Self-Medication Perceptions and Practice of Medical and Pharmacy Students in Serbia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. The Questionnaire
2.3. Data Analysis
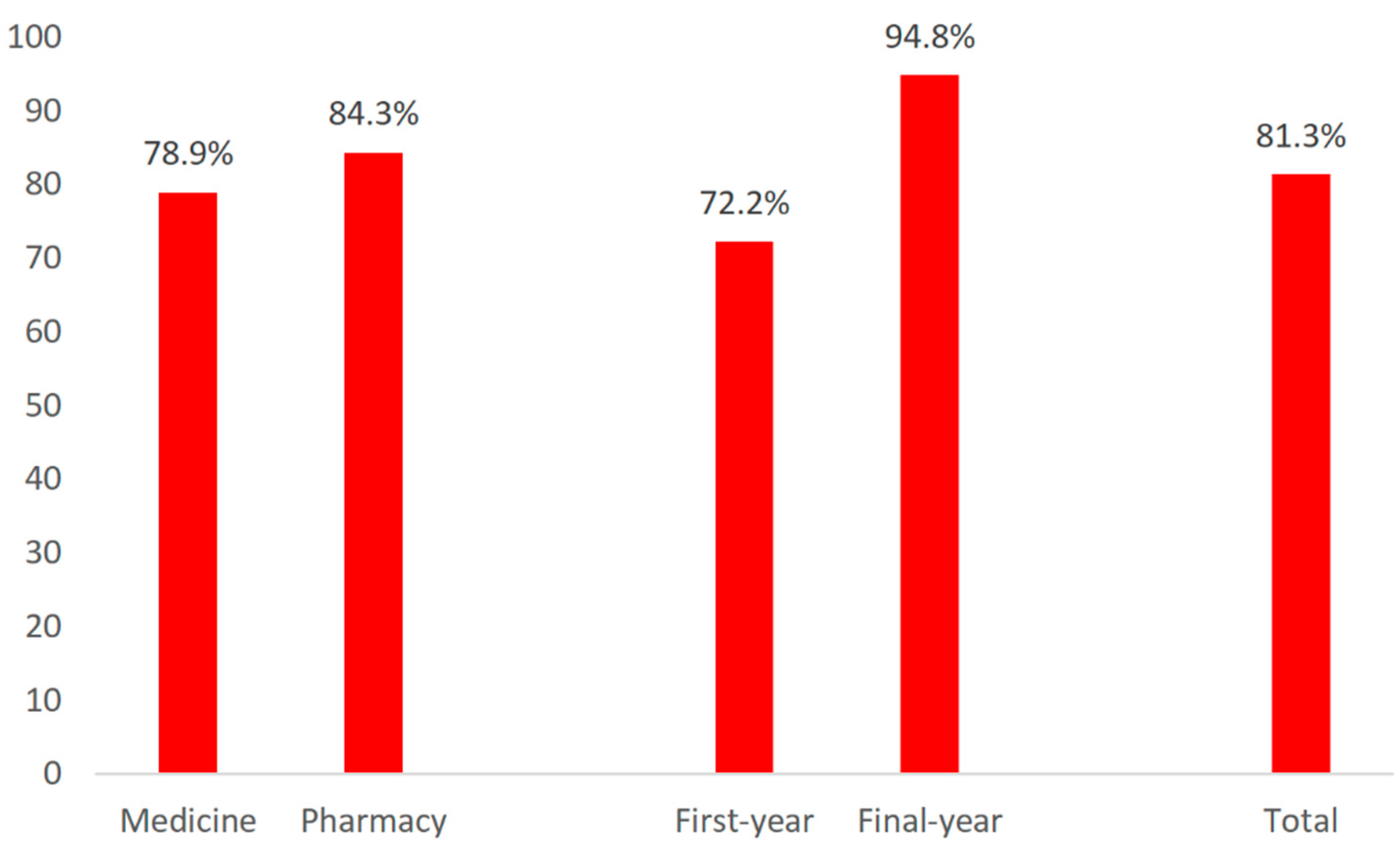
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hughes, C.M.; McElnay, J.C.; Fleming, G.F. Benefits and risks of self-medication. Drug Saf. 2001, 24, 1027–1037. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Role of the Pharmacist in Self-Care and Self-Medication: Report of the 4th WHO Consultative Group on the Role of the Pharmacist, The Hague, The Netherlands, 26–28 August 1998; WHO: Geneva, Switzerland, 1998.
