Factors Associated with Urinary 1-Hydroxypyrene and Malondialdehyde among Adults near a Petrochemical Factory: Implications for Sex and Lifestyle Modification
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Procedure and Ethical Approval
2.3. Measurements
2.4. Statistical Analyses
3. Results
3.1. Participant Demographic Characteristics
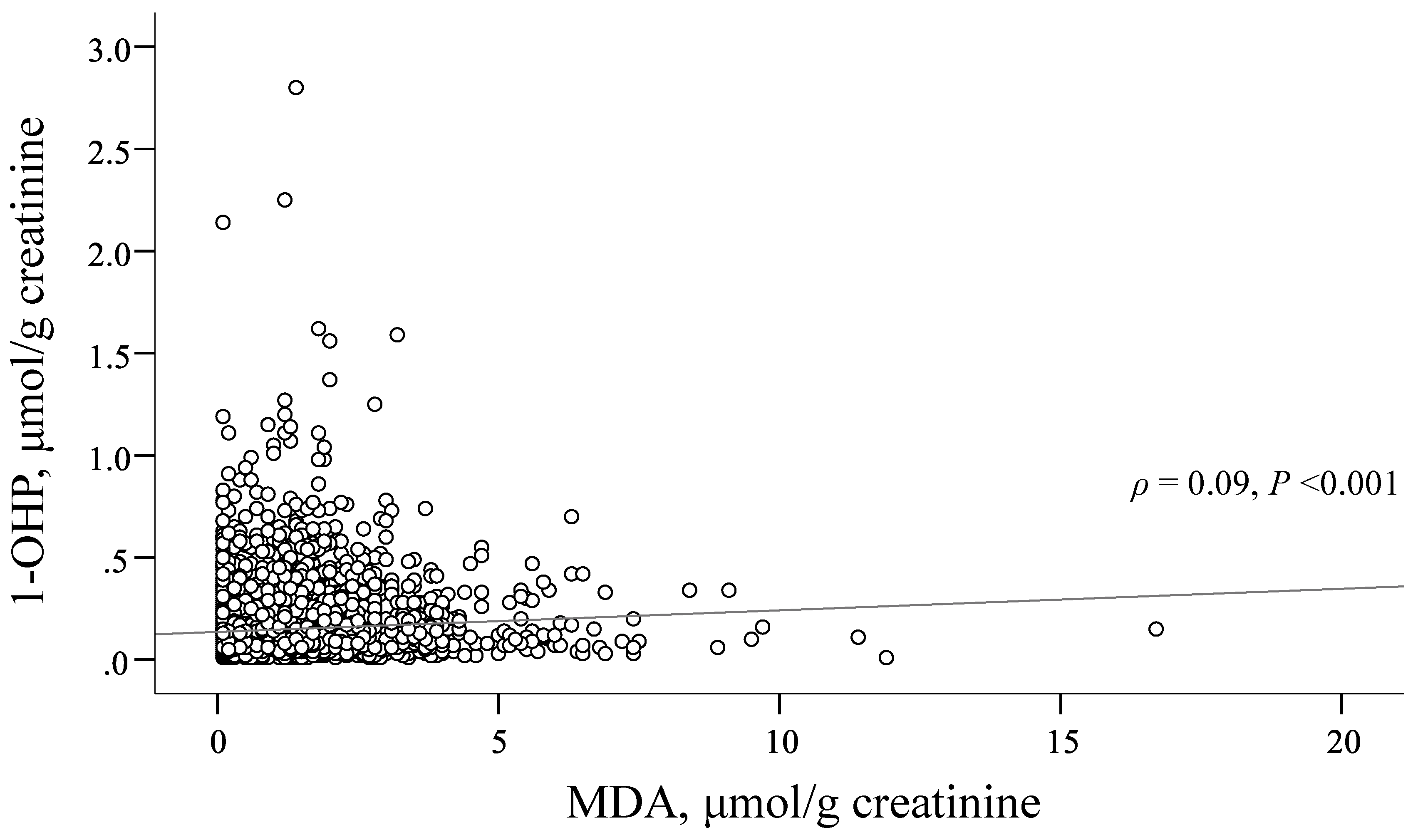
3.2. Factors Associated with 1-OHP Level
3.3. Factors Associated with MDA Level
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Chang, W.W.; Boonhat, H.; Lin, R.T. Incidence of respiratory symptoms for residents living near a petrochemical industrial complex: A meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 2474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Domingo, J.L.; Marquès, M.; Nadal, M.; Schuhmacher, M. Health risks for the population living near petrochemical industrial complexes. Cancer risks: A review of the scientific literature. Environ. Res. 2020, 186, 109495. [Google Scholar] [CrossRef] [PubMed]
- Yuan, T.H.; Ke, D.Y.; Wang, J.E.; Chan, C.C. Associations between renal functions and exposure of arsenic and polycyclic aromatic hydrocarbon in adults living near a petrochemical complex. Environ. Pollut. 2020, 256, 113457. [Google Scholar] [CrossRef] [PubMed]
- Environmental Protection Administration, EPA. Environmental White Paper-2020. Available online: https://www.epa.gov.tw/Page/3CFBDA8551D7D8E5 (accessed on 15 August 2021).
