Pain-Related Worrying and Goal Preferences Determine Walking Persistence in Women with Fibromyalgia
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Variables and Instruments
2.3. Design and Procedure
2.4. Research Design
2.5. Statistics
3. Results
3.1. Decision Making about Stopping or Following through with Walking Each 6 Min Bout
3.2. Walking Performance along the Walking Task
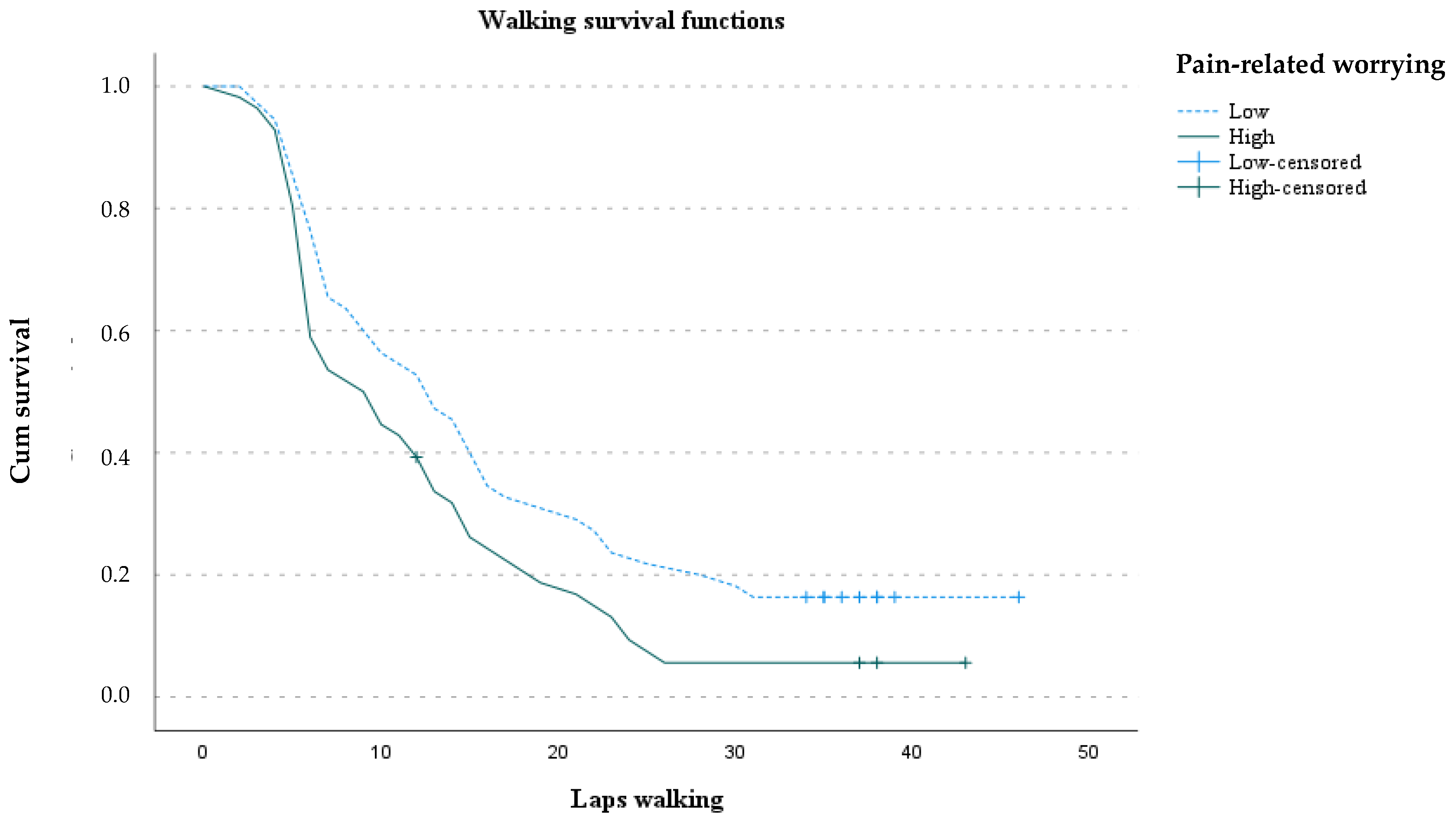
3.2.1. Total Number of Complete Laps: Survival Analysis
3.2.2. Total Walking Distance: Mediational Model of Pain-related Worrying through Goal Preference
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arnold, L.M.; Choy, E.; Clauw, D.J.; Goldenberg, D.L.; Harris, R.E.; Helfenstein, M.; Jensen, T.S.; Noguchi, K.; Silverman, S.L.; Ushida, T.; et al. Fibromyalgia and chronic pain syndromes: A white paper detailing current challenges in the field. Clin. J. Pain 2016, 32, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Häuser, W.; Ablin, J.; Fitzcharles, M.A.; Littlejohn, G.; Luciano, J.V.; Usui, C.; Walitt, B. Fibromyalgia. Nat. Rev. Dis. Prim. 2015, 1, 15022. [Google Scholar] [CrossRef] [PubMed]
- Sarzi-Puttini, P.; Giorgi, V.; Marotto, D.; Atzeni, F. Fibromyalgia: An update on clinical characteristics, aetiopathogenesis and treatment. Nat. Rev. Rheumatol. 2020, 16, 645–660. [Google Scholar] [CrossRef]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Flub, E.; Choy, E.; Kosek, E.; Amris, K.; Branco, J.; et al. EULAR revised recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 2017, 76, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Andrade, A.; Dominski, F.H.; Sieczkowska, S.M. What we already know about the effects of exercise in patients with fibromyalgia: An umbrella review. Semin. Arthritis Rheum. 2020, 50, 1465–1480. [Google Scholar] [CrossRef]
- Bidonde, J.; Busch, A.J.; Schachter, C.L.; Webber, S.C.; Musselman, K.E.; Overend, T.J.; Góes, S.M.; Dal Bello-Haas, V.; Boden, C. Mixed exercise training for adults with fibromyalgia. Cochrane Database Syst. Rev. 2019, 2019. [Google Scholar] [CrossRef]
- Bidonde, J.; Boden, C.; Foulds, H.; Kim, S.Y. Physical Activity and Exercise Training for Adults with Fibromyalgia. In Fibromyalgia Syndrome; Ablin, J.N., Schoenfeld, Y., Eds.; Springer: Cham, Switzerland, 2021; pp. 59–72. [Google Scholar]
- Loftus, N.; Dobbin, N.; Crampton, J.S. The effects of a group exercise and education programme on symptoms and physical fitness in patients with fibromyalgia: A prospective observational cohort study. Disabil. Rehabil. 2021, 1–8. [Google Scholar] [CrossRef]
