [CrossRef]
- Drzal-Grabiec, J.; Walicka-Cuprys, K.; Zajkiewicz, K.; Rachwal, M.; Piwonski, P.; Perenc, L. Parameters characterizing the posture of preterm children in standing and sitting position. J. Back Musculoskelet. Rehabil. 2020, 33, 455–462. [Google Scholar] [CrossRef]
- Gorga, D.; Stern, F.M.; Ross, G.; Nagler, W. Neuromotor development of preterm and full-term infants. Early Hum. Dev. 1988, 18, 137–149. [Google Scholar] [CrossRef]
- Council on Children with D; Section on Developmental Behavioral P; Bright Futures Steering C; Medical Home Initiatives for Children with Special Needs Project Advisory C. Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics 2006, 118, 405–420. [Google Scholar] [CrossRef] [Green Version]
- Georgieff, M.K.; Bernbaum, J.C.; Hoffman-Williamson, M.; Daft, A. Abnormal truncal muscle tone as a useful early marker for developmental delay in low birth weight infants. Pediatrics 1986, 77, 659–663. [Google Scholar] [CrossRef]
- Benzies, K.M.; Magill-Evans, J.; Ballantyne, M.; Kurilova, J. Longitudinal patterns of early development in Canadian late preterm infants: A prospective cohort study. J. Child Health Care 2017, 21, 85–93. [Google Scholar] [CrossRef]
- Benzies, K.M.; Magill-Evans, J.E.; Hayden, K.A.; Ballantyne, M. Key components of early intervention programs for preterm infants and their parents: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2013, 13 (Suppl. 1), S10. [Google Scholar] [CrossRef] [Green Version]
- Caesar, R.; Boyd, R.N.; Colditz, P.; Cioni, G.; Ware, R.S.; Salthouse, K.; Doherty, J.; Jackson, M.; Matthews, L.; Hurley, T.; et al. Early prediction of typical outcome and mild developmental delay for prioritisation of service delivery for very preterm and very low birthweight infants: A study protocol. BMJ Open 2016, 6, e010726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kepenek-Varol, B.; Hosbay, Z.; Varol, S.; Torun, E. Assessment of motor development using the Alberta Infant Motor Scale in full-term infants. Turk. J. Pediatr. 2020, 62, 94–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piper, M.; Darrah, J. Motor Assessment of the Developing Infant; Elsevier, Inc.: Philadelphia, PA, USA, 2021. [Google Scholar]
- Snyder, P.; Eason, J.M.; Philibert, D.; Ridgway, A.; McCaughey, T. Concurrent validity and reliability of the Alberta Infant Motor Scale in infants at dual risk for motor delays. Phys. Occup. Ther. Pediatrics 2008, 28, 267–282. [Google Scholar] [CrossRef] [PubMed]
- de Albuquerque, P.L.; Lemos, A.; Guerra, M.Q.; Eickmann, S.H. Accuracy of the Alberta Infant Motor Scale (AIMS) to detect developmental delay of gross motor skills in preterm infants: A systematic review. Dev. Neurorehabil. 2015, 18, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Pin, T.W.; Darrer, T.; Eldridge, B.; Galea, M.P. Motor development from 4 to 8 months corrected age in infants born at or less than 29 weeks’ gestation. Dev. Med. Child Neurol. 2009, 51, 739–745. [Google Scholar] [CrossRef]
- Albuquerque, P.L.; Guerra, M.Q.F.; Lima, M.C.; Eickmann, S.H. Concurrent validity of the Alberta Infant Motor Scale to detect delayed gross motor development in preterm infants: A comparative study with the Bayley III. Dev. Neurorehabil. 2018, 21, 408–414. [Google Scholar] [CrossRef]
