Impact of the COVID-19 Pandemic on Atopic Dermatitis Patients
Abstract
:1. Introduction
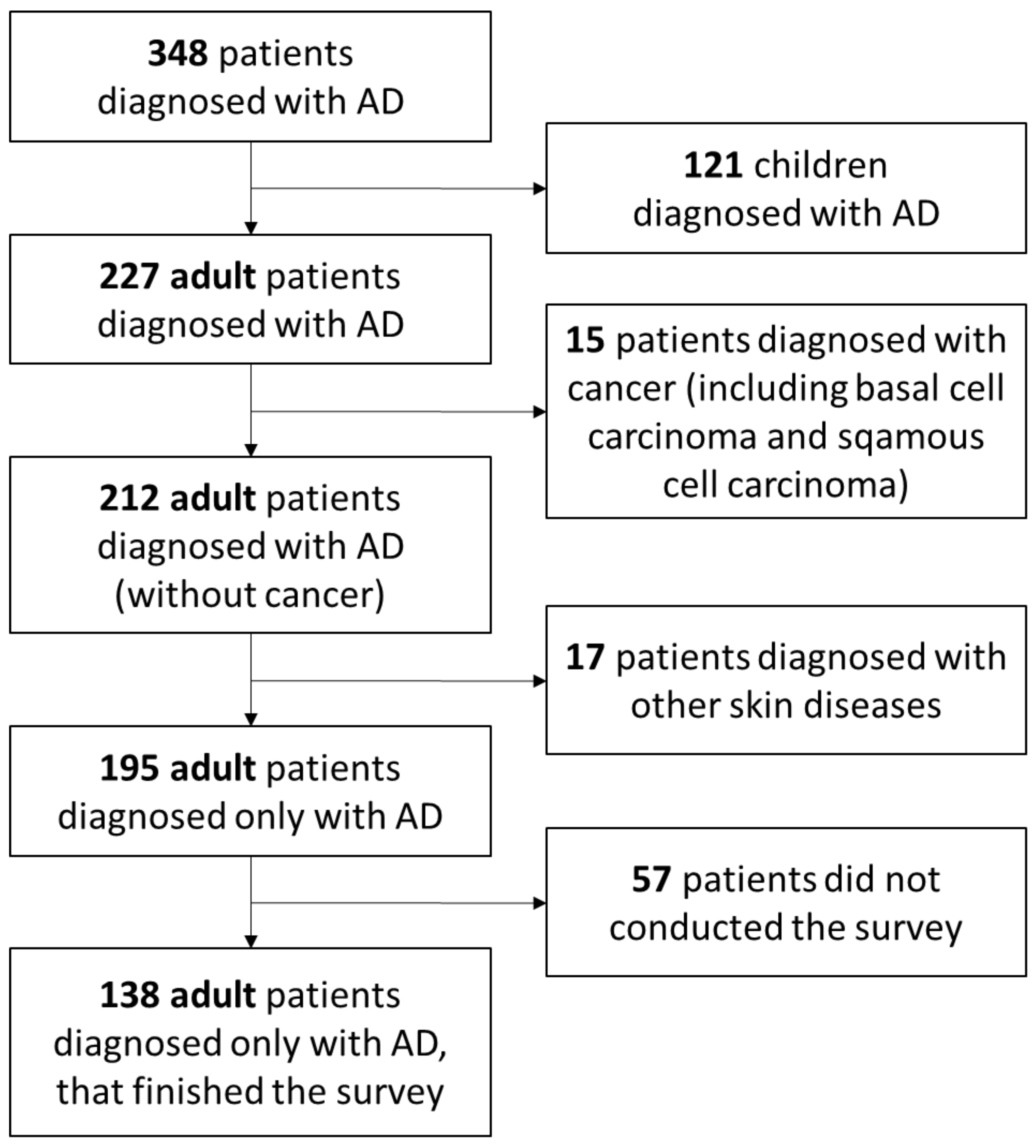
2. Material and Methods
2.1. Survey Structure
2.2. Quality of Life
2.3. Depression and Anxiety
2.4. Analysis
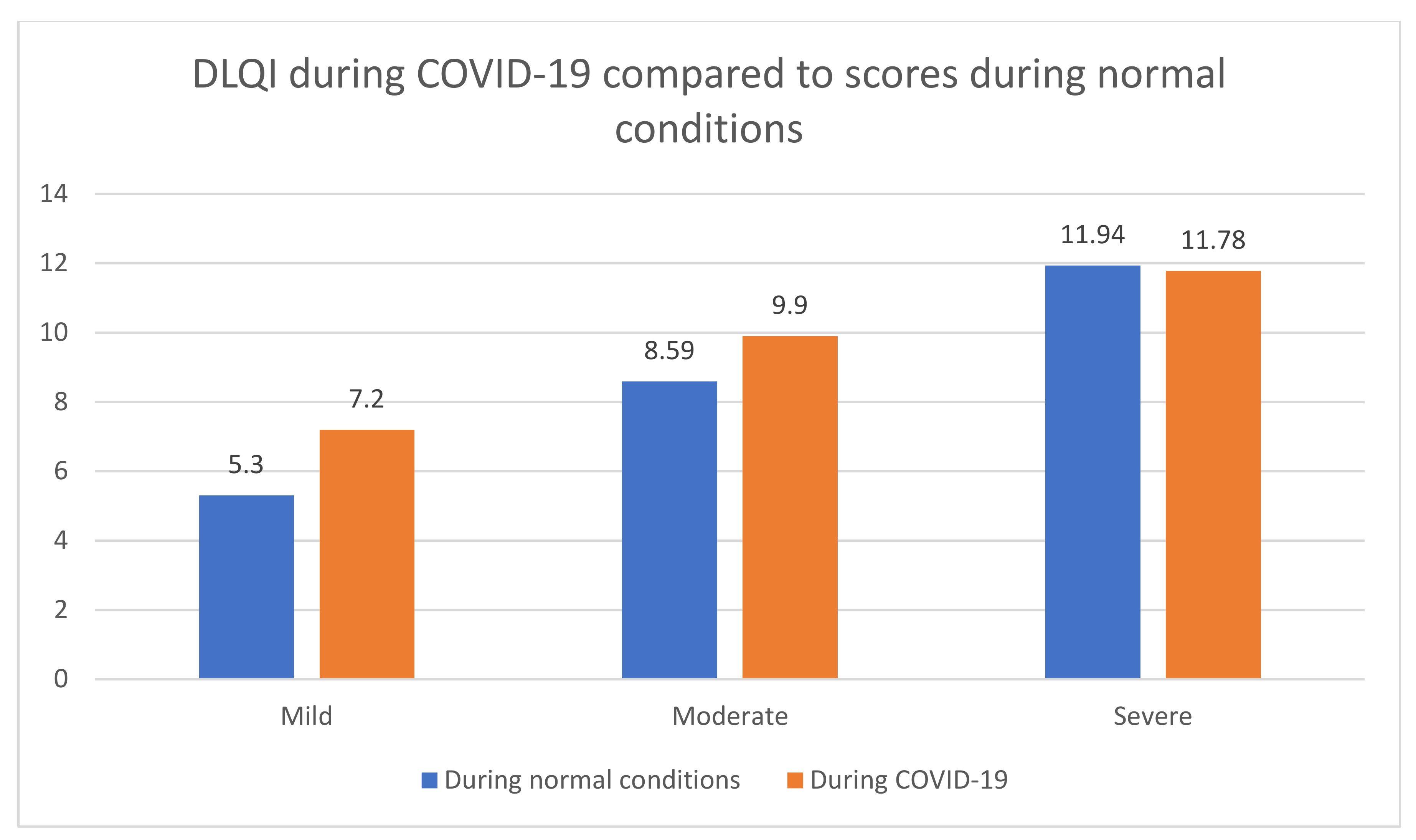
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ständer, S.; Steinhoff, M. Pathophysiology of pruritus in atopic dermatitis: An overview. Exp. Dermatol. 2002, 11, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.; Robertson, C.; Stewart, A.; Aït-Khaled, N.; Anabwani, G.; Anderson, R.; Asher, I.; Beasley, R.; Björkstén, B.; Burr, M.; et al. Worldwide variations in the prevalence of symptoms of atopic eczema in the international study of asthma and allergies in childhood. J. Allergy Clin. Immunol. 1999, 103, 125–138. [Google Scholar] [CrossRef]
- Cork, M.J.; Danby, S.G.; Ogg, G.S. Atopic dermatitis epidemiology and unmet need in the United Kingdom. J. Dermatol. Treat. 2020, 31, 801–809. [Google Scholar] [CrossRef]
- Winge, M.C.G.; Hoppe, T.; Berne, B.; Vahlquist, A.; Nordenskjöld, M.; Bradley, M.; Törmä, H. Filaggrin Genotype Determines Functional and Molecular Alterations in Skin of Patients with Atopic Dermatitis and Ichthyosis Vulgaris. PLoS ONE 2011, 6, e28254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakahara, T.; Kido-Nakahara, M.; Tsuji, G.; Furue, M. Basics and recent advances in the pathophysiology of atopic dermatitis. J. Dermatol. 2021, 48, 130–139. [Google Scholar] [CrossRef]
- Williams, H.C. Epidemiology of atopic dermatitis. Clin. Exp. Dermatol. 2000, 25, 522–529. [Google Scholar] [CrossRef]
- Chrostowska-Plak, D.; Reich, A.; Szepietowski, J. Relationship between itch and psychological status of patients with atopic dermatitis. J. Eur. Acad. Dermatol. Venereol. 2012, 27, e239–e242. [Google Scholar] [CrossRef]
- Birdi, G.; Cooke, R.; Knibb, R. Impact of atopic dermatitis on quality of life in adults: A systematic review and meta-analysis. Int. J. Dermatol. 2020, 59, E75–E91. [Google Scholar] [CrossRef]
