Early Detection of the Start of the Influenza Epidemic Using Surveillance Systems in Catalonia (PREVIGrip Study)
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Data Collection
2.3. Statistics Analysis
2.3.1. Analysis of Trends between the Three Surveillance Systems for Complete Seasons and in the Pre-Epidemic Data
2.3.2. Excess Diagnostic Rates Compared with Other Surveillance Systems
2.3.3. Time Lag between Clinical and Confirmed Diagnoses
3. Results
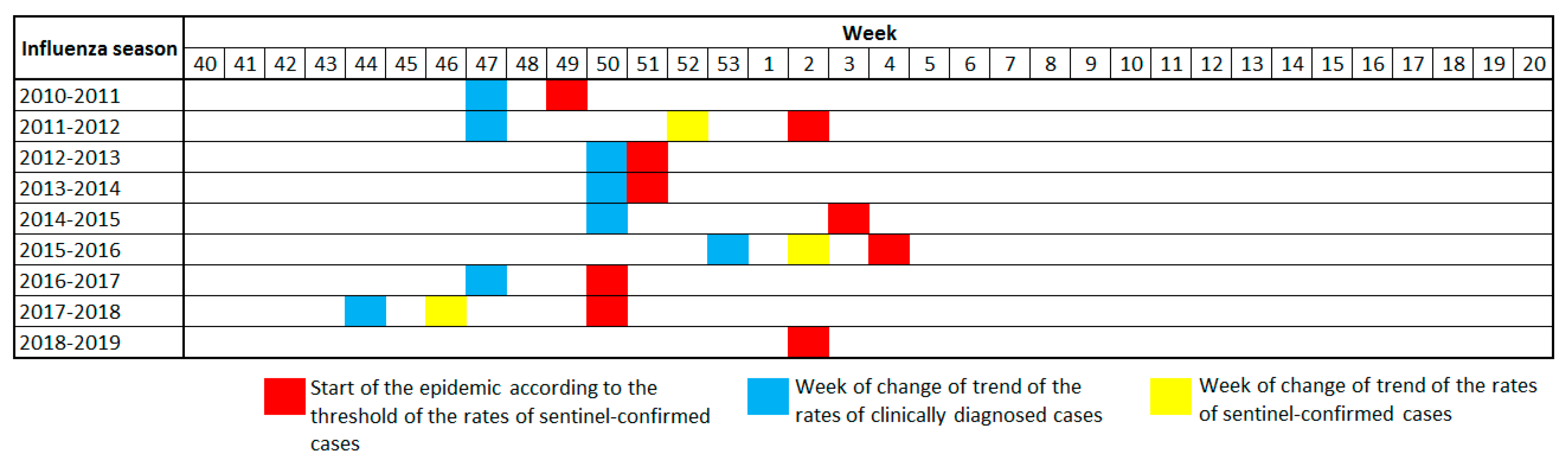
3.1. Trend Analysis
3.2. Quantification of Excess Diagnostic Rates Compared with Other Surveillance Systems
3.3. Time Lag between Surveillance Systems
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO (World Health Organization). Burden of Influenza. Available online: http://www.euro.who.int/en/health-topics/communicable-diseases/influenza/seasonal-influenza/burden-of-influenza (accessed on 16 September 2022).
- WHO (World Health Organization). Gripe (Estacional). Available online: https://www.who.int/es/news-room/fact-sheets/detail/influenza-(seasonal) (accessed on 7 July 2020).
- Instituto de Salud Carlos III; Red Nacional de Vigilancia Epidemiológica Sistema de Vigilancia de la Gripe en España. Red Nacional de Vigilancia Epidemiológica. Available online: https://vgripe.isciii.es/inicio.do;jsessionid=724C9005B17613D1D56C75B7125FE42B (accessed on 9 September 2022).