- Pin, T.W.; Eldridge, B.; Galea, M.P. Motor trajectories from 4 to 18 months corrected age in infants born at less than 30 weeks of gestation. Early Hum. Dev. 2010, 86, 573–580. [Google Scholar] [CrossRef]
- Wang, T.N.; Howe, T.H.; Hinojosa, J.; Hsu, Y.W. Postural control of pre-term infants at 6 and 12 months corrected age. Early Hum. Dev. 2010, 86, 433–437. [Google Scholar] [CrossRef]
- Su, Y.H.; Jeng, S.F.; Hsieh, W.S.; Tu, Y.K.; Wu, Y.T.; Chen, L.C. Gross Motor Trajectories during the First Year of Life for Preterm Infants with Very Low Birth Weight. Phys. Ther. 2017, 97, 365–373. [Google Scholar] [CrossRef]
- Valentini, N.C.; Saccani, R. Brazilian validation of the Alberta Infant Motor Scale. Phys. Ther. 2012, 92, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Morales-Monforte, E.; Bagur-Calafat, C.; Suc-Lerin, N.; Fornaguera-Marti, M.; Cazorla-Sanchez, E.; Girabent-Farres, M. The Spanish version of the Alberta Infant Motor Scale: Validity and reliability analysis. Dev. Neurorehabil. 2017, 20, 76–82. [Google Scholar] [CrossRef]
- Wang, H.; Li, H.; Wang, J.; Jin, H. Reliability and Concurrent Validity of a Chinese Version of the Alberta Infant Motor Scale Administered to High-Risk Infants in China. Biomed. Res. Int. 2018, 2018, 2197163. [Google Scholar] [CrossRef] [PubMed]
- Jeng, S.F.; Yau, K.I.; Chen, L.C.; Hsiao, S.F. Alberta infant motor scale: Reliability and validity when used on preterm infants in Taiwan. Phys. Ther. 2000, 80, 168–178. [Google Scholar] [CrossRef] [PubMed]
- Syrengelas, D.; Siahanidou, T.; Kourlaba, G.; Kleisiouni, P.; Bakoula, C.; Chrousos, G.P. Standardization of the Alberta infant motor scale in full-term Greek infants: Preliminary results. Early Hum. Dev. 2010, 86, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, Y.; Neilan, E.; Busanich, J.; Garavuso, L.; Klimas, D. Interrater reliability of early intervention providers scoring the alberta infant motor scale. Pediatric Phys. Ther. 2004, 16, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Lackovic, M.; Nikolic, D.; Filimonovic, D.; Petronic, I.; Mihajlovic, S.; Golubovic, Z.; Pavicevic, P.; Cirovic, D. Reliability, Consistency and Temporal Stability of Alberta Infant Motor Scale in Serbian Infants. Children 2020, 7, 16. [Google Scholar] [CrossRef] [Green Version]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Rey, E.; Carballo-Fazanes, A.; Varela-Casal, C.; Abelairas-Gomez, C.; on Behalf of ALFA-MOV Project Collaborators. Reliability of the test of gross motor development: A systematic review. PLoS ONE 2020, 15, e0236070. [Google Scholar] [CrossRef]
- Ricci, E.; Einspieler, C.; Craig, A.K. Feasibility of Using the General Movements Assessment of Infants in the United States. Phys. Occup. Ther. Pediatrics 2018, 38, 269–279. [Google Scholar] [CrossRef]
- Fuentefria, R.D.N.; Silveira, R.C.; Procianoy, R.S. Motor development of preterm infants assessed by the Alberta Infant Motor Scale: Systematic review article. J. Pediatr. (Rio J.) 2017, 93, 328–342. [Google Scholar] [CrossRef] [PubMed]
