Occupational Exposure to Wood Dust and the Burden of Nasopharynx and Sinonasal Cancer in Canada
Abstract
:1. Introduction
2. Materials and Methods
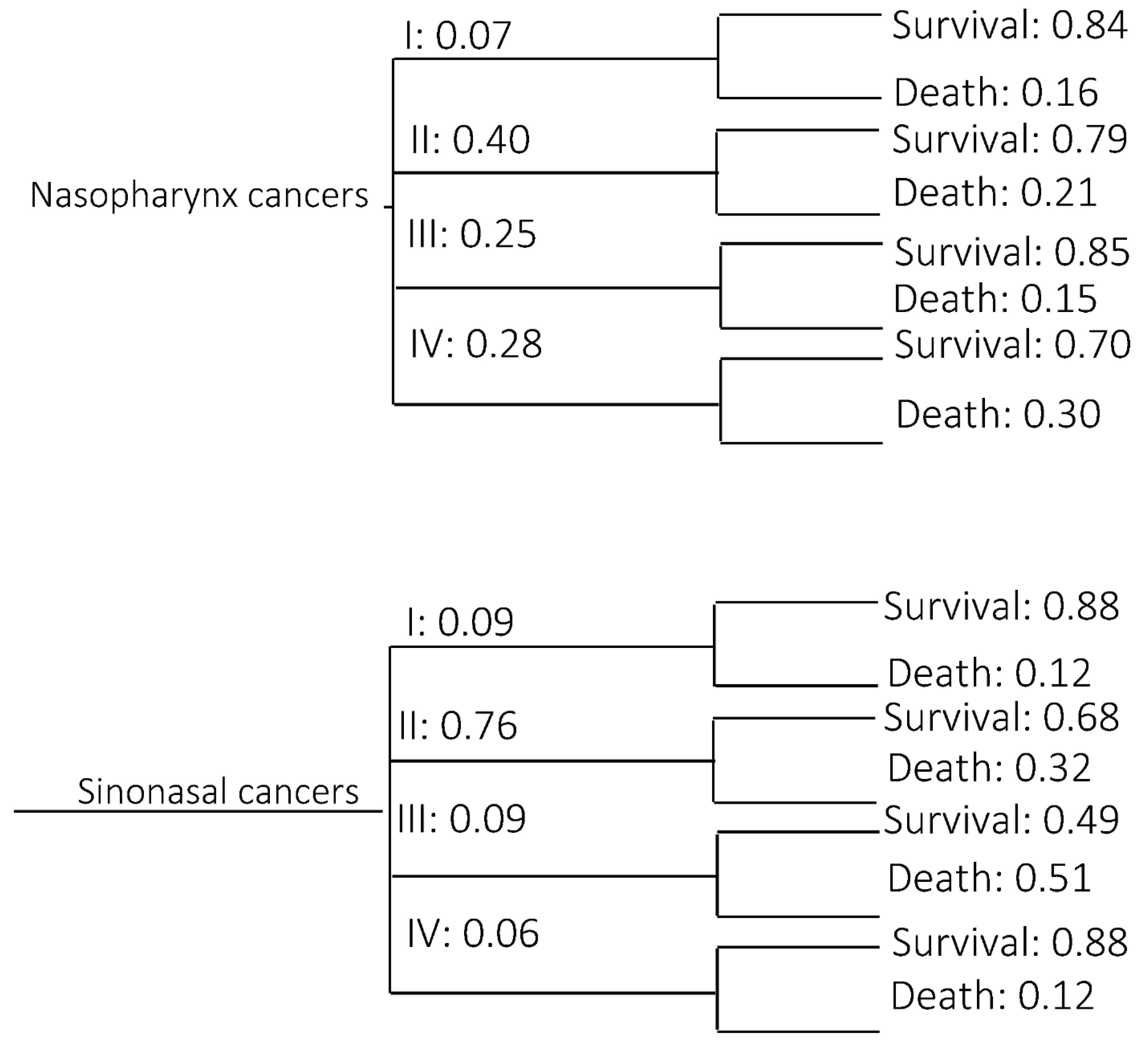
2.1. Incidence of Cancer among Exposed Workers
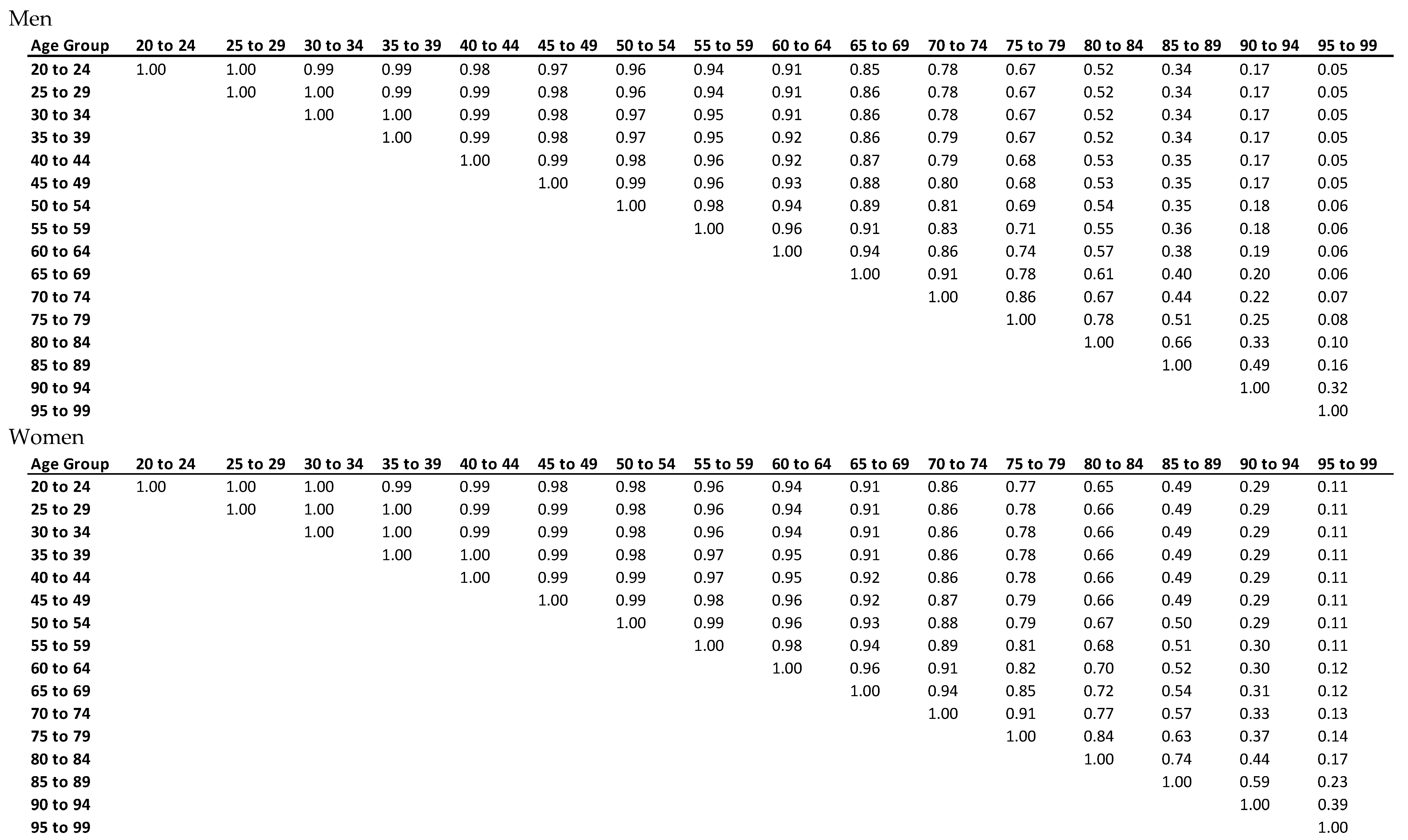
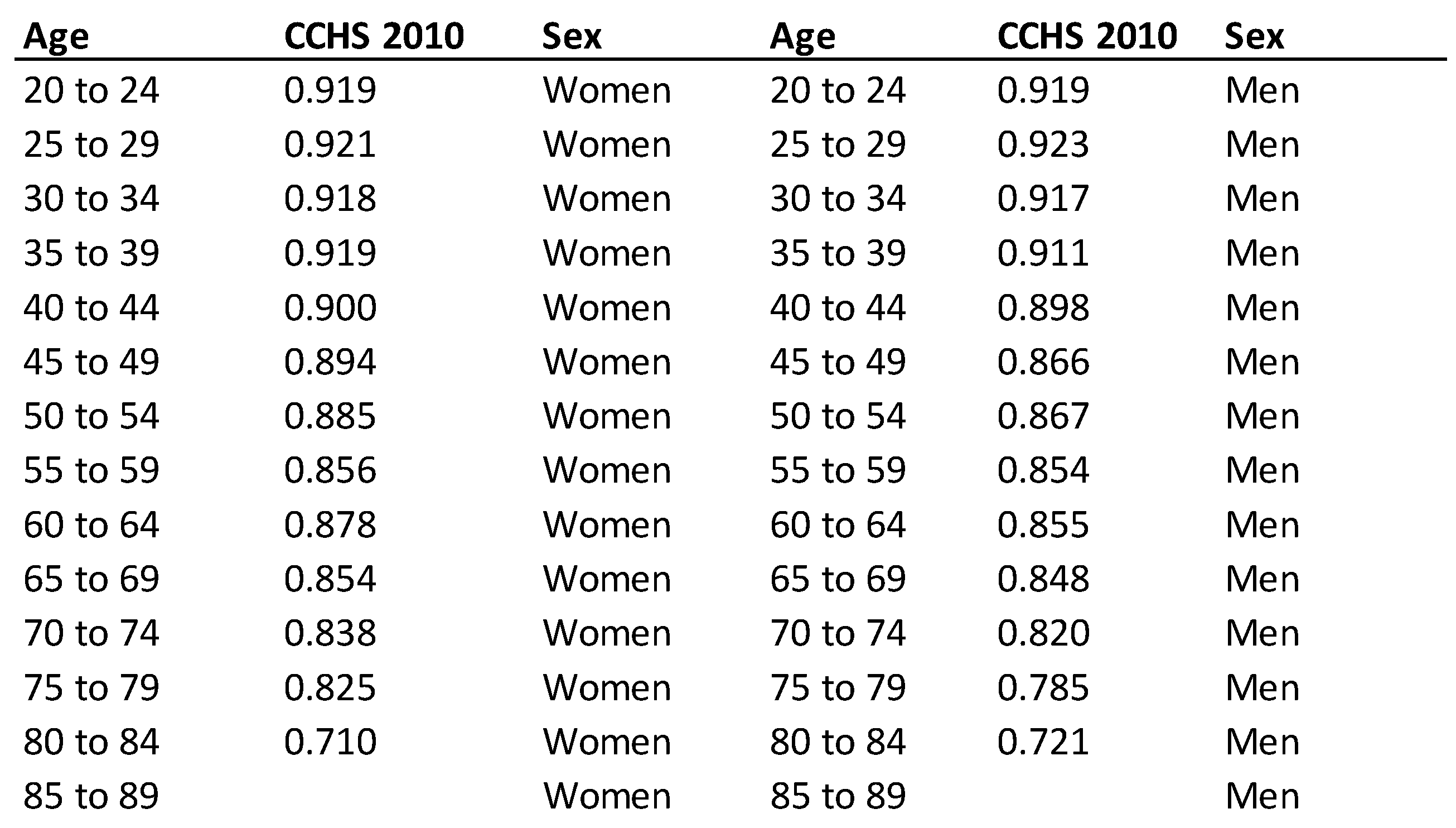
2.2. Economic Burden Modelling
2.3. Sensitivity Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Items a | Costs b |
|---|---|
| Head and neck consultation (otolaryngology) | CAD 49 |
| Baseline imaging of primary and neck (PET/CT) | CAD 238 |
| Thyroid stimulating hormone screening | CAD 34 |
| Speech/swallowing assessment | CAD 41 |
| Rehabilitation counselling | CAD 301 |
| Hearing evaluation and rehabilitation counselling | CAD 146 |
| Nutritional status counselling | CAD 150 |