- Horvat, O.J.; Tomas, A.D.; Kusturica, M.M.P.; Savkov, A.V.; Bukumirić, D.U.; Tomić, Z.S.; Sabo, A.J. Is the level of knowledge a predictor of rational antibiotic use in Serbia? PLoS ONE 2017, 12, e0180799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hughes, C.M. Monitoring self-medication. Expert Opin. Drug Saf. 2003, 2, 1–5. [Google Scholar] [CrossRef]
- Ekor, M. The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Front. Neurol. 2014, 4, 177. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Onakpoya, I.J.; Posadzki, P.; Eddouks, M. The safety of herbal medicine: From prejudice to evidence. Evid.-Based Complement. Altern. Med. 2015, 2015, 316706. [Google Scholar] [CrossRef] [Green Version]
- Raškovic, A.; Cvejic, J.; Stilinovic, N.; Golocorbin-Kon, S.; Vukmirovic, S.; Mimica-Dukic, N.; Mikov, M. Interaction between different extracts of hypericum perforatum L. from serbia and pentobarbital, diazepam and paracetamol. Molecules 2014, 19, 3869–3882. [Google Scholar] [CrossRef] [Green Version]
- Shehnaz, S.I.; Agarwal, A.K.; Khan, N. A systematic review of self-medication practices among adolescents. J. Adolesc. Health 2014, 55, 467–483. [Google Scholar] [CrossRef] [PubMed]
- Noone, J.; Blanchette, C.M. The value of self-medication: Summary of existing evidence. J. Med. Econ. 2018, 21, 201–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albusalih, F.A.; Naqvi, A.A.; Ahmad, R.; Ahmad, N. Prevalence of self-medication among students of pharmacy and medicine colleges of a public sector university in Dammam City, Saudi Arabia. Pharmacy 2017, 5, 51. [Google Scholar] [CrossRef] [Green Version]
- Ruiz, M.E. Risks of self-medication practices. Curr. Drug Saf. 2010, 5, 315–323. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication; WHO: Geneva, Switzerland, 2000.
- Shaghaghi, A.; Asadi, M.; Allahverdipour, H. Predictors of self-medication behavior: A systematic review. Iran. J. Public Health 2014, 43, 136–146. [Google Scholar]
- Galato, D.; Galafassi, L.D.M.; Alano, G.M.; Trauthman, S.C. Responsible self-medication: Review of the process of pharmaceutical attendance. Braz. J. Pharm. Sci. 2009, 45, 625–633. [Google Scholar] [CrossRef] [Green Version]
- Kusturica, M.P.; Tomic, Z.; Bukumiric, Z.; Ninkovic, L.; Tomas, A.; Stilinovic, N.; Sabo, A. Home pharmacies in Serbia: An insight into self-medication practice. Int. J. Clin. Pharm. 2015, 37, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, A.; Bradley, C.; Rochfort, A.; Panagopoulou, E. A review of self-medication in physicians and medical students. Occup. Med. 2011, 61, 490–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- James, H.; Handu, S.S.; Al Khaja, K.A.J.; Otoom, S.; Sequeira, R.P. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med. Princ. Pract. 2006, 15, 270–275. [Google Scholar] [CrossRef]
