Effects of a Physical Exercise Intervention on Pain in Workplaces: A Case Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects and Design
2.2. Instruments
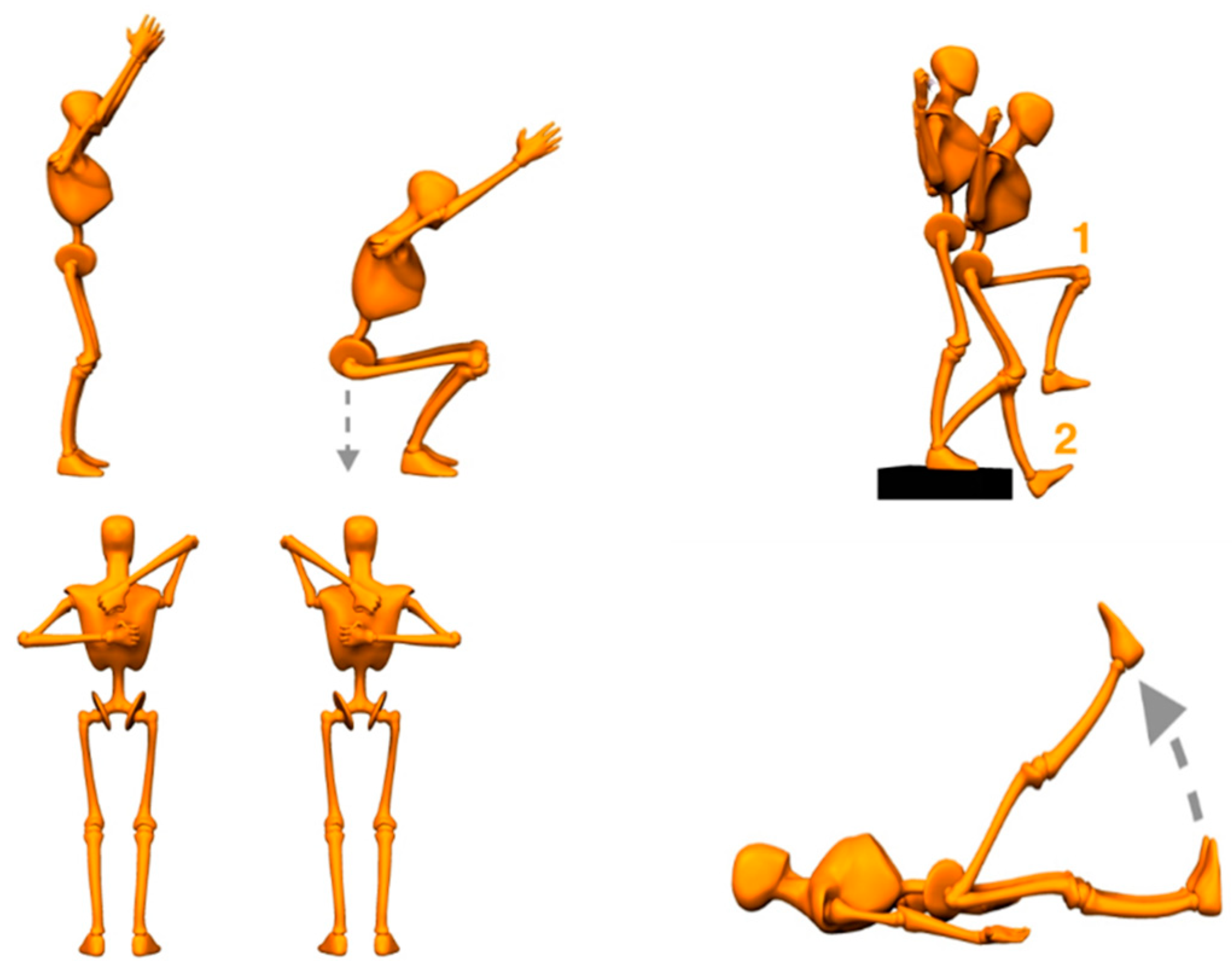
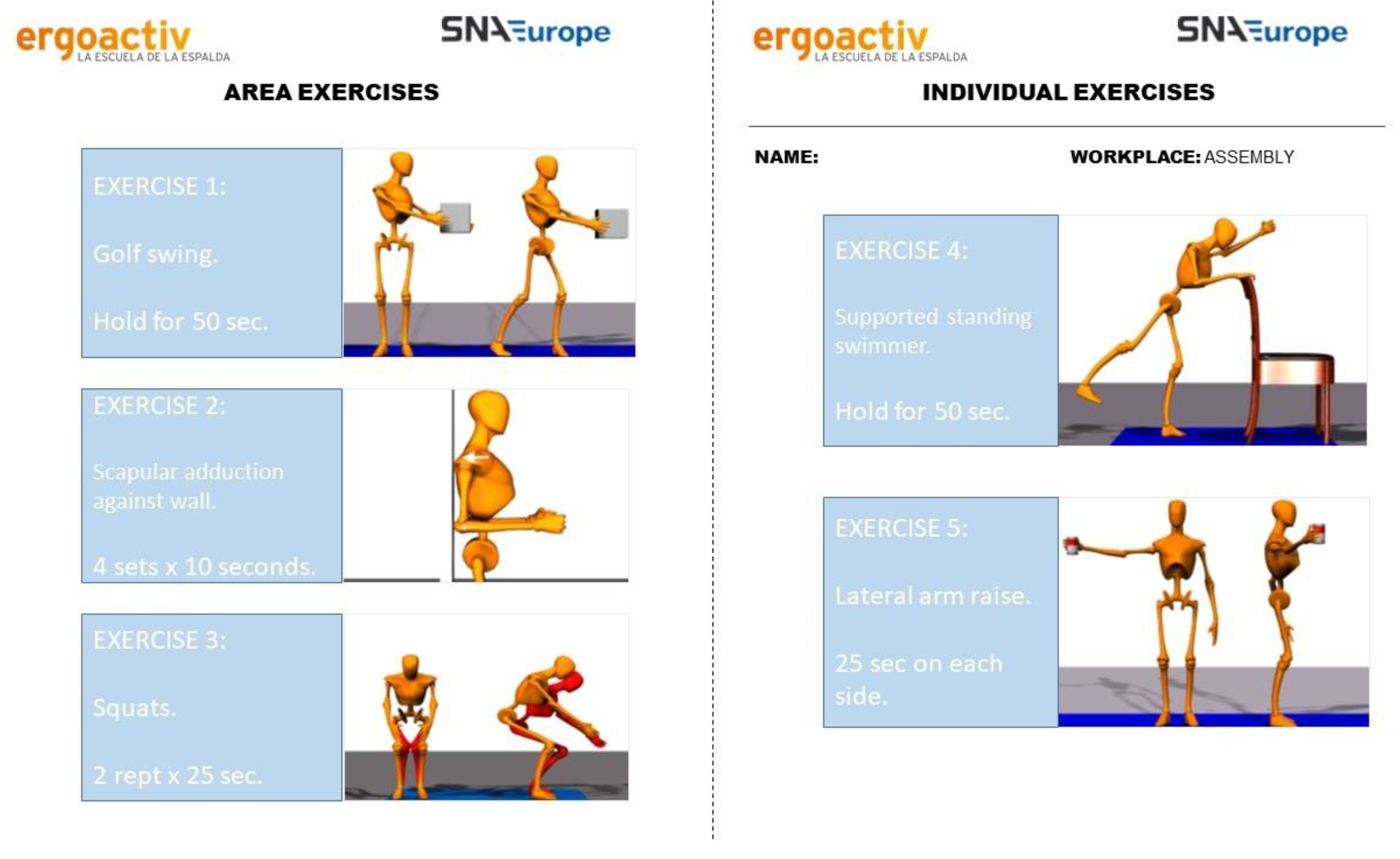
2.3. Procedure
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Inoue, K.; Drori, G.S. The global institutionalization of health as a social concern: Organizational and discursive trends. Int. Sociol. 2006, 21, 199–219. [Google Scholar] [CrossRef]
- Diaz, K.M.; Howard, V.J.; Hutto, B.; Colabianchi, N.; Vena, J.E.; Safford, M.M.; Blair, S.N.; Hooker, S.P.; Less, S. Patterns of sedentary behavior and mortality in US middle-aged and older adults: A national cohort study. Ann. Intern. Med. 2017, 167, 465–475. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Centre for Economics and Business Research. The Economic Cost of Physical Inactivity in Europe; International Council of Sport Science and Physical Education: Berlin, Germany, 2015. [Google Scholar]
- Ding, D.; Lawson, K.D.; Kolbe-Alexander, T.L.; Finkelstein, E.A.; Katzmarzyk, P.T.; Van Mechelen, W.; Pratt, M. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 2016, 388, 1311–1324. [Google Scholar] [CrossRef]
- World Health Organization. ACTIVE: Package of Technical Interventions to Increase Physical Activity; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- García-Hermoso, A.; Ramírez-Vélez, R.; Ramirez-Campillo, R.; Izquierdo, M. Relationship between ideal cardiovascular health and disability in older adults: The Chilean national health survey (2009–10). J. Am. Geriatr. Soc. 2017, 65, 