Influence of Self-Efficacy on Cancer-Related Fatigue and Health-Related Quality of Life in Young Survivors of Childhood Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Questionnaire Survey
2.3. Statistics
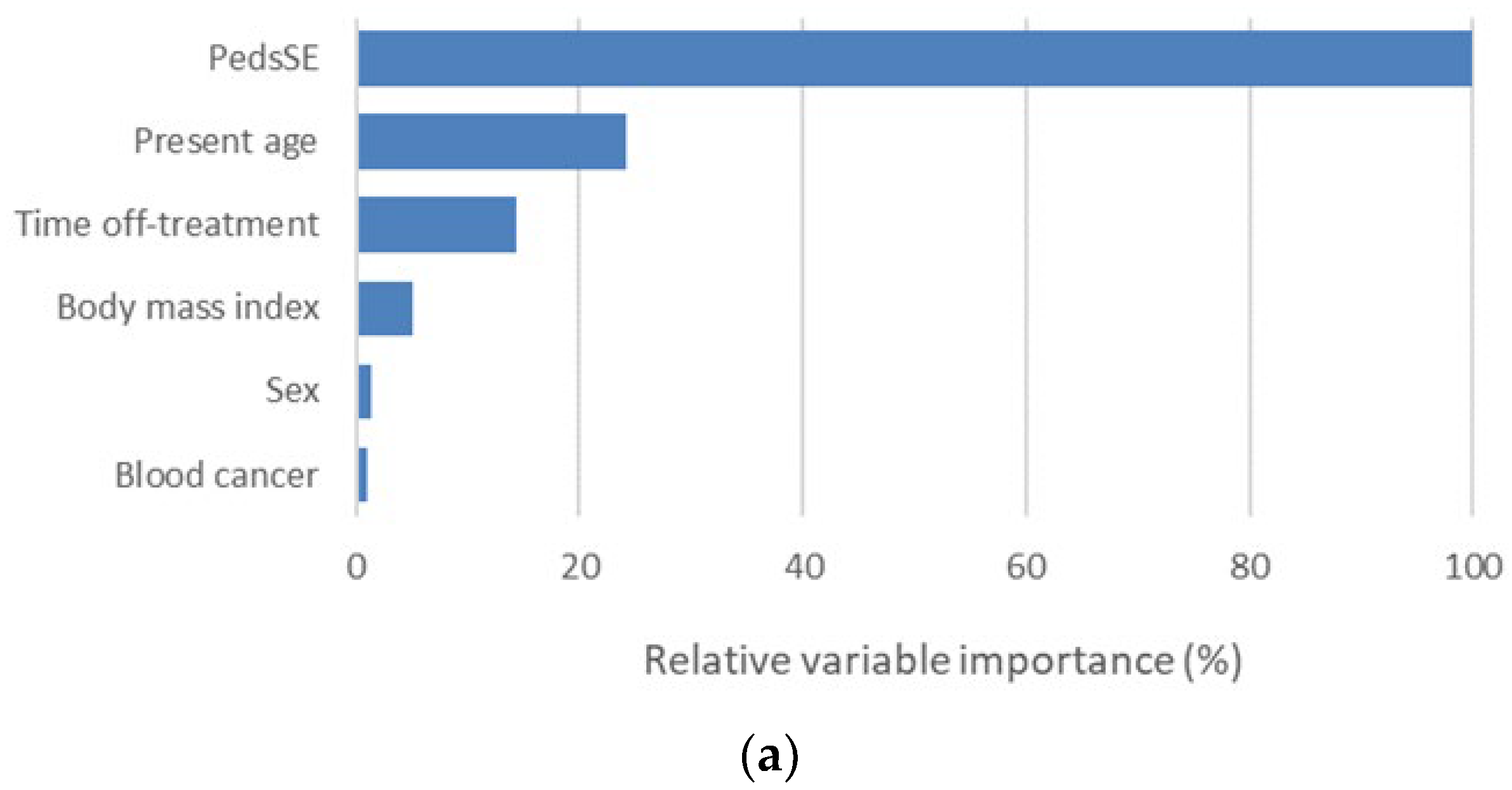
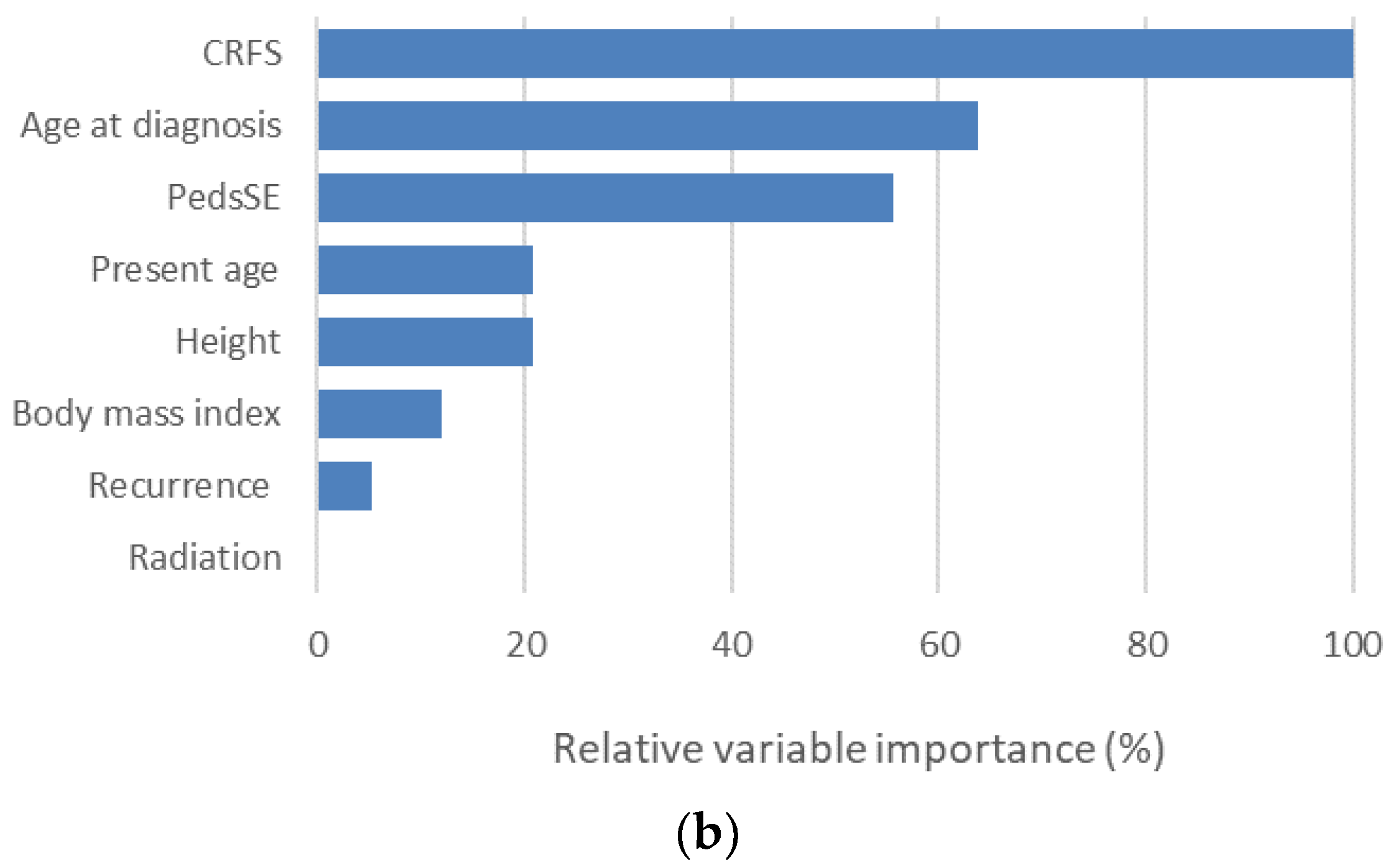
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Phillips, S.M.; Padgett, L.S.; Leisenring, W.M.; Stratton, K.K.; Bishop, K.; Krull, K.R.; Alfano, C.M.; Gibson, T.M.; de Moor, J.S.; Hartigan, D.B.; et al. Survivors of childhood cancer in the United States. Prevalence and burden of morbidity. Cancer Epidemiol. Biomark. Prev. 2015, 4, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Trama, A.; Botta, L.; Foschi, R.; Ferrari, A.; Stiller, C.; Desandes, E.; Maule, M.M.; Merletti, F.; Gatta, G.; EUROCARE-5 Working Group. Survival of European adolescents and young adults diagnosed with cancer in 2000-07: Population-based data from EUROCARE-5. Lancet Oncol. 2016, 17, 896–906. [Google Scholar] [CrossRef]
- Nakata, K.; Ito, Y.; Magadi, W.; Bonaventure, A.; Stiller, C.A.; Katanoda, K.; Matsuda, T.; Miyashiro, I.; Pritchard-Jones, K.; Rachet, B. Chilhood cancer incidence and survival in Japan and England: A population-based study (1993–2010). Cancer Sci. 2018, 109, 422–434. [Google Scholar] [CrossRef] [PubMed]
- Michel, G.; Brinkman, T.M.; Wakefield, C.E.; Grootenhuis, M. Psychological Outcomes, Health-Related Quality of Life, and Nerocognitive Functioning in Survivors of Childhood Cancer and Their Parents. Pediatr. Clin. N. Am. 2020, 67, 1103–1134. [Google Scholar] [CrossRef] [PubMed]
- Park, M.; Park, H.J.; Lee, J.M.; Ju, H.Y.; Park, B.K.; Yu, E.S.; Yang, H.K.; Kim, J.Y.; Park, S.K.; Lee, Y.H.; et al. School performance of childhood cancer survivors in Korea: A multi-institutional study on behalf of the Korean Society of Pediatric Hematology and Oncology. Psychooncology 2018, 27, 2257–2264. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Mo, L.; Huang, X.; Yu, L.; Liu, Y. The effects of self-efficacy and social support on behavior problems in 8~18 years old children with malignant tumors. PLoS ONE 2020, 15, e0236648. [Google Scholar] [CrossRef]