- Kobusiewicz, A.; Zalewska-Janowska, A.M.; Lesiak, A.; Narbutt, J. Management of severe atopic dermatitis in adult patients. Dermatol. Rev. 2020, 107, 234–245. [Google Scholar] [CrossRef]
- Stalder, J.-F.; Barbarot, S.; Wollenberg, P.-D.D.A.; Holm, E.A.; De Raeve, L.; Seidenari, S.; Oranje, A.; Deleuran, M.; Cambazard, F.; Svensson, A.; et al. Patient-Oriented SCORAD (PO-SCORAD): A new self-assessment scale in atopic dermatitis validated in Europe: PO-SCORAD self-assessment scale validation. Allergy 2011, 66, 1114–1121. [Google Scholar] [CrossRef]
- Finlay, A.; Khan, G. Dermatology Life Quality Index (DLQI)—A simple practical measure for routine clinical use. Clin. Exp. Dermatol. 1994, 19, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Szepietowski, J.C.; Salomon, J.; Finlay, A.Y.; Klepacki, A.; Chodynicka, B.; Marionneau, N.; Taieb, C.; Myon, E. Dermatology Life Quality Index (DLQI): Polish version. In Proceedings of the 11th International Congress European Society for Dermatology and Psychiatry, Giessen, Germany, 5–7 May 2005; p. 42, poz. [Google Scholar]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silverberg, J.; Gelfand, J.; Margolis, D.; Boguniewicz, M.; Fonacier, L.; Grayson, M.; Ong, P.; Fuxench, Z.C.; Simpson, E. Symptoms and diagnosis of anxiety and depression in atopic dermatitis in U.S. adults. Br. J. Dermatol. 2019, 181, 554–565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holm, J.; Agner, T.; Clausen, M.-L.; Thomsen, S. Quality of life and disease severity in patients with atopic dermatitis. J. Eur. Acad. Dermatol. Venereol. 2016, 30, 1760–1767. [Google Scholar] [CrossRef]
- Tamagawa-Mineoka, R.; Katoh, N. Atopic Dermatitis: Identification and Management of Complicating Factors. Int. J. Mol. Sci. 2020, 21, 2671. [Google Scholar] [CrossRef] [Green Version]
- Zachariae, R.; Zachariae, C.; Ibsen, H.H.; Mortensen, J.T.; Wulf, H.C. Psychological Symptoms and Quality of Life of Dermatology Outpatients and Hospitalized Dermatology Patients. Acta Derm. Venereol. 2004, 84, 205–212. [Google Scholar] [CrossRef] [Green Version]