2727–2732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, X.L.; Wang, L.N.; Wang, J.; Zhou, L.; Shen, X.H. Effects of exercise interventions for specific cognitive domains in old adults with mild cognitive impairment: A meta-analysis and subgroup analysis of randomized controlled trials. Medicine 2020, 99, e20105. [Google Scholar] [CrossRef] [PubMed]
- Gordon, B.R.; McDowell, C.P.; Hallgren, M.; Meyer, J.D.; Lyons, M.; Herring, M.P. Association of efficacy of resistance exercise training with depressive symptoms: Meta-analysis and meta-regression analysis of randomized clinical trials. JAMA Psychiatry 2018, 75, 566–576. [Google Scholar] [CrossRef] [PubMed]
- Klil-Drori, S.; Klil-Drori, A.J.; Pira, S.; Rej, S. Exercise intervention for late-life depression: A meta-analysis. J. Clin. Psychiatry 2020, 81, 19r12877. [Google Scholar] [CrossRef] [PubMed]
- Feter, N.; Mielke, G.I.; Leite, J.S.; Brown, W.J.; Coombes, J.S.; Rombaldi, A.J. Physical activity in later life and risk of dementia: Findings from a population-based cohort study. Exp. Gerontol. 2021, 143, 111145. [Google Scholar] [CrossRef]
- Ezzatvar, Y.; Ramírez-Vélez, R.; de Asteasu, M.S.; Martínez-Velilla, N.; Zambom-Ferraresi, F.; Izquierdo, M.; García-Hermoso, A. Physical function and all-cause mortality in older adults diagnosed with cancer: A systematic review and meta-analysis. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 76, 1447–1453. [Google Scholar] [CrossRef]
- Kirk, M.A.; Rhodes, R.E. Occupation correlates of adults’ participation in leisure-time physical activity—A systematic review. Am. J. Prev. Med. 2011, 40, 476–485. [Google Scholar] [CrossRef]
