Risk Factors for Multidrug-Resistant Gram-Negative Bacteria Carriage upon Admission to the Intensive Care Unit
Abstract
1. Introduction
2. Materials and Methods
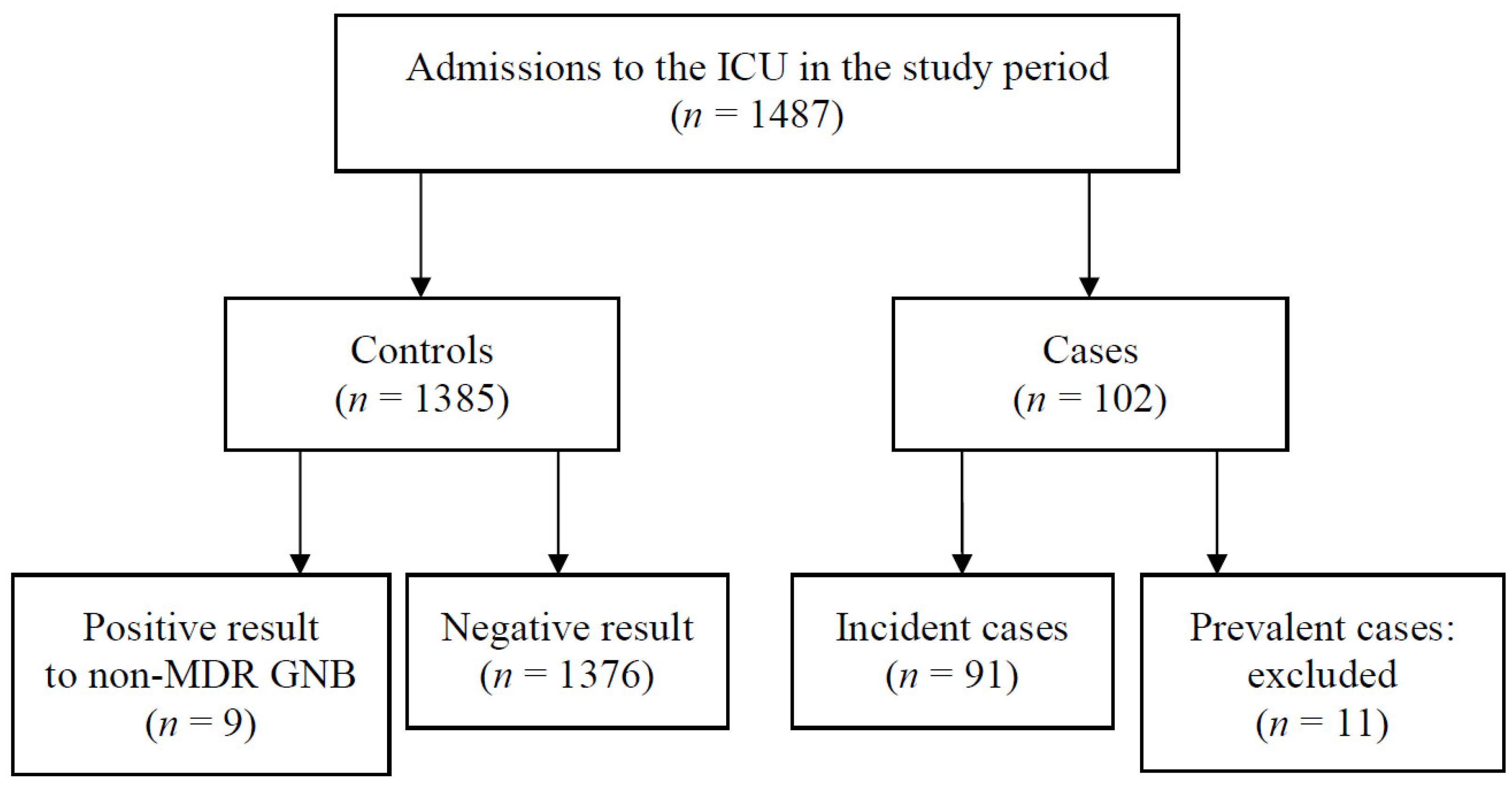
2.1. Study Design
2.2. Study Population
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Univariate and Bivariate Analysis
3.2. Multivariate Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ruppé, É.; Woerther, P.-L.; Barbier, F. Mechanisms of antimicrobial resistance in gram-negative bacilli. Ann. Intensive Care 2015, 5, 21. [Google Scholar] [CrossRef] [PubMed]
- Naylor, N.R.; Atun, R.; Zhu, N.; Kulasabanathan, K.; Silva, S.; Chatterjee, A.; Knight, G.M.; Robotham, J.V. Estimating the burden of antimicrobial resistance: A systematic literature review. Antimicrob. Resist. Infect. Control 2018, 7, 58. [Google Scholar] [CrossRef] [PubMed]
- Cole, J. Antimicrobial Resistance—A ‘Rising Tide’ of National (and International) Risk. J. Hosp. Infect. 2016, 92, 3–4. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Antimicrobial Resistance: Global Report on Surveillance 2014; WHO: Geneva, Switzerland, 2016; Available online: http://www.who.int/antimicrobial-resistance/publications/surveillancereport/en/ (accessed on 3 March 2021).
- European Centre for Disease Prevention and Control. Antimicrobial Resistance in the EU/EEA (EARS-Net)—Annual Epidemiological Report for 2019; ECDC: Stockholm, Sweden, 2020; Available online: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-resistance-europe-2019 (accessed on 3 March 2021).
- European Centre for Disease Prevention and Control. Last-Line Antibiotics are Failing: Options to Address This Urgent Threat to Patients and Healthcare Systems; ECDC: Stockholm, Sweden, 2016; Available online: https://www.ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/antibiotic-resistance-policy-briefing.pdf (accessed on 3 March 2021).