- Klemenc-Ketis, Z.; Hladnik, Z.; Kersnik, J. Self-medication among healthcare and non-healthcare students at university of Ljubljana, Slovenia. Med. Princ. Pract. 2010, 19, 395–401. [Google Scholar] [CrossRef]
- Lukovic, J.A.; Miletic, V.; Pekmezovic, T.; Trajkovic, G.; Ratkovic, N.; Aleksic, D.; Grgurevic, A. Self-medication practices and risk factors for self-medication among medical students in Belgrade, Serbia. PLoS ONE 2014, 9, e114644. [Google Scholar] [CrossRef] [Green Version]
- Tomas, A.; Kusturica, M.P.; Tomić, Z.; Horvat, O.; Koprivica, D.D.; Bukumirić, D.; Sabo, A. Self-medication with antibiotics in Serbian households: A case for action? Int. J. Clin. Pharm. 2017, 39, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Stojsin, S. Ethnic Diversity of Population in Vojvodina at the Beginning of the 21st Century. Eur. Q. Political Attitudes Ment. 2015, 4, 25. [Google Scholar]
- Scuri, S.; Petrelli, F.; Tanzi, E.; Nguyễn, T.T.C.; Grappasonni, I. European university students of pharmacy: Survey on the use of pharmaceutical drugs. Acta Biomed. 2019, 90, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Zafar, S.N.; Syed, R.; Waqar, S.; Zubairi, A.J.; Vaqar, T.; Shaikh, M.; Yousaf, W.; Shahid, S.; Saleem, S. Self-medication amongst university students of Karachi: Prevalence, knowledge and attitudes. J. Pak. Med. Assoc. 2008, 58, 214–217. [Google Scholar] [PubMed]
- Picking, D.; Younger, N.; Mitchell, S.; Delgoda, R. The prevalence of herbal medicine home use and concomitant use with pharmaceutical medicines in Jamaica. J. Ethnopharmacol. 2011, 137, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Nur, N. Knowledge and behaviours related to herbal remedies: A cross-sectional epidemiological study in adults in Middle Anatolia, Turkey. Health Soc. Care Community 2010, 18, 389–395. [Google Scholar] [CrossRef]
- Barros, A.J.D.; Hirakata, V.N. Alternatives for logistic regression in cross-sectional studies: An empirical comparison of models that directly estimate the prevalence ratio. BMC Med. Res. Methodol. 2003, 3, 21. [Google Scholar] [CrossRef] [Green Version]
- Hughes, K. Odds ratios in cross-sectional studies. Int. J. Epidemiol. 1995, 24, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Brlić, K.Č.; Holcer, N.J.; Sović, S.; Štimac, D. Characteristics of self-medication for pain relief among first-year health care students in Zagreb, Croatia. Psychiatr. Danub. 2014, 26, 459–465. [Google Scholar]
- Alam, N.; Saffoon, N.; Uddin, R. Self-medication among medical and pharmacy students in Bangladesh. BMC Res. Notes 2015, 8, 763. [Google Scholar] [CrossRef] [Green Version]