- Pulido-Martos, M.; Luque-Reca, O.; Segura-Jiménez, V.; Álvarez-Gallardo, I.C.; Soriano-Maldonado, A.; Acosta-Manzano, P.; Gavilán-Carrera, B.; McVeigh, J.G.; Geenen, R.; Delgado-Fernández, M.; et al. Physical and psychological paths toward less severe fibromyalgia: A structural equation model. Ann. Phys. Rehabil. Med. 2020, 63, 46–52. [Google Scholar] [CrossRef]
- Segura-Jiménez, V.; Borges-Cosic, M.; Soriano-Maldonado, A.; Estévez-López, F.; Álvarez-Gallardo, I.C.; Herrador-Colmenero, M.; Delgado-Fernández, M.; Ruiz, J.R. Association of sedentary time and physical activity with pain, fatigue, and impact of fibromyalgia: The al-Ándalus study. Scand. J. Med. Sci. Sports 2017, 27, 83–92. [Google Scholar] [CrossRef]
- Steiner, J.L.; Bigatti, S.M.; Ang, D.C. Trajectory of change in pain, depression, and physical functioning after physical activity adoption in fibromyalgia. J. Health Psychol. 2015, 20, 931–941. [Google Scholar] [CrossRef]
- Thieme, K.; Mathys, M.; Turk, D.C. Evidenced-Based Guidelines on the Treatment of Fibromyalgia Patients: Are They Consistent and If Not, Why Not? Have Effective Psychological Treatments Been Overlooked? J. Pain 2017, 18, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.H.; Nevill, A.M.; Murtagh, E.M.; Holder, R.L. The effect of walking on fitness, fatness and resting blood pressure: A meta-analysis of randomised, controlled trials. Prev. Med. 2007, 44, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Murtagh, E.M.; Nichols, L.; Mohammed, M.A.; Holder, R.; Nevill, A.M.; Murphy, M.H. The effect of walking on risk factors for cardiovascular disease: An updated systematic review and meta-analysis of randomised control trials. Prev. Med. 2015, 72, 34–43. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, S.R.; Tully, M.A.; Ryan, B.; Bleakley, C.M.; Baxter, G.D.; Bradley, J.M.; McDonough, S.M. Walking exercise for chronic musculoskeletal pain: Systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2015, 96, 724–734.E3. [Google Scholar] [CrossRef] [PubMed]
- McLoughlin, M.J.; Colbert, L.H.; Stegner, A.J.; Cook, D.B. Are women with fibromyalgia less physically active than healthy women? Med. Sci. Sports Exerc. 2011, 43, 905–912. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Segura-Jiménez, V.; Ortega, F.B.; Álvarez-Gallardo, I.C.; Camiletti-Moirón, D.; Aparicio, V.A.; Carbonell-Baeza, A.; Femia, P.; Munguía-Izquierdo, D.; Delgado-Fernández, M. Objectively measured sedentary time and physical activity in women with fibromyalgia: A cross-sectional study. BMJ Open 2013, 3, 1–9. [Google Scholar] [CrossRef]