- Aimsamrarn, P.; Janyachareon, T.; Rattanathanthong, K.; Emasithi, A.; Siritaratiwat, W. Cultural translation and adaptation of the Alberta Infant Motor Scale Thai version. Early Hum. Dev. 2019, 130, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Uesugi, M.; Tokuhisa, K.; Shimada, T. The reliability and validity of the Alberta Infant Motor Scale in Japan. J. Phys. Ther. Sci. 2008, 20, 169–175. [Google Scholar] [CrossRef] [Green Version]
- Gontijo, A.P.B.; Mambrini, J.V.M.; Mancini, M.C. Cross-country validity of the Alberta Infant Motor Scale using a Brazilian sample. Braz. J. Phys. Ther. 2021, 25, 444–449. [Google Scholar] [CrossRef]
- van Iersel, P.A.M.; la Bastide-van Gemert, S.; Wu, Y.C.; Hadders-Algra, M. Alberta Infant Motor Scale: Cross-cultural analysis of gross motor development in Dutch and Canadian infants and introduction of Dutch norms. Early Hum. Dev. 2020, 151, 105239. [Google Scholar] [CrossRef]
- Borsa, J.C.; Damásio, B.F.; Bandeira, D.R. Cross-cultural adaptation and validation of psychological instruments: Some considerations. Paidéia 2012, 22, 423–432. [Google Scholar] [CrossRef]
- Mendonca, B.; Sargent, B.; Fetters, L. Cross-cultural validity of standardized motor development screening and assessment tools: A systematic review. Dev. Med. Child Neurol. 2016, 58, 1213–1222. [Google Scholar] [CrossRef]
- Pivovarov Iu, P.; Kukhto, A.I. Effect of pH of food products on the development of Bac. cereus group bacteria. Vopr. Pitan. 1970, 29, 72–75. [Google Scholar]
- Dekkers, L.M.A.; Nijhuis-van der Sanden, M.W.G.; Jonker, M.; de Swart, B.J.M.; Janssen, A. Interrater Reliability of the Observable Movement Quality Scale for Children. Physiother. Can. 2018, 70, 113–119. [Google Scholar] [CrossRef]
- Boonzaaijer, M.; van Dam, E.; van Haastert, I.C.; Nuysink, J. Concurrent Validity between Live and Home Video Observations Using the Alberta Infant Motor Scale. Pediatric Phys. Ther. 2017, 29, 146–151. [Google Scholar] [CrossRef]
| Variables | |
|---|---|
| Age (days) | |
| Preterm infants (CA) | 145.2 ± 92.8 (16–431) |
| Full-term infants | 276.3 ± 103.4 (180–540) |
| Gestational age (days) | |
| Preterm infants | 209.5 ± 48.5 (161–258) |
| Full-term infants | 273 ± 7 (266–280) |
| Birth weight (grams) | |
| Preterm infants | 1790 ± 1230 (560–3020) |
| Full-term infants | 2885 ± 157.5 (2500–3810) |
| Preterm vs. full term (numbers) | |
| Preterm infants | 46 (65.7%) |
| Full-term infants | 24 (34.3%) |
| Gender | |
| Girls | 21 (30.0%) |
| Boys | 49 (70.0%) |
| Age bands (months) | |
| 3≥ | 12 (17.1%) |
| 4–7 | 36 (51.4%) |
| 8≤ | 22 (31.4%) |
| ≤3 Months (n = 12) | 4–7 Months (n = 36) | ≥8 Months (n = 22) | Total (n = 70) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Items | Prone | Supine | Sitting | Standing | Prone | Supine | Sitting | Standing | Prone | Supine | Sitting | Standing | Prone | Supine | Sitting | Standing |
| 1 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 |
| 2 | 0.775 | 1.000 | 1.000 | 0.153 | 1.000 | 1.000 | 0.897 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 0.796 | 1.000 | 0.958 | 0.192 |
| 3 | 1.000 | 0.649 | 0.635 | - | 0.792 | 1.000 | 0.701 | 0.721 | 1.000 | 1.000 | 1.000 | 0.801 | 0.946 | 0.808 | 0.823 | 0.830 |