- Sedmak, M.; Bogdanić, A.; Grubić, M. Correlates of Quality of Life in Pediatric Cancer Survivors. Psychiatr. Danub. 2020, 32, 533–539. [Google Scholar]
- Testa, M.A.; Simonson, D.C. Assessment of quality-of-life outcomes. N. Engl. J. Med. 1996, 334, 835–840. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman and Company: New York, NY, USA, 1997. [Google Scholar]
- Heckman, J.E.; Chamie, K.; Maliski, S.L.; Fink, A.; Kwan, L.; Connor, S.E.; Litwin, M.S. The role of self-efficacy in quality of life for disadvantaged men with prostate cancer. J. Urol. 2011, 186, 1855–1861. [Google Scholar] [CrossRef]
- McCarroll, M.L.; Armbruster, S.; Frasure, H.E.; Gothard, M.D.; Gil, K.M.; Kavanagh, M.B.; Waggoner, S.; von Gruenigen, V.E. Self-efficacy, quality of life, and weight loss in overweight/obese endometrial cancer survivors (SUCCEED): A randomized controlled trial. Gynecol. Oncol. 2014, 132, 397–402. [Google Scholar] [CrossRef]
- Chirico, A.; Lucidi, F.; Merluzzi, T.; Alivernini, F.; Laurentiis, M.; Botti, G.; Giordano, A. A meta-analytic review of the relationship of cancer coping self-efficacy with distress and quality of life. Oncotarget 2017, 8, 36800–36811. [Google Scholar] [CrossRef]
- Moreno, P.I.; Ramirez, A.G.; San Miguel-Majors, S.L.; Fox, R.S.; Castillo, L.; Gallion, K.J.; Munoz, E.; Estabrook, R.; Perez, A.; Lad, T.; et al. Satisfaction with cancer care, self-efficacy, and health-related quality of life in Latino cancer survivors. Cancer 2018, 124, 1770–1779. [Google Scholar] [CrossRef]
- Kwak, Y.; Kim, Y.; Choi, E.S.; Im, H.J. Self-efficacy, post-traumatic growth, and quality of life of pediatric cancer survivors: A cross-sectional study. Eur. J. Oncol. Nurs. 2021, 54, 102019. [Google Scholar] [CrossRef]
- Servaes, P.; Verhagen, C.; Bleijenberg, G. Fatigue in cancer patients during and after treatment: Prevalence, correlates and in-terventions. Eur. J. Cancer 2002, 38, 27–43. [Google Scholar] [CrossRef]