- Estévez-López, F.; Álvarez-Gallardo, I.C.; Segura-Jiménez, V.; Soriano-Maldonado, A.; Borges-Cosic, M.; Pulido-Martos, M.; Aparicio, V.A.; Carbonell-Baeza, A.; Delgado-Fernández, M.; Geenen, R. The discordance between subjectively and objectively measured physical function in women with fibromyalgia: Association with catastrophizing and self-efficacy cognitions. The al-Ándalus project. Disabil. Rehabil. 2018, 40, 329–337. [Google Scholar] [CrossRef]
- López-Roig, S.; Pastor, M.Á.; Peñacoba, C.; Lledó, A.; Sanz, Y.; Velasco, L. Prevalence and predictors of unsupervised walking and physical activity in a community population of women with fibromyalgia. Rheumatol. Int. 2016, 36, 1127–1133. [Google Scholar] [CrossRef]
- Sanz-Baños, Y.; Pastor-Mira, M.Á.; Lledó, A.; López-Roig, S.; Peñacoba, C.; Sánchez-Meca, J. Do women with fibromyalgia adhere to walking for exercise programs to improve their health? Systematic review and meta-analysis. Disabil. Rehabil. 2018, 40, 2475–2487. [Google Scholar] [CrossRef]
- Pastor-Mira, M.A.; López-Roig, S.; Peñacoba, C.; Sanz-Baños, Y.; Lledó, A.; Velasco, L. Predicting walking as exercise in women with fibromyalgia from the perspective of the theory of planned behavior. Women Health 2020, 60, 412–425. [Google Scholar] [CrossRef]
- Ang, D.C.; Kaleth, A.S.; Bigatti, S.; Mazzuca, S.A.; Jensen, M.P.; Hilligoss, J.; Slaven, J.; Saha, C. Research to Encourage Exercise for Fibromyalgia (REEF). Clin. J. Pain 2013, 29, 296–304. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.S.; Linton, S.J. Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 2000, 85, 317–332. [Google Scholar] [CrossRef]
- Nijs, J.; Roussel, N.; Van Oosterwijck, J.; De Kooning, M.; Ickmans, K.; Struyf, F.; Meeus, M.; Lundberg, M. Fear of movement and avoidance behaviour toward physical activity in chronic-fatigue syndrome and fibromyalgia: State of the art and implications for clinical practice. Clin. Rheumatol. 2013, 32, 1121–1129. [Google Scholar] [CrossRef]
- Crombez, G.; Eccleston, C.; Van Damme, S.; Vlaeyen, J.W.S.; Karoly, P. Fear-Avoidance Model of Chronic Pain. Clin. J. Pain 2012, 28, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Meulders, A. From fear of movement-related pain and avoidance to chronic pain disability: A state-of-the-art review. Curr. Opin. Behav. Sci. 2019, 26, 130–136. [Google Scholar] [CrossRef]
- Tabor, A.; Van Ryckeghem, D.M.L.; Hasenbring, M.I. Pain Unstuck: The Role of Action and Motivation. Clin. J. Pain 2020, 36, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, S.; Crombez, G.; Eccleston, C. Coping with pain: A motivational perspective. Pain 2008, 139, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Karsdorp, P.A.; Vlaeyen, J.W.S. Goals matter: Both achievement and pain-avoidance goals are associated with pain severity and disability in patients with low back and upper extremity pain. Pain 2011, 152, 1382–1390. [Google Scholar] [CrossRef]