| Routine hospital-based dental follow-up and evaluation | CAD 65 |
| Total | CAD 1497 |
Appendix B
Appendix C

Appendix D
Appendix E
References
- International Agency for Research on Cancer. Wood Dust and Formaldehyde; IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans: Lyon, France, 1995; Volume 62. [Google Scholar]
- Li, J.-X.; Lu, T.-X.; Huang, Y.; Han, F. Clinical Characteristics of Recurrent Nasopharyngeal Carcinoma in High-Incidence Area. Sci. World J. 2012, 2012, 719754. [Google Scholar] [CrossRef] [Green Version]
- Binazzi, A.; Ferrante, P.; Marinaccio, A. Occupational exposure and sinonasal cancer: A systematic review and meta-analysis. BMC Cancer 2015, 15, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Jacobsen, G.; Schaumburg, I.; Sigsgaard, T.; Schlunssen, V. Non-malignant respiratory diseases and occupational exposure to wood dust. Part II. Dry wood industry. Ann. Agr. Env. Med. 2010, 17, 29–44. [Google Scholar]
- Estlander, T.; Jolanki, R.; Alanko, K.; Kanerva, L. Occupational allergic contact dermatitis caused by wood dusts. Contact Dermat. 2001, 44, 213–217. [Google Scholar] [CrossRef]
- Puntarić, D.; Kos, A.; Smit, Z.; Zecić, Z.; Sega, K.; Beljo-Lucić, R.; Horvat, D.; Bosnir, J. Wood dust exposure in wood industry and forestry. Coll. Antropol. 2005, 29, 207–211. [Google Scholar] [PubMed]
- Natural Resources Canada. How Does the Forest Industry Contribute to Canada’s Economy? 2017. Available online: https://www.nrcan.gc.ca/our-natural-resources/forests-and-forestry/state-canadas-forests-report/forest-industry-contribute/16517 (accessed on 6 June 2018).
