Prevalence of Disability among the Chinese Older Population: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Quality of Assessment
2.5. Statistical Analysis
3. Results
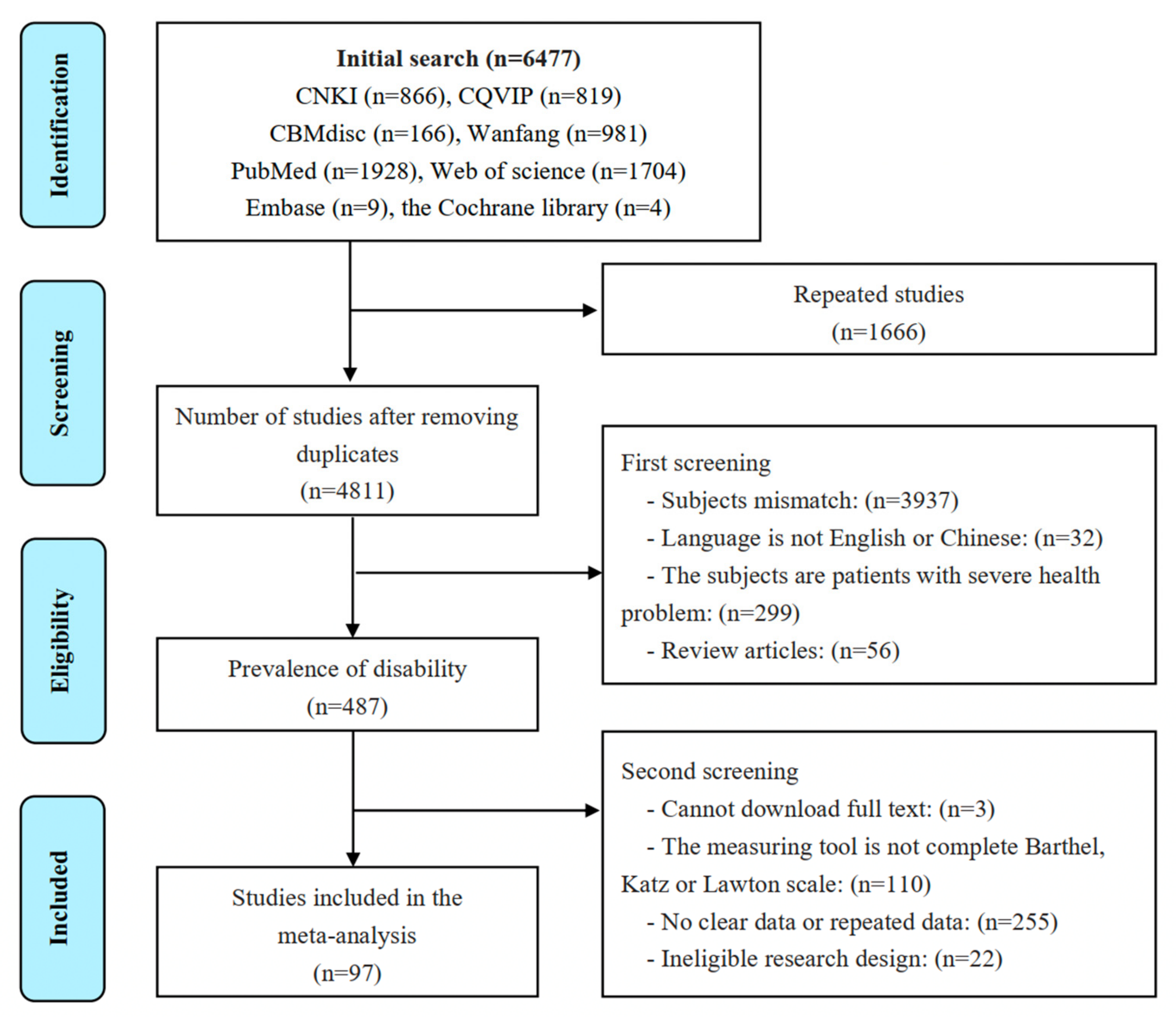
3.1. Search Strategy and Selection Criteria
3.2. Quality Assessment
3.3. Study Characteristics
3.4. Pooled Prevalence of Disability
3.5. Subgroup Analyses
3.6. Assessment of Disability by Using a Specific Type of ADL
3.6.1. BADL
3.6.2. Complete ADL
3.7. Meta-Regression
3.8. Publication Bias and Sensitivity Analyses
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| NO. | Study | Publication Year | Language | Survey Year | Sampling Province | Age (Mean) | Type of ADL | Sample Size | Female (N, %) | Rural (N, %) | Cases of Disability | Rate | Score of Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Huang et al. [27] | 1993 | CH | 1991 * | Sichuan | ≥60 (68.8) | PADL + IADL ** | 1242 | 657 (52.9) | NR | 422 | 33.98 | 6 |
| 2. | Meng et al. [28] | 1996 | CH | 1992 | Beijing | ≥60 | PADL + IADL | 3257 | 1415 (43.44) | NR | 778 | 23.90 | 7 |
| 3. | Tang et al. [29] | 1999 | EN | 1990 | Beijing | ≥60 (71.0) | PADL ** | 3440 | 1733 (50.38) | NR | 629 | 18.28 | 9 |
| 4. | Lv et al. [30] | 2001 | CH | 2000 | Anhui | ≥60 | PADL + IADL | 1424 | NR | NR | 274 | 19.24 | 5 |
| 5a. | Meng et al. [31] | 2002 | CH | 1992 | Beijing | ≥60 (72.3) | PADL | 2783 | NR | NR | 262 | 9.41 | 8 |
| 5b. | Meng et al. [31] | 2002 | CH | 1997 | Beijing | ≥60 (72.0) | PADL | 2786 | NR | NR | 171 | 6.14 | 8 |
| 5c. | Meng et al. [31] | 2002 | CH | 2000 | Beijing | ≥60 (72.9) | PADL | 2667 | NR | NR | 214 | 8.02 | 8 |
| 6. | Wang et al. [32] | 2002 | CH | 2000 | Guangzhou | ≥60 | PADL ** | 1161 | 631 (54.35) | NR | 94 | 8.10 | 7 |
| 7. | Lin et al. [33] | 2002 | CH | 2000 | Beijing | ≥60 | PADL | 895 | NR | NR | 174 | 19.44 | 7 |
| 8. | Ji et al. [34] | 2007 | CH | 2005 * | Jiangsu | ≥60 | PADL + IADL | 337 | NR | NR | 103 | 30.56 | 6 |
| 9. | Yin and Lu [35] | 2007 | EN | 2002 | National | ≥80 | PADL | 8844 | 4938 (55.83) | 4627 (52.3) | 3153 | 35.65 | 10 |
| 10a. | Huang et al. [36] | 2008 | CH | 2006 * | Guizhou | ≥60 (70.2) | PADL | 3221 | 1995 (61.94) | NR | 171 | 5.31 | 7 |
| 10b. | Huang et al. [36] | 2008 | CH | 2006 * | Guizhou | ≥60 (70.2) | IADL | 3221 | 1995 (61.94) | NR | 382 | 11.86 | 7 |
| 11. | Tang et al. [37] | 2009 | CH | 2008 | Hunan | ≥60 | PADL + IADL | 203 | 124 (61.08) | NR | 102 | 50.25 | 7 |
| 12. | Xu et al. [38] | 2011 | CH | 2009 * | Zhejiang | ≥60 (70.0) | PADL + IADL | 753 | 404 (53.65) | 753(100.00) | 129 | 17.13 | 7 |
| 13. | Chen et al. [39] | 2011 | CH | 2010 | Zhejiang | ≥80 (84.8) | PADL ** | 454 | 268 (59.03) | NR | 138 | 30.40 | 9 |
| 14. | Li et al. [40] | 2011 | EN | 2006 | Beijing | ≥60 | PADL + IADL | 1882 | 990 (52.60) | NR | 817 | 43.41 | 5 |
| 15. | Xue et al. [41] | 2011 | CH | 2010 | Shanghai | ≥80 (83.1) | PADL + IADL | 1027 | 140 (13.63) | NR | 674 | 65.63 | 9 |
| 16. | Li et al. [42] | 2012 | CH | 2009 | Shanghai | ≥60 (73.3) | PADL + IADL | 11,338 | 6043 (53.30) | NR | 2013 | 17.75 | 8 |
| 17. | Shi et al. [43] | 2012 | CH | 2011 | Shandong | ≥65 | PADL | 504 | 234 (46.43) | NR | 96 | 19.05 | 8 |
| 18. | Li et al. [44] | 2012 | CH | 2010 * | Ningxia | ≥60 | PADL + IADL ** | 904 | 459 (50.77) | NR | 261 | 28.87 | 7 |
| 19. | Zhang et al. [45] | 2012 | CH | 2010 * | Hebei | ≥60 | PADL + IADL ** | 2161 | NR | NR | 796 | 36.83 | 7 |
| 20. | Yu et al. [46] | 2012 | CH | 2011 | Shanghai | ≥60 | PADL + IADL | 1500 | 842 (56.13) | NR | 589 | 39.27 | 8 |
| 21. | Huang et al. [47] | 2012 | CH | 2008 | Anhui | ≥60 (70.2) | PADL + IADL ** | 1117 | 764 (68.40) | 1117(100.00) | 764 | 68.40 | 8 |
| 22. | Yin et al. [48] | 2012 | CH | 2009 | Zhejiang | ≥60 (71.2) | PADL + IADL ** | 2184 | 1218 (55.77) | 2184(100.00) | 566 | 25.92 | 8 |
| 23. | Zhang and Wei [49] | 2014 | CH | 2013 | Beijing | ≥60 | PADL | 2031 | NR | NR | 200 | 9.85 | 9 |
| 24. | Zhong et al. [50] | 2014 | CH | 2008 | Zhejiang, Gansu | ≥60 | PADL ** | 1157 | 547 (47.28) | 647 (55.92) | 214 | 18.50 | 9 |
| 25. | Yin et al. [51] | 2014 | EN | 2011 | National | ≥80 (92.3) | PADL | 5495 | 3192 (58.09) | NR | 1856 | 33.78 | 9 |
| 26. | Chen et al. [52] | 2015 | CH | 2013* | Fujian | ≥60 (71.5) | PADL | 14,292 | 7404 (51.81) | NR | 610 | 4.27 | 8 |
| 27. | Li et al. [53] | 2015 | CH | 2013* | Ningxia | ≥60 (70.0) | PADL + IADL ** | 817 | 457 (55.94) | NR | 84 | 10.28 | 7 |
| 28. | Li and Yuan [54] | 2015 | CH | 2013 | Shandong | ≥60 | PADL | 416 | 276 (66.19) | 172 (41.25) | 67 | 16.11 | 7 |
| 29. | Zhang et al. [55] | 2015 | CH | 2011 | Chongqing | ≥80 | PADL ** | 227 | 131 (57.71) | NR | 84 | 37.00 | 9 |
| 30. | Zhang et al. [56] | 2016 | EN | 2013 | Shanghai | ≥60 (72.1) | IADL | 8237 | 4473 (53.26) | NR | 1360 | 16.51 | 7 |
| 31. | Gong [57] | 2016 | CH | 2014 | Shanghai | ≥60 | PADL + IADL | 1233 | NR | NR | 226 | 18.33 | 6 |