- Karsdorp, P.A.; Nijst, S.E.; Goossens, M.E.J.B.; Vlaeyen, J.W.S. The role of current mood and stop rules on physical task performance: An experimental investigation in patients with work-related upper extremity pain. Eur. J. Pain 2010, 14, 434–440. [Google Scholar] [CrossRef]
- Crombez, G.; De Paepe, A.L.; Veirman, E.; Eccleston, C.; Verleysen, G.; Van Ryckeghem, D.M.L. Let’s talk about pain catastrophizing measures: An item content analysis. PeerJ 2020, 2020, e8643. [Google Scholar] [CrossRef]
- Amtmann, D.; Liljenquist, K.; Bamer, A.; Bocell, F.; Jensen, M.; Wilson, R.; Turk, D. Measuring Pain Catastrophizing and Pain-Related Self-Efficacy: Expert Panels, Focus Groups, and Cognitive Interviews. Patient 2018, 11, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Pastor, M.Á.; López-Roig, S.; Sanz, Y.; Peñacoba, C.; Cigarán, M.; Velasco, L.; Carmen Écija, A.L. Walking as physical exercise in Fibromyalgia: An elicitation study from the Theory of Planned Behavior. An. Psicol. 2015, 31, 433–446. [Google Scholar] [CrossRef]
- Conversano, C.; Laura, M.; Rebecca, C.; Mirabelli, V.; Angelo, G. Catastrophizing and Fibromyalgia: A Mini-Review. J. Transl. Neurosci. 2018, 3, 1–4. [Google Scholar] [CrossRef]
- Galvez-Sánchez, C.M.; Montoro, C.I.; Duschek, S.; del Paso, G.A.R. Pain catastrophizing mediates the negative influence of pain and trait-anxiety on health-related quality of life in fibromyalgia. Qual. Life Res. 2020, 29, 1871–1881. [Google Scholar] [CrossRef]
- Luciano, J.V.; Forero, C.G.; Cerdà-Lafont, M.; Peñarrubia-María, M.T.; Fernández-Vergel, R.; Cuesta-Vargas, A.I.; Ruíz, J.M.; Rozadilla-Sacanell, A.; Sirvent-Alierta, E.; Santo-Panero, P.; et al. Functional Status, Quality of Life, and Costs Associated With Fibromyalgia Subgroups. Clin. J. Pain 2016, 32, 829–840. [Google Scholar] [CrossRef]
- Martinez-Calderon, J.; Jensen, M.P.; Morales-Asencio, J.M.; Luque-Suarez, A. Pain Catastrophizing and Function in Individuals with Chronic Musculoskeletal Pain. Clin. J. Pain 2019, 35, 279–293. [Google Scholar] [CrossRef]
- Rodero, B.; Casanueva, B.; García-Campayo, J.; Roca, M.; Magallán, R.; Lápez Del Hoyo, Y. Stages of chronicity in fibromyalgia and pain catastrophising: A cross-sectional study. BMC Musculoskelet. Disord. 2010, 11, 251. [Google Scholar] [CrossRef]
