Epidemiology and Management of Proximal Femoral Fractures in Italy between 2001 and 2016 in Older Adults: Analysis of the National Discharge Registry
Abstract
1. Introduction
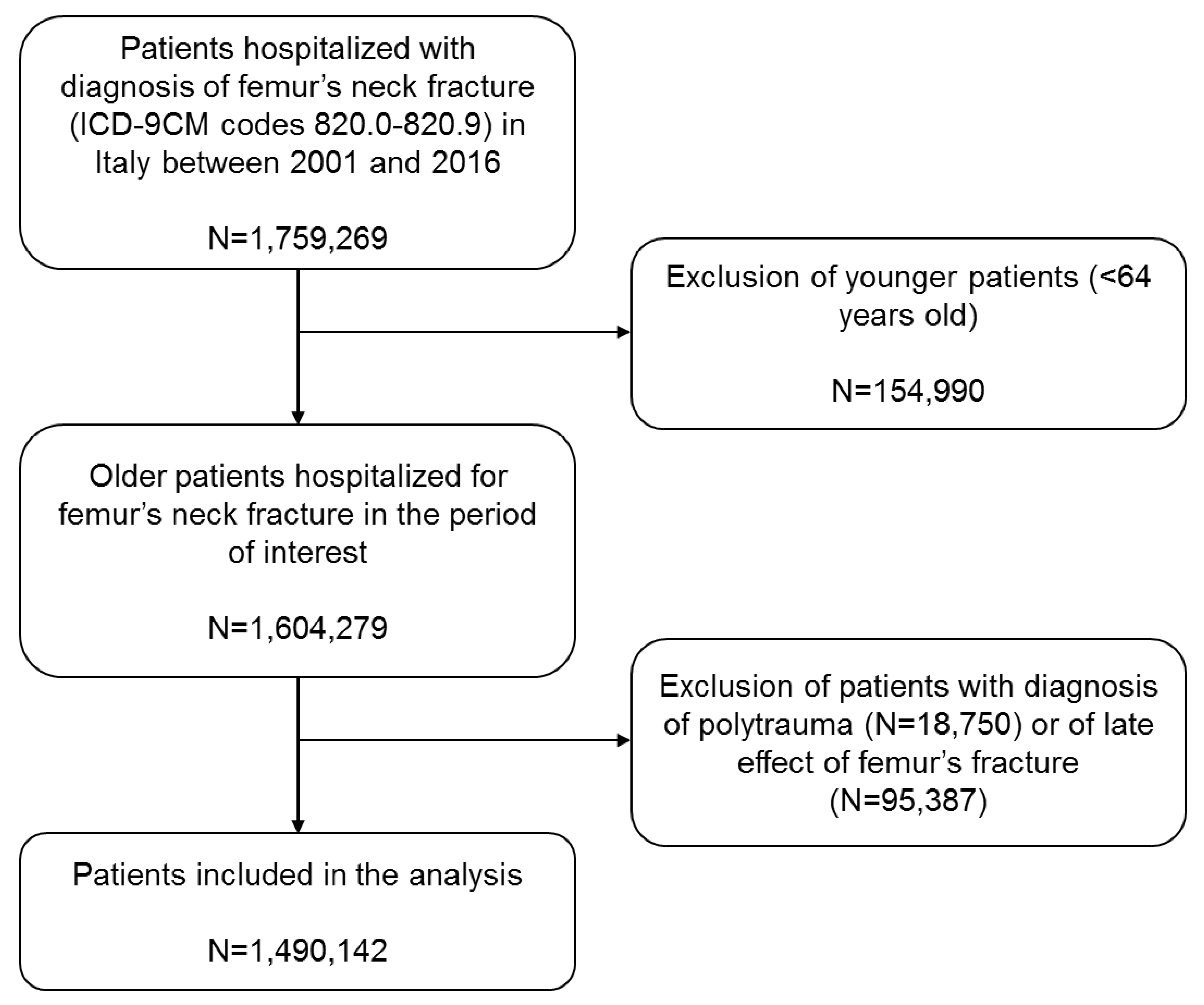
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
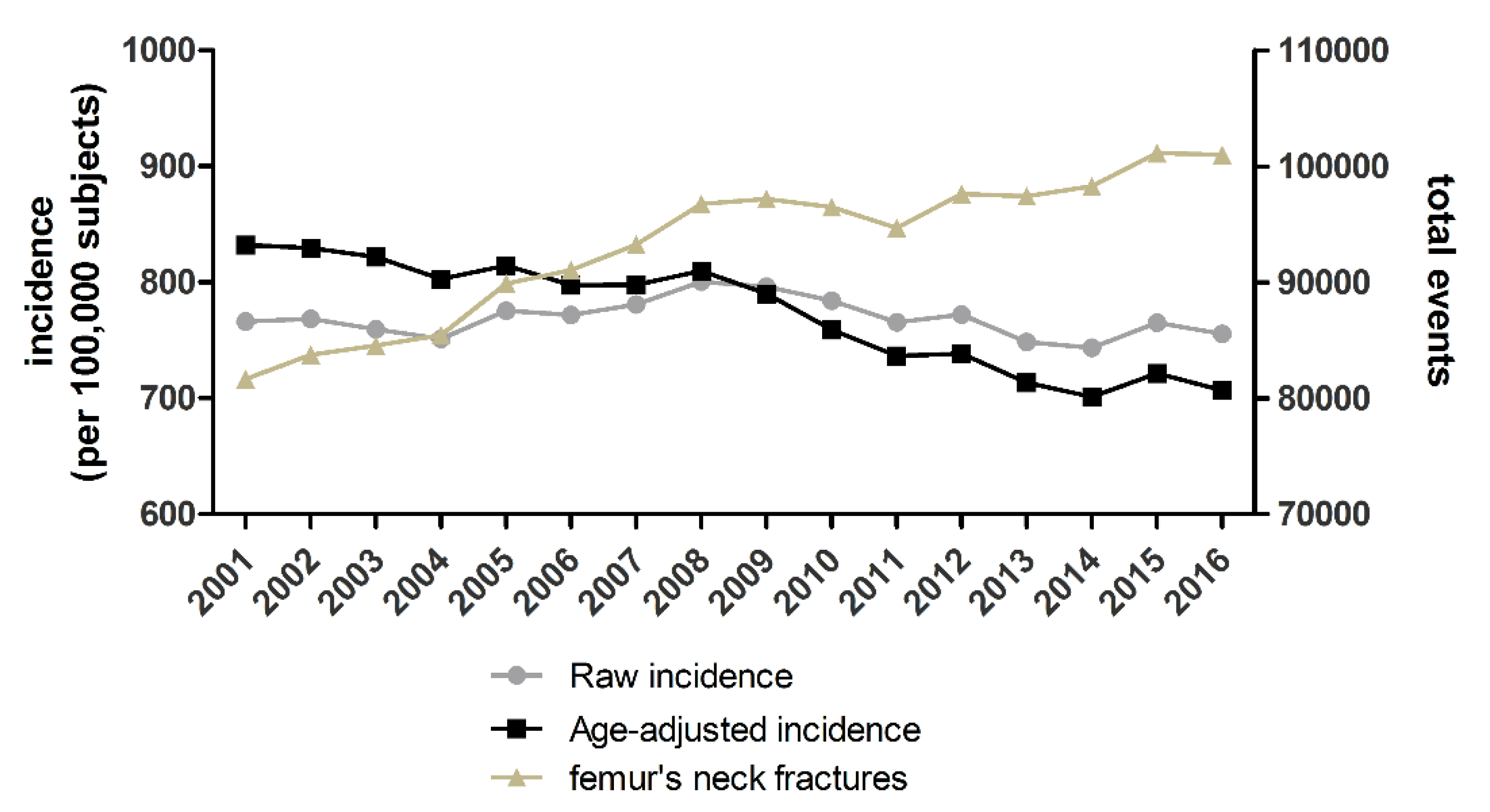
3.1. Total Number and Incidence of Hospitalizations in the Analyzed Period
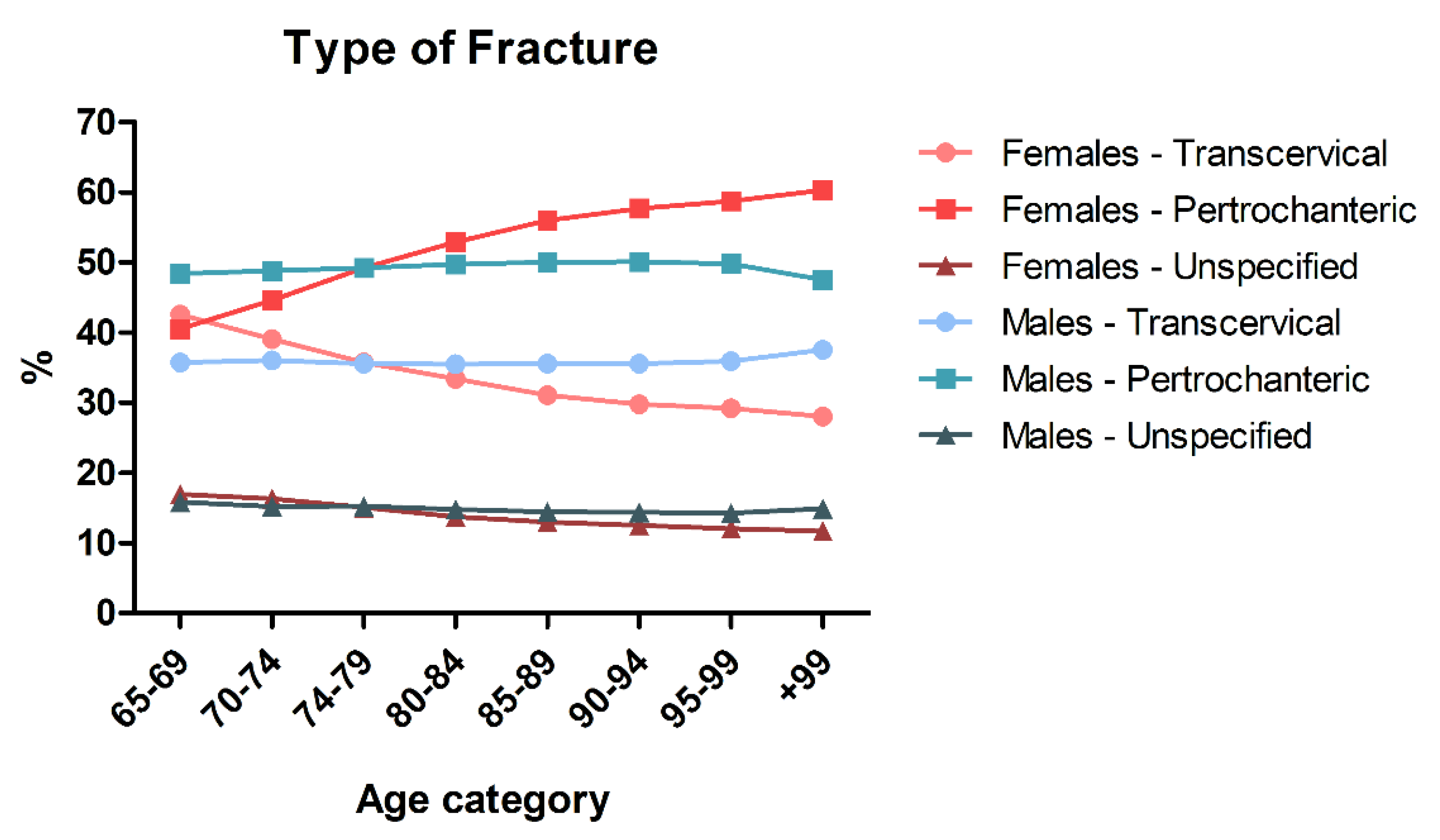
3.2. Type of Fracture Differs Based on Gender and Age
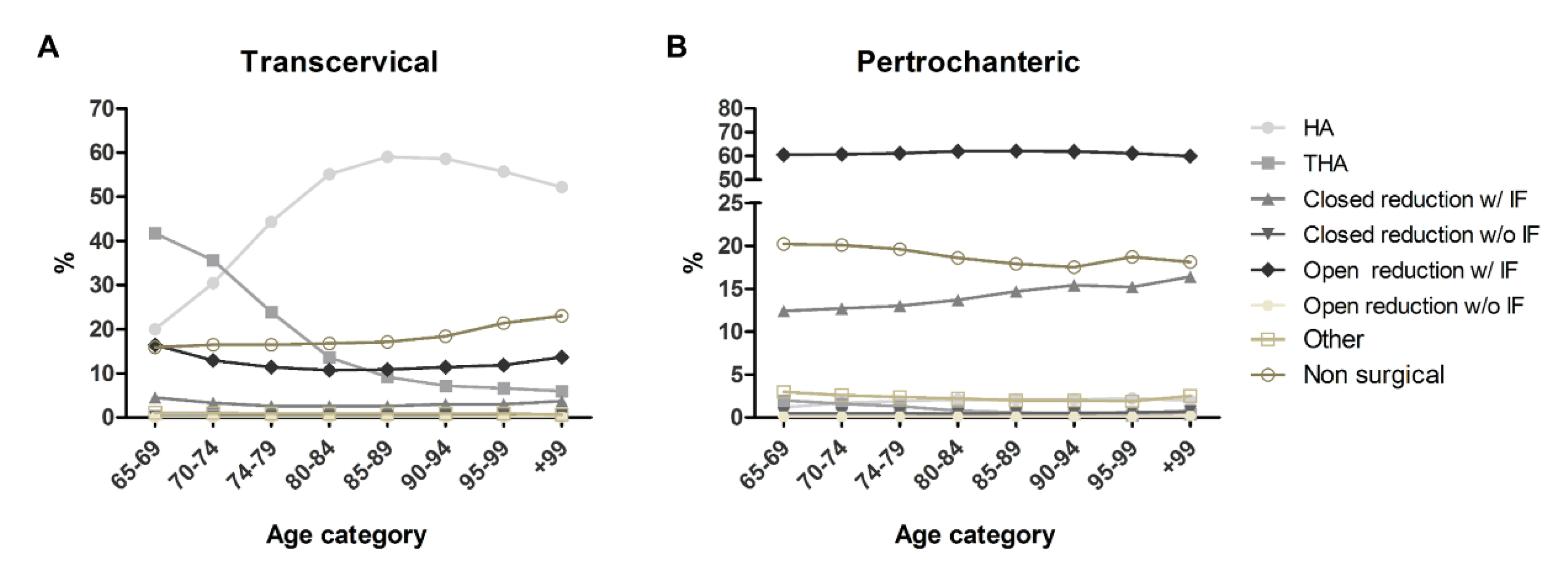
3.3. Fracture Management in Different Patients and Types of Fracture
3.4. Trends in Treatment Strategies during Study Years
3.5. Length of Hospitalization
3.6. Associated Diagnosis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Florschutz, A.V.; Langford, J.R.; Haidukewych, G.J.; Koval, K.J. Femoral Neck Fractures: Current Management. J. Orthop. Trauma 2015, 29, 121–129. [Google Scholar] [CrossRef]