| 4 | 0.831 | 0.757 | - | - | 0.881 | 0.721 | 0.779 | 1.000 | 1.000 | 0.587 | 1.000 | 0.942 | 0.906 | 0.822 | 0.887 | 0.979 |
| 5 | 0.738 | 0.531 | - | - | 0.727 | 0.726 | 0.745 | 1.000 | 1.000 | 0.832 | 0.915 | 0.866 | 0.830 | 0.778 | 0.861 | 0.945 |
| 6 | 0.675 | 0.871 | - | - | 0.583 | 0.693 | 0.862 | 0.949 | 0.441 | 0.913 | 0.814 | 0.764 | 0.727 | 0.809 | 0.894 | 0.871 |
| 7 | 1.000 | 0.775 | - | - | 0.707 | 0.790 | 0.919 | 0.860 | 0.842 | 0.735 | 0.947 | 0.825 | 0.821 | 0.830 | 0.955 | 0.859 |
| 8 | 1.000 | 0.814 | - | - | 0.797 | 0.755 | 0.896 | 0.843 | 0.773 | 0.689 | 0.862 | 0.891 | 0.861 | 0.814 | 0.923 | 0.890 |
| 9 | - | 0.606 | - | - | 0.783 | 0.650 | 0.885 | 0.866 | 0.845 | 0.777 | 0.818 | 0.768 | 0.856 | 0.740 | 0.896 | 0.879 |
| 10 | - | - | - | 0.892 | 0.882 | 0.876 | 0.853 | 0.500 | 0.845 | 0.924 | 0.763 | 0.868 | ||||
| 11 | - | - | - | 0.852 | 0.943 | 0.919 | 0.939 | 0.817 | 0.951 | 0.921 | 0.911 | 0.938 | ||||
| 12 | - | - | - | 0.865 | 0.933 | 0.912 | 0.818 | 0.597 | 0.947 | 0.884 | 0.787 | 0.933 | ||||
| 13 | - | - | 0.975 | 0.919 | 0.926 | 0.947 | 0.969 | 0.935 | ||||||||
| 14 | - | - | 0.889 | 0.879 | 0.682 | 0.585 | 0.831 | 0.756 | ||||||||
| 15 | - | - | 0.812 | 0.919 | 0.716 | 0.788 | 0.817 | 0.862 | ||||||||
| 16 | - | - | 0.910 | 0.951 | 0.835 | 0.901 | 0.904 | 0.936 | ||||||||
| 17 | - | 0.931 | 0.812 | 0.895 | ||||||||||||
| 18 | - | 0.920 | 0.737 | 0.851 | ||||||||||||
| 19 | - | 0.856 | 0.722 | 0.807 | ||||||||||||
| 20 | - | 0.793 | 0.662 | 0.749 | ||||||||||||
| 21 | - | 0.872 | 0.786 | 0.839 | ||||||||||||
| ≤3 Months (n = 12) | 4–7 Months (n = 36) | ≥8 Months (n = 22) | Total (n = 70) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Items | Prone | Supine | Sitting | Standing | Prone | Supine | Sitting | Standing | Prone | Supine | Sitting | Standing | Prone | Supine | Sitting | Standing |
| 1 | 1.000 | 0.308 | 1.000 | 1.000 | 1.000 | 0.654 | 1.000 | 1.000 | 1.000 | 0.478 | 1.000 | 1.000 | 1.000 | 0.478 | 1.000 | |
| 2 | 0.400 | 1.000 | 0.400 | 1.000 | 1.000 | 0.769 | 1.000 | 0.485 | 1.000 | 0.864 | 0.735 | 0.485 | 1.000 | 0.864 | 0.735 | |
| 3 | 0.824 | 0.400 | 1.000 | - | 0.654 | 0.654 | 0.769 | 0.862 | 0.818 | 0.569 | 0.899 | 0.850 | 0.818 | 0.569 | 0.899 | 0.850 |
| 4 | 0.750 | 0.625 | - | - | 0.842 | 0.800 | 0.780 | 1.000 | 0.906 | 0.881 | 0.886 | 0.964 | 0.906 | 0.881 | 0.886 | 0.964 |
| 5 | 0.250 | 0.625 | - | - | 0.520 | 0.833 | 0.625 | 1.000 | 0.639 | 0.827 | 0.745 | 0.925 | 0.639 | 0.827 | 0.745 | 0.925 |
| 6 | 1.000 | 1.000 | - | - | 0.536 | 0.667 | 0.799 | 0.842 | 0.730 | 0.714 | 0.909 | 0.811 | 0.730 | 0.714 | 0.909 | 0.811 |
| 7 | 1.000 | - | - | - | 0.827 | 0.942 | 0.852 | 0.636 | 0.857 | 0.886 | 0.909 | 0.598 | 0.857 | 0.886 | 0.909 | 0.598 |
| 8 | 1.000 | - | - | - | 1.000 | 0.778 | 1.000 | 0.873 | 0.881 | 0.885 | 0.969 | 0.881 | 0.881 | 0.885 | 0.969 | 0.881 |
| 9 | - | - | - | - | 0.630 | 0.869 | 0.545 | 1.000 | 0.706 | 0.910 | 0.766 | 0.906 | 0.706 | 0.910 | 0.766 | 0.906 |
| 10 | - | - | - | 0.862 | 1.000 | 0.471 | 0.882 | 0.868 | 0.618 | 0.882 | 0.868 | 0.618 | ||||