| 32. | Zhong [58] | 2016 | CH | 2012–2014 | Guangdong | ≥60 | PADL | 1706 | NR | NR | 331 | 19.40 | 7 |
| 33. | Liu et al. [59] | 2016 | EN | 2013 | Beijing | ≥60 (71.4) | PADL | 1036 | 522 (50.40) | NR | 219 | 21.10 | 7 |
| 34. | Peng and Wu [60] | 2016 | CH | 2011 | National | ≥65 | PADL | 9097 | 4918 (54.06) | 4755 (52.27) | 1948 | 21.41 | 10 |
| 35. | Huang et al. [61] | 2016 | CH | 2013–2015 | Zhejiang | ≥60 (73.8) | PADL | 883 | 490 (55.49) | NR | 191 | 21.63 | 8 |
| 36a | Su et al. [62] | 2016 | EN | 2013 | Shanghai | ≥80 | PADL | 2058 | 1191 (57.87) | NR | 478 | 23.23 | 7 |
| 36b. | Su et al. [62] | 2016 | EN | 2013 | Shanghai | ≥80 | IADL | 2058 | 1191 (57.87) | NR | 780 | 37.90 | 7 |
| 37. | Yue and Liu [63] | 2016 | CH | 2011 | National | ≥65 | PADL | 5118 | 2861 (55.90) | NR | 1214 | 23.72 | 10 |
| 38. | Chen et al. [64] | 2016 | CH | 2014 | Shanghai | ≥60 (74.2) | PADL + IADL | 3556 | 2114 (59.45) | NR | 879 | 24.72 | 8 |
| 39. | Yi et al. [65] | 2016 | CH | 2013 | Hubei | ≥65 (73.3) | PADL + IADL ** | 4002 | 2058 (51.42) | 4002(100.00) | 1375 | 34.36 | 8 |
| 40. | Zhang et al. [66] | 2016 | CH | 2014* | Hebei | ≥60 (68.7) | PADL + IADL ** | 2548 | 1322 (51.88) | 1350 (52.98) | 1076 | 42.23 | 7 |
| 41. | Zhai et al. [67] | 2016 | CH | 2011 | Shandong | ≥65 | PADL + IADL | 1355 | 706 (52.10) | 729 (53.80) | 921 | 67.97 | 10 |
| 42. | Luo et al. [68] | 2016 | CH | 2011 | Shandong, Henan, Hebei, Hunan, Guangdong, Guangxi, Hainan, Jiangsu | ≥65 | PADL ** | 2227 | 1227 (55.10) | NR | 553 | 24.83 | 10 |
| 43. | Dong et al. [5] | 2017 | EN | 2011 | Shanghai | ≥60 (71.6) | PADL | 1997 | 1153 (57.74) | NR | 37 | 1.85 | 6 |
| 44a. | Zhang et al. [69] | 2017 | EN | 2005–2014 | National | ≥65 (72.0) | PADL | 26,604 | 13,515 (50.80) | 16,022 (60.22) | 1862 | 7.00 | 9 |
| 44b. | Zhang et al. [69] | 2017 | EN | 2005–2014 | National | ≥65 (72.0) | IADL | 26,604 | 13,515 (50.80) | 16,022 (60.22) | 8513 | 32.00 | 9 |
| 45. | Zhou and Ma [70] | 2017 | CH | 2013 | National | ≥60 (68.9) | PADL | 7629 | 3988 (52.27) | 7629 (100.00) | 668 | 8.76 | 9 |
| 46. | Ding and Wang [71] | 2017 | CH | 2014 | National | 60–79 (67.7) | PADL + IADL | 6959 | 3549 (50.99) | 3897 (56.00) | 1038 | 14.92 | 9 |
| 47. | Jin [72] | 2017 | CH | 2011 | National | ≥60 | PADL ** | 9765 | NR | NR | 2084 | 21.34 | 9 |
| 48. | Li et al. [73] | 2017 | CH | 2013 | Anhui | ≥60 (72.3) | PADL + IADL ** | 746 | 438 (58.71) | NR | 211 | 28.28 | 9 |
| 49. | Hao et al. [74] | 2017 | EN | 2016 | Beijing | ≥60 | PADL + IADL | 1083 | 543 (50.14) | NR | 347 | 32.04 | 8 |
| 50. | Liu et al. [75] | 2017 | CH | 2016 | Shandong | ≥65 | PADL ** | 1196 | NR | NR | 404 | 33.78 | 8 |
| 51. | Wang et al. [76] | 2017 | CH | 2015* | Hebei | ≥60 (75.5) | PADL + IADL ** | 724 | 378 (52.20) | NR | 309 | 42.68 | 6 |
| 52a. | Hu et al. [77] | 2017 | CH | 2014 | National | ≥65 (66.4) | PADL ** | 6168 | 2813 (45.61) | NR | 1517 | 24.59 | 8 |
| 52b. | Hu et al. [77] | 2017 | CH | 2014 | National | ≥65 (66.4) | IADL ** | 6168 | NR | NR | 3864 | 62.65 | 8 |
| 53. | Wu et al. [78] | 2017 | EN | 2010 | Chongqing | ≥100 | PADL | 564 | 471 (83.51) | 564 (100.00) | 370 | 65.60 | 9 |
| 54. | Yang et al. [79] | 2018 | EN | 2015–2016 | Hubei | ≥65 (72.6) | PADL ** | 2096 | 1065 (50.81) | NR | 149 | 7.11 | 8 |
| 55. | Liu et al. [80] | 2018 | CH | 2013 | National | ≥60 | PADL ** | 8751 | NR | NR | 842 | 9.62 | 8 |
| 56. | Ding and Yan [81] | 2018 | CH | 2011 | National | ≥60 | PADL | 7626 | 3801 (49.84) | 5765 (75.60) | 845 | 11.08 | 8 |
| 57a. | Chen et al. [82] | 2018 | EN | 2016–2017 | Guangxi | ≥60 | PADL | 2300 | 1350 (58.70) | NR | 266 | 11.57 | 7 |
| 57b. | Chen et al. [82] | 2018 | EN | 2016–2017 | Guangxi | ≥60 | IADL | 2300 | 1350 (58.70) | NR | 976 | 42.43 | 7 |
| 57c. | Chen et al. [82] | 2018 | EN | 2016–2017 | Guangxi | ≥60 | PADL + IADL | 2300 | 1350 (58.70) | NR | 998 | 43.39 | 7 |
| 58. | Zhai et al. [83] | 2018 | CH | 2016* | Shanghai | ≥60 | PADL + IADL | 4003 | 2257 (56.38) | NR | 473 | 11.82 | 7 |
| 59. | Liu et al. [84] | 2018 | CH | 2010–2014 | Beijing | ≥60 (70.3) | PADL | 4499 | 2684 (59.66) | 2397 (53.28) | 544 | 12.10 | 8 |
| 60. | Xu et al. [85] | 2018 | CH | 2016 | Sichuan | ≥60 | PADL | 890 | 577 (64.83) | NR | 119 | 13.37 | 9 |
| 61. | Wu et al. [86] | 2018 | CH | 2016* | Beijing | ≥60 | PADL + IADL | 1158 | 713 (61.57) | NR | 220 | 19.00 | 8 |
| 62. | Fu et al. [87] | 2018 | EN | 2014 | Hubei | ≥65 (74.3) | PADL + IADL | 1210 | 672 (55.54) | NR | 249 | 20.58 | 7 |
| 63. | Liu et al. [88] | 2018 | EN | 2016* | Hubei | ≥65 | PADL + IADL | 622 | 358 (57.56) | NR | 179 | 28.78 | 6 |
| 64. | Gu and Feng [89] | 2018 | EN | 2000–2009 | National | ≥65 (88.1) | PADL ** | 32,281 | 18,914 (58.59) | NR | 9361 | 29.00 | 9 |
| 65a. | Hou et al. [90] | 2018 | EN | 1998 | National | ≥80 (92.0) | PADL | 8768 | 5240 (59.76) | 5455 (62.21) | 3236 | 36.91 | 10 |
| 65b. | Hou et al. [90] | 2018 | EN | 2000 | National | ≥80 (91.1) | PADL | 10,940 | 6356 (58.10) | 4181 (38.22) | 3805 | 34.78 | 10 |