- Chan, C.C.; Lin, L.Y.; Lai, C.H.; Chuang, K.J.; Wu, M.T.; Pan, C.H. Association of particulate matter from cooking oil fumes with heart rate variability and oxidative stress. Antioxidants 2021, 10, 1323. [Google Scholar] [CrossRef]
- Lin, C.K.; Hung, H.Y.; Christiani, D.C.; Forastiere, F.; Lin, R.T. Lung cancer mortality of residents living near petrochemical industrial complexes: A meta-analysis. Environ. Health 2017, 16, 101. [Google Scholar] [CrossRef] [Green Version]
- Patel, A.P.; Mehta, S.S.; White, A.J.; Niehoff, N.M.; Arroyave, W.D.; Wang, A. Urinary polycyclic aromatic hydrocarbon metabolites and mortality in the United States: A prospective analysis. PLoS ONE 2021, 16, e0252719. [Google Scholar] [CrossRef]
- Tombolini, F.; Pigini, D.; Tranfo, G.; Paci, E.; Carosi, I.; Marini, F. Levels of urinary metabolites of four PAHs and cotinine determined in 1016 volunteers living in central Italy. Environ. Sci. Pollut. Res. Int. 2018, 25, 28772–28779. [Google Scholar] [CrossRef]
- Fedeli, U.; Girardi, P.; Mastrangelo, G. Occupational exposure to viny chloride and liver diseases. World J. Gastroenterol. 2019, 25, 4885–4891. [Google Scholar] [CrossRef]
- Jephcote, C.; Brown, D.; Verbeek, T.; Mah, A. A systematic review and meta-analysis of haematological malignancies in residents living near petrochemical facilities. Environ. Health 2020, 19, 53. [Google Scholar] [CrossRef]
- Keir, J.L.A.; Cakmak, S.; Blais, J.M.; White, P.A. The influence of demographic and lifestyle factors on urinary levels of PAH metabolites-empirical analyses of cycle 2 (2009–2011) CHMS data. J. Expo. Sci. Environ. Epidemiol. 2021, 31, 386–397. [Google Scholar] [CrossRef] [Green Version]
- Hoseini, M.; Nabizadeh, R.; Delgado-Saborit, J.M.; Rafiee, A.; Yaghmaeian, K.; Parmy, S. Environmental and lifestyle factors affecting exposure to polycyclic aromatic hydrocarbons in the general population in a Middle Eastern area. Environ. Pollut. 2018, 240, 781–792. [Google Scholar] [CrossRef] [PubMed]
- Jain, R.B. Contributions of dietary, demographic, disease, lifestyle and other factors in explaining variabilities in concentrations of selected monohydroxylated polycyclic aromatic hydrocarbons in urine: Data for US children, adolescents, and adults. Environ. Pollut. 2020, 266, 115178. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Kamal, R.; Ahamed, I.; Wagh, M.; Bihari, V.; Sathian, B. PAH exposure-associated lung cancer: An updated meta-analysis. Occup. Med. 2018, 68, 255–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Senerat, A.M.; Manemann, S.M.; Clements, N.S.; Brook, R.D.; Hassett, L.C.; Roger, V.L. Biomarkers and indoor air quality: A translational research review. J. Clin. Transl. Sci. 2020, 5, e39. [Google Scholar] [CrossRef] [PubMed]
- Barrera, G.S.; Pizzimenti, M.; Daga, C.; Dianzani, A.; Arcaro, G.P.; Cetrangolo, G. Lipid peroxidation-derived aldehydes, 4-hydroxynonenal and malondialdehyde in aging-related disorders. Antioxidants 2018, 7, 102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, H.; Martinez-Moral, M.P.; Kannan, K. Variability in urinary biomarkers of human exposure to polycyclic aromatic hydrocarbons and its association with oxidative stress. Environ. Int. 2021, 156, 106720. [Google Scholar] [CrossRef]
- Akanji, M.A.; Rotimi, D.E.; Elebiyo, T.C.; Awakan, O.J.; Adeyemi, O.S. Redox homeostasis and prospects for therapeutic targeting in neurodegenerative disorders. Oxid. Med. Cell Longev. 2021, 2021, 9971885. [Google Scholar] [CrossRef]
- Masarone, M.; Rosato, V.; Dallio, M.; Gravina, A.G.; Aglitti, A.; Loguercio, C. Role of oxidative stress in pathophysiology of nonalcoholic fatty liver disease. Oxid. Med. Cell Longev. 2018, 2018, 9547613. [Google Scholar] [CrossRef]