- Alkhatatbeh, M.J.; Alefan, Q.; Alqudah, M.A.Y. High prevalence of self-medication practices among medical and pharmacy students: A study from Jordan. Int. J. Clin. Pharmacol. Ther. 2016, 54, 390–398. [Google Scholar] [CrossRef]
- Vukanovic, D.; Mrzic, A.; Omerbasic, Z.; Skopljak, E.; Zajimovic, Z.; Zeid, M.; Jusufovic, R.; Catic, T. Self-medication attitude, knowledge, and perception. Value Health 2018, 21, S309. [Google Scholar] [CrossRef] [Green Version]
- Sharif, S.I.; Mohamed Ibrahim, O.H.; Mouslli, L.; Waisi, R. Evaluation of self-medication among pharmacy students. Am. J. Pharmacol. Toxicol. 2012, 7, 135–140. [Google Scholar] [CrossRef] [Green Version]
- Sawalha, A.F.; Sweileh, W.M.; Zyoud, S.H.; Jabi, S.W. Self-therapy practices among university students in Palestine: Focus on herbal remedies. Complementary Ther. Med. 2008, 16, 343–349. [Google Scholar] [CrossRef]
- Shehnaz, S.I.; Khan, N.; Sreedharan, J.; Issa, K.J.; Arifulla, M. Self-medication and related health complaints among expatriate high school students in the United Arab Emirates. Pharm. Pract. 2013, 11, 211–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ibrahim, N.K.; Alamoudi, B.M.; Baamer, W.O.; Al-Raddadi, R.M. Self-medication with analgesics among medical students and interns in King Abdulaziz University, Jeddah, Saudi Arabia. Pak. J. Med. Sci. 2015, 31, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Osemene, K.P.; Lamikanra, A. A study of the prevalence of self-medication practice among university students in southwestern Nigeria. Trop. J. Pharm. Res. 2012, 11, 683–689. [Google Scholar] [CrossRef] [Green Version]
- Corrêa Da Silva, M.G.; Soares, M.C.F.; Muccillo-Baisch, A.L. Self-medication in university students from the city of Rio Grande, Brazil. BMC Public Health 2012, 12, 339. [Google Scholar] [CrossRef] [Green Version]

| Characteristics | Study Program | Study Year | Total n (%) | |||
|---|---|---|---|---|---|---|
| Medicine n (%) | Pharmacy n (%) | First n (%) | Final n (%) | No Answer n (%) | ||
| Gender | ||||||
| Female | 91 (83.5%) | 73 (87.9%) | 91 (84.3%) | 68 (88.3%) | 5 (71.4%) | 164 (84.5%) |
| Male | 18 (16.5%) | 10 (12.0%) | 17 (15.7%) | 9 (11.7%) | 2 (28.6%) | 28 (14.4%) |
| Housing conditions | ||||||
| Living with parents | 42 (38.5%) | 27 (32.5%) | 37 (34.3%) | 29 (37.7%) | 3 (42.9%) | 69 (35.9%) |
| In a student dormitory | 56 (51.4%) | 45 (54.2%) | 57 (52.8%) | 40 (52.0%) | 4 (57.1%) | 101 (52.6%) |
| In a leased apartment | 10 (9.2%) | 11 (13.3%) | 13 (12.0%) | 8 (10.4%) | 0 (0.0%) | 21 (10.9%) |
| No answer | 1 (0.9%) | 0 (0.0%) | 1 (0.9%) | 0 (0.0%) | 0 (0.0%) | 1 (0.5%) |
| Cigarette consumption | ||||||
| Yes | 17 (15.6%) | 17 (20.5%) | 13 (12.0%) | 19 (24.7%) | 2 (28.6%) | 34 (17.7%) |
| No | 92 (84.4%) | 66 (79.5%) | 95 (88.0%) | 58 (75.3%) | 5 (71.4%) | 158 (82.3%) |
| Alcohol consumption | ||||||