- Teschke, K.; Hertzman, C.; Morrison, B. Level and distribution of employee exposures to total and respirable wood dust in two Canadian sawmills. Am. Ind. Hyg. Assoc. J. 1994, 55, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Vallières, E.; Pintos, J.; Parent, M.-E.; Siemiatycki, J. Occupational exposure to wood dust and risk of lung cancer in two population-based case–control studies in Montreal, Canada. Environ. Health 2015, 14, 1. [Google Scholar] [CrossRef] [Green Version]
- Tompa, E.; Culyer, A.J.; Dolinschi, R. (Eds.) . Economic Evaluation of Interventions for Occupational Health and Safety: Developing Good Practice; Oxford University Press: Oxford, UK, 2008. [Google Scholar]
- Orenstein, M.R.; Dall, T.; Curley, P.; Chen, J.; Tamburrini, A.L.; Petersen, J. The Economic Burden of Occupational Cancers in Alberta. Calgary: Alberta Health Services. Health Protection, Environment Unit. 2010. Available online: https://www.albertahealthservices.ca/poph/hi-poph-surv-phids-economic-burden-occup-cancer-2010.pdf (accessed on 30 November 2021).
- Jacobson, J.J.; Epstein, J.B.; Eichmiller, F.C.; Gibson, T.B.; Carls, G.S.; Vogtmann, E.; Wang, S.; Murphy, B. The cost burden of oral, oral pharyngeal, and salivary gland cancers in three groups: Commercial insurance, medicare, and medicaid. Head Neck Oncol. 2012, 4, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Epstein, J.D.; Knight, T.K.; Epstein, J.B.; Bride, M.A.; Nichol, M.B. Cost of care for early-and late-stage oral and pharyngeal cancer in the California Medicaid population. Head Neck 2008, 30, 178–186. [Google Scholar] [CrossRef]
- OCRC (Occupational Cancer Research Centre). Burden of Occupational Cancer in Ontario: Major Workplace Carcinogens and Prevention of Exposure. Toronto: Queen’s Printer for Ontario. 2017. Available online: http://www.occupationalcancer.ca/wp-content/uploads/2017/09/Burden-of-Occupational-Cancer-in-Ontario.pdf (accessed on 6 June 2018).
- CAREX Canada. Wood Dust Exposure. 2018. Available online: https://www.carexcanada.ca/profile/wood_dust/ (accessed on 6 June 2018).
- Statistics Canada. Life Tables, Canada, Provinces and Territories 2010 to 2012. Statistics Canada.; 2016. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/160519/dq160519c-eng.pdf (accessed on 6 June 2018).
- Ontario Ministry of Healthcare. Schedule of Benefits. 2015. Available online: http://www.health.gov.on.ca/en/pro/programs/ohip/sob/physserv/sob_master20151221.pdf (accessed on 6 June 2018).
- Statistics Canada. Labour force Surveey (LFS), employment and unemployment, levels and rates, by province (Quebec, Ontario, Manitoba). 2011. Available online: http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/labor07b-eng.htm (accessed on 6 June 2018).
- Statistics Canada. Survey of Labour and Income Dynamics (SLID), Survey Overview. 2011. Available online: http://www.statcan.gc.ca/pub/75f0011x/75f0011x2013001-eng.htm (accessed on 6 June 2018).
- Statistics Canada. The System of National Accounts (CSNA), Health Utility Index. 2010. Available online: https://www150.statcan.gc.ca/n1/pub/67-001-x/2010004/beforetoc-avanttdm1-eng.htm (accessed on 6 June 2018).
- Statistics Canada. Guide to the Survey of Employment, Payrolls and Hours (SEPH). 2016. Available online: https://www150.statcan.gc.ca/n1/en/pub/72-203-g/72-203-g2016001-eng.pdf?st=IzYMvcwL (accessed on 30 November 2021).