| 65c. | Hou et al. [90] | 2018 | EN | 2002 | National | ≥80 (92.3) | PADL | 10,905 | 6579 (60.33) | 5785 (53.05) | 4414 | 40.48 | 10 |
| 65d. | Hou et al. [90] | 2018 | EN | 2005 | National | ≥80 (92.5) | PADL | 10,393 | 6260 (60.23) | 5723 (55.07) | 3516 | 33.83 | 10 |
| 65e. | Hou et al. [90] | 2018 | EN | 2008 | National | ≥80 (92.4) | PADL | 11,658 | 7074 (60.68) | 7016 (60.18) | 3318 | 28.46 | 10 |
| 66. | Bai et al. [91] | 2018 | CH | 2013 | Hebei | ≥60 | PADL + IADL | 1374 | 785 (57.13) | NR | 584 | 42.50 | 7 |
| 67. | Gong et al. [92] | 2018 | EN | 2016* | Anhui | ≥60 (70.7) | PADL + IADL | 3182 | 1862 (58.52) | 3182 (100.00) | 1942 | 61.03 | 6 |
| 68. | Dong et al. [93] | 2018 | EN | 2014 | Anhui | ≥60 | PADL + IADL | 945 | 580 (61.38) | 945 (100.00) | 599 | 63.39 | 9 |
| 69a. | Zhang et al. [94] | 2019 | CH | 2015 | Beijing, Shanghai, Hebei, Sichuan, Yunnan, Guangxi | ≥60 | PADL | 23,803 | 13,234 (55.60) | 11,029 (46.33) | 500 | 2.10 | 9 |
| 69b. | Zhang et al. [94] | 2019 | CH | 2015 | Beijing, Shanghai, Hebei, Sichuan, Yunnan, Guangxi | ≥60 | IADL | 23,803 | 13,234 (55.60) | 11,029 (46.33) | 4570 | 19.20 | 9 |
| 79. | Li et al. [95] | 2019 | CH | 2015 | Fujian | ≥60 | PADL ** | 5174 | 2716 (52.49) | NR | 280 | 5.41 | 9 |
| 71. | Liu et al. [96] | 2019 | CH | 2016–2017 | Hebei | ≥60 | PADL + IADL | 3125 | 1670 (53.44) | NR | 324 | 10.37 | 8 |
| 72. | Fu et al. [97] | 2019 | CH | 2017 * | Sichuan | ≥60 | PADL ** | 1000 | 562 (56.20) | NR | 158 | 15.80 | 7 |
| 73. | Chen et al. [98] | 2019 | EN | 2016 | Jiangsu | ≥60 | PADL | 2493 | 1314 (52.71) | 1584 (63.54) | 402 | 16.13 | 7 |
| 74. | Chen et al. [99] | 2019 | EN | 2014 | National | ≥80 | PADL | 4076 | 2308 (56.62) | 2259 (55.42) | 1083 | 26.57 | 9 |
| 75. | Xu et al. [100] | 2019 | CH | 2017 | Hunan | ≥60 | PADL + IADL ** | 194 | NR | 194 (100.00) | 55 | 28.35 | 8 |
| 76. | Bai et al. [101] | 2019 | CH | 2016–2017 | Hebei | ≥60 | PADL + IADL ** | 6171 | 3024 (49.00) | NR | 2489 | 40.33 | 9 |
| 77. | Ma et al. [102] | 2019 | CH | 2016–2017 | Hebei | ≥60 | PADL + IADL ** | 6171 | NR | NR | 2489 | 40.33 | 8 |
| 78. | Zhao et al. [103] | 2019 | CH | 2017 * | Hebei | ≥60 (75.5) | PADL + IADL | 724 | NR | NR | 309 | 42.68 | 7 |
| 79. | Yao et al. [6] | 2019 | CH | 2014–2016 | Hainan | ≥100 (102.8) | PADL | 940 | 765 (81.38) | NR | 670 | 71.28 | 9 |
| 80. | Chen et al. [104] | 2020 | CH | 2015 | National | ≥60 | PADL | 4485 | 2422 (54.00) | NR | 297 | 6.62 | 9 |
| 81. | Ning et al. [105] | 2020 | CH | 2018 | Shandong | ≥60 (69.9) | PADL | 3349 | 1715 (51.21) | NR | 229 | 6.84 | 9 |
| 82. | Xu et al. [106] | 2020 | CH | 2018 * | Hainan | ≥60 | PADL ** | 365 | 213 (58.36) | 221 (60.55) | 29 | 7.95 | 8 |
| 83. | Gu et al. [107] | 2020 | CH | 2018 | Jiangsu | ≥60 (69.4) | PADL | 3259 | 1644 (50.44) | 1544 (47.38) | 344 | 10.56 | 9 |
| 84. | Peng et al. [108] | 2020 | EN | 2018 | Guangdong | ≥60 (71.6) | PADL | 1321 | NR | NR | 160 | 12.11 | 8 |
| 85. | Xu et al. [20] | 2020 | EN | 2018 | Ningxia | ≥60 (70.5) | PADL | 1040 | 513 (49.33) | NR | 179 | 17.21 | 8 |
| 86. | Zhang et al. [109] | 2020 | CH | 2018* | Henan | ≥60 (70.9) | PADL | 5570 | 2825 (50.72) | 4074 (73.14) | 1139 | 20.45 | 6 |
| 87. | Cai et al. [110] | 2020 | CH | 2015 | Yunnan | ≥60 (70.9) | PADL + IADL | 3978 | 2213 (55.63) | 2000 (50.28) | 1017 | 25.57 | 9 |
| 88. | Song et al. [111] | 2020 | CH | 2014 | Shandong | ≥65 | PADL ** | 559 | 254 (45.44) | 312 (55.81) | 143 | 25.58 | 9 |
| 89. | Liu et al. [112] | 2020 | CH | 2015–2018 | Guangdong | ≥60 (74.3) | PADL + IADL ** | 221 | 104 (47.06) | NR | 58 | 26.24 | 9 |
| 90. | Du et al. [113] | 2020 | CH | 2016 | Anhui | ≥60 (71.7) | PADL | 983 | 527 (53.61) | NR | 312 | 31.74 | 10 |
| 91. | Zhang et al. [114] | 2020 | CH | 2016 | Chongqing | ≥65 | PADL + IADL ** | 1341 | 609 (45.41) | NR | 596 | 44.44 | 8 |
| 92. | Lin et al. [115] | 2020 | CH | 2018 * | Yunnan | ≥60 (76.7) | PADL | 182 | 118 (64.84) | NR | 96 | 52.75 | 8 |
| 93. | Xiao et al. [116] | 2021 | EN | 2018 | Guizhou, Yunnan, Sichuan, Xinjiang | ≥60 (69.4) | PADL | 3770 | NR | NR | 488 | 12.94 | 8 |
| 94. | Cheng and Yan [117] | 2021 | EN | 1998–2014 | National | ≥80 | PADL | 30,317 | 17,663 (58.26) | NR | 4884 | 16.11 | 10 |
| 95. | Gao et al. [118] | 2021 | CH | 2017 | Shandong | ≥60 (69.8) | PADL + IADL | 7070 | 4224 (59.75) | NR | 1603 | 22.67 | 9 |
| 96. | Chen et al. [119] | 2021 | CH | 2014 | National | ≥60 (70.5) | PADL | 6182 | 3305 (53.46) | 3337 (53.98) | 1517 | 24.54 | 9 |
| 97. | Yan et al. [120] | 2021 | CH | 2018 | National | ≥65 (85.6) | PADL | 15,771 | 8902 (56.45) | NR | 4196 | 26.61 | 10 |
References
- United Nations Department of Economic and Social Affairs/Population Division World Population Prospects: The 2017 Revision, Key Findings, and Advance Tables. 2017. Available online: https://esa.un.org/unpd/wpp/Publications/Files/WPP2017_KeyFindings.pdf (accessed on 6 December 2021).