- Estévez-López, F.; Segura-Jiménez, V.; Álvarez-Gallardo, I.C.; Borges-Cosic, M.; Pulido-Martos, M.; Carbonell-Baeza, A.; Aparicio, V.A.; Geenen, R.; Delgado-Fernández, M. Adaptation profiles comprising objective and subjective measures in fibromyalgia: The al-Ándalus project. Rheumatology 2017, 56, 2015–2024. [Google Scholar] [CrossRef][Green Version]
- Westman, A.E.; Boersma, K.; Leppert, J.; Linton, S.J. Fear-Avoidance Beliefs, Catastrophizing, and Distress. Clin. J. Pain 2011, 27, 567–577. [Google Scholar] [CrossRef]
- Lazaridou, A.; Paschali, M.; Schreiber, K.; Galenkamp, L.; Berry, M.; Paschalis, T.; Napadow, V.; Edwards, R.R. The association between daily physical exercise and pain among women with fibromyalgia: The moderating role of pain catastrophizing. Pain Rep. 2020, 5, 53–55. [Google Scholar] [CrossRef]
- Sullivan, M.; Bishop, S.; Pivik, J. The pain catastrophizing scale: User Manual. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Jensen, M.P.; Turner, L.R.; Turner, J.A.; Romano, J.M. The use of multiple-item scales for pain intensity measurement in chronic pain patients. Pain 1996, 67, 35–40. [Google Scholar] [CrossRef]
- Martín-Aragón, M.; Pastor, M.A.; Rodríguez-Martín, J.; March, M.J.; Lledó, A.; López-Roig, S.; Terol, M.C. Dpto de Psicología de la Salud. Facultad de Medicina. Universidad Miguel Hernández. J. Health Psychol. 1999, 11, 53–75. [Google Scholar]
- Lledó-Boyer, A.; Pastor-Mira, M.A.; Pons-Calatayud, N.; López-Roig, S.; Rodríguez-Marín, J.; Bruehl, S. Control beliefs, coping and emotions: Exploring relationships to explain fibromyalgia health outcomes. Int. J. Clin. Health Psychol. 2010, 10, 459–476. [Google Scholar]
- Pastor-Mira, M.-Á.; López-Roig, S.; Martínez-Zaragoza, F.; Toribio, E.; Nardi-Rodríguez, A.; Peñacoba, C. Motivational Determinants of Objective Physical Activity in Women with Fibromyalgia Who Attended Rehabilitation Settings. J. Clin. Med. 2021, 10, 5547. [Google Scholar] [CrossRef]
- Pastor-Mira, M.-A.; López-Roig, S.; Martínez-Zaragoza, F.; León, E.; Abad, E.; Lledó, A.; Peñacoba, C. Goal Preferences, Affect, Activity Patterns and Health Outcomes in Women with Fibromyalgia. Front. Psychol. 2019, 10, 1–15. [Google Scholar] [CrossRef]
- Salgueiro, M.; García-Leiva, J.M.; Ballesteros, J.; Hidalgo, J.; Molina, R.; Calandre, E.P. Validation of a Spanish version of the Revised Fibromyalgia Impact Questionnaire (FIQR). Health Qual. Life Outcomes 2013, 11, 132. [Google Scholar] [CrossRef]
- IPAQ Group. International Physical Activity Questionnaire Self Administered Short Form (IPAQ-S), Spanish Version. 2011. Available online: https://sites.google.com/site/theipaq/questionnaire_links (accessed on 14 December 2021).