- Statistics Canada. General Social Survey (GSS), Cycle 24: Time-Stress and Well-Being Public Use Microdata File Documentation and User’s Guide. 2011. Available online: https://www150.statcan.gc.ca/n1/en/catalogue/12M0024X (accessed on 6 June 2018).
- Statistics Canada. Canadian Community Health Survey (CCHS), Health Utility Index. 2010. Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs.html (accessed on 6 June 2018).
- Hutchings, S.J.; Rushton, L. Occupational cancer in Britain: Statistical methodology. Br. J. Cancer 2012, 107, S8. [Google Scholar] [CrossRef] [Green Version]
- Rushton, L.; Hutchings, S.; Fortunato, L.; Young, C.; Evans, G.S.; Brown, T.; Bevan, R.; Slack, R.; Holmes, P.; Bagga, S.; et al. Occupational cancer burden in Great Britain. Br. J. Cancer 2012, 107, S3–S7. [Google Scholar] [CrossRef] [PubMed]
- Labrèche, F.; Kim, J.; Song, C.; Pahwa, M.; Ge, C.B.; Arrandale, V.H.; McLeod, C.; Peters, C.E.; Lavoué, J.; Davies, H.W.; et al. The current burden of cancer attributable to occupational exposures in Canada. Prev. Med. 2019, 122, 128–139. [Google Scholar] [CrossRef]
- Kim, J.; Peters, C.E.; Arrandale, V.H.; Labrèche, F.; Ge, C.B.; McLeod, C.B.; Song, C.; Lavoué, J.; Davies, H.W.; Nicol, A.-M.; et al. Burden of lung cancer attributable to occupational diesel engine exhaust exposure in Canada. Occup. Environ. Med. 2018, 75, 617–622. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, C.; Bremner, K.E.; Pataky, R.; Gunraj, N.; Chan, K.; Peacock, S.; Krahn, M.D. Understanding the costs of cancer care before and after diagnosis for the 21 most common cancers in Ontario: A population-based descriptive study. CMAJ Open 2013, 1, E1. [Google Scholar] [CrossRef] [Green Version]
- Amin, M.B.; Edge, S.B.; Greene, F.L.; Byrd, D.R.; Brookland, R.K.; Washington, M.K.; Gershenwald, J.E.; Compton, C.C.; Hess, K.R.; Sullivan, D.C.; et al. (Eds.) AJCC Cancer Staging Manual, 8th ed.; Springer International Publishing: Berlin/Heidelberg, Germany, 2017; ISBN 978-3-319-40617-6. [Google Scholar]
- Xu, T.; Tang, J.; Gu, M.; Liu, L.; Wei, W.; Yang, H. Recurrent Nasopharyngeal Carcinoma: A Clinical Dilemma and Challenge. Curr. Oncol. 2013, 20, 406–419. [Google Scholar] [CrossRef] [Green Version]
- Won, H.S.; Chun, S.H.; Kim, B.S.; Chung, S.R.; Yoo, I.R.; Jung, C.K.; Kim, Y.S.; Sun, D.I.; Kim, M.S.; Kang, J.H. Treatment outcome of maxillary sinus cancer. Rare Tumors 2009, 1, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Alberta Health Services. Clinical Practice Guideline, Nasopharyngeal Cancer Treatment. HN-003HN-003. 2013. Available online: https://www.albertahealthservices.ca/assets/info/hp/cancer/if-hp-cancer-guide-hn003-nasopharyngeal.pdf (accessed on 6 June 2018).
- Longo, C.J.; Deber, R.; Fitch, M.; Williams, A.P.; D’souza, D. An examination of cancer patients’ monthly ‘out-of-pocket’costs in Ontario, Canada. Eur. J. Cancer Care 2007, 16, 500–507. [Google Scholar] [CrossRef]
- Yabroff, K.R.; Kim, Y. Time costs associated with informal caregiving for cancer survivors. Cancer 2009, 115, 4362–4373. [Google Scholar] [CrossRef]
- Statistic Canada. Hourly Minimum Wages in Canada for Adult Workers. 2017. Available online: http://srv116.services.gc.ca/dimt-wid/sm-mw/rpt2.aspx?lang=eng&dec=5 (accessed on 6 June 2018).
- Rezagholi, M.; Bantekas, A. Making economic social decisions for improving occupational health a predictive cost-benefit analysis. Occup. Med. Health Aff. 2015, 3, 2–9. [Google Scholar] [CrossRef] [Green Version]
- Loke, Y.; Tan, J.; Manickam, K.; Heng, P.; Tjong, C.; Kheng, L.G.; Lim, S.; Lin, G.S.; Takala, J. Economic cost of work-related injuries and ill-health in Singapore. 2013. Available online: https://www.wsh-institute.sg/~/media/wshi/past%20publications/2013/economic%20cost%20of%20worrelated%20injuries%20and%20ill-health%20in%20singapore.pdf?la=en (accessed on 6 June 2018).