| 11 | - | - | - | 0.862 | 0.893 | 1.000 | 0.942 | 0.964 | 0.925 | 0.942 | 0.964 | 0.925 | ||||
| 12 | - | - | - | 0.916 | 0.842 | 1.000 | 0.902 | 0.811 | 0.841 | 0.902 | 0.811 | 0.841 | ||||
| 13 | - | - | 1.000 | 1.000 | 1.000 | 0.925 | 1.000 | 0.925 | ||||||||
| 14 | - | - | 0.801 | 1.000 | 0.851 | 0.639 | 0.851 | 0.639 | ||||||||
| 15 | - | - | 0.722 | 1.000 | 0.711 | 0.747 | 0.711 | 0.747 | ||||||||
| 16 | - | - | 0.906 | 1.000 | 0.930 | 0.785 | 0.930 | 0.785 | ||||||||
| 17 | - | 1.000 | 0.850 | 0.850 | ||||||||||||
| 18 | - | 0.620 | 0.783 | 0.783 | ||||||||||||
| 19 | - | 0.640 | 0.742 | 0.742 | ||||||||||||
| 20 | - | 0.636 | 0.720 | 0.720 | ||||||||||||
| 21 | - | 0.786 | 0.883 | 0.883 | ||||||||||||
| Interrater Reliability | ||||||||
|---|---|---|---|---|---|---|---|---|
| ≤3 Months (n = 12) | 4–7 Months (n = 36) | ≥8 Months (n = 22) | Total (n = 70) | |||||
| ICC | 95% CI | ICC | 95% CI | ICC | 95% CI | ICC | 95% CI | |
| Prone total | 0.981 | 0.956–0.994 | 0.979 | 0.966–0.988 | 0.979 | 0.961–0.990 | 0.987 | 0.981–0.991 |
| Supine total | 0.963 | 0.917–0.988 | 0.981 | 0.969–0.989 | 0.977 | 0.959–0.989 | 0.985 | 0.979–0.990 |
| Sitting total | 0.962 | 0.916–0.988 | 0.993 | 0.989–0.996 | 0.992 | 0.985–0.996 | 0.996 | 0.994–0.997 |
| Standing total | 0.796 | 0.544–0.932 | 0.998 | 0.996–0.999 | 0.995 | 0.991–0.998 | 0.997 | 0.996–0.998 |
| Total | 0.940 | 0.849–0.984 | 0.998 | 0.996–0.999 | 0.995 | 0.991–0.998 | 0.998 | 0.997–0.999 |
| Intrarater Reliability | ||||||||
| ≤3 months (n = 12) | 4–7 months (n = 36) | ≥8 months (n = 22) | Total (n = 70) | |||||
| ICC | 95% CI | ICC | 95% CI | ICC | 95% CI | ICC | 95% CI | |
| Prone total | 0.855 | 0.495–0.958 | 0.973 | 0.947–0.986 | 0.982 | 0.971–0.989 | 0.982 | 0.971–0.989 |
| Supine total | 0.749 | 0.129–0.928 | 0.885 | 0.775–0.942 | 0.940 | 0.904–0.963 | 0.940 | 0.904–0.963 |
| Sitting total | 0.776 | 0.187–0.933 | 0.971 | 0.944–0.985 | 0.987 | 0.979–0.992 | 0.987 | 0.979–0.992 |
| Standing total | 0.867 | 0.540–0.962 | 0.995 | 0.990–0.997 | 0.994 | 0.991–0.996 | 0.994 | 0.991–0.996 |
| Total | 0.940 | 0.792–0.983 | 0.988 | 0.976–0.994 | 0.994 | 0.991–0.996 | 0.994 | 0.991–0.996 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ko, J.; Lim, H.K. Reliability Study of the Items of the Alberta Infant Motor Scale (AIMS) Using Kappa Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1767. https://doi.org/10.3390/ijerph19031767
Ko J, Lim HK. Reliability Study of the Items of the Alberta Infant Motor Scale (AIMS) Using Kappa Analysis. International Journal of Environmental Research and Public Health. 2022; 19(3):1767. https://doi.org/10.3390/ijerph19031767
Chicago/Turabian StyleKo, Jooyeon, and Hyun Kyoon Lim. 2022. "Reliability Study of the Items of the Alberta Infant Motor Scale (AIMS) Using Kappa Analysis" International Journal of Environmental Research and Public Health 19, no. 3: 1767. https://doi.org/10.3390/ijerph19031767
APA StyleKo, J., & Lim, H. K. (2022). Reliability Study of the Items of the Alberta Infant Motor Scale (AIMS) Using Kappa Analysis. International Journal of Environmental Research and Public Health, 19(3), 1767. https://doi.org/10.3390/ijerph19031767