- Uchida, D.; Takaki, A.; Oyama, A.; Adachi, T.; Wada, N.; Onishi, H. Oxidative stress management in chronic liver diseases and hepatocellular carcinoma. Nutrients 2020, 12, 6. [Google Scholar] [CrossRef]
- Wang, J.H.; Lee, S.B.; Lee, D.S.; Son, C.G. Total antioxidant capacity in HBV carriers, a promising biomarker for evaluating hepatic fibrosis: A pilot study. Antioxidants 2021, 10, 77. [Google Scholar] [CrossRef]
- Yuan, T.; Yang, T.; Chen, H.; Fu, D.; Hu, Y.; Wang, J. New insights into oxidative stress and inflammation during diabetes mellitus-accelerated atherosclerosis. Redox Biol. 2019, 20, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Alavian, S.M.; Showraki, A. Hepatitis B and its relationship with oxidative stress. Hepat. Mon. 2016, 16, e37973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paliogiannis, P.G.; Fois, A.G.; Sotgia, S.; Mangoni, A.A.; Zinellu, E.; Pirina, P. Circulating malondialdehyde concentrations in patients with stable chronic obstructive pulmonary disease: A systematic review and meta-analysis. Biomark. Med. 2018, 12, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Pinna, A.; Boscia, F.; Paliogiannis, P.; Carru, C.; Zinellu, A. Malondialdehyde levels in patients with age-related macular degeneration: A systematic review and meta-analysis. Retina 2020, 40, 195–203. [Google Scholar] [CrossRef]
- Yegorov, Y.E.; Poznyak, A.V.; Nikiforov, N.G.; Sobenin, I.A.; Orekhov, A.N. The link between chronic stress and accelerated aging. Biomedicines 2020, 8, 198. [Google Scholar] [CrossRef]
- Poznyak, A.; Grechko, A.; Poggio, P.; Myasoedova, V.A.; Alfieri, V.; Orekhov, A.N. The diabetes mellitus-atherosclerosis connection: The role of lipid and glucose metabolism and chronic inflammation. Int. J. Mol. Sci. 2020, 21, 1835. [Google Scholar] [CrossRef] [Green Version]
- Ahmad, S.; Moorthy, M.; Demler, O.V.; Hu, F.B.; Ridker, P.M.; Chasman, D.I. Assessment of risk factors and biomarkers associated with risk of cardiovascular disease among women consuming a Mediterranean diet. JAMA Netw. Open 2018, 1, e185708. [Google Scholar] [CrossRef] [Green Version]
- Elpek, G.O. Molecular pathways in viral hepatitis-associated liver carcinogenesis: An update. World J. Clin. Cases 2021, 9, 4890–4917. [Google Scholar] [CrossRef]
- Ivanov, A.V.; Valuev-Elliston, V.T.; Tyurina, D.A.; Ivanova, O.N.; Kochetkov, S.N.; Bartosch, B. Oxidative stress, a trigger of hepatitis C and B virus-induced liver carcinogenesis. Oncotarget 2017, 8, 3895–3932. [Google Scholar] [CrossRef] [Green Version]
- Guo, S.E.; Huang, T.J.; Lin, M.S.; Huang, R.M.; Chang, C.H.; Chen, M.Y. Alcohol, betel nut, and cigarette consumption are negatively associated with health promoting behaviors in Taiwan: A cross sectional study. BMC Public Health 2013, 13, 257. [Google Scholar] [CrossRef] [Green Version]
- Li, W.; Chang, T.S.; Chang, S.Z.; Chen, C.H.; Chen, M.Y. Challenges of transferring rural adults with chronic HCV infection for further HCV RNA confirmation and free DAAs treatment: A success story of the interdisciplinary collaboration approach. BMC Infect. Dis. 2020, 20, 737. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.C.; Chiu, W.; Chang, T.S.; Huang, T.J.; Chen, M.Y. Liver health literacy and health status among adults with hepatitis C: Implications for the nursing profession as part of the 2030 global elimination goal. J. Nurs. Scholarsh. 2019, 52, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Health Promotion Administration, HPA. Metabolic Syndrome. Available online: https://www.hpa.gov.tw/Pages/List.aspx?nodeid=359 (accessed on 1 January 2021).