- Owen, N.; Sugiyama, T.; Eakin, E.E.; Gardiner, P.A.; Trembly, M.S.; Sallis, J.F. Adults’ sedentary behaviour determinants and interventions. Am. J. Prev. Med. 2011, 41, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.N.; Heady, J.A.; Raffle, P.A.B.; Roberts, C.G.; Parks, J.W. Coronary heart-disease and physical activity of work. Lancet 1958, 262, 1111–1120. [Google Scholar] [CrossRef]
- Paffenbarger, R.S., Jr.; Laughlin, M.E.; Gima, A.S.; Black, R.A. Work activity of longshoremen as related to death from coronary heart disease and stroke. N. Engl. J. Med. 1970, 282, 1109–1114. [Google Scholar] [CrossRef] [PubMed]
- Clemes, S.A.; O’Connell, S.E.; Edwardson, C.L. Office workers’ objectively measured sedentary behavior and physical activity during and outside working hours. J. Occup. Environ. Med. 2014, 56, 298–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ECORYS. Physical Activity at the Workplace: Literature Review and Best Practice Case Studies: A Report to the European Commission; EU Publications: Brussels, Belgium, 2017. [Google Scholar]
- Parry, S.; Straker, L. The contribution of office work to sedentary behaviour associated risk. BMC Public Health 2013, 13, 296–305. [Google Scholar] [CrossRef] [Green Version]
- National Institute of Safety and Hygiene at Work (INSHT). Socio-Economic Evaluation of a Physical Activity Program for the Workers of a Company 2013; Ministry of Employment and Social Security: Madrid, Spain, 2013.
- Price Waterhouse Coopers. Work, Health and Wellbeing: Building the Case for Wellness; Department for Work and Pensions: London, UK, 2013.