- National Bureau of Statistics. The Outcome of the Seventh National Population Census. 2021. Available online: http://www.stats.gov.cn/tjsj/sjjd/202105/t20210512_1817336.html (accessed on 6 December 2021).
- World Health Organization. World Report on Disability. 2011. Available online: www.who.int/disabilities/world_report/2011/en/ (accessed on 6 December 2021).
- The Central People’s Government of the People’s Republic of China. China Releases the Results of the Second National Sample Survey on Disability. 2007. Available online: http://www.gov.cn/jrzg/2007-05/28/content_628517.htm (accessed on 6 December 2021).
- Dong, W.; Wan, J.; Xu, Y.; Chen, C.; Bai, G.; Fang, L.; Sun, A.; Yang, Y.; Wang, Y. Determinants of self-rated health among shanghai elders: A cross-sectional study. BMC Public Health 2017, 17, 807. [Google Scholar] [CrossRef] [Green Version]
- Yao, Y.; Fu, S.H.; Zhang, C.; Lv, F.Q.; Zhang, F.; Luan, F.X.; Zhao, Y.L. A study of health status in Hainan centenarians. Chin. J. Geriatr. 2019, 38, 1413–1417. (In Chinese) [Google Scholar]
- Li, T.; Liu, B.Y.; Wang, J.Y.; Wang, J.; Wu, X.; Liu, B.Y. Meta-analysis on the impaired rate of activities of daily living in the Chinese elderly aged 60 or above from 2010 to 2017. Chin. J. Gerontol. 2020, 40, 2439–2442. (In Chinese) [Google Scholar]
- Wang, Z.J.; Liu, B.; Guo, Z.Y.; Yang, H.M. Meta-analysis on the disability of the elderly in China. Chin. J. Gerontol. 2020, 40, 1671–1674. (In Chinese) [Google Scholar]
- Shao, P. A meta-analysis on the activities of daily living of the Chinese elderly from 2004 to 2014. Chin. J. Gerontol. 2017, 37, 3865–3866. (In Chinese) [Google Scholar]
- World Health Organization. International Classification of Functioning, Disability and Health: ICF; WHO: Geneva, Switzerland, 2001. [Google Scholar]
- Barberger-Gateau, P.; Rainville, C.; Letenneur, L.; Dartigues, J.-F. A hierarchical model of domains of disablement in the elderly: A longitudinal approach. Disabil. Rehabil. 2000, 22, 308–317. [Google Scholar] [CrossRef]
- Salvador-Carulla, L.; Gasca, V.I. Defining disability, functioning, autonomy and dependency in person-centered medicine and integrated care. Int. J. Integr. Care 2010, 10, e025. [Google Scholar] [CrossRef] [Green Version]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Rostom, A.; Dubé, C.; Cranney, A.; Saloojee, N.; Sy, R.; Garritty, C.; Sampson, M.; Zhang, L.; Yazdi, F.; Mamaladze, V.; et al. Celiac Disease. Evid. Rep./Technol. Assess. 2004, 1–6. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Introduction to Meta-Analysis || When Does It Make Sense to Perform a Meta-Analysis? John Wiley & Sons: Chichester, UK, 2009. [Google Scholar] [CrossRef]
- Wu, X.L.; Liu, J.; Dong, T.Y. Longitudinal dynamic analysis of Chinese Elderly’s activities of daily living. Sci. Res. Aging 2018, 6, 28–45. (In Chinese) [Google Scholar]
- Chen, F.; Liu, K. The activities of daily living of the older adults in the community and its influencing factors. Chin. J. Gerontol. 2015, 35, 4662–4664. (In Chinese) [Google Scholar]
- Xu, X.; Yang, L.; Miao, X.; Hu, X.Y. An investigation and analysis of the activities of daily living of older adults living at home in Ningxia Hui Autonomous Region of China: A cross-sectional study. BMC Geriatr. 2020, 20, 369. [Google Scholar] [CrossRef] [PubMed]
- Chalise, H.N.; Saito, T.; Kai, I. Functional disability in activities of daily living and instrumental activities of daily living among Nepalese Newar elderly. Public Health 2008, 122, 394–396. [Google Scholar] [CrossRef]
- Ma, L.N.; Li, Z.Z.; Tang, Z.; Sun, F.; Diao, L.J.; Li, J.; He, Y.; Dong, B.R.; Li, Y. Prevalence and socio-demographic characteristics of disability in older adults in China: Findings from China Comprehensive Geriatric Assessment Study. Arch. Gerontol. Geriat. 2017, 73, 199–203. [Google Scholar] [CrossRef]
- Modig, K.; Andersson, T.; Vaupel, J.; Rau, R.; Ahlbom, A. How long do centenarians survive? Life expectancy and maximum lifespan. J. Intern. Med. 2017, 282, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.G. Why sources of heterogeneity in meta-analysis should be investigated. Br. Med. J. 1994, 309, 1351–1355. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Altman, D.G. Systematic Reviews in Health Care: Meta-Analysis in Context; BMJ Publishing Group: London, UK, 2001. [Google Scholar]
- Gerta, R.; Guido, S.; James, R.C.; Martin, S. Undue reliance on I2 in assessing heterogeneity may mislead. BMC Med. Res. Methodol. 2008, 8, 79. [Google Scholar] [CrossRef] [Green Version]
- Huang, S.Z.; Zhou, J.C. A preliminary study of the ability of the elderly to move in daily life and related factors. Sichuan Ment. Health 1993, 6, 112–114. (In Chinese) [Google Scholar]
- Meng, J.M.; Xiang, M.J.; Zhu, H. Prevalence of Physical Dependence and Factors Related in Beijing Elderly. Geriatr. Health Care 1996, 2, 1–4. (In Chinese) [Google Scholar]
- Tang, Z.; Wang, H.X.; Meng, C.; Wu, X.G.; Ericsson, K.; Winblad, B.; Pei, J.J. The prevalence of functional disability in activities of daily living and instrumental activities of daily living among elderly Beijing Chinese. Arch. Gerontol. Geriat. 1999, 29, 115–125. [Google Scholar] [CrossRef]
- Lv, H.; Li, S.; Ni, Z.Z. The status of chronic conditions among the elderly and the influencing factors related to ADL of old people. Acta Univ. Med. Nahui 2001, 36, 29–32. (In Chinese) [Google Scholar]
- Meng, C.; Xiang, M.J. Epidemiological status and prospect of daily life activity in Beijing. Int. J. Med. 2002, 6, 63–65. (In Chinese) [Google Scholar]
- Wang, M.H.; Liu, Q.; Yang, J.R. Related Factors Analysis on Dependency of Activities of Daily Life for the Elderly. Chin. J. Public Health 2002, 18, 107–109. (In Chinese) [Google Scholar]
- Lin, H.; Zhang, T.H.; Yang, H.; Wang, C.B.; Liu, N.; Zhang, X.P.; Gong, G.C. Analysis of Influential Factors of Activities of Daily Life of the Elderly. Chin. Health Serv. Manag. 2002, 18, 495–497. (In Chinese) [Google Scholar]
- Ji, J.; Zhang, H.; Geng, Q. Relative Analysis on the Depression and ADL Function of the Elderly. China J. Health Psychol. 2007, 11, 1031–1032. (In Chinese) [Google Scholar]
- Yin, D.T.; Lu, J.H. Hierarchical Linear Model Approach to the Determinants of Activities of Daily Living of Chinese Oldest Old at Both Individual and Regional levels. Chin. J. Popul. Resour. 2007, 5, 31–41. [Google Scholar] [CrossRef]