- Forsh, D.A.; Ferguson, T.A. Contemporary Management of Femoral Neck Fractures: The Young and the Old. Curr. Rev. Musculoskelet Med. 2012, 5, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Guyen, O. Hemiarthroplasty or Total Hip Arthroplasty in Recent Femoral Neck Fractures? Orthop. Traumatol. Surg. Res. 2019, 105, S95–S101. [Google Scholar] [CrossRef]
- Roberts, K.C.; Brox, W.T.; Jevsevar, D.S.; Sevarino, K. Management of Hip Fractures in the Elderly. JAAOS-J. Am. Acad. Orthop. Surg. 2015, 23, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Lutnick, E.; Kang, J.; Freccero, D.M. Surgical Treatment of Femoral Neck Fractures: A Brief Review. Geriatrics 2020, 5, 22. [Google Scholar] [CrossRef] [PubMed]
- Ko, F.C.; Morrison, R.S. Hip Fracture: A Trigger for Palliative Care in Vulnerable Older Adults. JAMA Intern. Med. 2014, 174, 1281–1282. [Google Scholar] [CrossRef]
- Balasegaram, S.; Majeed, A.; Fitz-Clarence, H. Trends in Hospital Admissions for Fractures of the Hip and Femur in England, 1989–1990 to 1997–1998. J. Public Health Med. 2001, 23, 11–17. [Google Scholar] [CrossRef]
- Boufous, S.; Finch, C.F.; Lord, S.R. Incidence of Hip Fracture in New South Wales: Are Our Efforts Having an Effect? Med. J. Aust. 2004, 180, 623–626. [Google Scholar] [CrossRef]