- Akogun, O.; Dillon, A.; Friedman, J.; Prasann, A.; Serneels, P. Productivity and Health: Physical Activity as a Measure of Effort. World Bank Econ. Rev. 2021, 35, 652–680. [Google Scholar] [CrossRef]
- Gebreslassie, M.; Sampaio, F.; Nystrand, C.; Ssegonja, R.; Feldman, I. Economic evaluations of public health interventions for physical activity and healthy diet: A systematic review. Prev. Med. 2020, 136, 106100. [Google Scholar] [CrossRef] [PubMed]
- Abu-Omar, K.; Rütten, A.; Burlacu, I.; Schätzlein, V.; Messing, S.; Suhrcke, M. The cost-effectiveness of physical activity interventions: A systematic review of reviews. Prev. Med. Rep. 2017, 8, 72–78. [Google Scholar] [CrossRef]
- Ryde, G.C.; Gilson, N.D.; Burton, N.W.; Brown, W.J. Recruitment rates in workplace physical activity interventions: Characteristics for success. Am. J. Health Promot. 2013, 27, 101–112. [Google Scholar] [CrossRef]
- Heise, T.L.; Frense, J.; Christianson, L.; Seuring, T. Using financial incentives to increase physical activity among employees as a strategy of workplace health promotion: Protocol for a systematic review. BMJ Open 2021, 11, e042888. [Google Scholar] [CrossRef]
- Chapman, L.S. Meta-evaluation of worksite health promotion economic return studies: 2005 update. Am. J. Health Promot. 2005, 19, 1–11. [Google Scholar] [CrossRef] [PubMed]
- López-Bueno, R.; Casajús-Mallén, J.A.; Garatachea-Vallejo, N. La actividad física como herramienta para reducir el absentismo laboral debido a enfermedad en trabajadores sedentarios: Una revisión sistemática. Rev. Esp. Salud Pública 2018, 92, 1–11. [Google Scholar]
- Mulchandani, R.; Chandrasekaran, A.M.; Shivashankar, R.; Kondal, D.; Agrawal, A.; Panniyammakal, J.; Tandon, N.; Prabhakaran, D.; Sharma, M.; Goenka, S. Effect of workplace physical activity interventions on the cardio-metabolic health of working adults: Systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 134–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sultana, R.N.; Sabag, A.; Keating, S.E.; Johnson, N.A. The effect of low-volume high-intensity interval training on body composition and cardiorespiratory fitness: A systematic review and meta-analysis. Sports Med. 2019, 49, 1687–1721. [Google Scholar] [CrossRef] [PubMed]
- Chimenti, R.L.; Frey-Law, L.A.; Sluka, K.A. A mechanism-based approach to physical therapist management of pain. Phys. Ther. 2018, 98, 302–314. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar] [CrossRef] [Green Version]
- Da Costa, B.R.; Vieira, E.R. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. Am. J. Ind. Med. 2010, 53, 285–323. [Google Scholar] [CrossRef]
- Gaskin, D.J.; Richard, P. The economic costs of pain in the United States. J. Pain 2012, 13, 715–724. [Google Scholar] [CrossRef]
- Korshøj, M.; Birk Jørgensen, M.; Lidegaard, M.; Mortensen, O.S.; Krustrup, P.; Holtermann, A.; Søgaard, K. Decrease in musculoskeletal pain after 4 and 12 months of an aerobic exercise intervention: A worksite RCT among cleaners. Scand. J. Public Health 2018, 46, 846–853. [Google Scholar] [CrossRef]
- Bell, J.A.; Burnett, A. Exercise for the Primary, Secondary and Tertiary Prevention of Low Back Pain in the Workplace: A Systematic Review. J. Occup. Rehabil. 2009, 19, 8–24. [Google Scholar] [CrossRef] [Green Version]
- Hallam, J.S.; Petosa, R. The long-term impact of a four-session work-site intervention on selected social cognitive theory variables linked to adult exercise adherence. Health Educ. Behav. 2004, 31, 88–100. [Google Scholar] [CrossRef] [PubMed]