- Magiorakos, A.P.; Burns, K.; Rodríguez Baño, J.; Borg, M.; Daikos, G.; Dumpis, U.; Lucet, J.C.; Moro, M.L.; Tacconelli, E.; Simonsen, G.S.; et al. Infection prevention and control measures and tools for the prevention of entry of carbapenem-resistant enterobacteriaceae into healthcare settings: Guidance from the European Centre for Disease Prevention and Control. Antimicrob. Resist. Infect. Control 2017, 6, 113. [Google Scholar] [CrossRef] [PubMed]
- Banach, D.B.; Bearman, G.; Barnden, M.; Hanrahan, J.A.; Leekha, S.; Morgan, D.J.; Murthy, R.; Munoz-Price, L.S.; Sullivan, K.V.; Popovich, K.J.; et al. Duration of contact precautions for acute-care settings. Infect. Control Hosp. Epidemiol. 2018, 39, 127–144. [Google Scholar] [CrossRef] [PubMed]
- Garnacho Montero, J.; Lerma, F.Á.; Galleymore, P.R.; Martínez, M.P.; Rocha, L.Á.; Gaite, F.B.; Rodríguez, J.Á.; González, M.C.; Moreno, I.F.; Baño, J.R.; et al. Combatting resistance in intensive care: The multimodal approach of the Spanish ICU “Zero Resistance” program. Crit. Care 2015, 19, 114. [Google Scholar] [CrossRef][Green Version]
- Razazi, K.; Derde, L.P.G.; Verachten, M.; Legrand, P.; Lesprit, P.; Brun-Buisson, C. Clinical impact and risk factors for colonization with extended-spectrum β-lactamase-producing bacteria in the intensive care unit. Intensive Care Med. 2012, 38, 1769–1778. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Risk Assessment on the Spread of Carbapenemase-Producing Enterobacteriaceae (CPE): Through Patient Transfer between Healthcare Facilities, with Special Emphasis on Cross-Border Transfer; Publications Office: Luxembourg, 2011. [Google Scholar] [CrossRef]
- López-Cerero, L.; Egea, P.; Gracia-Ahufinger, I.; González-Padilla, M.; Rodríguez-López, F.; Rodríguez-Baño, J.; Pascual, A. Characterisation of the first ongoing outbreak due to KPC-3-producing Klebsiella pneumoniae (ST512) in Spain. Int. J. Antimicrob. Agents 2014, 44, 538–540. [Google Scholar] [CrossRef]
- Siegel, J.D.; Rhinehart, E.; Jackson, M.; Chiarello, L. Management of Multidrug-Resistant Organisms in Healthcare Settings, 2006 (Updated 2017). 2006. Available online: https://www.cdc.gov/infectioncontrol/guidelines/mdro/ (accessed on 3 March 2021).