- Cicvarić, T.; Bencević-Striehl, H.; Juretić, I.; Marinović, M.; Grzalja, N.; Ostrić, M. Hip Fractures in Elderly—Ten Years Analysis. Coll. Antropol. 2010, 34 (Suppl. S2), 199–204. [Google Scholar]
- Hagino, H.; Osaki, M.; Okuda, R.; Enokida, S.; Nagashima, H. Recent Trends in the Incidence of Hip Fracture in Tottori Prefecture, Japan: Changes over 32 Years. Arch. Osteoporos. 2020, 15, 152. [Google Scholar] [CrossRef]
- Langley, J.; Samaranayaka, A.; Davie, G.; Campbell, A.J. Age, Cohort and Period Effects on Hip Fracture Incidence: Analysis and Predictions from New Zealand Data 1974–2007. Osteoporos. Int. 2011, 22, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Lehtonen, E.J.I.; Stibolt, R.D.; Smith, W.; Wills, B.; Pinto, M.C.; McGwin, G.; Shah, A.; Godoy-Santos, A.L.; Naranje, S. Trends in Surgical Treatment of Femoral Neck Fractures in the Elderly. Einstein 2018, 16, eAO4351. [Google Scholar] [CrossRef] [PubMed]
- Requena, G.; Abbing-Karahagopian, V.; Huerta, C.; De Bruin, M.L.; Alvarez, Y.; Miret, M.; Hesse, U.; Gardarsdottir, H.; Souverein, P.C.; Slattery, J.; et al. Incidence Rates and Trends of Hip/Femur Fractures in Five European Countries: Comparison Using e-Healthcare Records Databases. Calcif. Tissue Int. 2014, 94, 580–589. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, S.; Langley, J.; Campbell, J.; Gillespie, W. Upward Trends in the Incidence of Neck of Femur Fractures in the Elderly. N. Z. Med. J. 2003, 116, U665. [Google Scholar] [PubMed]
- Wilk, R.; Skrzypek, M.; Kowalska, M.; Kusz, D.; Koczy, B.; Zagórski, P.; Pluskiewicz, W. The 13-Year Observation of Hip Fracture in Poland-Worrying Trend and Prognosis for the Future. Aging Clin. Exp. Res. 2018, 30, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Ju, D.G.; Rajaee, S.S.; Mirocha, J.; Lin, C.A.; Moon, C.N. Nationwide Analysis of Femoral Neck Fractures in Elderly Patients: A Receding Tide. J. Bone Joint Surg. Am. 2017, 99, 1932–1940. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.J.; Lu, X.; Cram, P. The Trends in Treatment of Femoral Neck Fractures in the Medicare Population from 1991 to 2008. J. Bone Joint Surg. Am. 2013, 95, e132. [Google Scholar] [CrossRef] [PubMed]