- Caliri, A.W.; Tommasi, S.; Besaratinia, A. Relationships among smoking, oxidative stress, inflammation, macromolecular damage, and cancer. Mutat. Res. 2021, 787, 108365. [Google Scholar] [CrossRef] [PubMed]
- Gearhart-Serna, L.M.; Tacam, M., Jr.; Slotkin, T.A.; Devi, G.R. Analysis of polycyclic aromatic hydrocarbon intake in the US adult population from NHANES 2005-2014 identifies vulnerable subpopulations, suggests interaction between tobacco smoke exposure and sociodemographic factors. Environ. Res. 2021, 201, 111614. [Google Scholar] [CrossRef]
- Ding, Y.S.; Ward, J.; Hammond, D.; Watson, C.H. Mouth-level intake of benzo[a]pyrene from reduced nicotine cigarettes. Int. J. Environ. Res. Public Health 2014, 11, 11898–11914. [Google Scholar] [CrossRef] [Green Version]
- Zhou, B.; Ma, Y.; Wei, F.; Zhang, L.; Chen, X.; Peng, S. Association of active/passive smoking and urinary 1-hydroxypyrene with poor sleep quality: A cross-sectional survey among Chinese male enterprise workers. Tob. Induc. Dis. 2018, 16, 23. [Google Scholar] [CrossRef]
- Chen, I.C.; Chiang, W.F.; Chen, P.F.; Chiang, H.C. STRESS-responsive deacetylase SIRT3 is up-regulated by areca nut extract-induced oxidative stress in human oral keratinocytes. J. Cell Biochem. 2014, 115, 328–339. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Mathangasinghe, Y.; Jayawardena, R.; Hills, A.P.; Misra, A. Prevalence and trends of metabolic syndrome among adults in the Asia-pacific region: A systematic review. BMC Public Health 2017, 17, 101. [Google Scholar] [CrossRef] [Green Version]
- Lechner, K.; von Schacky, C.; McKenzie, A.L.; Worm, N.; Nixdorff, U.; Lechner, B. Lifestyle factors and high-risk atherosclerosis: Pathways and mechanisms beyond traditional risk factors. Eur. J. Prev. Cardiol. 2020, 7, 394–406. [Google Scholar] [CrossRef] [Green Version]
- Taiwan Medical Association, TMA. Hepatitis C Epidemiology and Prevention Strategy. Available online: http://www.fma.org.tw/2016/I-1-3.html/ (accessed on 20 May 2020).
- World Health Organization. Fact Sheet: Hepatitis C. Available online: http://www.who.int/newsroom/fact-sheets/detail/hepatitis-c/ (accessed on 15 May 2020).
- National Health Insurance, NHI. Hepatitis C Full Oral New Drug Health Insurance Payment Implementation Plan. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=A4EFF6CD1C4891CA&topn=3FC7D09599D25979 (accessed on 25 May 2021).
- Wu, P.S.; Chang, T.S.; Lu, S.N.; Chang, S.Z.; Su, H.J.; Chen, M.Y. An investigation of the side effects, patient feedback, and physiological changes associated with direct-acting antiviral therapy for hepatitis C. Int. J. Environ. Res. Public Health 2019, 16, 4981. [Google Scholar] [CrossRef] [Green Version]
- Chen, M.Y. The negative impact of parental smoking on adolescents’ health- promoting behaviors: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 2514. [Google Scholar] [CrossRef] [PubMed]