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Grupo de trabajo de HAM. Vigilancia de Microorganismos Multirresistentes. Criterios para Instaurar Precauciones de Control, Gestión y Seguimiento de las Alertas. Sistema de Vigilancia Epidemiológica de Andalucía; Consejería de Salud y Familias: Seville, Spain, 2018. [Google Scholar]
- Gonzalez, V.E.P.; Marco, F.; Arteaga, M.; Reverter, E.; Escorsell, A.; Carpio, A.; Mezzano, G.; Rodríguez, S.; Juanola, A.; Mensa, J.; et al. Prevalence and clinical impact of rectal colonization by multidrug-resistant bacteria in critically ill patients with and without cirrhosis. J. Hepatol. 2017, 66, S564. [Google Scholar] [CrossRef]
- Hernandez-Tejero, M.; Aziz, F.; Pitart, C.; Reverte, F.M.; Campo, I.; Carpio, A.; Reverter, E.; Escorsell, A.; Ortiz, S.; Mezzano, G.; et al. SAT-045-Prevalence, type and risk factors of colonization by multidrug-resistant bacteria in a large series of patients with decompensated cirrhosis. J. Hepatol. 2019, 70, e646–e647. [Google Scholar] [CrossRef]
- Irvine, K.M.; Ratnasekera, I.; Powell, E.E.; Hume, D.A. Causes and consequences of innate immune dysfunction in cirrhosis. Front. Immunol. 2019, 10, 293. [Google Scholar] [CrossRef] [PubMed]
- Schellongowski, P.; Sperr, W.R.; Wohlfarth, P.; Knoebl, P.; Rabitsch, W.; Watzke, H.H. Critically ill patients with cancer: Chances and limitations of intensive care medicine—A narrative review. ESMO Open 2016, 1, 18. [Google Scholar] [CrossRef]
- Jalan, R.; Fernandez, J.; Wiest, R.; Schnabl, B.; Moreau, R.; Angeli, P.; Stadlbauer, V.; Gustot, T.; Bernardi, M.; Canton, R.; et al. Bacterial infections in cirrhosis: A position statement based on the EASL Special Conference 2013. J. Hepatol. 2014, 60, 1310–1324. [Google Scholar] [CrossRef]
- Platteel, T.N.; Leverstein-van Hall, M.A.; Cohen Stuart, J.W.; Thijsen, S.F.T.; Mascini, E.M.; van Hees, B.C.; Scharringa, J.; Fluit, A.C.; Bonten, M.J.M. Predicting carriage with extended-spectrum beta-lactamase-producing bacteria at hospital admission: A cross-sectional study. Clin. Microbiol. Infect. 2015, 21, 141–146. [Google Scholar] [CrossRef][Green Version]
- O’Horo, J.C.; Farrell, A.; Sohail, M.R.; Safdar, N. Carbapenem-resistant enterobacteriaceae and endoscopy: An evolving threat. Am. J. Infect. Control. 2016, 44, 1032–1036. [Google Scholar] [CrossRef]
- Salomão, M.C.; Freire, M.P.; Boszczowski, I.; Raymundo, S.F.; Guedes, A.R.; Levin, A.S. Increased risk for carbapenem-resistant enterobacteriaceae colonization in intensive care units after hospitalization in emergency department. Emerg. Infect. Dis. 2020, 26, 1156–1163. [Google Scholar] [CrossRef]
- Kizilates, F.; Yakupogullari, Y.; Berk, H.; Oztoprak, N.; Otlu, B. Risk factors for fecal carriage of extended-spectrum beta-lactamase-producing and carbapenem-resistant Escherichia coli and Klebsiella pneumoniae strains among patients at hospital admission. Am. J. Infect. Control. 2021, 49, 333–339. [Google Scholar] [CrossRef]