- Gehlbach, S.H.; Avrunin, J.S.; Puleo, E. Trends in Hospital Care for Hip Fractures. Osteoporos. Int. 2007, 18, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Leslie, W.D.; O’Donnell, S.; Jean, S.; Lagacé, C.; Walsh, P.; Bancej, C.; Morin, S.; Hanley, D.A.; Papaioannou, A. Osteoporosis Surveillance Expert Working Group Trends in Hip Fracture Rates in Canada. JAMA 2009, 302, 883–889. [Google Scholar] [CrossRef]
- Wang, Z.; Bhattacharyya, T. Trends in Incidence of Subtrochanteric Fragility Fractures and Bisphosphonate Use among the US Elderly, 1996–2007. J. Bone Miner. Res. 2011, 26, 553–560. [Google Scholar] [CrossRef]
- MacKinlay, K.; Falls, T.; Lau, E.; Day, J.; Kurtz, S.; Ong, K.; Malkani, A. Decreasing Incidence of Femoral Neck Fractures in the Medicare Population. Orthopedics 2014, 37, e917–e924. [Google Scholar] [CrossRef] [PubMed]
- Brauer, C.A.; Coca-Perraillon, M.; Cutler, D.M.; Rosen, A.B. Incidence and Mortality of Hip Fractures in the United States. JAMA 2009, 302, 1573–1579. [Google Scholar] [CrossRef]