- Sistema de Vigilancia de la Gripe en España; Red Nacional Vigilancia de Epidemiológica (RENAVE); Instituto de Salud Carlos III; Instituto de Salud Carlos III; Red Nacional de Vigilancia Epidemiológica. Sistemas y Fuentes de Información Temporada 2019–2020; Sistema de Vigilancia de Gripe en España: Madrid, Spain, 2019; pp. 1–9. [Google Scholar]
- Generalitat de Catalunya. Departament de Salut Pla d’informació de les Infeccions Respiratòries agudes a Catalunya. 2019; pp. 1–10. Available online: https://canalsalut.gencat.cat/web/.content/_Professionals/Vigilancia_epidemiologica/documents/arxius/pla-pidirac-2020-21.pdf (accessed on 15 September 2022).
- Closas, P.; Coma, E.; Méndez, L. Sequential detection of influenza epidemics by the Kolmogorov-Smirnov test. BMC Med. Inform. Decis. Mak. 2012, 12, 112. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. End-to-End Integration of SARS-CoV-2 and Influenza Sentinel Surveillance: Revised Interim Guidance; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Red Nacional de Vigilancia Epidemiológica. Ministerio de Sanidad Gobierno de España Protocolo para la Vigilancia Cen-tinela de Infección Respiratoria Aguda (IRAs) en Atención Primaria en España; Red Nacional de Vigilancia Epidemiológica: Madrid, Spain, 2022; pp. 1–17. [Google Scholar]
- Red Nacional Vigilancia de Epidemiológica (RENAVE); Instituto de Salud Carlos III. Sistema de Vigilancia de Infección Respiratoria Aguda Protocolo para la Vigilancia Centinela de Infección Respiratoria Aguda Grave (IRAG) en Hospitales en España; Instituto de Salud Carlos III: Madrid, Spain, 2022; Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/Protocolos_SiVIRA/Protocolo%20vigilancia%20IRAG%20en%20Espa%C3%B1a_v04%20de%20febrero2022.pdf (accessed on 15 September 2022).
- Generalitat de Catalunya. Departament de Salut SIVIC. Available online: https://sivic.salut.gencat.cat/ (accessed on 9 September 2022).
- Generalitat de Catalunya. Departament de Salut Dades COVID. Available online: https://dadescovid.cat/ (accessed on 27 September 2022).
- Aguilar, M.C.; Dalmau, L.M.R.; Castro, B.E.; Carrasco-Querol, N.; Hernández, R.Z.; Forcadell, D.E.; Rodríguez, C.D.; Queiroga, G.A.; Fernández-Sáez, J. Concordance between the Clinical Diagnosis of Influenza in Primary Care and Epidemiological Surveillance Systems (PREVIGrip Study). Int. J. Environ. Res. Public Health 2022, 19, 1263. [Google Scholar] [CrossRef] [PubMed]
- Arranz, I.J.; Leiva, R.A.; Carandell, J.E.; Pujol, B.A.; Méndez, C.M.C.; Salvà, F.A.; Esteva, C.M. Vigilancia sindrómica de la gripe en atención primaria, un instrumento complementario a las redes centinelas para períodos de elevada incidencia de gripe. Aten. Primaria. 2012, 44, 258–264. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cocoros, N.M.; Panucci, G.; Haug, N.; Maher, C.; Reichman, M.; Toh, S. Outpatient influenza antivirals in a distributed data network for influenza surveillance. Influenza Respi. Viruses. 2018, 12, 804–807. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.B.; Song, J.Y.; Cheong, H.J.; Cho, Y.D.; Wie, S.H.; Jeong, H.W.; Kim, W.J. Hospital-based influenza morbidity and mortality surveillance system for influenza-like illnesses: A comparison with national influenza surveillance systems. Influenza Respi. Viruses 2014, 8, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Liu, D.; Wei, K.; Liu, X.; Meng, L.; Yu, D.; Li, H.; Li, B.; He, J.; Hu, W. Comparing the similarity and difference of three influenza surveillance systems in China. Sci. Rep. 2018, 8, 2840. [Google Scholar] [CrossRef] [PubMed]
- Torner, N.; Basile, L.; Martínez, A.; Rius, C.; Godoy, P.; Jané, M.; Domínguez, Á.; Aizpurua, J.; Alonso, J.; Azemar, J.; et al. Assessment of two complementary influenza surveillance systems: Sentinel primary care influenza-like illness versus severe hospitalized laboratory-confirmed influenza using the moving epidemic method. BMC Public Health 2019, 19, 1089. [Google Scholar] [CrossRef] [PubMed]