- Liu, P.; Li, X.; Luo, M.; Xu, X.; Su, K.; Chen, S.; Qing, Y.; Li, Y.; Qiu, J. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection: A meta-analysis. Microb. Drug Resist. 2018, 24, 190–198. [Google Scholar] [CrossRef]
- Lima, E.M.; Cid, P.A.; Beck, D.S.; Pinheiro, L.H.Z.; Tonhá, J.P.S.; Alves, M.Z.O.; Lourenço, N.D.; Santos, R.Q.; Asensi, M.D.; Marques, J.A.; et al. Predictive factors for sepsis by carbapenem resistant gram-negative bacilli in adult critical patients in Rio de Janeiro: A case-case-control design in a prospective cohort study. Antimicrob. Resist. Infect. Control 2020, 9, 132. [Google Scholar] [CrossRef]
- Birgand, G.; Armand-Lefevre, L.; Lolom, I.; Ruppe, E.; Andremont, A.; Lucet, J.-C. Duration of colonization by extended-spectrum β-lactamase-producing enterobacteriaceae after hospital discharge. Am. J. Infect. Control 2013, 41, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, F.S.; Assous, M.V.; Bdolah-Abram, T.; Lachish, T.; Yinnon, A.M.; Wiener-Well, Y. Duration of carriage of carbapenem-resistant enterobacteriaceae following hospital discharge. Am. J. Infect. Control 2013, 41, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Haverkate, M.R.; Weiner, S.; Lolans, K.; Moore, N.M.; Weinstein, R.A.; Bonten, M.J.M.; Hayden, M.K.; Bootsma, M.C.J. Duration of colonization with Klebsiella pneumoniae carbapenemase-producing bacteria at long-term acute care hospitals in Chicago, Illinois. Open Forum Infect. Dis. 2016, 3, ofw178. [Google Scholar] [CrossRef]
- Christaki, E.; Marcou, M.; Tofarides, A. Antimicrobial resistance in bacteria: Mechanisms, evolution, and persistence. J. Mol. Evol. 2020, 88, 26–40. [Google Scholar] [CrossRef]
- Schechner, V.; Temkin, E.; Harbarth, S.; Carmeli, Y.; Schwaber, M.J. Epidemiological interpretation of studies examining the effect of antibiotic usage on resistance. Clin. Microbiol. Rev. 2013, 26, 289–307. [Google Scholar] [CrossRef]
- Aliyu, S.; Smaldone, A.; Larson, E. Prevalence of multidrug-resistant gram-negative bacteria among nursing home residents: A systematic review and meta-analysis. Am. J. Infect. Control 2017, 45, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Nseir, S.; Grailles, G.; Soury-Lavergne, A.; Minacori, F.; Alves, I.; Durocher, A. Accuracy of American Thoracic Society/Infectious Diseases Society of America criteria in predicting infection or colonization with multidrug-resistant bacteria at intensive-care unit admission. Clin. Microbiol. Infect. 2010, 16, 902–908. [Google Scholar] [CrossRef]
- Van Hout, D.; Bruijning-Verhagen, P.C.J.; Blok, H.E.M.; Troelstra, A.; Bonten, M.J.M. Universal risk assessment upon hospital admission for screening of carriage with multidrug-resistant micro-organisms in a Dutch tertiary care centre. J. Hosp. Infect. 2021, 109, 32–39. [Google Scholar] [CrossRef]
- Siegel, J.D.; Rhinehart, E.; Jackson, M.; Chiarello, L. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007). 2019. Available online: https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html (accessed on 7 March 2021).