- Araujo, T.P.F.; Guimaraes, T.M.; Andrade-Silva, F.B.; Kojima, K.E.; Silva, J.D.S. Influence of Time to Surgery on the Incidence of Complications in Femoral Neck Fracture Treated with Cannulated Screws. Injury 2014, 45 (Suppl. S5), S36–S39. [Google Scholar] [CrossRef] [PubMed]
- Major, L.J.; North, J.B. Predictors of Mortality in Patients with Femoral Neck Fracture. J. Orthop. Surg. 2016, 24, 150–152. [Google Scholar] [CrossRef] [PubMed]
- Mabry, S.E.; Cichos, K.H.; McMurtrie, J.T.; Pearson, J.M.; McGwin, G.; Ghanem, E.S. Does Surgeon Fellowship Training Influence Outcomes in Hemiarthroplasty for Femoral Neck Fracture? J. Arthroplast. 2019, 34, 1980–1986. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Popolazione Residente al 1° Gennaio. Available online: http://dati.istat.it/Index.aspx?QueryId=18460 (accessed on 27 June 2022).
- Linee Guida per La Qualità Delle Statistiche Del Sistema Statistico Nazionale. Available online: https://www.istat.it/it/files/2018/08/Linee-Guida-2.5-agosto-2018.pdf (accessed on 9 December 2022).