- Páscoa, R.; Rodrigues, A.P.; Silva, S.; Nunes, B.; Martins, C. Comparison between influenza coded primary care consultations and national influenza incidence obtained by the General Practitioners Sentinel Network in Portugal from 2012 to 2017. PLoS ONE 2018, 13, e0192681. [Google Scholar] [CrossRef] [PubMed]
- Truyers, C.; Lesaffre, E.; Bartholomeeusen, S.; Aertgeerts, B.; Snacken, R.; Brochier, B.; Yane, F.; Buntinx, F. Computerized general practice based networks yield comparable performance with sentinel data in monitoring epidemiological time-course of influenza-like illness and acute respiratory illness. BMC. Fam. Pract. 2010, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Perrotta, D.; Bella, A.; Rizzo, C.; Paolotti, D. Participatory Online Surveillance as a Supplementary Tool to Sentinel Doctors for Influenza-Like Illness Surveillance in Italy. PLoS ONE 2017, 12, e0169801. [Google Scholar] [CrossRef]
- Krieger, N.; Chen, J.T.; Waterman, P.D. Decline in US breast cancer rates after the Women’s Health Initiative: Socioeconomic and racial/ethnic differentials. Am. J. Public Health 2010, 100, 132–139. [Google Scholar] [CrossRef]
- Lynch, B.; Fitzgerald, A.P.; Corcoran, P.; Healy, O.; Buckley, C.; Foley, C.; Browne, J. Case fatality ratios for serious emergency conditions in the Republic of Ireland: A longitudinal investigation of trends over the period 2002-2014 using joinpoint analysis. BMC Health Serv. Res. 2018, 18, 474. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- National Cancer Institute. Joinpoint Regression Program. 2020. Available online: https://surveillance.cancer.gov/joinpoint/ (accessed on 15 September 2022).
- Vega, T.; Lozano, J.E.; Meerhoff, T.; Snacken, R.; Mott, J.; Ortiz de Lejarazu, R.; Nunes, B. Influenza surveillance in Europe: Establishing epidemic thresholds by the Moving Epidemic Method. Influenza Respi. Viruses 2012, 7, 546–558. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Molnar, A.; Iancu, M.; Radu, R.; Borzan, C.M. A Joinpoint Regression Analysis of Syphilis and Gonorrhea Incidence in 15–19-Year Old Adolescents between 2005 and 2017: A Regional Study. Int. J. Environ. Res. Public Health 2020, 17, 5385. [Google Scholar] [CrossRef] [PubMed]
- De Paula, A.; Cardoso-dos-santos, A.C.; Souza, M. COVID-19 Epidemic in Brazil: Where Are We at? Int. J. Infect. Dis. 2020, 97, 382–385. [Google Scholar]
- Hswen, Y.; Brownstein, J.S.; Xu, X.; Yom-Tov, E. Early detection of COVID-19 in China and the USA: Summary of the implementation of a digital decision-support and disease surveillance tool. BMJ Open 2020, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Drevon, D.; Fursa, S.R.; Malcolm, A.L. Intercoder Reliability and Validity of WebPlotDigitizer in Extracting Graphed Data. Behav. Modif. 2017, 41, 323–339. [Google Scholar] [CrossRef]
- Moeyaert, M.; Maggin, D.; Verkuilen, J. Reliability, Validity, and Usability of Data Extraction Programs for Single-Case Research Designs. Behav. Modif. 2016, 40, 874–900. [Google Scholar] [CrossRef] [PubMed]
- Burda, B.U.; O’Connor, E.A.; Webber, E.M.; Redmond, N.; Perdue, L.A. Estimating data from figures with a Web-based program: Considerations for a systematic review. Res. Synth. Methods 2017, 8, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Canal Salut Pla D’informació de les Infeccions Respiratòries Agudes a Catalunya (PIDIRAC). Canal Salut. Available online: https://canalsalut.gencat.cat/ca/professionals/vigilancia-epidemiologica/pla-dinformacio-de-les-infeccions-respiratories-agudes-a-catalunya-pidirac/ (accessed on 15 September 2022).