- Huang, W.Y.; Yang, J.Y.; Yang, X.; Cai, Y.Y.; Wang, J.H. The relationship between chronic diseases and daily life function of the elderly in Guiyang community. J. Guiyang Med. Coll. 2008, 33, 132–135. (In Chinese) [Google Scholar]
- Tang, Y.; Xue, G.E.; Chen, Z.Y. A Survey of Self-Care Ability in Elderly People of Ethnic Minority Area of Western Hunan Province. Chin. Gen. Pract. 2009, 12, 1783–1784. (In Chinese) [Google Scholar]
- Xu, X.Q.; Dong, B.; Zhou, W.; Li, Y.J.; Liu, J.; Wang, S.H.; Jiang, Z.Q. A Study on Activities of Daily Living and Its Risk Factors of the Aged in the Rural Areas. Zhejiang J. Prev. Med. 2011, 23, 1–3. (In Chinese) [Google Scholar]
- Chen, X.P.; Fan, Y.F.; Xu, H.; Cao, J.X.; Lu, Y.M. Survey on living status and long-term care of aged citizens in Hangzhou city. J. Nurs. Sci. 2011, 26, 86–89. (In Chinese) [Google Scholar]
- Li, N.; Pang, L.H.; Chen, G.; Song, X.M.; Zhang, J.; Zheng, X.Y. Risk factors for depression in older adults in Beijing. Can. J. Psychiat. 2011, 56, 466–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xue, B.; Chen, X.B.; Ding, D.X.; Shen, Q.; Mou, Y.Y.; Zhong, G.J. Survey and influencing factors on chronic diseases and daily life ability of the elderly. Chin. J. Gerontol. 2011, 31, 4431–4432. (In Chinese) [Google Scholar]
- Li, Y.T.; Feng, X.S.; Yang, F.H.; Gu, X.Y.; Zong, W.H. The Evaluation and Risk Factors of ADL among the Elderly People in Zhabei District. Chin. Prim. Health Care 2012, 26, 42–44. (In Chinese) [Google Scholar]
- Shi, H.W.; Song, A.Q.; Guo, L.Y.; Zhai, J.H.; Wang, W.J.; Kang, D.M. Assessment on the Ability in Activity of Daily Living Among the Urban Elderly in Jining City, 2011. Prev. Med. Trib. 2012, 18, 203–205. (In Chinese) [Google Scholar]
- Li, W.P.; Liu, L.; Song, Q.R.; Zhang, Y.H.; Wang, H.; Gong, A.H. Analysis on the life quality of over 60-year elderly in Litong district of Wuzhong. Ningxia Med. J. 2012, 34, 642–644. (In Chinese) [Google Scholar]
- Zhang, J.Y.; Chang, Y.; Hu, G.Y.; Wu, X.H.; Li, Y.H. A survey on the correlation between daily life ability and cognitive function in the elderly. Chin. J. Misdiagn. 2012, 12, 1642. (In Chinese) [Google Scholar]
- Yu, Q.; Li, H.; Zhang, X.; Gong, Q.Q.; Xu, D.H.; Zhou, J.H. Survey of the needs of the elderly and community care for the elderly who are inaction in the Caohejing community. Shanghai Med. Pharm. J. 2012, 33, 45–47. (In Chinese) [Google Scholar]
- Huang, W.; Ge, X.J.; Hou, S.; Gao, G.P.; Zhang, X.J.; Yu, Y.L. Ability of daily living and its influencing factors among rural elderly in Dabieshan Mountain area. Chin. J. Public Health 2012, 28, 884–886. (In Chinese) [Google Scholar]
- Yin, Z.Q.; Yang, Y.X.; Chen, L.L.; Tu, H.X.; Chen, J. Health status and its influential factors among rural elderly in Zhejiang province. Chin. J. Public Health 2012, 28, 293–295. (In Chinese) [Google Scholar]
- Zhang, W.J.; Wei, M. A Study on the Factors Associated with Preferences for Institutional Care of the Elderly in Urban China: Evidences from Xicheng District of Beijing. Popul. Econ. 2014, 6, 22–34. (In Chinese) [Google Scholar]
- Zhong, Y.Q.; Wang, J.; Zhang, G.J. Analysis on ability of daily living and its influence factors among the elderly. Mod. Prev. Med. 2014, 41, 852–855. (In Chinese) [Google Scholar]
- Yin, Z.; Shi, X.; Kraus, V.B.; Brasher, M.S.; Chen, H.; Liu, Y.; Lv, Y.; Zeng, Y. Gender-Dependent Association of Body Mass Index and Waist Circumference with Disability in the Chinese Oldest. Obesity 2014, 22, 1918–1925. [Google Scholar] [CrossRef] [Green Version]
- Chen, W.; Hao, S.C.; Mao, F.Z.; Fang, Y. Research on the Situation of Elderly Disability and its Impact Factors in Xiamen. Chin. J. Health Stat. 2015, 32, 770–773. (In Chinese) [Google Scholar]
- Li, Y.; Yang, C.; Li, W.P.; Wang, X.X.; Song, Q.R. Activity of daily living and its influencing factors of people over 60, Yinchuan. Mod. Prev. Med. 2015, 42, 1621–1623. (In Chinese) [Google Scholar]
- Li, W.F.; Yuan, C.J. Study on long-term care needs and influencing factors of the elderly. Shandong Soc. Sci. 2015, 12, 67–72. (In Chinese) [Google Scholar]
- Zhang, C.H.; Wang, Y.L.; Ding, X.B.; Mao, D.Q.; Lv, X.Y.; Jiao, Y.; Qi, L.; Shen, Z.Z. The investigation of activities of daily living (ADL) and chronic non-communicable diseases (NCD) for people over age of 80 in Chongqing City. Chin. J. Dis. Control Prev. 2015, 19, 894–896. (In Chinese) [Google Scholar]
- Zhang, W.; Ding, H.; Su, P.; Duan, G.; Chen, R.; Long, J.; Du, L.; Xie, C.; Jin, C.; Hu, C.; et al. Does disability predict attempted suicide in the elderly? A community-based study of elderly residents in Shanghai, China. Aging Ment. Health 2015, 20, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Gong, X.Q. The impact of living arrangement and social support on health services’ utilization among the elderly: Taking shanghai as an example. South China J. Econ. 2016, 1, 11–27. (In Chinese) [Google Scholar]
- Zhong, C.Y.; Wu, C.P.; Huang, S.Q.; Li, L.W.; Ni, D.J.; Xia, H.M. The investigation of the status quo of community disability elderly and their quality of life and family bed service needs. Heilongjiang Med. J. 2016, 40, 457–459. (In Chinese) [Google Scholar]
- Liu, T.; Hao, X.; Zhang, Z. Identifying community health care supports for the elderly and the factors affecting their aging care model preference: Evidence from three districts of Beijing. BMC Health Serv. Res. 2016, 16, 83–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, C.; Wu, M. Research and Analysis on Disability, Dementia and Long-Term Care among Chinese Elders. J. Prev. Med. Chin. People’s Lib. Army 2016, 34, 382–384. (In Chinese) [Google Scholar]
- Huang, X.A.; Lin, J.; Jiang, X.F.; Liang, H.B.; Liu, X.L.; Zang, R.; Wang, D.D.; Li, J.R. An investigation on the situation of disability and its influencing factors among the elderly in community. Zhejiang J. Prev. Med. 2016, 28, 541–545. (In Chinese) [Google Scholar]
- Su, P.; Ding, H.S.; Zhang, W.; Duan, G.F.; Yang, Y.T.; Chen, R.; Duan, Z.J.; Du, L.X.; Xie, C.Y.; Jin, C.L.; et al. The association of multimorbidity and disability in a community-based sample of elderly aged 80 or older in Shanghai, China. BMC Geriatr. 2016, 16, 178. [Google Scholar] [CrossRef] [Green Version]