- Galán, S.; Aguado, F.; Diez, F.; Mira, J. NasoNet, modeling the spread of nasopharyngeal cancer with networks of probabilistic events in discrete time. Artif. Intell. Med. 2002, 25, 247–264. [Google Scholar] [CrossRef] [Green Version]
- Llorente, J.L.; López, F.; Suárez, C.; Hermsen, M.A. Sinonasal carcinoma: Clinical, pathological, genetic and therapeutic advances. Nat. Rev. Clin. Oncol. 2014, 11, 460–472. [Google Scholar] [CrossRef] [PubMed]
- Noel, C.W.; Lee, D.; Kong, Q.; Xu, W.; Simpson, C.; Brown, D.; Gilbert, R.W.; Gullane, P.J.; Irish, J.C.; Huang, S.H.; et al. Comparison of Health State Utility Measures in Patients with Head and Neck Cancer. JAMA Otolaryngol. Neck Surg. 2015, 141, 696–703. [Google Scholar] [CrossRef] [PubMed]
- Skarsgard, D.P.; Groome, P.A.; Mackillop, W.J.; Zhou, S.; Rothwell, D.; Dixon, P.F.; O’Sullivan, B.; Hall, S.F.; Holowaty, E.J. Cancers of the upper aerodigestive tract in Ontario, Canada, and the United States. Cancer 2000, 88, 1728–1738. [Google Scholar] [CrossRef]
- Neumann, P.J.; Cohen, J.T.; Weinstein, M.C. Updating cost-effectiveness—The curious resilience of the $50,000-per-QALY threshold. N. Engl. J. Med. Overseas Ed. 2014, 371, 796–797. [Google Scholar] [CrossRef] [Green Version]
- Hirth, R.A.; Chernew, M.E.; Miller, E.; Fendrick, A.M.; Weissert, W.G. Willingness to pay for a quality-adjusted life year: In search of a standard. Med. Decis. Mak. 2000, 20, 332–342. [Google Scholar] [CrossRef]
- Olsson, A.; Kromhout, H. Occupational cancer burden: The contribution of exposure to process-generated substances at the workplace. Mol. Oncol. 2021, 15, 753–763. [Google Scholar] [CrossRef]
- Sun, L.; Paez, O.; Lee, D.; Salem, S.; Daraiseh, N. Estimating the uninsured costs of work-related accidents, part I: A systematic review. Theor. Issues Ergon. Sci. 2006, 7, 227–245. [Google Scholar] [CrossRef]
- Nicholson, S.; Pauly, M.V.; Polsky, D.; Sharda, C.; Szrek, H.; Berger, M.L. Measuring the effects of work loss on productivity with team production. Health Econ. 2006, 15, 111–123. [Google Scholar] [CrossRef] [Green Version]
| Exposed workers a | Total NPC b | Occupational NPC c | Total SNC d | Occupational SNC e | |
|---|---|---|---|---|---|
| Total | |||||
| 1,354,263 | 235 | 11 (4.6%) | 245 | 11 (4.4%) | |
| Sex | |||||
| Men | 812,558 (60%) | 165 | 11 (6.4%) | 145 | 10 (7.0%) |
| Women | 541,705 (40%) | 70 | 0 (0.4%) | 100 | 1 (0.5%) |
| Provinces of residence | |||||
| AB | 61,553 (9.1%) | 20 | 1 (4.0%) | 3 | 1 (26.7%) |
| BC | 141,639 (21.0%) | 45 | 3 (6.4%) | 15 | 2 (10.7%) |
| MB | 680,186 (3.5%) | 5 | 0 (6.0%) | 5 | 0 (8.0%) |
| NB | 23,550 (4.1%) | 5 | 0 (0.4%) | 5 | 1 (14.0%) |
| NL | 27,374 (2.4%) | 10 | 0 (0.2%) | 3 | 0 (16.7%) |
| NS | 16,035 (3.5%) | 10 | 1 (9.0%) | 5 | 1 (10.0%) |
| ON | 23,753 (27.7%) | 75 | 2 (3.2%) | 48 | 3 (6.5%) |
| PE | 186,830 (0.5%) | 0 | 0 (0%) | 0 | 0 (0%) |
| QC | 3465 (25.4%) | 35 | 2 (4.9%) | 33 | 3 (9.7%) |
| SK | 171,352 (2.7%) | 0 | 0 (0%) | 5 | 0 (6.0%) |
| Exposed workers a | Low (%) | Medium (%) | High (%) | NPC Cases (%) b | SNC Cases (%) c | |
|---|---|---|---|---|---|---|
| Total | ||||||
| 100 1,354,263 | 28 (379,228) | 43 (575,834) | 29 (399,201) | 100 (11) | 100 (11) | |