- van Dongen, J.M.; Proper, K.I.; van Wier, M.F.; van der Beek, A.J.; Bongers, P.M.; van Mechelen, W.; van Tulder, M.W. A systematic review of the cost-effectiveness of worksite physical activity and/or nutrition programs. Scand. J. Work Environ. Health 2012, 38, 393–408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aldana, S.G. Financial impact of health promotion programs: A comprehensive review of the literature. Am. J. Health Promot. 2001, 15, 296–320. [Google Scholar] [CrossRef] [PubMed]
- Proper, K.; Mechelen, W. Effectiveness and Economic Impact of Worksite Interventions to Promote Physical Activity and Healthy Diet; World Health Organization: Amsterdam, The Netherlands, 2007. [Google Scholar]
- UK Healthzone. Why Should Small and Medium Size Enterprises (SMEs) Bother with a Health and Wellbeing Strategy? UK Healthzone: London, UK, 2009. [Google Scholar]
- Vicente-Herrero, M.T.; Delgado-Bueno, S.; Bandrés-Moyá, F.; Capdevilla-García, L. Valoración del dolor. Revisión comparativa de escalas y cuestionarios. Assessment of pain. Comparative review of scales and questionnaires. Rev. De La Soc. Esp. Del Dolor 2018, 25, 228–236. [Google Scholar] [CrossRef]
- Toohey, K.; Pumpa, K.; McKune, A.; Cooke, J.; DuBose, K.D.; Yip, D.; Craft, P.; Semple, S. Does low volume high-intensity interval training elicit superior benefits to continuous low to moderate-intensity training in cancer survivors? World J. Clin. Oncol. 2018, 9, 1–12. [Google Scholar] [CrossRef]
- Podnar, H.; Novak, D.; Radman, I. Effects of a 5-minute classroom-based physical activity on on-task behaviour and physical activity levels. Kinesiology 2018, 50, 251–259. [Google Scholar] [CrossRef]
- Andersen, L.L.; Saervoll, C.A.; Mortensen, O.S.; Poulsen, O.M.; Hannerz, H.; Zebis, M.K. Effectiveness of small daily amounts of progressive resistance training for frequent neck/shoulder pain: Randomised controlled trial. Pain 2011, 152, 440–446. [Google Scholar] [CrossRef]
- Andersen, C.H.; Andersen, L.L.; Gram, B.; Pedersen, M.T.; Mortensen, O.S.; Zebis, M.K.; Sjøgaard, G. Influence of frequency and duration of strength training for effective management of neck and shoulder pain: A randomised controlled trial. Br. J. Sports Med. 2012, 46, 1004–1010. [Google Scholar] [CrossRef] [Green Version]
- Davenport, L.J.; Allisey, A.F.; Page, K.M.; LaMontagne, A.D.; Reavley, N.J. How can organisations help employees thrive? The development of guidelines for promoting positive mental health at work. Int. J. Workplace Health 2016, 9, 411–427. [Google Scholar] [CrossRef]
- Hood, M.S.; Little, J.P.; Tarnopolsky, M.A.; Myslik, F.; Gibala, M.J. Low-volume interval training improves muscle oxidative capacity in sedentary adults. Med. Sci. Sports Exerc. 2011, 43, 1849–1856. [Google Scholar] [CrossRef]