- Gupta, M.A.; Gupta, A.K. Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. Br. J. Dermatol. 1998, 139, 846–850. [Google Scholar] [CrossRef]
- Armstrong, A.W.; Huang, A.; Wang, L.; Miao, R.; Patel, M.; Gadkari, A.; Mallya, U.G.; Chao, J. Real-world utilization patterns of systemic immunosuppressants among US adult patients with atopic dermatitis. PLoS ONE 2019, 14, e0210517. [Google Scholar] [CrossRef]
- Pérez-Ferriols, A.; Aranegui, B.; Pujol-Montcusí, J.; Martin-Gorgojo, A.; Campos-Domínguez, M.; Feltes, R.; Gilaberte, Y.; Echeverría-García, B.; Alvarez-Pérez, A.; Garcia-Doval, I. Modalidades de fototerapia para el tratamiento de la dermatitis atópica: Revisión sistemática de la literatura. Actas Dermo-Sifiliográficas 2015, 106, 387–401. [Google Scholar] [CrossRef]
- Trettin, B.; Feldman, S.; Andersen, F.; Danbjørg, D.; Agerskov, H. A changed life: The life experiences of patients with psoriasis receiving biological treatment. Br. J. Dermatol. 2020, 183, 516–523. [Google Scholar] [CrossRef]
- Maniadakis, N.; Toth, E.; Schiff, M.; Wang, X.; Nassim, M.; Szegvari, B.; Mountian, I.; Curtis, J.R. A Targeted Literature Review Examining Biologic Therapy Compliance and Persistence in Chronic Inflammatory Diseases to Identify the Associated Unmet Needs, Driving Factors, and Consequences. Adv. Ther. 2018, 35, 1333–1355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chernyshov, P.V. The Evolution of Quality of Life Assessment and Use in Dermatology. Dermatology 2019, 235, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Ricardo, J.W.; Lipner, S.R. Considerations for safety in the use of systemic medications for psoriasis and atopic dermatitis during the COVID-19 pandemic. Dermatol. Ther. 2020, 33, 33. [Google Scholar] [CrossRef] [PubMed]
| PO-SCORAD | HADS-A Score during Normal Conditions [14] | HADS-A Score during the COVID Pandemic | p |