- Instituto de Salud Carlos III; Red Nacional Vigilancia de Epidemiológica (RENAVE). Sistema de Vigilancia de la Gripe en España. Available online: https://vgripe.isciii.es/inicio.do (accessed on 6 September 2022).


| Variable | Clinical Diagnosis | Sentinel-Confirmed | Total Confirmed |
|---|---|---|---|
| Source | DiagnostiCat, now SIVIC | PIDIRAC | SISS |
| Source Description | Open public website. Secondary data. Weekly update. Published on Sunday of the registration week. https://sivic.salut.gencat.cat/ (accessed on 9 September 2022) | Public website. Secondary data. Weekly update. Published on Thursday following week of registration. https://canalsalut.gencat.cat/ca/professionals/vigilancia-epidemiologica/pla-dinformacio-de-les-infeccions-respiratories-agudes-a-catalunya-pidirac/ (accessed on 15 September 2022) | Public website. Secondary data. Weekly update. Published on Thursday following week of registration. http://vgripe.isciii.es/PresentarGraficos.do (accessed on 15 September 2022) |
| Method of acquisition | Download from website | WebPlotDigitizer * https://apps.automeris.io/wpd/ (accessed on 15 September 2022) | WebPlotDigitizer * https://apps.automeris.io/wpd/ (accessed on 15 September 2022) |
| Origin of data | Primary Care of Catalonia, from the Institut Català de la Salut (ICS) | Primary Care sentinel doctors of Catalonia | Hospitals and centres that carry out confirmatory laboratory diagnostic tests in Catalonia |
| Description of data | Public clinical diagnosis data from SISCAT and other health services in Catalonia that use eCAP (all the ages and sex are included) | Cases confirmed by the network of sentinel doctors in Catalonia, which publishes weekly reports in the Pla d’Informació d’Infections Respiratòries Agudes in Catalonia (all the ages and sex are included) Laboratory confirmation by PCR | Cases confirmed by sentinel doctors and all cases confirmed outside the sentinel network (non-sentinel) (all the ages and sex are included) Laboratory confirmation by PCR |
| Calculation of rates |
| Influenza Season | Starting Week of Epidemic. Threshold: MEM Sentinel-Confirmed Reference | Starting Week of Epidemic. Threshold: MEM Clinical Diagnosis | Week Change Trend Clinical Diagnosis | Week Change Trend Sentinel-Confirmed | Week Change of Trend Total Confirmed |
|---|---|---|---|---|---|
| 2010–2011 | 49/2010 | 50/2010 | 49/2010 | 47/2010 | 46/2010 |
| 2011–2012 | 2/2012 | 4/2012 | 1/2012 | 51/2011 | 1/2012 |
| 2012–2013 | 51/2012 | 2/2013 | 2/2013 | 1/2013 | 1/2013 |
| 2013–2014 | 51/2013 | 52/2013 | 50/2013 | 48/2013 | 50/2013 |
| 2014–2015 | 3/2015 | 52/2014 | 49/2014 | 1/2015 | 1/2015 |
| 2015–2016 | 4/2016 | 3/2015 | 1/2016 | 2/2016 | 2/2016 |
| 2016–2017 | 50/2016 | 50/2015 | 47/2016 | 48/2016 | 49/2016 |
| 2017–2018 | 50/2017 | 50/2017 | 48/2017 | 48/2017 | 50/2017 |
| 2018–2019 | 2/2019 | 52/2018 | 50/2018 | 46/2018 | 52/2018 |