- Nybo, L.; Sundstrup, E.; Jakobsen, M.D.; Mohr, M.; Hornstrup, T.; Simonsen, L.; Bulow, J.; Randers, M.B.; Nielsen, J.J.; Aagaard, P.; et al. High-intensity training versus traditional exercise interventions for promoting health. Med. Sci. Sports Exerc. 2010, 42, 1951–1958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wisloff, U.; Stoylen, A.; Loennechen, J.P.; Bruvold, M.; Rognmo, O.; Haram, P.M.; Tjonna, A.E.; Helgerud, J.; Slordahl, S.A.; Lee, S.J.; et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation 2007, 115, 30863094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Losina, E.; Smith, S.R.; Usiskin, I.M.; Klara, K.M.; Michl, G.L.; Deshpande, B.R.; Yang, H.Y.; Smith, K.C.; Collins, J.E.; Katz, J.N. Implementation of a workplace intervention using financial rewards to promote adherence to physical activity guidelines: A feasibility study. BMC Public Health 2017, 17, 921–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nurminen, E.; Malmivaara, A.; Ilmarinen, J.; Ylostalo, P.; Mutanen, P.; Ahonen, G.; Aro, T. Effectiveness of a worksite exercise program with respect to perceived work ability and sick leaves among women with physical work. Scand. J. Work Environ. Health 2002, 28, 85–93. [Google Scholar] [CrossRef] [Green Version]
- Díaz-Benito, V.J.; Vanderhaegen, F.; Barriopedro, M.J. Physical activity and health promotion programs in the workplace: A meta-analysis of effectiveness in European organizations. J. Workplace Behav. Health 2020, 35, 232–255. [Google Scholar] [CrossRef]
- Atlantis, E.; Chow, C.M.; Kirby, A.; Fiatarone, M.A. Worksite intervention effects on physical health: A randomized controlled trial. Health Promot. Int. 2006, 21, 191–200. [Google Scholar] [CrossRef] [Green Version]
- Biber, D.D.; Ellis, R.; Rice, K. Self-compassion training within a workplace physical activity program: A pilot study. Work 2021, 68, 1059–1067. [Google Scholar] [CrossRef]
- Van Eerd, D.; Munhall, C.; Irvin, E.; Rempel, D.; Brewer, S.; van der Beek, A.J.; Dennerlein, J.T.; Tullar, J.; Skivington, K.; Pinion, C.; et al. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: An update of the evidence. Occup. Environ. Med. 2016, 73, 62–70. [Google Scholar] [CrossRef]
- Silverstein, B.; Clark, R. Interventions to reduce work-related musculoskeletal disorders. J. Electromyogr. Kinesiol. 2004, 14, 135–152. [Google Scholar] [CrossRef]
- van Eerd, D.; Cole, D.; Irvin, E.; Mahood, Q.; Keown, K.; Theberge, N.; Village, J.; St. Vincent, M.; Cullen, K. Process and implementation of participatory ergonomic interventions: A systematic review. Ergonomics 2010, 53, 1153–1166. [Google Scholar] [CrossRef]
- Warburton, D.E.; Bredin, S.S.; Charlesworth, S.A.; Foulds, H.J.; McKenzie, D.C.; Shephard, R.J. Evidence-based risk recommendations for best practices in the training of qualified exercise professionals working with clinical populations. Appl. Physiol. Nutr. Metab. 2011, 36, 232–265. [Google Scholar] [CrossRef] [PubMed]
- Burke, S.M.; Carron, A.V.; Eys, M.A.; Ntoumanis, N.; Estabrooks, P.A. Group versus individual approach? A meta-analysis of the effectiveness of interventions to promote physical activity. Sport Exerc. Psychol. Rev. 2006, 2, 19–35. [Google Scholar]
- Zebis, M.K.; Andersen, L.L.; Pedersen, M.T.; Mortensen, P.; Andersen, C.H.; Pedersen, M.M.; Boysen, M.; Roessler, K.K.; Hannerz, H.; Mortensen, O.S.; et al. Implementation of neck/shoulder exercises for pain relief among industrial workers: A randomized controlled trial. BMC Musculoskelet. Disord. 2011, 12, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christensen, J.R.; Overgaard, K.; Hansen, K.; Søgaard, K.; Holtermann, A. Effects on presenteeism and absenteeism from a 1-year workplace randomized controlled trial among health care workers. J. Occup. Environ. Med. 2013, 55, 1186–1190. [Google Scholar] [CrossRef]