- Mitchell, S.A. Cancer-related fatigue: State of the science. PM&R 2010, 2, 364–383. [Google Scholar] [CrossRef]
- Nunes, M.D.R.; Jacob, E.; Bomfim, E.O.; Lopes-Junior, L.C.; de Lima, R.A.G.; Floria-Santos, M.; Nascimento, L.C. Fatigue and health related quality of life in children and adolescents with cancer. Eur. J. Oncol. Nurs. 2017, 29, 39–46. [Google Scholar] [CrossRef]
- Karimi, M.; Cox, A.D.; White, S.V.; Karlson, C.W. Fatigue, Physical and Functional Mobility, and Obesity in Pediatric Cancer Survivors. Cancer Nurs. 2020, 43, E239–E245. [Google Scholar] [CrossRef]
- Gupta, D.; Lis, C.G.; Grutsch, J.F. The relationship between cancer-related fatigue and patient satisfaction with quality of life in cancer. J. Pain Symptom Manag. 2007, 34, 40–47. [Google Scholar] [CrossRef]
- Akin, S.; Kas Guner, C. Investigation of the relationship among fatigue, self-efficacy and quality of life during chemotherapy in patients with breast, lung or gastrointestinal cancer. Eur. J. Cancer Care 2019, 28, e12898. [Google Scholar] [CrossRef]
- Choi, K.W.; Stein, M.B.; Dunn, E.C.; Koenen, K.C.; Smoller, J.W. Genomics and psychological resilience: A research agenda. Mol. Psychiatry 2019, 24, 1770–1778. [Google Scholar] [CrossRef]
- Zhang, H.; Zhao, Q.; Cao, P.; Ren, G. Resilience and Quality of Life: Exploring the Mediator Role of Social Support in Patients with Breast Cancer. Med. Sci. Monit. 2017, 23, 5969–5979. [Google Scholar] [CrossRef]
- Huang, Y.; Huang, Y.; Bao, M.; Zheng, S.; Du, T.; Wu, K. Psychological resilience of women after breast cancer surgery: A cross-sectional study of associated influencing factors. Psychol. Health Med. 2019, 24, 866–878. [Google Scholar] [CrossRef]
- Chen, S.; Mei, R.; Tan, C.; Li, X.; Zhong, C.; Ye, M. Psychological resilience and related influencing factors in postoperative non-small cell lung cancer patients: A cross-sectional study. Psychooncology 2020, 29, 1815–1822. [Google Scholar] [CrossRef]