| Time Lag (CCF Value) | ||
|---|---|---|
| Influenza Season | Comparison | Pre-Whitened CCF |
| 2010–2011 | Clinical diagnoses—Sentinel-confirmed | −2 (0.395) |
| Clinical diagnoses—Total confirmed | 0 (0.372) | |
| 2011–2012 | Clinical diagnoses—Sentinel-confirmed | NS |
| Clinical diagnoses—Total confirmed | 0 (0.649) | |
| 2012–2013 | Clinical diagnoses—Sentinel-confirmed | 1 (0.443) |
| Clinical diagnoses—Total confirmed | 1 (0.495) | |
| 2013–2014 | Clinical diagnoses—Sentinel-confirmed | 3 (−0.375) |
| Clinical diagnoses—Total confirmed | 3 (−0.398) | |
| 2014–2015 | Clinical diagnoses—Sentinel-confirmed | −2 (0.488) |
| Clinical diagnoses—Total confirmed | −3 (0.772) | |
| 2015–2016 | Clinical diagnoses—Sentinel-confirmed | −1 (0.421) |
| Clinical diagnoses—Total confirmed | 0 (0.650) | |
| 2016–2017 | Clinical diagnoses—Sentinel-confirmed | 1 (0.460) |
| Clinical diagnoses—Total confirmed | 0 (0.388) | |
| 2017–2018 | Clinical diagnoses—Sentinel-confirmed | −1 (0.628) |
| Clinical diagnoses—Total confirmed | 0 (0.497) | |
| 2018–2019 | Clinical diagnoses—Sentinel-confirmed | 0 (0.440) |
| Clinical diagnoses—Total confirmed | 0 (0.452) | |
| Global | Clinical diagnoses—Sentinel-confirmed | 1 (0.163)/−1 (0.149) |
| Clinical diagnoses—Total confirmed | 0 (0.401) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dalmau Llorca, M.R.; Castro Blanco, E.; Aguilar Martín, C.; Carrasco-Querol, N.; Hernández Rojas, Z.; Gonçalves, A.Q.; Fernández-Sáez, J. Early Detection of the Start of the Influenza Epidemic Using Surveillance Systems in Catalonia (PREVIGrip Study). Int. J. Environ. Res. Public Health 2022, 19, 17048. https://doi.org/10.3390/ijerph192417048
Dalmau Llorca MR, Castro Blanco E, Aguilar Martín C, Carrasco-Querol N, Hernández Rojas Z, Gonçalves AQ, Fernández-Sáez J. Early Detection of the Start of the Influenza Epidemic Using Surveillance Systems in Catalonia (PREVIGrip Study). International Journal of Environmental Research and Public Health. 2022; 19(24):17048. https://doi.org/10.3390/ijerph192417048
Chicago/Turabian StyleDalmau Llorca, M. Rosa, Elisabet Castro Blanco, Carina Aguilar Martín, Noèlia Carrasco-Querol, Zojaina Hernández Rojas, Alessandra Queiroga Gonçalves, and José Fernández-Sáez. 2022. "Early Detection of the Start of the Influenza Epidemic Using Surveillance Systems in Catalonia (PREVIGrip Study)" International Journal of Environmental Research and Public Health 19, no. 24: 17048. https://doi.org/10.3390/ijerph192417048
APA StyleDalmau Llorca, M. R., Castro Blanco, E., Aguilar Martín, C., Carrasco-Querol, N., Hernández Rojas, Z., Gonçalves, A. Q., & Fernández-Sáez, J. (2022). Early Detection of the Start of the Influenza Epidemic Using Surveillance Systems in Catalonia (PREVIGrip Study). International Journal of Environmental Research and Public Health, 19(24), 17048. https://doi.org/10.3390/ijerph192417048