| Industrial sector | ||||||
| Accommodation and food services | 7131 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.5) |
| Agriculture | 2681 | 97 | 3 | 0 | 0 (0.01) | 0 (0.2) |
| Business/management/other support | 2229 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.2) |
| Construction | 560,139 | 27 | 73 | 0 | 5 (43.4) | 4 (38.5) |
| Educational services | 23,491 | 31 | 4 | 65 | 0 (1.1) | 0 (1.7) |
| Finance/insurance/real estate/leasing | 7638 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.5) |
| Fishing/hunting/trap | 81 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.01) |
| Forestry and logging | 51,251 | 47 | 1 | 52 | 0 (3.0) | 0 (3.9) |
| Health care/social assistance | 7592 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.5) |
| Info/culture/recreation | 8224 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.5) |
| Manufacturing | 585,951 | 12 | 27 | 61 | 6 (51.7) | 5 (47.2) |
| Mining/oil/gas extract | 5046 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.4) |
| Other services | 9469 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.6) |
| Professional scientific/technical service | 7896 | 97 | 3 | 0 | 0 (0.02) | 0 (0.5) |
| Public administration | 19,832 | 84 | 16 | 0 | 0 (0.4) | 0 (1.4) |
| Trade | 44,517 | 92 | 8 | 0 | 0 (0.4) | 0 (2.7) |
| Transportation/warehousing | 7405 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.5) |
| Utilities | 3689 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.3) |
| Occupational group | ||||||
| Construction trades | 710,805 | 26 | 60 | 14 | 6 (54.1) | 5 (50.9) |
| Contractors, supervisors in trades, transportation | 94,732 | 100 | 0 | 0 | 0 (0.01) | 1(6.5) |
| Labourer in processing, manufacturing, utilities | 101,095 | 6 | 11 | 84 | 1 (9.7) | 1(7.9) |
| Machine operators and assemblers in manufacturing | 215,202 | 9 | 19 | 72 | 2 (20.2) | 2 (18.4) |
| Natural and applied sciences | 3438 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.2) |
| Art, culture, recreation and sport | 315 | 19 | 81 | 0 | 0 (0.02) | 0 (4.3) |
| Social science/government service/religion | 76 | 100 | 0 | 0 | 0 (<0.01) | 0 (0.02) |
| Occupations unique to primary industry | 57,281 | 52 | 1 | 47 | 0 (3.0) | 0 (0.01) |
| Other management occupations | 310 | 100 | 0 | 0% | 0 (<0.01) | 0 (0.02) |
| Other trades occupations | 75,231 | 20 | 80 | 0 | 1 (6) | 1 (4.9) |
| Sales and service occupations | 9132 | 4 | 96 | 0 | 0 (0.9) | 0 (0.6) |
| Teachers and professors | 16,185 | 0 | 6 | 94 | 0 (1.1) | 0 (1.2) |
| Trades helpers, construction, transportation labourers | 69,002 | 33 | 39 | 29 | 1 (4.9) | 1 (5.1) |
| Transport and equipment operators | 1459 | 75 | 25 | 0 | 0 (0.04) | 0 (0.1) |
| Type of Cancer | NPC | SNC | ||||
|---|---|---|---|---|---|---|
| Per-Case | Total | % | Per-Case | Total | % | |
| Direct costs | ||||||
| Healthcare cost | CAD 52,531 | CAD 575,206 | 11 | CAD 53,275 | CAD 572,459 | 9 |
| Out-of-pocket cost | CAD 21,060 | CAD 230,603 | 4 | CAD 21,060 | CAD 226,296 | 3 |
| Informal caregiving | CAD 24,909 | CAD 272,749 | 5 | CAD 24,879 | CAD 267,328 | 4 |
| Sum | CAD 98,500 | CAD 1,078,558 | 20 | CAD 99,214 | CAD 1,066,083 | 16 |
| Indirect costs | ||||||