- LeLaurin, J.H.; Shorr, R.I. Preventing Falls in Hospitalized Patients: State of the Science. Clin. Geriatr. Med. 2019, 35, 273–283. [Google Scholar] [CrossRef]
- Hempel, S.; Newberry, S.; Wang, Z.; Booth, M.; Shanman, R.; Johnsen, B.; Shier, V.; Saliba, D.; Spector, W.D.; Ganz, D.A. Hospital Fall Prevention: A Systematic Review of Implementation, Components, Adherence, and Effectiveness. J. Am. Geriatr. Soc. 2013, 61, 483–494. [Google Scholar] [CrossRef]
- Campani, D.; Caristia, S.; Amariglio, A.; Piscone, S.; Ferrara, L.I.; Barisone, M.; Bortoluzzi, S.; Faggiano, F.; Dal Molin, A.; IPEST Working Group. Home and Environmental Hazards Modification for Fall Prevention among the Elderly. Public Health Nurs. 2020, 38, 493–501. [Google Scholar] [CrossRef]
- Rossini, M.; Adami, S.; Bertoldo, F.; Diacinti, D.; Gatti, D.; Giannini, S.; Giusti, A.; Malavolta, N.; Minisola, S.; Osella, G.; et al. Guidelines for the Diagnosis, Prevention and Management of Osteoporosis. Reumatismo 2016, 68, 1–39. [Google Scholar] [CrossRef]
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and Economic Burden of Osteoporosis-Related Fractures in the United States, 2005–2025. J. Bone Miner. Res. 2007, 22, 465–475. [Google Scholar] [CrossRef]
- Hagino, H.; Furukawa, K.; Fujiwara, S.; Okano, T.; Katagiri, H.; Yamamoto, K.; Teshima, R. Recent Trends in the Incidence and Lifetime Risk of Hip Fracture in Tottori, Japan. Osteoporos. Int. 2009, 20, 543–548. [Google Scholar] [CrossRef]
- Switzer, J.A.; O’Connor, M. American Academy of Orthopaedic Surgeons Management of Hip Fractures in Older Adults Evidence-Based Clinical Practice Guideline. J. Am. Acad. Orthop. Surg. 2021, 30, e1297–e1301. [Google Scholar] [CrossRef]
- Cram, P.; Yan, L.; Bohm, E.; Kuzyk, P.; Lix, L.M.; Morin, S.N.; Majumdar, S.R.; Leslie, W.D. Trends in Operative and Nonoperative Hip Fracture Management 1990-2014: A Longitudinal Analysis of Manitoba Administrative Data. J. Am. Geriatr. Soc. 2017, 65, 27–34. [Google Scholar] [CrossRef]
- Stronach, B.M.; Bergin, P.F.; Perez, J.L.; Watson, S.; Jones, L.C.; McGwin, G.; Ponce, B.A. The Rising Use of Total Hip Arthroplasty for Femoral Neck Fractures in the United States. Hip Int. 2020, 30, 107–113. [Google Scholar] [CrossRef]
- Hongisto, M.T.; Pihlajamäki, H.; Niemi, S.; Nuotio, M.; Kannus, P.; Mattila, V.M. Surgical Procedures in Femoral Neck Fractures in Finland: A Nationwide Study between 1998 and 2011. Int. Orthop. 2014, 38, 1685–1690. [Google Scholar] [CrossRef]
- Harris, I.A.; Cuthbert, A.; de Steiger, R.; Lewis, P.; Graves, S.E. Practice Variation in Total Hip Arthroplasty versus Hemiarthroplasty for Treatment of Fractured Neck of Femur in Australia. Bone Joint J. 2019, 101-B, 92–95. [Google Scholar] [CrossRef]
- Lee, Y.-K.; Ha, Y.-C.; Park, C.; Koo, K.-H. Trends of Surgical Treatment in Femoral Neck Fracture: A Nationwide Study Based on Claim Registry. J. Arthroplast. 2013, 28, 1839–1841. [Google Scholar] [CrossRef]
- Bishop, J.; Yang, A.; Githens, M.; Sox, A.H.S. Evaluation of Contemporary Trends in Femoral Neck Fracture Management Reveals Discrepancies in Treatment. Geriatr. Orthop. Surg. Rehabil. 2016, 7, 135–141. [Google Scholar] [CrossRef]