- Sharma, T.; Khapre, M. Exposure of secondhand smoke in women and children: A narrative review. J. Family Med. Prim. Care 2021, 10, 1804–1807. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total (N = 6335) | Female (n = 3574) | Male (n = 2761) | p-Value |
|---|---|---|---|---|
| Age, year | 47.7 ± 16.1 | 47.9 ± 16.2 | 47.3 ± 16.0 | 0.109 |
| Education level, years | 9.6 ± 5.8 | 8.8 ± 6.2 | 10.7 ± 4.9 | <0.001 |
| Body mass index ≥ 24 kg/m2 | 3518 (55.5) | 1672 (46.8) | 1846 (66.9) | <0.001 |
| Metabolic syndrome (MetS) | 1909 (30.1) | 980 (27.4) | 929 (33.6) | <0.001 |
| No. of MetS components | 1.74 ± 1.39 | 1.59 ± 1.42 | 1.93 ± 1.33 | <0.001 |
| Each component of MetS | ||||
| SBP/DBP ≥ 130/85 mmHg | 3468 (54.7) | 1703 (47.6) | 1765 (63.9) | <0.001 |
| Waist circumference 1 | 2636 (41.6) | 1518 (42.5) | 1118 (40.5) | 0.113 |
| FBG ≥ 100 mg/dL | 2217 (35.0) | 1096 (30.7) | 1121 (40.6) | <0.001 |
| HDL-C < 40/50 (M/F) mg/dL | 778 (12.3) | 210 (5.9) | 568 (20.6) | <0.001 |
| Triglyceride ≥ 150 mg/dL | 1213 (19.1) | 460 (12.9) | 753 (27.3) | <0.001 |
| Smoking | <0.001 | |||
| Never | 5055 (79.8) | 3412 (95.5) | 1643 (59.5) | |
| Current/Quit | 1280 (20.2) | 162 (4.5) | 1118 (40.5) | |
| Alcoholic drinking | <0.001 | |||
| Never | 5520 (87.1) | 3472 (97.1) | 2048 (74.2) | |
| Current/Quit | 815 (12.9) | 102 (2.9) | 713 (25.8) | |
| Betel nut chewing | <0.001 | |||
| Never | 5699 (90.0) | 3544 (99.2) | 2155 (78.1) | |
| Current/Quit | 636 (10.0) | 30 (0.8) | 606 (21.9) | |
| Intake vegetables | <0.001 | |||
| Never/Seldom | 2144 (33.8) | 1056 (29.5) | 1088 (39.4) | |
| Often | 4191 (66.2) | 2518 (70.5) | 1673 (60.6) | |
| Intake fruit | <0.001 | |||
| Never/Seldom | 3512 (55.4) | 1823 (51.0) | 1689 (61.2) | |
| Often | 2823 (44.6) | 1751 (49.0) | 1072 (38.8) | |
| Adopt regular exercise | <0.001 | |||
| Never/Seldom | 4392 (69.3) | 2593 (72.6) | 1799 (65.2) | |
| Often | 1943 (30.7) | 981 (27.4) | 962 (34.8) | |
| HBsAg | 1067 (16.8) | 528 (14.8) | 539 (19.5) | <0.001 |
| Anti-HCV | 909 (14.3) | 553 (15.5) | 356 (12.9) | 0.004 |
| AST > 35 U/L | 653 (10.3) | 277 (7.8) | 376 (13.6) | <0.001 |
| ALT > 35 U/L | 1362 (21.5) | 461 (12.9) | 901 (32.6) | <0.001 |
| 1-OHP, μg/g CRE | 0.11 [0.07, 0.18] | 0.11 [0.07, 0.17] | 0.10 [0.06, 0.19] | 0.015 |
| MDA, μg/g CRE | 0.90 [0.40, 1.50] | 0.90 [0.40, 1.50] | 1.00 [0.50, 1.50] | 0.034 |
| Variable | Q1 (n = 1864) | Q2 (n = 1483) | Q3 (n = 1462) | Q4 (n = 1526) | p-Value | p Trend |
|---|---|---|---|---|---|---|
| Level, μmol/g CRE 1 | ≤0.07 | 0.07–0.11 | 0.11–0.18 | >0.18 | ||
| Age, year | 50.7 ± 17.2 | 47.3 ± 16.4 a | 46.1 ± 15.8 a | 45.8 ± 14.2 a | <0.001 | <0.001 |
| Female | 946 (50.8) | 874 (58.9) a | 956 (65.4) a,b | 798 (52.3) b,c | <0.001 | 0.014 |
| Education level, years | 9.4 ± 6.3 | 9.9 ± 6.0 | 9.7 ± 5.7 | 9.4 ± 5.0 | 0.064 | 0.867 |
| BMI ≥ 24 kg/m2 | 1079 (57.9) | 828 (55.8) | 767 (52.5) a | 844 (55.3) | 0.020 | 0.035 |
| MetS | 581 (31.2) | 433 (29.2) | 412 (28.2) | 483 (31.7) | 0.117 | 0.970 |
| Each component of MetS | 1.83 ± 1.39 | 1.66 ± 1.38 a | 1.66 ± 1.38 a | 1.78 ± 1.41 | 0.001 | 0.335 |