| Yes | 4 (3.7%) | 12 (14.5%) | 3 (2.8%) | 13 (16.9%) | 0 (0.0%) | 16 (8.3%) |
| No | 105 (96.3%) | 71 (85.5%) | 105 (97.2%) | 64 (83.1%) | 7 (100.0%) | 176 (90.7%) |
| Chosen general practitioner | ||||||
| Yes | 87 (79.8%) | 60 (72.3%) | 86 (79.6%) | 58 (75.3%) | 3 (42.9%) | 147 (76.6%) |
| No | 22 (20.2%) | 23(27.7%) | 22 (20.4%) | 19 (24.7%) | 4 (57.1%) | 45 (23.4%) |
| Chronic illness | ||||||
| Yes | 11 (10.1%) | 8 (9.6%) | 10 (9.3%) | 8 (10.4%) | 1 (14.3%) | 19 (9.9%) |
| No | 98 (89.9%) | 75 (90.4%) | 98 (90.7%) | 69 (89.6%) | 6 (85.7%) | 173 (90.1%) |
| Taking medication for chronic illnesses | ||||||
| Yes | 7 (6.4%) | 6 (7.2%) | 4 (3.7%) | 8 (10.4%) | 1 (14.3%) | 13 (6.8%) |
| No | 101 (92.7%) | 71 (85.6%) | 101 (93.5%) | 66 (85.7%) | 5 (71.4%) | 172 (89.6%) |
| No answer | 1 (0.9%) | 6 (7.2%) | 3 (2.8%) | 3 (3.9%) | 1 (14.3%) | 7 (3.7%) |
| Total | 109 (100.0%) | 83 (100.0%) | 108 (100.0%) | 77 (100.0%) | 7 (100.0%) | 192 (100.0%) |
| Attitudes about Self-Medication | Study Program | Study Year * | Total n (%) | ||
|---|---|---|---|---|---|
| Medicine n (%) | Pharmacy n (%) | First n (%) | Final n (%) | ||
| Reasons for practicing self-medication | |||||
| Lack of free time | 18 (20.9%) | 8 (11.4%) | 8 (10.3%) | 17 (23.3%) | 26 (16.6%) |
| Mild symptoms (perceived as unnecessary for a visit to a doctor) | 55 (64.0%) | 53 (75.7%) | 55 (70.5%) | 50 (68.5%) | 108 (69.2%) |
| Distance to a doctor’s office | 6 (7.0%) | 1 (1.4%) | 0 (0.0%) | 6 (8.2%) | 7 (4.48%) |
| Having a positive experience with the same medicine | 36 (41.9%) | 30 (42.9%) | 34 (43.6%) | 31 (42.5%) | 66 (42.3%) |
| Other | 1 (1.2%) | 2 (2.9%) | 0 (0.0%) | 2 (2.7%) | 1 (0.6%) |
| Reasons against practicing self-medication | |||||
| There was no need | 18 (78.3%) | 7 (53.8%) | 21 (70.0%) | 3 (75.0%) | 26 (70.3%) |
| Due to safety concerns | 5 (21.7%) | 6 (46.2%) | 9 (30.0%) | 1 (25.0%) | 11 (29.7%) |
| Sources of Medicines and Information for Self-Medication | Study Program | p-Value | Study Year * | p-Value | Total n (%) | ||
|---|---|---|---|---|---|---|---|
| Medicine n (%) | Pharmacy n (%) | First n (%) | Final n (%) | ||||
| Sources of medicines | |||||||
| Pharmacy | 78 (90.7%) | 65 (92.9%) | p = 0.175 | 72 (92.3%) | 68 (93.2%) | p = 0.385 | 143 (91.7%) |
| Relatives, friends, neighbors | 8 (9.3%) | 3 (4.3%) | 4 (5.1%) | 7 (9.6%) | 11 (7.1%) | ||
| Traditional healer, homeopath | 1 (1.2%) | 1 (1.4%) | 1 (1.3%) | 1 (1.4%) | 2 (1.3%) | ||
| Health food stores, herbal pharmacies | 8 (9.3%) | 6 (8.6%) | 6 (7.7%) | 7 (9.6%) | 14 (9.0%) | ||
| Home pharmacies | 43 (50.0%) | 26 (37.1%) | 32 (41.0%) | 35 (47.9%) | 69 (44.2%) | ||
| Sources of information on desired drug | |||||||
| Mass media (TV, radio) | 1 (1.2%) | 3 (4.3%) | p = 0.486 | 2 (2.6%) | 2 (2.7%) | p < 0.01 | 4 (2.6%) |