- Öcalan, S.; Üzar-Özçetin, Y.S. The relationship between rumination, fatigue and psychological resilience among cancer survivors. J. Clin. Nurs. 2021. online ahead of print. [Google Scholar] [CrossRef]
- Hoffman, A.J.; von Eye, A.; Gift, A.G.; Given, B.A.; Given, C.W.; Rothert, M. Testing a theoretical model of perceived self-efficacy for cancer-related fatigue self-management and optimal physical functional status. Nurs. Res. 2009, 58, 32–41. [Google Scholar] [CrossRef]
- Haas, B.K. Fatigue, self-efficacy, physical activity, and quality of life in women with breast cancer. Cancer Nurs. 2011, 34, 322–334. [Google Scholar] [CrossRef]
- Buffart, L.M.; Ros, W.J.; Chinapaw, M.J.; Brug, J.; Knol, D.L.; Korstjens, I.; van Weert, E.; Mesters, I.; van den Borne, B.; Hoekstra-Weebers, J.E.; et al. Mediators of physical exercise for improvement in cancer survivors’ quality of life. Psychooncology 2014, 23, 330–338. [Google Scholar] [CrossRef]
- Phillips, S.M.; McAuley, E. Physical activity and quality of life in breast cancer survivors: The role of self-efficacy and health status. Psychooncology 2014, 23, 27–34. [Google Scholar] [CrossRef]
- Chen, H.L.; Liu, K.; You, Q.S. Self-efficacy, cancer-related fatigue, and quality of life in patients with resected lung cancer. Eur. J. Cancer Care 2018, 27, e12934. [Google Scholar] [CrossRef]
- Braam, K.I.; van der Torre, P.; Takken, T.; Veening, M.A.; van Dulmen-den Broeder, E.; Kaspers, G.J. Physical exercise training in-terventions for children and young adults during and after treatment for childhood cancer. Cochrane Database Syst. Rev. 2016, 3, CD008796. [Google Scholar] [CrossRef]
- Oka, T.; Ishikawa, S.I.; Saito, A.; Maruo, K.; Stickley, A.; Watanabe, N.; Sasamori, H.; Shioiri, T.; Kamio, Y. Changes in self-efficacy in Japanese school-age children with and without high autistic traits after the Universal Unified Prevention Program: A sin-gle-group pilot study. Child Adolesc. Psychiatry Ment. Health 2021, 15, 42. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Jerusalem, M. Generalized Self-Efficacy scale. In Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs; Weinman, J., Wright, S., Johnston, M., Eds.; NFER-NELSON: Windsor, UK, 1995; pp. 35–37. [Google Scholar]