| Productivity losses | CAD 240,201 | CAD 2,630,149 | 48 | CAD 228,334 | CAD 2,453,514 | 36 |
| Home production losses | CAD 18,873 | CAD 206,655 | 4 | CAD 18,895 | CAD 203,035 | 3 |
| Friction losses | CAD 16,833 | CAD 184,322 | 3 | CAD 16,264 | CAD 174,767 | 3 |
| Sum | CAD 275,907 | CAD 3,021,126 | 55 | CAD 263,493 | CAD 2,831,316 | 42 |
| Intangible costs | ||||||
| Health-related quality of life losses (QALY) | 2.4 | 26.7 | - | 5.3 | 56.9 | - |
| Monetary value of health-related quality of life losses (CAD 50 k/QALY) | CAD 121,904 | CAD 1,334,824 | 25 | CAD 264,730 | CAD 2,844,602 | 42 |
| Sum | CAD 496,311 | CAD 5,434,508 | 100 | CAD 627,437 | CAD 6,742,000 | 100 |
| Assumptions | Range | NPC a | Change | SNC b | Change |
|---|---|---|---|---|---|
| Healthcare costs (pre-diagnosis; initial phases) | CAD 32,659; CAD 55,761 | CAD 5.28 M | −2.9% | CAD 6.72 M | −0.4% |
| CAD 36,283; CAD 60,630 | CAD 5.46 M | 0.5% | CAD 6.77 M | 0.4% | |
| Out-of-pocket costs (per month) | CAD 400 | CAD 5.20 M | −4.2% | CAD 6.52 M | −3.4% |
| CAD 600 | CAD 5.90 M | 8.6% | CAD 7.20 M | 6.8% | |
| Informal caregiving wage (per hours) | CAD 6 | CAD 5.34 M | −1.8% | CAD 6.65 M | −1.4% |
| CAD 13 | CAD 5.54 M | 1.9% | CAD 6.84 M | 1.5% | |
| Recurrence rate | 12% | CAD 5.41 M | −0.5% | CAD 6.65 M | −1.4% |
| 22% | CAD 5.46 M | 0.5% | CAD 6.84 M | 1.5% | |
| Fringe benefit | 10% | CAD 5.34 M | −1.8% | CAD 6.65 M | −1.4% |
| 20% | CAD 5.58 M | 2.7% | CAD 6.88 M | 2.1% | |
| Productivity growth | 0.5% | CAD 5.38 M | −1.0% | CAD 6.69 M | −0.8% |
| 2% | CAD 5.55 M | 2.1% | CAD 6.85 M | 1.6% | |
| Monetary value per QALY c | CAD 100,000 | CAD 6.77 M | 24.6% | CAD 8.14 M | 20.7% |
| CAD 150,000 | CAD 8.10 M | 49.1% | CAD 10.26 M | 52.1% | |
| Cases (Cl of 95%) d | NPC:9; SNC:6 | CAD 4.22 M | −22.4% | CAD 3.82 M | −43.3% |
| NPC:29; SNC:32 | CAD 14.51 M | 167.0% | CAD 19.98 M | 196.3% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mofidi, A.; Tompa, E.; Kalcevich, C.; McLeod, C.; Lebeau, M.; Song, C.; Kim, J.; Demers, P.A. Occupational Exposure to Wood Dust and the Burden of Nasopharynx and Sinonasal Cancer in Canada. Int. J. Environ. Res. Public Health 2022, 19, 1144. https://doi.org/10.3390/ijerph19031144
Mofidi A, Tompa E, Kalcevich C, McLeod C, Lebeau M, Song C, Kim J, Demers PA. Occupational Exposure to Wood Dust and the Burden of Nasopharynx and Sinonasal Cancer in Canada. International Journal of Environmental Research and Public Health. 2022; 19(3):1144. https://doi.org/10.3390/ijerph19031144
Chicago/Turabian StyleMofidi, Amirabbas, Emile Tompa, Christina Kalcevich, Christopher McLeod, Martin Lebeau, Chaojie Song, Joanne Kim, and Paul A. Demers. 2022. "Occupational Exposure to Wood Dust and the Burden of Nasopharynx and Sinonasal Cancer in Canada" International Journal of Environmental Research and Public Health 19, no. 3: 1144. https://doi.org/10.3390/ijerph19031144
APA StyleMofidi, A., Tompa, E., Kalcevich, C., McLeod, C., Lebeau, M., Song, C., Kim, J., & Demers, P. A. (2022). Occupational Exposure to Wood Dust and the Burden of Nasopharynx and Sinonasal Cancer in Canada. International Journal of Environmental Research and Public Health, 19(3), 1144. https://doi.org/10.3390/ijerph19031144