- Sjøgaard, G.; Christensen, J.R.; Justesen, J.B.; Murray, M.; Dalager, T.; Fredslund, G.H.; Søgaard, K. Exercise is more than medicine: The working age population’s well-being and productivity. J. Sport Health Sci. 2016, 5, 159–165. [Google Scholar] [CrossRef] [Green Version]
- de Sousa, C.S.; de Jesus, F.L.A.; Machado, M.B.; Ferreira, G.; Ayres, I.G.T.; de Aquino, L.M.; Fukuda, T.Y.; Gomes-Neto, M. Lower limb muscle strength in patients with low back pain: A systematic review and meta-analysis. J. Musculoskelet. Neuronal Interact. 2019, 19, 69–78. [Google Scholar]
- Barros dos Santos, A.O.; Pinto de Castro, J.B.; Lima, V.P.; da Silva, E.B.; de Souza Vale, R.G. Effects of physical exercise on low back pain and cortisol levels: A systematic review with meta-analysis of randomized controlled trials. Pain Manag. 2021, 11, 49–57. [Google Scholar] [CrossRef]
- Ferro, K.; Lenoir, D.; dos Santos, Y.R.; Jandre, F.J.; Nunes, C.M.; Meeus, M. Prescription of exercises for the treatment of chronic pain along the continuum of nociplastic pain: A systematic review with meta-analysis. Eur. J. Pain 2021, 25, 51–70. [Google Scholar] [CrossRef]
- Lazaridou, A.; Martel, M.O.; Cornelius, M.; Franceschelli, O.; Campbell, C.; Smith, M.; Haythornthwaite, J.A.; Wright, J.R.; Edwards, R.R. The association between daily physical activity and pain among patients with knee osteoarthritis: The moderating role of pain catastrophizing. Pain Med. 2019, 20, 916–924. [Google Scholar] [CrossRef]
- Murray, C.J.; Barber, R.M.; Foreman, K.J.; Ozgoren, A.A.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Abraham, J.P.; Abubakar, I.; Abu-Raddad, L.J.; et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: Quantifying the epidemiological transition. Lancet 2015, 386, 2145–2191. [Google Scholar] [CrossRef] [Green Version]
- Shariat, A.; Lam, E.T.; Kargarfard, M.; Tamrin, S.B.; Danaee, M. The application of a feasible exercise training program in the office setting. Work 2017, 56, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Fernández, P.; Díaz, P. Significancia estadística y relevancia clínica. Statistical significance and clinical relevance. Cad. Aten. Primaria 2000, 8, 191–195. [Google Scholar]
- Castillo, M.S.; Anglada, R.A.; Maymó, I.L.; Bassols, A.R.; Gil, M. Estudio epidemiológico de la lumbalgia. Análisis de factores predictivos de incapacidad. Rehabilitación 2003, 37, 3–10. [Google Scholar] [CrossRef]
| Mcnemar Test | Wilcoxon Signed Rank Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Anatomical Area | M (SD) Pre | M (SD) Post | Diff. | p Value | n | Mdn Pre | Mdn Post | z | p | Effect Size |
| Trunk | 2.54 (1.15) | 2.09 (1.22) | 0.45 | 0.000 | 160 | 13 | 9 | −5.34 | 0.000 | 0.42 |
| Lumbar | 3.18 (2.91) | 2.75 (2.44) | 0.43 | 0.410 | 104 | 5.5 | 4 | −1.76 | 0.079 | 0.17 |
| Dorsal | 2.19 (2.55) | 1.83 (1.90) | 0.36 | 1.000 | 57 | 6 | 3 | −2.00 | 0.045 | 0.26 |
| Cervical | 3.87 (3.12) | 2.73 (2.40) | 1.14 | 0.112 | 110 | 7 | 3 | −4.96 | 0.000 | 0.47 |
| Right shoulder | 1.97 (2.30) | 1.76 (1.89) | 0.21 | 1.000 | 47 | 6 | 3 | −1.27 | 0.205 | 0.19 |
| Left Shoulder | 1.51 (1.73) | 1.28 (1.31) | 0.23 | 0.109 | 18 | 6.5 | 3 | −1.97 | 0.049 | 0.46 |
| Limbs | 1.35 (0.62) | 1.28 (0.52) | 0.07 | 0.683 | 97 | 16 | 14 | −1.52 | 0.128 | 0.15 |
| Right ankle | 1.12 (0.90) | 1.10 (0.59) | 0.02 | 0.727 | 9 | 1 | 3 | 0.00 | 1.000 | 0.00 |
| Left ankle | 1.06 (0.69) | 1.05 (0.46) | 0.01 | 1.000 | 4 | 2.5 | 3 | 0.00 | 1.000 | 0.00 |