- Scholz, U.; Benicio, G.D.; Sud, S.; Schwarzer, R. Is General Self-Efficacy a Universal Construct? Psychometric Findings from 25 Countries. Eur. J. Psychol. Assess. 2002, 18, 242–251. Available online: http://userpage.fu-berlin.de/~health/self/gse-25countries_2002.pdf (accessed on 16 December 2021). [CrossRef]
- Nagai, A.; Zou, N.; Kubota, M.; Kojima, C.; Adachi, S.; Usami, I.; Okada, M.; Tanizawa, A.; Hamahata, K.; Matsubara, K.; et al. Fatigue in survivors of childhood acute lymphoblastic and myeloid leukemia in Japan. Pediatr. Int. 2012, 54, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Seid, M.; Rode, C.A. The PedsQL: Measurement Model for the Pediatric Quality of Life Inventory. Med. Care 1999, 37, 126–139. [Google Scholar] [CrossRef]
- Kobayashi, K.; Kamibeppu, K. Measuring quality of life in Japanese children: Development of the Japanese version of PedsQL. Pediatr. Int. 2010, 52, 80–88. [Google Scholar] [CrossRef]
- Zeltzer, L.K.; Recklitis, C.; Buchbinder, D.; Zebrack, B.; Casillas, J.; Tsao, J.C.; Lu, Q.; Krull, K. Psychological status in childhood cancer survivors: A report from the Childhood Cancer Survivor Study. J. Clin. Oncol. 2009, 27, 2396–2404. [Google Scholar] [CrossRef]
- Cantrell, M.A. A narrative review summarizing the state of the evidence on the health-related quality of life among childhood cancer survivors. J. Pediatr. Oncol. Nurs. 2010, 28, 75–82. [Google Scholar] [CrossRef]
- Nayiager, T.; Anderson, L.; Cranston, A.; Athale, U.; Barr, R.D. Health-related quality of life in long-term survivors of acute lymphoblastic leukemia in childhood and adolescence. Qual. Life Res. 2017, 26, 1371–1377. [Google Scholar] [CrossRef]
- Shin, H.; Bartlett, R.; De Gagne, J.C. Health-Related Quality of Life among Survivors of Cancer in Adolescence: An Integrative Literature Review. J. Pediatr. Nurs. 2019, 44, 97–106. [Google Scholar] [CrossRef]