- Guzmán Herrador, B.R.; Romero Muñoz, M.J.; Ruiz Montero, R.; de la Fuente Martos, C.; Salcedo Leal, I.; Barranco Quintana, J.L.; Amor Díaz, I.; González Priego, M.L.; Díaz Molina, C. Grupos de discusión como abordaje para valorar conocimiento, actitudes y prácticas de higiene de manos en profesionales de la unidad de cuidados intensivos de adultos de un hospital de referencia. J. Healthc. Qual. Res. 2020, 35, 297–304. [Google Scholar] [CrossRef]
- Yoon, Y.K.; Ryu, J.M.; Lee, M.J.; Lee, S.E.; Yang, K.S.; Lee, C.K.; Kim, M.J.; Sohn, J.W. Active surveillance at the time of hospital admission for multidrug-resistant microorganisms among patients who had recently been hospitalized at health care facilities. Am. J. Infect. Control 2019, 47, 1188–1193. [Google Scholar] [CrossRef] [PubMed]
- Strich, J.R.; Palmore, T.N. Preventing transmission of multidrug-resistant pathogens in the intensive care unit. Infect. Dis. Clin. 2017, 31, 535–550. [Google Scholar] [CrossRef] [PubMed]
- Rutala, W.A.; Weber, D.J. Best practices for disinfection of noncritical environmental surfaces and equipment in health care facilities: A bundle approach. Am. J. Infect. Control 2019, 47, A96–A105. [Google Scholar] [CrossRef] [PubMed]
- Muscarella, L.F. Risk of transmission of carbapenem-resistant enterobacteriaceae and related “superbugs” during gastrointestinal endoscopy. World J. Gastrointest. Endosc. 2014, 6, 457. [Google Scholar] [CrossRef]
- Balan, G.G.; Sfarti, C.V.; Chiriac, S.A.; Stanciu, C.; Trifan, A. Duodenoscope-associated infections: A review. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 2205–2213. [Google Scholar] [CrossRef] [PubMed]
- Baur, D.; Gladstone, B.P.; Burkert, F.; Carrara, E.; Foschi, F.; Döbele, S.; Tacconelli, E. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and clostridium difficile infection: A systematic review and meta-analysis. Lancet Infect. Dis. 2017, 17, 990–1001. [Google Scholar] [CrossRef]
- Sánchez-Ramírez, C.; Hípola-Escalada, S.; Cabrera-Santana, M.; Hernández-Viera, M.A.; Caipe-Balcázar, L.; Saavedra, P.; Artiles-Campelo, F.; Sangil-Monroy, N.; Lübbe-Vázquez, C.F.; Ruiz-Santana, S. Long-term use of selective digestive decontamination in an ICU highly endemic for bacterial resistance. Crit. Care 2018, 22, 141. [Google Scholar] [CrossRef]
- Bar-Yoseph, H.; Lulu, C.; Shklar, S.; Korytny, A.; Even Dar, R.; Daoud, H.; Hussein, K.; Bar-Lavie, Y.; Jabareen, A.; Geffen, Y.; et al. Efficacy of a hospital policy of selective digestive decontamination for carbapenem-resistant enterobacterales carriers: Prospective before–after study. J. Hosp. Infect. 2020, 106, 495–499. [Google Scholar] [CrossRef]