- Rivera, J.; Alegre, C.; Carbonell, J.; Ballina, F.J. Documento de consenso de la Sociedad Española de Reumatología sobre la fibromialgia. Reumatol. Clínica 2006, 2, S55–S66. [Google Scholar] [CrossRef]
- Ratter, J.; Radlinger, L.; Lucas, C. Several submaximal exercise tests are reliable, valid and acceptable in people with chronic pain, fibromyalgia or chronic fatigue: A systematic review. J. Physiother. 2014, 60, 144–150. [Google Scholar] [CrossRef]
- Esteve, R.; Ramírez-Maestre, C.; Peters, M.L.; Serrano-Ibáñez, E.R.; Ruíz-Párraga, G.T.; López-Martínez, A.E. Development and initial validation of the activity patterns scale in patients with chronic pain. J. Pain 2016, 17, 451–461. [Google Scholar] [CrossRef]
- Kindermans, H.P.J.; Roelofs, J.; Goossens, M.E.J.B.; Huijnen, I.P.J.; Verbunt, J.A.; Vlaeyen, J.W.S. Activity patterns in chronic pain: Underlying dimensions and associations with disability and depressed mood. J. Pain 2011, 12, 1049–1058. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Häuser, W.; Katz, R.L.; Mease, P.J.; Russell, A.S.; Russell, I.J.; Walitt, B. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis Rheum. 2016, 46, 319–329. [Google Scholar] [CrossRef] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care 2002, 166, 111–117. [CrossRef] [PubMed]
- Pastor, M.-Á.; López-Roig, S.; Lledó, A.; Peñacoba, C.; Velasco, L.; Schweiger-Gallo, I.; Cigarán, M.; Écija, C.; Limón, R.; Sanz, Y. Combining motivational and volitional strategies to promote unsupervised walking in patients with fibromyalgia: Study protocol for a randomized controlled trial. Trials 2014, 15, 120. [Google Scholar] [CrossRef]
- Sullivan, M.J.L. The Pain Catastrophizing Scale: User Manual; McGill University: Montreal, QC, Canada, 2009. [Google Scholar]
- Lazaridou, A.; Franceschelli, O.; Buliteanu, A.; Cornelius, M.; Edwards, R.R.; Jamison, R.N. Influence of catastrophizing on pain intensity, disability, side effects, and opioid misuse among pain patients in primary care. J. Appl. Biobehav. Res. 2017, 22, 1–13. [Google Scholar] [CrossRef]
- Osman, A.; Barrios, F.X.; Kopper, B.A.; Hauptmann, W.; Jones, J.; O’Neill, E. Factor structure, reliability, and validity of the pain catastrophizing scale. J. Behav. Med. 1997, 20, 589–605. [Google Scholar] [CrossRef] [PubMed]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression, 2nd ed.; Wiley & Sons: New York, NY, USA, 2000. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; The Guildford Press: New York, NY, USA, 2018. [Google Scholar]
- Sosa-Reina, M.D.; Nunez-Nagy, S.; Gallego-Izquierdo, T.; Pecos-Martín, D.; Monserrat, J.; Álvarez-Mon, M. Effectiveness of Therapeutic Exercise in Fibromyalgia Syndrome: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Biomed. Res. Int. 2017, 2017. [Google Scholar] [CrossRef]