| Internet | 16 (18.6%) | 9 (12.9%) | 14 (17.9%) | 9 (12.3%) | 25 (16.0%) | ||
| Relatives, friends, neighbors | 24 (27.9%) | 14 (20.0%) | 23 (29.5%) | 14 (19.2%) | 38 (24.4%) | ||
| Pharmacist | 27 (31.4%) | 31 (44.3%) | 34 (43.6%) | 23 (31.5%) | 58 (37.2%) | ||
| Medical doctor (from previous visits) | 46 (53.5%) | 33 (47.1%) | 43 (55.1%) | 34 (46.6%) | 79 (50.6%) | ||
| Professional literature (class books) | 34 (41.9%) | 20 (28.6%) | 10 (12.8%) | 43 (58.9%) | 54 (34.6%) | ||
| Claims about Conventional and Herbal Medication | Study Program | p-Value | Study Year * | p-Value | Total n (%) | ||
|---|---|---|---|---|---|---|---|
| Medicine n (%) | Pharmacy n (%) | First n (%) | Final n (%) | ||||
| Concomitant use of conventional drugs and herbal preparations (in previous 12 months) | |||||||
| Yes | 44 (40.4%) | 29 (34.9%) | p = 0.200 | 38 (35.2%) | 32 (41.6%) | p = 0.669 | 73 (38.0%) |
| No | 41 (37.6%) | 41 (49.4%) | 39 (36.1%) | 41 (53.3%) | 82 (42.7%) | ||
| No answer | 24 (22.0%) | 13 (15.7%) | 31 (28.7%) | 4 (5.2%) | 37 (19.3%) | ||
| Reasons for their concomitant use of conventional drugs and herbal preparations ** | |||||||
| They’re used for different indications | 1 (2.3%) | 6 (20.7%) | p = 0.004 | 3 (7.9%) | 3 (9.4%) | p = 0.364 | 7 (9.6%) |
| I think they act better in combination | 12 (27.3%) | 5 (17.2%) | 7 (18.4%) | 10 (31.3%) | 17 (23.3%) | ||
| I do not think it is harmful | 30 (68.2%) | 13 (44.8%) | 27 (71.1%) | 14 (43.8%) | 43 (58.9%) | ||
| Other | 1 (2.3%) | 1 (3.4%) | 0 (0.0%) | 2 (6.3%) | 2 (2.7%) | ||
| Preference for one option to continue the therapy (if required) | |||||||
| Conventional drug | 71 (65.1%) | 45 (54.2%) | p = 0.009 | 51 (47.2%) | 62 (80.5%) | p = 0.045 | 116 (60.4%) |
| Herbal drug/preparation | 15 (13.8%) | 25 (30.1%) | 27 (25.0%) | 11 (14.3%) | 40 (20.8%) | ||
| No answer | 23 (21.1%) | 13 (15.7%) | 30 (27.8%) | 4 (5.2%) | 36 (18.8%) | ||
| Attitudes on the efficacy of herbal drugs | |||||||
| Herbal drugs are more efficient | 4 (3.7%) | 6 (7.2%) | p = 0.45 | 8 (7.4%) | 1 (1.3%) | p = 0.001 | 10 (5.2%) |
| Conventional drugs are more efficient | 39 (35.8%) | 32 (38.6%) | 25 (23.2%) | 44 (57.1%) | 71 (37.0%) | ||
| They are equally efficient | 14 (12.8%) | 15 (18.1%) | 15 (13.9%) | 14 (18.2%) | 29 (15.1%) | ||
| Not sure | 29 (26.6%) | 17 (20.5%) | 30 (27.8%) | 14 (18.2%) | 46 (24.0%) | ||
| No answer | 23 (21.1%) | 13 (15.7%) | 30 (27.8%) | 4 (5.2%) | 36 (18.8%) | ||
| Attitudes on the safety of herbal drugs | |||||||
| Herbal drugs have less adverse effects | 35 (31.8%) | 30 (36.6%) | p = 0.001 | 41 (37.6%) | 22 (28.9%) | p = 0.004 | 66 (34.4%) |
| Conventional drugs have less adverse effects | 15 (13.6%) | 17 (20.7%) | 9 (8.3%) | 22 (28.9%) | 32 (16.7%) | ||