| Each MetS component | ||||||
| SBP/DBP ≥ 130/85 mmHg | 1162 (62.3) | 788 (53.1) a | 753 (51.5) a | 765 (50.1) a | <0.001 | <0.001 |
| WC 1 | 749 (40.2) | 633 (42.7) | 613 (41.9) | 641 (42.0) | 0.489 | 0.335 |
| FBG ≥ 100 mg/dL | 732 (39.3) | 499 (33.6) a | 456 (31.2) a | 530 (34.7) a | <0.001 | 0.001 |
| HDL-C < 40/50(M/F) mg/dL | 216 (11.6) | 147 (9.9) | 157 (10.7) | 258 (16.9) a,b,c | <0.001 | <0.001 |
| TG ≥ 150 mg/dL | 352 (18.9) | 234 (15.8) | 261 (17.9) | 366 (24.0) a,b,c | <0.001 | <0.001 |
| Smoking | <0.001 | <0.001 | ||||
| Never | 1696 (91.0) | 1322 (89.1) | 1197 (81.9) a,b | 840 (55.0) a,b,c | ||
| Current/Quit | 168 (9.0) | 161 (10.9) | 265 (18.1) a,b | 686 (45.0) a,b,c | ||
| Alcoholic drinking | <0.001 | <0.001 | ||||
| Never | 1703 (91.4) | 1321 (89.1) | 1284 (87.8) a | 1212 (79.4) a,b,c | ||
| Current/Quit | 161 (8.6) | 162 (10.9) | 178 (12.2) a | 314 (20.6) a,b,c | ||
| Betel nut chewing | <0.001 | <0.001 | ||||
| Never | 1743 (93.5) | 1392 (93.9) | 1334 (91.2) b | 1230 (80.6) a,b,c | ||
| Current/Quit | 121 (6.5) | 91 (6.1) | 128 (8.8) b | 296 (19.4) a,b,c | ||
| Intake vegetables | <0.001 | <0.001 | ||||
| Never/Seldom | 589 (31.6) | 464 (31.3) | 508 (34.7) | 583 (38.2) a,b | ||
| Often | 1275 (68.4) | 1019 (68.7) | 954 (65.3) | 943 (61.8) a,b | ||
| Intake fruit | <0.001 | <0.001 | ||||
| Never/Seldom | 985 (52.8) | 784 (52.9) | 811 (55.5) | 932 (61.1) a,b,c | ||
| Often | 879 (47.2) | 699 (47.1) | 651 (44.5) | 594 (38.9) a,b,c | ||
| Adopt regular exercise | <0.001 | <0.001 | ||||
| Never/Seldom | 1211 (65.0) | 1004 (67.7) | 1055 (72.2) a,b | 1122 (73.5) a,b | ||
| Often | 653 (35.0) | 479 (32.3) | 407 (27.8) a,b | 404 (26.5) a,b | ||
| HBsAg | 275 (14.8) | 238 (16.0) | 270 (18.5) a | 284 (18.6) a | 0.005 | 0.001 |
| Anti-HCV | 247 (13.3) | 214 (14.4) | 204 (14.0) | 244 (16.0) | 0.147 | 0.043 |
| AST > 35 U/L | 159 (8.5) | 133 (9.0) | 148 (10.1) | 213 (14.0) a,b,c | <0.001 | <0.001 |
| ALT > 35 U/L | 379 (20.3) | 291 (19.6) | 310 (21.2) | 382 (25.0) a,b | 0.001 | 0.001 |
| Explanatory Variable | Total | Female | Male | |||
|---|---|---|---|---|---|---|
| Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | |
| Age, year | 0.97 (0.96–0.98) | <0.001 | 0.97 (0.96–0.98) | <0.001 | 0.98 (0.97–0.98) | <0.001 |
| Female | 2.30 (2.06–2.57) | <0.001 | - | - | - | - |
| Education level, years | 0.96 (0.95–0.97) | <0.001 | 0.96 (0.95–0.98) | <0.001 | 0.94 (0.93–0.96) | <0.001 |
| Metabolic syndrome | 1.10 (0.99–1.22) | 0.082 | 1.05 (0.90–1.21) | 0.561 | 1.17 (1.00–1.36) | 0.049 |
| Frequent intake vegetables | 1.00 (0.90–1.11) | 0.990 | 1.06 (0.92–1.22) | 0.457 | 0.97 (0.83–1.13) | 0.665 |
| Frequent intake fruit | 0.96 (0.87–1.07) | 0.465 | 1.02 (0.89–1.16) | 0.766 | 0.86 (0.73–1.01) | 0.060 |
| Adopt regular exercise | 0.93 (0.84–1.03) | 0.179 | 1.09 (0.95–1.25) | 0.237 | 0.80 (0.69–0.94) | 0.005 |
| Smoking | 6.94 (5.96–8.08) | <0.001 | 9.27 (6.46–13.30) | <0.001 | 6.01 (5.06–7.15) | <0.001 |