- Bidonde, J.; Busch, A.J.; Schachter, C.L.; Overend, T.J.; Kim, S.Y.; Góes, S.M.; Boden, C.; Foulds, H.J. Aerobic exercise training for adults with fibromyalgia. Cochrane Database Syst. Rev. 2017. [Google Scholar] [CrossRef]
- Aldrich, S.; Eccleston, C.; Crombez, G. Worrying about chronic pain: Vigilance to threat and misdirected problem solving. Behav. Res. Ther. 2000, 38, 457–470. [Google Scholar] [CrossRef]
- De Vlieger, P.; Van den Bussche, E.; Eccleston, C.; Crombez, G. Finding a solution to the problem of pain: Conceptual formulation and the development of the Pain Solutions Questionnaire (PaSol). Pain 2006, 123, 285–293. [Google Scholar] [CrossRef]
- Gatchel, R.J. Introduction to the “Special Issue on Pain Catastrophizing”. J. Appl. Biobehav. Res. 2017, 22, 1–5. [Google Scholar] [CrossRef]
- Velasco, L.; López-Gómez, I.; Gutiérrez, L.; Écija, C.; Catalá, P.; Peñacoba, C. Exploring the Preference for Fatigue-avoidance Goals as a Mediator Between Pain Catastrophizing, Functional Impairment and Walking Behavior in Women with Fibromyalgia. Clin. J. Pain 2021. [Google Scholar] [CrossRef] [PubMed]
- De Gier, M.; Peters, M.L.; Vlaeyen, J.W.S. Fear of pain, physical performance, and attentional processes in patients with fibromyalgia. Pain 2003, 104, 121–130. [Google Scholar] [CrossRef]
- Estévez-López, F.; Rodriguez-Ayllon, M.; Soriano-Maldonado, A.; Acosta-Manzano, P.; Segura-Jiménez, V.; Álvarez-Gallardo, I.C.; Pulido-Martos, M.; Herrador-Colmenero, M.; Geenen, R.; Carbonell-Baeza, A.; et al. Lower Fatigue in Fit and Positive Women with Fibromyalgia: The al-Ándalus Project. Pain Med. 2019, 20, 2506–2515. [Google Scholar] [CrossRef] [PubMed]
- Mannerkorpi, K.; Svantesson, U.; Broberg, C. Relationships between performance-based tests and patients’ ratings of activity limitations, self-efficacy, and pain in fibromyalgia. Arch. Phys. Med. Rehabil. 2006, 87, 259–264. [Google Scholar] [CrossRef] [PubMed]

| Entire Sample | Low Pain-Related Worrying | High Pain-Related Worrying | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Mean | (SD) | [95% CI] | n (%) | Mean | (SD) | [95% CI] | n (%) | Mean | (SD) | [95% CI] | t | |
| Pain-related worrying | 111 (100) | 30.9 | (12.3) | [28.6–33.2] | 55 (49.5) | 20.7 | (7.8) | [18.6–22.8] | 56(50.5) | 40.9 | (6.2) | [39.2–42.5] | |
| Age (years) | 51.4 | (9.7) | [49.6–53.2] | ns | |||||||||
| Time from symptoms | 14.1 | (9.8) | [12.1–16.0] | ns | |||||||||
| Time from diagnosis | 6.2 | (6.2) | [5.0–7.4] | ns | |||||||||
| Fatigue intensity b. t.a | 7.3 | (2.2) | [6.9–7.7] | ns | |||||||||
| Pain intensity b. t.a | 6.5 | (2.2) | [6.1–6.9] | 5.7 | (2.1) | [5.2–6.3] | 7.3 | (2.1) | [6.8–7.9] | −4.16 *** | |||
| Pain intensity | 6.8 | (1.7) | [6.5–7.1] | 6.1 | (1.6) | [5.7–6.5] | 7.4 | (1.5) | [7.0–7.8] | −4.68 *** | |||
| Fibromyalgia impact | 72.3 | (15.8) | [69.3–75.2] | 66.0 | (17.2) | [61.4–70.2] | 78.4 | (11.6) | [75.3–81.5] | −4.44 *** | |||
| Goal preferences | 4.4 | (1.3) | [4.2–4.7] | 4.1 | (1.4) | [3.8–4.5] | 4.7 | (1.2) | [4.4–5.1] | −2.44 * | |||