| They are equally safe | 10 (10.0%) | 15 (18.3%) | 8 (7.3%) | 17 (22.4%) | 25 (13.0%) | ||
| Not sure | 26 (23.6%) | 7 (8.5%) | 20 (18.3%) | 12 (15.9%) | 33 (17.2%) | ||
| No answer | 23 (20.9%) | 13 (15.9%) | 31 (28.4%) | 3 (3.9%) | 36 (18.8%) | ||
| Did the pharmacist warn you about the risks of concomitant use of conventional and herbal drugs? *** | |||||||
| Yes | 9 (37.5%) | 12 (60.0%) | p = 0.839 | 12 (48.0%) | 9 (52.9%) | p = 0.734 | 21 (47.7%) |
| No | 15 (62.5%) | 8 (40.0%) | 13 (52.0%) | 8 (47.1%) | 23 (52.3%) | ||
| Independent Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| PR (95% CI) | p-Value | PR (95% CI) | p-Value | |
| Gender (female/male) | 0.94 (0.79–1.11) | 0.465 | ||
| Study program (pharmacy/medicine) | 1.07 (0.94–1.22) | 0.330 | ||
| Study year (final/first) | 1.31 (1.16–1.49) | <0.001 | 1.28 (1.13–1.44) | <0.001 |
| Housing conditions Living with parents In leased apartment/room In a student dormitory | reference 1.23 (1.04–1.45) 1.27 (1.04–1.56) | 0.017 0.021 | reference 1.25 (1.06–1.47) 1.33 (1.09–1.64) | 0.008 0.006 |
| Cigarette consumption | 1.25 (1.13–1.38) | <0.001 | 1.20 (1.08–1.33) | 0.001 |
| Alcohol consumption | 1.26 (1.17–1.36) | <0.001 | ||
| Chosen general practitioner | 1.02 (0.87–1.20) | 0.810 | ||
| Chronic illness | 1.11 (0.94–1.32) | 0.217 | ||
| Taking medication for chronic illnesses | 1.04 (0.82–1.33) | 0.754 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomas Petrović, A.; Pavlović, N.; Stilinović, N.; Lalović, N.; Paut Kusturica, M.; Dugandžija, T.; Zaklan, D.; Horvat, O. Self-Medication Perceptions and Practice of Medical and Pharmacy Students in Serbia. Int. J. Environ. Res. Public Health 2022, 19, 1193. https://doi.org/10.3390/ijerph19031193
Tomas Petrović A, Pavlović N, Stilinović N, Lalović N, Paut Kusturica M, Dugandžija T, Zaklan D, Horvat O. Self-Medication Perceptions and Practice of Medical and Pharmacy Students in Serbia. International Journal of Environmental Research and Public Health. 2022; 19(3):1193. https://doi.org/10.3390/ijerph19031193
Chicago/Turabian StyleTomas Petrović, Ana, Nebojša Pavlović, Nebojša Stilinović, Nikola Lalović, Milica Paut Kusturica, Tihomir Dugandžija, Dragana Zaklan, and Olga Horvat. 2022. "Self-Medication Perceptions and Practice of Medical and Pharmacy Students in Serbia" International Journal of Environmental Research and Public Health 19, no. 3: 1193. https://doi.org/10.3390/ijerph19031193
APA StyleTomas Petrović, A., Pavlović, N., Stilinović, N., Lalović, N., Paut Kusturica, M., Dugandžija, T., Zaklan, D., & Horvat, O. (2022). Self-Medication Perceptions and Practice of Medical and Pharmacy Students in Serbia. International Journal of Environmental Research and Public Health, 19(3), 1193. https://doi.org/10.3390/ijerph19031193