| Right knee | 1.45 (1.59) | 1.51 (1.56) | −0.06 | 0.345 | 32 | 1 | 4 | −0.45 | 0.653 | 0.08 |
| Left knee | 1.43 (1.52) | 1.28 (1.22) | 0.15 | 0.454 | 21 | 6 | 3 | −1.20 | 0.231 | 0.26 |
| Right hip | 1.24 (1.17) | 1.32 (1.13) | −0.08 | 0.077 | 20 | 1 | 4 | −0.69 | 0.492 | 0.15 |
| Left hip | 1.14 (0.96) | 1.09 (0.60) | 0.05 | 1.000 | 7 | 6 | 3 | −1.03 | 0.302 | 0.39 |
| Right elbow | 1.92 (2.15) | 1.74 (1.76) | 0.18 | 0.845 | 46 | 6 | 4 | −1.38 | 0.167 | 0.20 |
| Left elbow | 1.46 (1.55) | 1.38 (1.36) | 0.08 | 1.000 | 25 | 6 | 3 | −0.54 | 0.591 | 0.11 |
| Right wrist | 1.45 (1.58) | 1.28 (1.13) | 0.17 | 0.774 | 21 | 6 | 3 | −1.77 | 0.077 | 0.39 |
| Left wrist | 1.31 (1.30) | 1.12 (0.79) | 0.19 | 0.070 | 12 | 6.5 | 1 | −1.93 | 0.054 | 0.56 |
| Total Pain | 1.75 (0.58) | 1.54 (0.64) | 0.21 | 0.000 | 170 | 26 | 21 | −4.74 | 0.000 | 0.36 |
| McNemar Test | Wilcoxon Signed Rank Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Centre (n) | M (SD) Pre | M (SD) Post | Diff. | p Value | n | Mdn Pre | Mdn Post | z | p-Value | Effect Size |
| 1 (31) | 1.37 (0.36) | 1.20 (0.22) | 0.17 | 0.500 | 22 | 21.5 | 19 | −2.76 | 0.006 | 0.59 |
| 2 (39) | 1.90 (0.63) | 1.67 (0.54) | 0.23 | 0.063 | 39 | 27 | 25 | −2.61 | 0.009 | 0.42 |
| 3 (47) | 1.75 (0.43) | 1.27 (0.38) | 0.48 | 0.000 | 43 | 27 | 17 | −4.89 | 0.000 | 0.75 |
| 4 (69) | 1.85 (0.66) | 1.83 (0.82) | 0.03 | 0.549 | 66 | 27 | 25 | −0.27 | 0.791 | 0.03 |
| McNemar Test | Wilcoxon Signed Rank Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Days of Adherence (n) | M (SD) Pre | M (SD) Post | Diff. | p Value | n | Mdn Pre | Mdn Post | z | p | Effect Size |
| 0–14 (32) | 1.66 (0.55) | 1.72 (0.67) | −0.06 | 1.000 | 29 | 24 | 25 | −0.54 | 0.588 | 0.10 |
| 15–30 (154) | 1.77 (0.59) | 1.51 (0.63) | 0.26 | 0.000 | 141 | 26 | 20 | −5.41 | 0.000 | 0.46 |
| Total Pre Pain | Total Post Pain | Active | Adherence to the Program | |
|---|---|---|---|---|
| Total Pre pain | ||||
| Total Post pain | τb = 0.325 p = 0.000 | |||
| Active | τb = 0.150 p = 0.014 | τb = 0.148 p = 0.018 | ||
| Adherence to the program | τb = 0.085 p = 0.167 | τb = 0.238 p = 0.000 | τb = 0.184 p = 0.012 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Río, X.; Sáez, I.; González, J.; Besga, Á.; Santano, E.; Ruiz, N.; Solabarrieta, J.; Coca, A. Effects of a Physical Exercise Intervention on Pain in Workplaces: A Case Study. Int. J. Environ. Res. Public Health 2022, 19, 1331. https://doi.org/10.3390/ijerph19031331
Río X, Sáez I, González J, Besga Á, Santano E, Ruiz N, Solabarrieta J, Coca A. Effects of a Physical Exercise Intervention on Pain in Workplaces: A Case Study. International Journal of Environmental Research and Public Health. 2022; 19(3):1331. https://doi.org/10.3390/ijerph19031331
Chicago/Turabian StyleRío, Xabier, Iker Sáez, Javier González, Ángel Besga, Eneko Santano, Natxo Ruiz, Josu Solabarrieta, and Aitor Coca. 2022. "Effects of a Physical Exercise Intervention on Pain in Workplaces: A Case Study" International Journal of Environmental Research and Public Health 19, no. 3: 1331. https://doi.org/10.3390/ijerph19031331
APA StyleRío, X., Sáez, I., González, J., Besga, Á., Santano, E., Ruiz, N., Solabarrieta, J., & Coca, A. (2022). Effects of a Physical Exercise Intervention on Pain in Workplaces: A Case Study. International Journal of Environmental Research and Public Health, 19(3), 1331. https://doi.org/10.3390/ijerph19031331