- Knight, G.M.; Glover, R.E.; McQuaid, C.F.; Olaru, I.D.; Gallandat, K.; Leclerc, Q.J.; Fuller, N.M.; Willcocks, S.J.; Hasan, R.; van Kleef, E.; et al. Antimicrobial resistance and COVID-19: Intersections and implications. eLife 2021, 10, e64139. [Google Scholar] [CrossRef]
- Giannella, M.; Trecarichi, E.M.; De Rosa, F.G.; Del Bono, V.; Bassetti, M.; Lewis, R.E.; Losito, A.R.; Corcione, S.; Saffioti, C.; Bartoletti, M.; et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae bloodstream infection among rectal carriers: A prospective observational multicentre study. Clin. Microbiol. Infect. 2014, 20, 1357–1362. [Google Scholar] [CrossRef]
- Nakai, H.; Hagihara, M.; Kato, H.; Hirai, J.; Nishiyama, N.; Koizumi, Y.; Sakanashi, D.; Suematsu, H.; Yamagishi, Y.; Mikamo, H. Prevalence and risk factors of infections caused by extended-spectrum β-lactamase (ESBL)-producing enterobacteriaceae. J. Infect. Chemother. 2016, 22, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Kang, C.-I.; Wi, Y.M.; Chung, D.R.; Peck, K.R.; Lee, N.-Y.; Song, J.-H. Risk factors and molecular epidemiology of community-onset, multidrug resistance extended-spectrum β-lactamase-producing Escherichia coli infections. Korean J. Intern. Med. 2017, 32, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Padilla-Serrano, A.; Serrano-Castañeda, J.J.; Carranza-González, R.; García-Bonillo, M.P. Clinical significance and risk factors for multidrug resistant Enterobacteriaceae colonization. Rev. Esp. Quim. 2018, 31, 257–262. [Google Scholar]
- Gómez-Zorrilla, S.; Camoez, M.; Tubau, F.; Periche, E.; Cañizares, R.; Dominguez, M.A.; Ariza, J.; Peña, C. Antibiotic pressure is a major risk factor for rectal colonization by multidrug-resistant pseudomonas aeruginosa in critically ill patients. Antimicrob. Agents Chemother. 2014, 58, 5863–5870. [Google Scholar] [CrossRef] [PubMed]
- EU Action on Antimicrobial Resistance. Public Health. Available online: https://ec.europa.eu/health/antimicrobial-resistance/eu-action-on-antimicrobial-resistance_en (accessed on 5 April 2021).

| Characteristic | Cases n = 91 (6.2%) | Controls n = 1385 (93.8%) | p Value |
|---|---|---|---|
| Age (years), median (IQR) | 63.87 (52.94, 74.10) | 63.16 (52.60, 73.14) | 0.933 1 |
| Sex | 0.331 2 | ||
| Female | 35 (38.5%) | 456 (32.9%) | |
| Male | 56 (61.5%) | 929 (67.1%) | |
| Stay in congregate settings | 0 | 7 (0.5%) | 1 3 |
| Nursing home | 0 | 4 (0.3%) | |
| Prison | 0 | 2 (0.1%) | |
| Other | 0 | 1 (0.1%) | |
| Referring ward | <0.001 *4 | ||
| Cardiology | 24 (26.4%) | 361 (26.1%) | |
| Cardiovascular surgery | 9 (9.9%) | 283 (20.4%) | |
| General & Digestive surgery | 7 (7.7%) | 35 (2.5%) | |
| Emergency Department | 19 (20.9%) | 394 (28.4%) | |
| Hepatology | 12 (13.2%) | 63 (4.5%) | |
| Pulmonology | 4 (4.4%) | 69 (5.0%) | |
| Other | 16 (17.6%) | 180 (13.0%) | |