| Alcoholic drinking | 1.16 (0.99–1.36) | 0.061 | 1.20 (0.82–1.75) | 0.347 | 1.13 (0.95–1.35) | 0.162 |
| Betel nut chewing | 1.25 (1.04–1.52) | 0.019 | 2.04 (1.01–4.10) | 0.046 | 1.14 (0.93–1.39) | 0.204 |
| HBsAg | 1.27 (1.12–1.43) | <0.001 | 1.26 (1.07–1.49) | 0.007 | 1.30 (1.09–1.55) | 0.003 |
| Anti-HCV | 1.43 (1.24–1.64) | <0.001 | 1.49 (1.24–1.79) | <0.001 | 1.39 (1.11–1.73) | 0.003 |
| Variable | Q1 (n = 1654) | Q2 (n = 1581) | Q3 (n = 1601) | Q4 (n = 1499) | p-Value | p Trend |
|---|---|---|---|---|---|---|
| Level, μmol/g creatinine | ≤0.4 | 0.4–0.9 | 0.9–1.5 | >1.5 | ||
| Age, year | 43.7 ± 15.3 | 44.7 ± 15.5 | 48.3 ± 15.5 a,b | 54.4 ± 16.1 a,b,c | <0.001 | <0.001 |
| Female | 1022 (61.8) | 839 (53.1) a | 826 (51.6) a | 887 (59.2) b,c | <0.001 | 0.058 |
| Education level, years | 10.8 ± 5.5 | 10.7 ± 5.5 | 9.5 ± 5.6 a,b | 7.3 ± 6.0 a,b,c | <0.001 | <0.001 |
| Body mass index ≥ 24 kg/m2 | 814 (49.2) | 833 (52.7) | 941 (58.8) a,b | 930 (62.0) a,b | <0.001 | <0.001 |
| Metabolic syndrome (MetS) | 398 (24.1) | 433 (27.4) | 502 (31.4) a | 576 (38.4) a,b,c | <0.001 | <0.001 |
| No. of MetS components | 1.51 ± 1.32 | 1.63 ± 1.40 | 1.81 ± 1.40 a,b | 2.04 ± 1.40 a,b,c | <0.001 | <0.001 |
| Each component of MetS | ||||||
| SBP/DBP ≥ 130/85 mmHg | 818 (49.5) | 814 (51.5) | 907 (56.7) a,b | 929 (62.0) a,b,c | <0.001 | <0.001 |
| Waist circumference 1 | 607 (36.7) | 612 (38.7) | 675 (42.2) a | 742 (49.5) a,b,c | <0.001 | <0.001 |
| FBG ≥ 100 mg/dL | 487 (29.4) | 499 (31.6) | 583 (36.4) a,b | 648 (43.2) a,b,c | <0.001 | <0.001 |
| HDL-C < 40/50 (M/F) mg/dL | 153 (9.3) | 187 (11.8) | 210 (13.1) a | 228 (15.2) a,b | <0.001 | <0.001 |
| Triglyceride ≥ 150 mg/dL | 258 (15.6) | 295 (18.7) | 348 (21.7) a | 312 (20.8) a | <0.001 | <0.001 |
| Smoking | <0.001 | <0.001 | ||||
| Never | 1400 (84.6) | 1266 (80.1) a | 1219 (76.1) a,b | 1170 (78.1) a | ||
| Current/Quit | 254 (15.4) | 315 (19.9) a | 382 (23.9) a,b | 329 (21.9) a | ||
| Alcoholic drinking | <0.001 | 0.002 | ||||
| Never | 1481 (89.5) | 1385 (87.6) | 1354 (84.6) a | 1300 (86.7) | ||
| Current/Quit | 173 (10.5) | 196 (12.4) | 247 (15.4) a | 199 (13.3) | ||
| Betel nut chewing | <0.001 | <0.001 | ||||
| Never | 1543 (93.3) | 1449 (91.7) | 1404 (87.7) a,b | 1303 (86.9) a,b | ||
| Current/Quit | 111 (6.7) | 132 (8.3) | 197 (12.3) a,b | 196 (13.1) a,b | ||
| Intake vegetables | 0.078 | 0.017 | ||||
| Never/Seldom | 591 (35.7) | 552 (34.9) | 515 (32.2) | 486 (32.4) | ||
| Often | 1063 (64.3) | 1029 (65.1) | 1086 (67.8) | 1013 (67.6) | ||
| Intake fruit | 0.382 | 0.125 | ||||
| Never/Seldom | 934 (56.5) | 894 (56.5) | 869 (54.3) | 815 (54.4) | ||
| Often | 720 (43.5) | 687 (43.5) | 732 (45.7) | 684 (45.6) | ||
| Adopt regular exercise | 0.071 | 0.018 | ||||
| Never/Seldom | 1168 (70.6) | 1110 (70.2) | 1115 (69.6) | 999 (66.6) | ||
| Often | 486 (29.4) | 471 (29.8) | 486 (30.4) | 500 (33.4) | ||
| HBsAg | 235 (14.2) | 247 (15.6) | 299 (18.7) a | 286 (19.1) a | <0.001 | <0.001 |
| Anti-HCV | 164 (9.9) | 153 (9.7) | 225 (14.1) a,b | 367 (24.5) a,b,c | <0.001 | <0.001 |