| Total MET-min/week b | 694 | (1635) | [439–873] | 856 | (1701) | [509–1506] | 384 | (879) | [231–693] | 4.76 * c | |||
| Number of laps | 14.3 | (10.6) | [12.3–16.3] | 16.4 | (11.7) | [13.2–19.6] | 12.3 | (9.1) | [9.8–14.7] | 2.07 * | |||
| Walking distance d: | |||||||||||||
| Total | 886 | (637) | [766–1006] | 1010 | (702) | [820–1200] | 765 | (546) | [619–911] | 2.05 * | |||
| Bout 1 | 111 (100) | 396 | (85) | [380–412] | 55 (49.5) | 420 | (77) | [399–441] | 56(50.5) | 372 | (86) | [349–395] | 3.14 ** |
| Bout 2 | 65 (58.6) | 396 | (91) | [374–419] | 34 (61.8) | 423 | (80) | [396–452] | 31(55.4) | 366 | (95) | [332–401] | 2.65 ** |
| Bout 3 | 35 (31.5) | 412 | (86) | [383–442] | 19 (54.3) | 16(45.7) | ns | ||||||
| Bout 4 | 20 (18.0) | 425 | (86) | [384–465] | 13 (65.0) | 7 (35.0) | ns | ||||||
| Bout 5 | 13 (11.7) | 443 | (107) | [379–508] | 9 (69.2) | 4 (30.8) | ns | ||||||
| Stop vs. Walking | ||||||
|---|---|---|---|---|---|---|
| Model a | n b | OR | [95% CI] | p | χ2 c | Cp |
| 1st bout | 111/46 | |||||
| Goals preference | 1.443 | [1.026–2.030] | 0.027 | 13.467 ** | 3.28 | |
| Fibromyalgia impact | 1.029 | [1.000–1.060] | 0.037 | |||
| Educational level | 2.428 | [1.055–5.589] | 0.033 | |||
| 2nd bout | 65/30 | |||||
| Goals preference | 1.621 | [1.166–2.255] | 0.003 | 11.295 ** | 4.04 | |
| Educational level | 2.300 | [0.957–5.530] | 0.058 | |||
| 3rd bout | 35/10 | |||||
| Goals preference | 1.540 | [1.073–2.210] | 0.018 | 5.617 * | 1.78 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pastor-Mira, M.Á.; López-Roig, S.; Toribio, E.; Martínez-Zaragoza, F.; Nardi-Rodríguez, A.; Peñacoba, C. Pain-Related Worrying and Goal Preferences Determine Walking Persistence in Women with Fibromyalgia. Int. J. Environ. Res. Public Health 2022, 19, 1513. https://doi.org/10.3390/ijerph19031513
Pastor-Mira MÁ, López-Roig S, Toribio E, Martínez-Zaragoza F, Nardi-Rodríguez A, Peñacoba C. Pain-Related Worrying and Goal Preferences Determine Walking Persistence in Women with Fibromyalgia. International Journal of Environmental Research and Public Health. 2022; 19(3):1513. https://doi.org/10.3390/ijerph19031513
Chicago/Turabian StylePastor-Mira, María Ángeles, Sofía López-Roig, Eva Toribio, Fermín Martínez-Zaragoza, Ainara Nardi-Rodríguez, and Cecilia Peñacoba. 2022. "Pain-Related Worrying and Goal Preferences Determine Walking Persistence in Women with Fibromyalgia" International Journal of Environmental Research and Public Health 19, no. 3: 1513. https://doi.org/10.3390/ijerph19031513
APA StylePastor-Mira, M. Á., López-Roig, S., Toribio, E., Martínez-Zaragoza, F., Nardi-Rodríguez, A., & Peñacoba, C. (2022). Pain-Related Worrying and Goal Preferences Determine Walking Persistence in Women with Fibromyalgia. International Journal of Environmental Research and Public Health, 19(3), 1513. https://doi.org/10.3390/ijerph19031513