- Iannotti, R.J.; Schneider, S.; Nansel, T.R.; Haynie, D.L.; Plotnick, L.P.; Clark, L.M.; Sobel, D.O.; Simons-Morton, B. Self-efficacy, outcome expectations, and diabetes self-management in adolescents with type 1 diabetes. J. Dev. Behav. Pediatr. 2006, 27, 98–105. [Google Scholar] [CrossRef]
- Carissimi, A.; Adan, A.; Tonetti, L.; Fabbri, M.; Hidalgo, M.P.; Levandovski, R.; Natale, V.; Martoni, M. Physical self-efficacy is asso-ciated to body mass index in schoolchildren. J. Pediatr. 2017, 93, 64–69. [Google Scholar] [CrossRef][Green Version]
- Arekapudi, K.L.; Noris, C.; Updegrove, S. Improving Self-Efficacy of Student Asthma Management in Elementary and Preschool Staff. J. Sch. Nurs. 2021, 37, 513–522. [Google Scholar] [CrossRef]
- Santucci, N.R.; Rein, L.E.; van Tilburg, M.A.; Karpinski, A.; Rosenberg, A.; Amado-Feeley, A.; Stoops, E.; Herdes, R.E.; Hyman, P.E. Self-Efficacy in Children with Functional Constipation Is Associated with Treatment Success. J. Pediatr. 2020, 216, 19–24. [Google Scholar] [CrossRef]
- Brown, J.C.; Huedo-Medina, T.B.; Pescatello, L.S.; Pescatello, S.M.; Ferrer, R.A.; Johnson, B.T. Efficacy of Exercise Interventions in Modulating Cancer-Related Fatigue among Adult Cancer Survivors: A Meta-Analysis. Cancer Epidemiol. Biomark. Prev. 2011, 20, 123–133. [Google Scholar] [CrossRef]
- Medysky, M.E.; Temesia, J.; Culos-Reed, S.N.; Mille, G.Y. Exercise, sleep and cancer-related fatigue: Are they related? Neurophysiol. Clin. 2017, 47, 111–122. [Google Scholar] [CrossRef]
- Hoffman, A.J.; Brintnall, R.A.; Given, B.A.; von Eye, A.; Jones, L.W.; Brown, B.K. Using Perceived Self-Efficacy to Improve Fatigue and Fatigability in Post-Surgical Lung Cancer Patients: A Pilot Randomized Controlled Trial. Cancer Nurs. 2017, 40, 1. [Google Scholar] [CrossRef]
- Zhu, X.; Han, S.; Chu, H.; Wang, M.; Chen, S. Influence of self-management exercise intervention on the cancer related fatigue severity and self-management efficacy of patients with non-small cell lung cancer after operation. J. Pak. Med. Assoc. 2020, 70, 88–93. [Google Scholar]