| AST > 35 U/L | 105 (6.3) | 134 (8.5) | 175 (10.9) a | 239 (15.9) a,b,c | <0.001 | <0.001 |
| ALT > 35 U/L | 293 (17.7) | 317 (20.1) | 377 (23.5) a | 375 (25.0) a,b | <0.001 | <0.001 |
| Explanatory Variable | Total | Female | Male | |||
|---|---|---|---|---|---|---|
| Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | |
| Age, year | 1.02 (1.01–1.02) | <0.001 | 1.02 (1.01–1.03) | <0.001 | 1.02 (1.01–1.03) | <0.001 |
| Female | 0.99 (0.89–1.10) | 0.792 | - | - | - | - |
| Education level, years | 0.98 (0.97–0.99) | 0.001 | 0.99 (0.97–1.01) | 0.217 | 0.96 (0.94–0.98) | <0.001 |
| Metabolic syndrome | 1.08 (0.98–1.20) | 0.129 | 1.13 (0.97–1.31) | 0.113 | 1.06 (0.91–1.22) | 0.482 |
| Frequent intake vegetables | 1.08 (0.97–1.19) | 0.173 | 1.14 (0.99–1.31) | 0.074 | 1.01 (0.87–1.18) | 0.884 |
| Frequent intake fruit | 1.00 (0.91–1.10) | 0.994 | 0.96 (0.84–1.09) | 0.518 | 1.05 (0.90–1.22) | 0.517 |
| Adopt regular exercise | 1.01 (0.91–1.11) | 0.914 | 0.98 (0.85–1.12) | 0.756 | 1.05 (0.90–1.21) | 0.551 |
| Smoking | 1.32 (1.15–1.51) | <0.001 | 1.30 (0.97–1.74) | 0.079 | 1.33 (1.14–1.56) | <0.001 |
| Alcoholic drinking | 1.00 (0.86–1.16) | 0.956 | 1.18 (0.82–1.70) | 0.381 | 0.96 (0.81–1.14) | 0.637 |
| Betel nut chewing | 1.22 (1.02–1.45) | 0.029 | 1.10 (0.55–2.21) | 0.780 | 1.23 (1.01–1.49) | 0.039 |
| HBsAg | 1.25 (1.11–1.41) | <0.001 | 1.25 (1.06–1.47) | 0.009 | 1.28 (1.08–1.52) | 0.004 |
| Anti-HCV | 1.48 (1.29–1.70) | <0.001 | 1.43 (1.19–1.72) | <0.001 | 1.56 (1.26–1.94) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, C.-H.; Huang, T.-J.; Lin, Y.-C.; Lin, C.-N.; Chen, M.-Y. Factors Associated with Urinary 1-Hydroxypyrene and Malondialdehyde among Adults near a Petrochemical Factory: Implications for Sex and Lifestyle Modification. Int. J. Environ. Res. Public Health 2022, 19, 1362. https://doi.org/10.3390/ijerph19031362
Huang C-H, Huang T-J, Lin Y-C, Lin C-N, Chen M-Y. Factors Associated with Urinary 1-Hydroxypyrene and Malondialdehyde among Adults near a Petrochemical Factory: Implications for Sex and Lifestyle Modification. International Journal of Environmental Research and Public Health. 2022; 19(3):1362. https://doi.org/10.3390/ijerph19031362
Chicago/Turabian StyleHuang, Cheng-Hsien, Tung-Jung Huang, Yu-Chih Lin, Chia-Ni Lin, and Mei-Yen Chen. 2022. "Factors Associated with Urinary 1-Hydroxypyrene and Malondialdehyde among Adults near a Petrochemical Factory: Implications for Sex and Lifestyle Modification" International Journal of Environmental Research and Public Health 19, no. 3: 1362. https://doi.org/10.3390/ijerph19031362
APA StyleHuang, C.-H., Huang, T.-J., Lin, Y.-C., Lin, C.-N., & Chen, M.-Y. (2022). Factors Associated with Urinary 1-Hydroxypyrene and Malondialdehyde among Adults near a Petrochemical Factory: Implications for Sex and Lifestyle Modification. International Journal of Environmental Research and Public Health, 19(3), 1362. https://doi.org/10.3390/ijerph19031362