- Yue, Z.; Liu, E.P. An empirical study on the influencing mechanisms of health services on rural elderly disability—based on the 2011 Chinese longitudinal healthy longevity survey data. J. China Agric. Univ. (Soc. Sci.) 2016, 33, 124–132. (In Chinese) [Google Scholar]
- Chen, J.; Li, W.X.; Liu, Y.X.; Luo, L.; Hua, G.C.; Liang, Y.; Yu, J.L.; Deng, H.J. Daily living activities of the elderly and their influencing factors in Putuo District. Chin. Health Resour. 2016, 19, 65–69. (In Chinese) [Google Scholar] [CrossRef]
- Yi, L.P.; Zhang, X.H.; Wang, K.Y.; Sun, B. Status of the daily living ability among people over 65 years old in rural mountainous area and its influence factors. J. Public Health Prev. Med. 2016, 27, 49–52. (In Chinese) [Google Scholar]
- Zhang, J.; Li, S.X.; Chen, C.X.; Dou, N.; Zhang, M.; Shao, T. The current status of the quality of life among the elderly in Tangshan. Chin. J. Gerontol. 2016, 36, 3306–3307. (In Chinese) [Google Scholar]
- Zhai, X.M.; Zhu, Q.L.; Li, H.Y.; Li, Y. The elderly disability situation and influencing factors in Shandong province. Chin. Nurs. Manag. 2016, 16, 1633–1638. (In Chinese) [Google Scholar]
- Luo, J.S.; Yin, Z.X.; Lv, Y.B.; Wang, J.L.; Shi, X.M. Association between the hypersensitive C-reactive protein and activities of daily living among elderly adults in longevity areas of China. Chin. J. Prev. Med. 2016, 50, 605–610. (In Chinese) [Google Scholar]
- Zhang, X.; Dupre, M.E.; Qiu, L.; Zhou, W.; Zhao, Y.; Gu, D. Urban-rural differences in the association between access to health care and health outcomes among older adults in China. BMC Geriatr. 2017, 17, 151. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.F.; Ma, Y.N. Prevalence and impact factors of disability among elderly people in rural China. Chin. J. Public Health 2017, 33, 1665–1668. (In Chinese) [Google Scholar]
- Ding, B.R.; Wang, Y.J. From Body to Mind: Chinese Elderly People’s Disability Status and Happiness. Popul. Dev. 2017, 23, 82–90. (In Chinese) [Google Scholar]
- Jin, H. Social status and life care of disabled elderly: An analysis based on CLHLS 2011. Zhejiang Acad. J. 2017, 2, 45–50. (In Chinese) [Google Scholar]
- Li, C.; Zhang, X.L.; Zhang, P.; Wang, F.L.; Dong, L.S.; Xing, F.M. Ability of daily living and its influencing factors among community elderlies in Bengbu city. Chin. J. Public Health 2017, 33, 991–993. (In Chinese) [Google Scholar]
- Hao, X.; Gu, J.; Ying, X.; Bo, T.; Fu, W. Social support and care needs of the disabled elderly population: An empirical study based on survey data from Beijing, China. Biosci. Trends 2017, 11, 507–515. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.Y.; Song, P.; Liu, X.X.; Liu, W.H. Investigation on physical function situation of long-term care of disabled elderly in community. Chin. Nurs. Res. 2017, 31, 3875–3876. (In Chinese) [Google Scholar]
- Wang, F.L.; Zhang, L.N.; Zhang, P.; Sun, S.F.; Dong, S.L.; Zhang, X.L.; Xing, F.M.; Liu, X.W.; Guo, X.W. Survey and analysis on the requirements for elderly care service among elderlies with different ADL. Mod. Prev. Med. 2017, 44, 1044–1046. (In Chinese) [Google Scholar]
- Hu, H.W.; Li, Y.Y.; Zhang, C.; Zhang, J.X. Participation of Social Activities, Health Promotion and Disability Prevention: Empirical Analysis based on Active Ageing Structure. Chin. J. Popul. Sci. 2017, 4, 87–96. (In Chinese) [Google Scholar]
- Wu, T.T.; Lu, L.; Luo, L.; Guo, Y.Q.; Ying, L.Y.; Tao, Q.L.; Zeng, H.; Han, L.L.; Shi, Z.M.; Zhao, Y. Factors Associated with Activities of Daily Life Disability among Centenarians in Rural Chongqing, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2017, 14, 1364. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, M.; Guo, Y.; Gong, J.; Deng, M.; Yang, N.; Yan, Y. Relationships between functional fitness and cognitive impairment in Chinese community-dwelling older adults: A cross-sectional study. BMJ Open 2018, 8, e020695. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Dai, T.; Huang, J. Demand and utilization of medical service among home-dwelling elderly with disability in China: 2011–2015. Chin. J. Public Health 2018, 34, 687–689. (In Chinese) [Google Scholar]
- Ding, H.; Yan, J. Research on Disability Rate Estimation of Chinese Elderly and Its Trend. Chin. J. Popul. Sci. 2018, 3, 97–108. (In Chinese) [Google Scholar]
- Chen, S.Y.; Qin, J.; Li, Y.; Wei, Y.; Long, B.S.; Cai, J.S.; Tang, J.X.; Xu, X.; Yu, G.Q.; Zhang, Z.Y. Disability and Its Influencing Factors among the Elderly in a County, Guangxi Province, China. Int. J. Environ. Res. 2018, 15, 1967. [Google Scholar] [CrossRef] [Green Version]
- Zhai, X.T.; Huang, L.M.; Ruan, Y.; Huang, Z.Z.; Fei, J.H.; Ding, G.M.; Qi, S.G.; Wang, Z.H. Status of elderly daily life ability in Songjiang District, Shanghai. Shanghai J. Prev. Med. 2018, 30, 320–323. (In Chinese) [Google Scholar]
- Liu, M.; Wang, J.H.; Yang, S.S.; Yao, Y.; Wang, S.S.; He, Y. Daily activities of the elderly in Beijing community and comparison between urban and rural areas. Chin. J. Epidemiol. 2018, 39, 268–272. (In Chinese) [Google Scholar]
- Xu, X.F.; Chen, Q.; Hu, X.Y. Analysis on the present situation and influencing factors of the self-care ability of the elderly living at home in Chengdu. Chin. J. Mod. Nurs. 2018, 24, 2267–2270. (In Chinese) [Google Scholar]
- Wu, F.Q.; Fan, H.; Xiao, S.Q.; Yang, X.; Xiao, Y.Y.; Wu, Y. The demand for care and its influencing factors in community-dwelling disabled elderly in Beijing. Chin. J. Nurs. 2018, 53, 841–845. (In Chinese) [Google Scholar]
- Fu, C.; Yang, F.; Mao, Z. Factors associated with cognitive decline among elderly in Wuhan, China living alone versus those living with children. Southeast Asian J. Trop. Med. Public Health 2018, 49, 696–706. [Google Scholar]
- Liu, X.; Yin, X.; Tan, A.; He, M.; Jiang, D.; Hou, Y.; Lu, Y.; Mao, Z. Correlates of Mild Cognitive Impairment of Community-Dwelling Older Adults in Wuhan, China. Int. J. Environ. Res. Public Health 2018, 15, 2705. [Google Scholar] [CrossRef] [Green Version]
- Gu, D.; Feng, Q. Psychological resilience of Chinese centenarians and its associations with survival and health: A fuzzy set analysis. J. Gerontol. B-Psychol. 2018, 73, 880–889. [Google Scholar] [CrossRef] [Green Version]