- Van Dijk-Lokkart, E.M.; Steur, L.M.H.; Braam, K.I.; Veening, M.A.; Huisman, J.; Takken, T.; Bierings, M.; Merks, J.H.; Van den Heuvel-Eibrink, M.M.; Kaspers, G.J.L.; et al. Longitudinal development of cancer-related fatigue and physical activity in childhood cancer patients. Pediatr. Blood Cancer 2019, 66, e27949. [Google Scholar] [CrossRef]
- Mustian, K.M.; Alfano, C.M.; Heckler, C.; Kleckner, A.S.; Kleckner, I.R.; Leach, C.R.; Mohr, D.; Palesh, O.G.; Peppone, L.J.; Piper, B.F.; et al. Comparison of Pharmaceutical, Psychological, and Exercise Treatments for Cancer-Related Fatigue: A Meta-analysis. JAMA Oncol. 2017, 3, 961–968. [Google Scholar] [CrossRef]
| Distribution | Range | |
|---|---|---|
| Demographic characteristics | ||
| Age (years) | 13.3 ± 3.1 | 8–18 |
| Sex (male) | 26 (56.5) | - |
| Height (±standard deviation) | −0.09 ± 1.20 | −3.50–3.10 |
| Body mass index (kg/m2) | 18.2 ±3.0 | 14.6–27.3 |
| Clinical characteristics | ||
| Age at diagnosis (years) | 4.1 ± 4.4 | 0–14 |
| Duration of hospital stay (months) | 86.8 ± 12.8 | 1–52 |
| Time off-treatment (months) | 101 ± 50 | 12–206 |
| Diagnosis | ||
| Blood cancer | 33 (71.7) | - |
| Solid cancers | 13 (28.3) | - |
| Treatment | ||
| Chemotherapy | 46 (100) | - |
| Surgery | 10 (21.7) | - |
| Radiation | 9 (20.0) | - |
| Stem cell transplantation | 3 (6.5) | - |
| Recurrence of cancer | 5 (10.9) | - |
| Distribution | Range | |
|---|---|---|
| General Self-Efficacy Scale | ||
| General Self-Efficacy Scale for Children—Revised | 53.1 ± 9.4 | 38–70 |
| (For survivors of 8–12 years old, n = 18) | ||
| General Self-Efficacy Scale | 28.2 ± 5.1 | 20–37 |
| (For survivors of 13–18 years old, n = 28) | ||
| Pediatric General Self-Efficacy Scale (PedsSE) | 50.0 ± 9.9 | 33.9–67.9 |
| (For all survivors, n = 46) | ||
| Cancer-related Fatigue Score (CRFS) | ||
| Total score | 10.9 ± 6.5 | 0–25 |
| Physical fatigue | 3.8 ± 2.8 | 0–9 |
| Decreased function | 4.7 ± 2.5 | 1–9 |
| Altered mood | 2.5 ± 2.4 | 0–10 |