| APACHE classification system | 0.119 4 | ||
| Medical | 73 (80.2%) | 977 (70.5%) | |
| Non-emergency surgical | 13 (14.3%) | 261 (18.8%) | |
| Emergency surgical | 5 (5.5%) | 147 (10.6%) | |
| Previous hospital admissions | 44 (48.4%) | 609 (44.0%) | 0.480 2 |
| Previous hospital admissions (number), median (IQR) | 1 (1, 2) | 1 (1, 2) | 0.311 1 |
| Length of hospital stay in the last year (days), median (IQR) | 5 (0, 16.50) | 2 (0, 7) | 0.001 *1 |
| Previous MDR-GNB carriage | 6 (6.6%) | 13 (0.9%) | 0.001 *3 |
| Cancer chemotherapy | 2 (2.2%) | 46 (3.3%) | 0.844 3 |
| Dialysis | 1 (1.1%) | 18 (1.3%) | 1 3 |
| Previous antibacterial therapy | 15 (16.5%) | 57 (4.1%) | <0.001 *3 |
| Previous therapy with third-, fourth- or fifth-generation cephalosporins | 2 (2.2%) | 10 (0.7%) | 0.332 3 |
| Previous therapy with carbapenems | 2 (2.2%) | 6 (0.4%) | 0.165 3 |
| Cystic fibrosis | 0 | 15 (1.1%) | 0.766 3 |
| Bronchiectasis | 1 (1.1%) | 18 (1.3%) | 1 3 |
| COPD | 9 (9.9%) | 109 (7.9%) | 0.625 2 |
| Chronic ulcers | 0 | 0 | - |
| Liver cirrhosis | 8 (8.8%) | 46 (3.3%) | 0.030 *3 |
| Immunodeficiency | 1 (1.1%) | 12 (0.9%) | 1 3 |
| Cancer | 12 (13.2%) | 131 (9.5%) | 0.326 2 |
| Neutropenia | 6 (6.6%) | 35 (2.5%) | 0.073 3 |
| Type 1 diabetes | 2 (2.2%) | 20 (1.4) | 0.796 3 |
| Type 2 diabetes | 21 (23.1%) | 322 (23.2%) | 0.928 2 |
| Pressure ulcers | 1 (1.1%) | 10 (0.7%) | 1 3 |
| Digestive surgery in the last year | 15 (16.5%) | 50 (3.6%) | <0.001 *3 |
| Previous gastrointestinal endoscopy | 11 (12.1%) | 54 (3.9%) | 0.001 *4 |
| Upper | 7 (7.7%) | 26 (1.9%) | |
| Lower | 4 (4.4%) | 29 (2.1%) | |
| APACHE II score (points), mean (SD) | 17.76 (9.57) | 18.41 (7.51) | 0.528 5 |
| Solid organ transplantation | 10 (11.0%) | 123 (8.9%) | 0.623 2 |
| Hematopoietic stem cell transplantation | 0 | 4 (0.3%) | 1 3 |
| Biliary drainage | 1 (1.1%) | 1 (0.1%) | 0.239 3 |
| MDR-GNB | Mechanism(s) of Resistance | n | % (Same Species) | % (Overall) |
|---|---|---|---|---|
| Escherichia coli | ESBL production | 56 | 96.6 | 55.4 |
| IMP production | 1 | 1.7 | 1.0 | |
| OXA-48 production | 1 | 1.7 | 1.0 | |
| Klebsiella pneumoniae | ESBL production | 13 | 81.3 | 12.9 |
| IMP production | 1 | 6.3 | 1.0 | |
| KPC production | 1 | 6.3 | 1.0 | |
| OXA-48 production | 1 | 6.3 | 1.0 | |
| Klebsiella aerogenes | AmpC derepression | 4 | 80 | 4.0 |
| ESBL production | 1 | 20 | 1.0 | |
| Klebsiella oxytoca | ESBL production | 4 | 100 | 4.0 |
| Citrobacter freundii | AmpC derepression | 7 | 100 | 6.9 |
| Enterobacter cloacae | AmpC derepression | 4 | 66.7 | 4.0 |
| ESBL production | 1 | 16.7 | 1.0 | |
| OXA-48 production | 1 | 16.7 | 1.0 | |
| Proteus mirabilis | ESBL production | 2 | 66.7 | 2.0 |
| OXA-48 production | 1 | 33.3 | 1.0 | |
| Pseudomonas aeruginosa | Other * | 2 | 100 | 2.0 |