- Hou, C.; Ping, Z.; Yang, K.; Chen, S.; Liu, X.; Li, H.; Liu, M.; Halmlutterod, N.V.; Tao, L. Trends of Activities of Daily Living Disability Situation and Association with Chronic Conditions among Elderly Aged 80 Years and Over in China. J. Nutr. Health Aging 2018, 22, 439–445. [Google Scholar] [CrossRef]
- Bai, Y.P.; Wang, Q.; Jin, R.; Zhang, X.L.; Wang, F.L.; Xing, F.M. The present situation of the elderly at home in Hebei Province and its relationship with living habits and physical condition. Chin. J. Gerontol. 2018, 38, 201–203. (In Chinese) [Google Scholar]
- Gong, F.F.; Zhao, D.D.; Zhao, Y.Y.; Lu, S.S.; Qian, Z.Z.; Sun, Y.H. The factors associated with geriatric depression in rural China: Stratified by household structure. Psychol. Health Med. 2018, 23, 593–603. [Google Scholar] [CrossRef]
- Dong, B.; Li, J.; Zhao, D.D.; Yu, D.D.; Ren, Q.Q.; Sun, Y.H. The associated factors for the quality of life among Chinese rural elderly: 1-year follow-up study. J. Public Health-Heid. 2018, 26, 185–193. [Google Scholar] [CrossRef]
- Zhang, H.; Wang, Z.H.; Wang, L.M.; Qi, S.G.; Li, Z.X. Survey on the disability of the elderly residents in Chinese community. Chin. J. Epidemiol. 2019, 3, 266–271. (In Chinese) [Google Scholar]
- Li, Z.; Xu, H.N.; Wang, D.W. Care demand and its determinants among community disabled elderly in Fujian province. Chin. J. Public Health 2019, 35, 1205–1209. (In Chinese) [Google Scholar]
- Liu, X.M.; Chen, C.X.; Wang, J.H. Analysis of frailty status and influencing factors of the elderly in community. Chin. Nurs. Res. 2019, 33, 390–393. (In Chinese) [Google Scholar]
- Fu, M.X.; Lin, Q.; Zhang, M.X.; Liu, L.F. The population structure of disabled elderly in Chengdu and its enlightenment to long-term care service model. World Latest Med. Inf. 2019, 19, 225–228. (In Chinese) [Google Scholar]
- Chen, N.; Li, X.; Yuan, N.; Zhou, C.C.; Wang, C.Q. Utilization willingness of institutional care between disabled and non-disabled seniors: Evidence from Jiangsu, China. BMC Health Serv. Res. 2019, 19, 410. [Google Scholar] [CrossRef]
- Chen, N.; Li, X.; Wang, J.; Zhou, C.C.; Wang, C.Q. Rural-urban differences in the association between disability and body mass index among the oldest-old in China. Arch. Gerontol. Geriat. 2019, 81, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.X.; Mao, K.; Wang, K.D.; Gong, F.; Zhang, J.; Wang, W.H. The present situation of the daily living activities of the elderly in rural areas. Chin. J. Gerontol. 2019, 39, 5837–5840. (In Chinese) [Google Scholar]
- Bai, J.W.; Ma, X.B.; Chen, C.X. Disability Status of Community-dwelling Elderly and the Influence of Chronic Diseases on Them. Chin. Gen. Pract. 2019, 22, 43–47. (In Chinese) [Google Scholar]
- Ma, X.B.; Bai, J.W.; Chen, C.X. Disability status of the elderly in community and its influence on the behavior of seeking medical care. Chin. J. Gerontol. 2019, 39, 4079–4081. (In Chinese) [Google Scholar]
- Zhao, M.; Zhang, X.L.; Han, H.; Wang, F.L.; Xing, F.M. Influence of different health for the home endowment needs of elderly people. Chin. J. Gerontol. 2019, 39, 189–192. (In Chinese) [Google Scholar]
- Chen, J.F.; Xiao, C.H.; Fang, M.W.; Ma, X. The influence of physical fitness on the activity of daily living in Chinese elderly. Chin. J. Epidemiol. 2020, 41, 220–225. (In Chinese) [Google Scholar]
- Ning, P.; Du, E.Q.; Du, C.J.; Meng, Q.H.; Wu, B.Y. Prevalence of the disability and inflection point age of the disability level change, Shandong Province. Mod. Prev. Med. 2020, 47, 1633–1636. (In Chinese) [Google Scholar]
- Xu, S.; Huang, X.L.; Yan, J.W.; Li, T.; Gao, F.; Chen, C.L. Analysis on the Self-care Ability of the Elderly in Haikou and Its Influencing Factors. Jiangsu Health Syst. Manag. 2020, 31, 1672–1676. (In Chinese) [Google Scholar]
- Gu, X.Y.; Xu, A.J.; Dai, S.Y.; Chen, A.Q. Study on the ability of daily life activities and its influencing factors among the elderly in Jiangsu province. Chin. J. Health Educ. 2020, 36, 821–825. (In Chinese) [Google Scholar]
- Peng, X.; Bao, X.Y.; Xie, Y.X.; Zhang, X.X.; Huang, J.X.; Liu, Y.; Cheng, M.J.; Liu, N.; Wang, P.X. The mediating effect of pain on the association between multimorbidity and disability and impaired physical performance among community-dwelling older adults in southern China. Aging Clin. Exp. Res. 2020, 32, 1327–1334. [Google Scholar] [CrossRef]
- Zhang, T.T.; Tian, Q.F.; Cao, M.; Huang, J.Y.; Guo, Q. The Study on the activity of daily living of the elderly in Henan Province and the inflection point of attenuation. Mod. Prev. Med. 2020, 47, 4129–4132. (In Chinese) [Google Scholar]
- Cai, Y.N.; Xiao, Y.Z.; Zhang, H.M. Impairment and influencing factors of ability in activities of daily living among residents aged 60 years and over in Yunnan Province. South China J. Prev. Med. 2020, 46, 205–209. (In Chinese) [Google Scholar]
- Song, Y.Y.; Yang, H.; Hu, X.H. Self-care ability of the elderly in daily life and its influencing factors in Shandong Province. Chin. J. Hosp. Stat. 2020, 27, 268–271. (In Chinese) [Google Scholar]
- Liu, Q.Y.; Chang, J.; Su, X.M. Exploring the impact of disability and chronic disease on the elderly in community. Cap. Food Med. 2020, 27, 142–143. (In Chinese) [Google Scholar]
- Du, Z.P.; Wang, Q.; Li, Y.L.; Lu, J.; Feng, S.; Biao, Y.S.; Cao, H.J.; Yang, L.S.; Tao, F.B. Associations between chronic diseases and activities of daily living of elderly in Liu’an urban and rural communities. Acta Univ. Med. Anhui 2020, 55, 1758–1762. (In Chinese) [Google Scholar]
- Zhang, L.; Chen, J.; Lu, L.; Rong, H.H.; Peng, Y. Influencing factors for activities of daily living in the elderly people in Chongqing. Prev. Med. 2020, 32, 22–26. (In Chinese) [Google Scholar]
- Lin, Y.; Dong, Z.J.; Xu, C.Z.; Zhao, Y.N.; You, D.Y.; Zhang, J.J. Survey on disability status, its influencing factors and correlation with health utility among elderly residents in urban communities of Kunming. J. Kunming Med. Univ. 2020, 41, 44–50. (In Chinese) [Google Scholar]
- Xiao, Y.; Jia, S.; Zhao, W.; Zhang, Y.; Qiao, R.; Xia, X.; Hou, L.; Dong, B.R. The combined effect of hearing impairment and cognitive impairment with health-related outcomes in Chinese older people. J. Nutr. Health Aging 2021, 25, 783–789. [Google Scholar] [CrossRef]