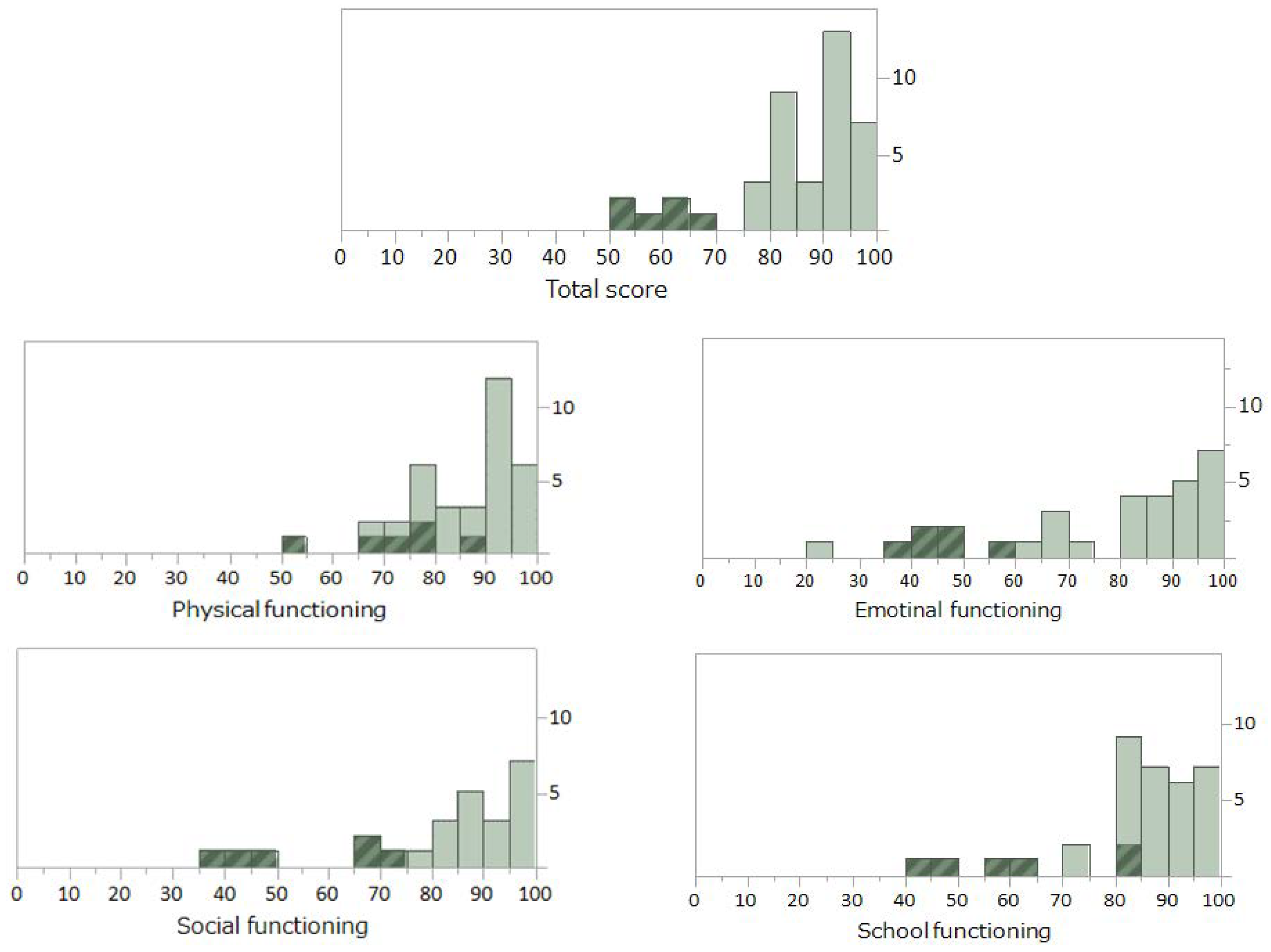
| Pediatric Quality of Life Inventory (PedsQL) | ||
| Total score | 86.8 ± 12.8 | 54.3–100 |
| Physical functioning | 89.3 ± 11.2 | 53.1–100 |
| Emotional functioning | 82.3 ± 21.4 | 20–100 |
| Social functioning | 89.1 ± 16.4 | 35–100 |
| School functioning | 86.1 ± 14.2 | 40–100 |
| CRFS | |||
|---|---|---|---|
| Physical Fatigue | Decreased Function | Altered Mood | |
| PedsSE | −0.384 | −0.523 | −0.47 |
| PedsQL | |||
| Total score | −0.587 | −0.484 | −0.737 |
| Physical functioning | −0.569 | −0.391 | −0.665 |
| Emotional functioning | −0.436 | −0.411 | −0.659 |
| Social functioning | −0.383 | −0.309 | −0.381 |
| School functioning | −0.441 | −0.437 | −0.675 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saito, M.; Hiramoto, I.; Yano, M.; Watanabe, A.; Kodama, H. Influence of Self-Efficacy on Cancer-Related Fatigue and Health-Related Quality of Life in Young Survivors of Childhood Cancer. Int. J. Environ. Res. Public Health 2022, 19, 1467. https://doi.org/10.3390/ijerph19031467
Saito M, Hiramoto I, Yano M, Watanabe A, Kodama H. Influence of Self-Efficacy on Cancer-Related Fatigue and Health-Related Quality of Life in Young Survivors of Childhood Cancer. International Journal of Environmental Research and Public Health. 2022; 19(3):1467. https://doi.org/10.3390/ijerph19031467
Chicago/Turabian StyleSaito, Masayo, Izumi Hiramoto, Michihiro Yano, Arata Watanabe, and Hideya Kodama. 2022. "Influence of Self-Efficacy on Cancer-Related Fatigue and Health-Related Quality of Life in Young Survivors of Childhood Cancer" International Journal of Environmental Research and Public Health 19, no. 3: 1467. https://doi.org/10.3390/ijerph19031467
APA StyleSaito, M., Hiramoto, I., Yano, M., Watanabe, A., & Kodama, H. (2022). Influence of Self-Efficacy on Cancer-Related Fatigue and Health-Related Quality of Life in Young Survivors of Childhood Cancer. International Journal of Environmental Research and Public Health, 19(3), 1467. https://doi.org/10.3390/ijerph19031467