|---|---|---|---|
| Mild | 6.1 (5.5–6.7) | 7.3 (6.0–7.9) | p < 0.05 |
| Moderate | 9.2 (8.2–10.2) | 10.1 (8.6–12.0) | p < 0.05 |
| Severe | 11.2 (9.2–13.1) | 11.3 (9.3–13.0) | p = 0.097 |
| PO-SCORAD | HADS-D Score during Normal Conditions [14] | HADS-D Score during the COVID Pandemic | p |
|---|---|---|---|
| Mild | 4.6 (4.1–5.2) | 5.7 (4.9–6.9) | p < 0.05 |
| Moderate | 7.4 (6.6–8.2) | 8.5 (7.6–10.0) | p < 0.05 |
| Severe | 9.1 (7.8–10.5) | 8.7 (8.3–11.2) | p = 0.142 |
| PO-SCORAD | Usage of Telemedicine Yes | Usage of Telemedicine No |
|---|---|---|
| Mild | 51% | 49% |
| Moderate | 42% | 58% |
| Severe | 26% | 74% |
| PO-SCORAD | Level of Content (LoC) Definitely Yes | LoC Yes | LoC Neutral | LoC No | LoC Definitely No |
|---|---|---|---|---|---|
| Mild | 28% | 25% | 24% | 14% | 9% |
| Moderate | 10% | 14% | 30% | 19% | 27% |
| Severe | 2% | 11% | 28% | 24% | 35% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sieniawska, J.; Lesiak, A.; Ciążyński, K.; Narbutt, J.; Ciążyńska, M. Impact of the COVID-19 Pandemic on Atopic Dermatitis Patients. Int. J. Environ. Res. Public Health 2022, 19, 1734. https://doi.org/10.3390/ijerph19031734
Sieniawska J, Lesiak A, Ciążyński K, Narbutt J, Ciążyńska M. Impact of the COVID-19 Pandemic on Atopic Dermatitis Patients. International Journal of Environmental Research and Public Health. 2022; 19(3):1734. https://doi.org/10.3390/ijerph19031734
Chicago/Turabian StyleSieniawska, Joanna, Aleksandra Lesiak, Karol Ciążyński, Joanna Narbutt, and Magdalena Ciążyńska. 2022. "Impact of the COVID-19 Pandemic on Atopic Dermatitis Patients" International Journal of Environmental Research and Public Health 19, no. 3: 1734. https://doi.org/10.3390/ijerph19031734
APA StyleSieniawska, J., Lesiak, A., Ciążyński, K., Narbutt, J., & Ciążyńska, M. (2022). Impact of the COVID-19 Pandemic on Atopic Dermatitis Patients. International Journal of Environmental Research and Public Health, 19(3), 1734. https://doi.org/10.3390/ijerph19031734