- Cheng, G.; Yan, Y. Sociodemographic, health-related, and social predictors of subjective well-being among Chinese oldest-old: A national community-based cohort study. BMC Geriatr. 2021, 21, 124. [Google Scholar] [CrossRef]
- Gao, Z.R.; Xu, L.Z.; Hu, F.F.; Hong, Z. Demand analysis of long-term care services for the elderly based on daily living ability assessment. Chin. J. Hosp. Adm. 2021, 37, 130–134. (In Chinese) [Google Scholar]
- Chen, L.; Wei, X.X.; Wang, F.L.; Jing, L.W.; Xing, F.M.; Hao, Z.M. Disability status and related factors among the elderly over 60 years old in China. Mod. Prev. Med. 2021, 48, 1241–1245. (In Chinese) [Google Scholar]
- Yan, W.; He, M.J.; Lu, Y.; Chang, F. Research on status quo and influencing factors of elderly disability in China based on CLHLS. Chin. Nurs. Res. 2021, 35, 1807–1811. (In Chinese) [Google Scholar]
| Item | Yes | No | Unclear |
|---|---|---|---|
| (1) Define the source of information (survey, record review) | 97 | 0 | 0 |
| (2) List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications | 97 | 0 | 0 |
| (3) Indicate time period used for identifying patients | 78 | 19 | 0 |
| (4) Indicate whether or not subjects were consecutive if not population-based | 97 | 0 | 0 |
| (5) Indicate if evaluators of subjective components of the study were masked to other aspects of the status of the participants | 0 | 97 | 0 |
| (6) Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) | 60 | 36 | 1 |
| (7) Explain any patient exclusions from the analysis | 89 | 7 | 1 |
| (8) Describe how confounding was assessed and/or controlled. | 65 | 32 | 0 |
| (9) If applicable, explain how missing data were handled in the analysis | 13 | 82 | 2 |
| (10) Summarize patient response rates and completeness of data collection | 86 | 11 | 0 |
| (11) Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained | 0 | 97 | 0 |
| Variables | Classification | Number of Studies | Number of Results | Event Rate (%) | 95% CI (%) | Heterogeneity I2 (%) | Q-Value | p-Value |
|---|---|---|---|---|---|---|---|---|
| Pooled prevalence | 97 | 110 | 26.2 | 23.7–28.6 | 99.9 | 81,405.53 | ||
| Type of ADL | BADL | 56 | 62 | 20.5 | 17.7–23.3 | 99.9 | 26.55 | <0.001 |
| IADL | 7 | 7 | 31.8 | 21.2–42.4 | 99.9 | |||
| BADL + IADL | 41 | 41 | 33.8 | 29.4–38.3 | 99.6 | |||
| Gender | Male | 53 | 60 | 22.7 | 20.0–25.5 | 99.7 | 5.35 | 0.021 |
| Female | 53 | 60 | 28.5 | 24.5–32.5 | 99.8 | |||
| Age group | 60–69 | 23 | 26 | 12.8 | 10.1–15.5 | 99.6 | 104.92 | <0.001 |
| 70–79 | 23 | 26 | 22.4 | 16.5–28.3 | 99.7 | |||
| ≥80 | 36 | 44 | 36.8 | 33.1–40.5 | 99.6 | |||
| Region | Eastern China | 32 | 33 | 27.0 | 22.3–31.7 | 99.8 | 2.44 | 0.786 |
| Northern China | 18 | 20 | 26.0 | 19.9–32.1 | 99.7 | |||
| Southern China | 6 | 6 | 24.2 | 8.0–40.3 | 99.7 | |||
| Central China | 7 | 7 | 26.9 | 17.9–35.8 | 99.4 | |||
| Southwest China | 10 | 13 | 30.9 | 22.3–39.4 | 99.7 | |||
| Northwest China | 4 | 4 | 21.3 | 12.3–30.3 | 97.8 | |||
| Hukou | Urban | 17 | 22 | 22.4 | 16.9–27.9 | 99.9 | 2.13 | 0.143 |
| Rural | 26 | 31 | 28.0 | 22.9–33.0 | 99.9 | |||
| Survey year | 1999 and before | 5 | 6 | 21.4 | 10.4–32.4 | 99.8 | 2.16 | 0.706 |
| 2000–2004 | 6 | 7 | 23.7 | 13.0–34.3 | 99.8 | |||
| 2005–2009 | 10 | 12 | 29.1 | 21.6–36.7 | 99.7 | |||
| 2010–2014 | 41 | 43 | 27.7 | 23.6–31.8 | 99.8 | |||
| 2015–2019 | 36 | 38 | 25.3 | 20.9–29.7 | 99.9 | |||
| Variables | Classification | Number of Studies | Number of Results | Event Rate (%) | 95% CI (%) | Heterogeneity I2 (%) | Q-Value | p-Value |
|---|---|---|---|---|---|---|---|---|
| Pooled prevalence | 56 | 62 | 20.5 | 17.7–23.3 | 99.9 | 45,852.90 | ||
| Gender | Male | 37 | 41 | 19.4 | 16.4–22.4 | 99.7 | 3.95 | 0.047 |
| Female | 37 | 41 | 25.1 | 20.3–29.9 | 99.8 | |||
| Age group | 60–69 | 17 | 17 | 7.3 | 5.7–8.9 | 98.6 | 111.60 | <0.001 |
| 70–79 | 17 | 17 | 13.1 | 10.4–15.9 | 98.4 | |||
| ≥80 | 29 | 33 | 30.0 | 26.2–33.9 | 99.6 | |||
| Region | Eastern China | 15 | 15 | 16.8 | 13.5–20.1 | 99.3 | 10.45 | 0.005 |
| Northern China | 6 | 8 | 12.9 | 9.7–16.1 | 99.2 | |||
| Other regions * | 16 | 16 | 24.4 | 18.0–30.7 | 99.5 | |||
| Hukou | Urban | 14 | 18 | 22.6 | 16.1–29.2 | 99.9 | 0.00 | 0.944 |
| Rural | 16 | 20 | 22.4 | 17.4–27.3 | 99.9 | |||
| Survey year | 2009 and before * | 8 | 14 | 21.7 | 14.2–29.1 | 99.9 | 0.78 | 0.678 |
| 2010–2014 | 25 | 25 | 21.3 | 17.6–25.1 | 99.7 | |||
| 2015–2019 | 20 | 20 | 18.9 | 14.3–23.4 | 99.8 | |||
| Variables | Classification | Number of Studies | Number of Results | Event Rate (%) | 95% CI (%) | Heterogeneity I2 (%) | Q-Value | p-Value |
|---|---|---|---|---|---|---|---|---|
| Pooled prevalence | 41 | 41 | 33.8 | 29.4–38.3 | 99.6 | 10,997.47 | ||
| Gender | Male | 16 | 16 | 32.2 | 23.1–41.4 | 99.5 | 0.52 | 0.472 |
| Female | 16 | 16 | 36.7 | 28.7–44.7 | 99.4 | |||
| Age group | 60–69 | 6 | 6 | 25.5 | 14.0–36.9 | 99.7 | 22.45 | <0.001 |
| 70–79 | 6 | 6 | 40.5 | 24.9–56.1 | 99.6 | |||
| ≥80 | 7 | 7 | 61.9 | 51.9–71.9 | 97.3 | |||
| Region | Eastern China | 16 | 16 | 36.4 | 27.8–44.9 | 99.8 | 1.10 | 0.578 |
| Northern China | 12 | 12 | 34.7 | 26.9–42.4 | 99.6 | |||
| Other regions * | 12 | 12 | 31.2 | 25.1–37.2 | 99.6 | |||
| Survey year | 2009 and before * | 10 | 10 | 32.9 | 24.4–41.5 | 99.5 | 0.38 | 0.827 |
| 2010–2014 | 15 | 15 | 35.9 | 27.4–44.3 | 99.7 | |||
| 2015–2019 | 16 | 16 | 32.5 | 24.9–40.1 | 99.7 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, P.-P.; Guo, Z.-L.; Du, X.-J.; Yang, H.-M.; Wang, Z.-J. Prevalence of Disability among the Chinese Older Population: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1656. https://doi.org/10.3390/ijerph19031656
Zheng P-P, Guo Z-L, Du X-J, Yang H-M, Wang Z-J. Prevalence of Disability among the Chinese Older Population: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(3):1656. https://doi.org/10.3390/ijerph19031656
Chicago/Turabian StyleZheng, Pian-Pian, Zi-Le Guo, Xiao-Jing Du, Han-Mo Yang, and Zhen-Jie Wang. 2022. "Prevalence of Disability among the Chinese Older Population: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 3: 1656. https://doi.org/10.3390/ijerph19031656
APA StyleZheng, P.-P., Guo, Z.-L., Du, X.-J., Yang, H.-M., & Wang, Z.-J. (2022). Prevalence of Disability among the Chinese Older Population: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(3), 1656. https://doi.org/10.3390/ijerph19031656