| Total | - | 101 | - | 100 |
| Risk Factor | Crude OR | Adjusted OR (95% CI) | p Value |
|---|---|---|---|
| Liver cirrhosis | 2.81 | 6.54 (2.17–19.17) | <0.001 *1 |
| Previous MDR-GNB carriage | 7.45 | 5.34 (1.55–16.60) | 0.005 *1 |
| Digestive surgery in the last year | 5.27 | 2.83 (1.29–5.89) | 0.007 *1 |
| Length of hospital stay in the last year (days) | 1.02 | 1.01 (1.00–1.03) | 0.026 *1 |
| Previous gastrointestinal endoscopy | 3.63 | 1.98 (0.92–4.01) | 0.067 1 |
| APACHE classification system | 0.098 2 | ||
| Emergency surgical (reference) | 1 | 1 | |
| Non-emergency surgical | 1.46 | 4.10 (1.20–16.71) | |
| Medical | 2.20 | 5.17 (1.76–19.04) | |
| Cancer chemotherapy | 0.65 | 0.27 (0.04–1.07) | 0.113 1 |
| Previous antibacterial therapy | 4.60 | 1.89 (0.83–4.05) | 0.114 1 |
| Sex (female) | 1.27 | 1.32 (0.83–2.08) | 0.234 1 |
| Age (years) | 1.00 | 1.00 (0.98–1.01) | 0.833 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Martínez, N.F.; Cárcel-Fernández, S.; De la Fuente-Martos, C.; Ruiz-Montero, R.; Guzmán-Herrador, B.R.; León-López, R.; Gómez, F.J.; Guzmán-Puche, J.; Martínez-Martínez, L.; Salcedo-Leal, I. Risk Factors for Multidrug-Resistant Gram-Negative Bacteria Carriage upon Admission to the Intensive Care Unit. Int. J. Environ. Res. Public Health 2022, 19, 1039. https://doi.org/10.3390/ijerph19031039
Fernández-Martínez NF, Cárcel-Fernández S, De la Fuente-Martos C, Ruiz-Montero R, Guzmán-Herrador BR, León-López R, Gómez FJ, Guzmán-Puche J, Martínez-Martínez L, Salcedo-Leal I. Risk Factors for Multidrug-Resistant Gram-Negative Bacteria Carriage upon Admission to the Intensive Care Unit. International Journal of Environmental Research and Public Health. 2022; 19(3):1039. https://doi.org/10.3390/ijerph19031039
Chicago/Turabian StyleFernández-Martínez, Nicolás Francisco, Sheila Cárcel-Fernández, Carmen De la Fuente-Martos, Rafael Ruiz-Montero, Bernardo R. Guzmán-Herrador, Rafael León-López, Francisco Javier Gómez, Julia Guzmán-Puche, Luis Martínez-Martínez, and Inmaculada Salcedo-Leal. 2022. "Risk Factors for Multidrug-Resistant Gram-Negative Bacteria Carriage upon Admission to the Intensive Care Unit" International Journal of Environmental Research and Public Health 19, no. 3: 1039. https://doi.org/10.3390/ijerph19031039
APA StyleFernández-Martínez, N. F., Cárcel-Fernández, S., De la Fuente-Martos, C., Ruiz-Montero, R., Guzmán-Herrador, B. R., León-López, R., Gómez, F. J., Guzmán-Puche, J., Martínez-Martínez, L., & Salcedo-Leal, I. (2022). Risk Factors for Multidrug-Resistant Gram-Negative Bacteria Carriage upon Admission to the Intensive Care Unit. International Journal of Environmental Research and Public Health, 19(3), 1039. https://doi.org/10.3390/ijerph19031039