- Ekhtiari, S.; Gormley, J.; Axelrod, D.E.; Devji, T.; Bhandari, M.; Guyatt, G.H. Total Hip Arthroplasty Versus Hemiarthroplasty for Displaced Femoral Neck Fracture: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Bone Joint Surg. Am. 2020, 102, 1638–1645. [Google Scholar] [CrossRef]
- Roberts, K.C.; Brox, W.T. AAOS Clinical Practice Guideline: Management of Hip Fractures in the Elderly. JAAOS J. Am. Acad. Orthop. Surg. 2015, 23, 138–140. [Google Scholar] [CrossRef]
- Hochfelder, J.P.; Khatib, O.N.; Glait, S.A.; Slover, J.D. Femoral Neck Fractures in New York State. Is the Rate of THA Increasing, and Do Race or Payer Influence Decision Making? J. Orthop. Trauma 2014, 28, 422–426. [Google Scholar] [CrossRef]
- Cree, M.; Yang, Q.; Scharfenberger, A.; Johnson, D.; Carrière, K.C. Variations in Treatment of Femoral Neck Fractures in Alberta. Can. J. Surg. 2002, 45, 248–254. [Google Scholar]
- OECD. Average Length of Stay in Hospitals; OECD: Paris, France, 2017; pp. 176–177. [Google Scholar] [CrossRef]
- Bottle, A.; Aylin, P. Mortality Associated with Delay in Operation after Hip Fracture: Observational Study. BMJ 2006, 332, 947–951. [Google Scholar] [CrossRef]
- Bretherton, C.P.; Parker, M.J. Early Surgery for Patients with a Fracture of the Hip Decreases 30-Day Mortality. Bone Jt. J. 2015, 97-B, 104–108. [Google Scholar] [CrossRef]
- Gundel, O.; Thygesen, L.C.; Gögenur, I.; Ekeloef, S. Postoperative Mortality after a Hip Fracture over a 15-Year Period in Denmark: A National Register Study. Acta Orthop. 2020, 91, 58–62. [Google Scholar] [CrossRef]
- Wu, T.Y.; Hu, H.Y.; Lin, S.Y.; Chie, W.C.; Yang, R.S.; Liaw, C.K. Trends in Hip Fracture Rates in Taiwan: A Nationwide Study from 1996 to 2010. Osteoporos. Int. 2017, 28, 653–665. [Google Scholar] [CrossRef]
- Rajeev, A.; Ali, M.; Tuinebreijer, W.; Zourob, E.; Anto, J. Preexisting Dementia Is Associated with Higher Mortality Rate in Patients with Femoral Neck Fracture. Aging Med. 2021, 4, 12–18. [Google Scholar] [CrossRef]
- Du, M.-J.; Lin, Y.-H.; Chen, W.-T.; Zhao, H. Advances in the Application of Ultrasound for Fracture Diagnosis and Treatment. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 7949–7954. [Google Scholar] [CrossRef]
- Tornetta, P.; Kain, M.S.H.; Creevy, W.R. Diagnosis of Femoral Neck Fractures in Patients with a Femoral Shaft Fracture. Improvement with a Standard Protocol. J. Bone Jt. Surg. Am. 2007, 89, 39–43. [Google Scholar] [CrossRef]
- Saarenpää, I.; Partanen, J.; Jalovaara, P. Basicervical Fracture—A Rare Type of Hip Fracture. Arch. Orthop. Trauma Surg. 2002, 122, 69–72. [Google Scholar] [CrossRef]

| Males | Females | Total | |
|---|---|---|---|
| Events | 348,426 (23.4%) | 1,141,716 (76.6%) | 1,490,142 |
| Age, years (Median, IQR) | 82 (77–87) | 83 (78–88) | 83 (78–88) |
| 820.01 | 820.02 | 820.03 | 820.11 | 820.12 | 820.13 | 820.20 | 820.21 | 820.22 | 820.30 | 820.31 | 820.32 | Unspecified | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 5091 (6.2%) | 6583 (8.1%) | 9206 (11.3%) | 78 (0.1%) | 324 (0.4%) | 348 (0.4%) | 25,643 (31.4%) | 10,149 (12.4%) | 2909 (3.6%) | 345 (0.4%) | 219 (0.3%) | 211 (0.3%) | 20,542 (25.2%) |
| 2002 | 7855 (9.4%) | 8186 (9.8%) | 9551 (11.4%) | 69 (0.1%) | 296 (0.4%) | 298 (0.4%) | 26,478 (31.6%) | 10,512 (12.5%) | 3473 (4.1%) | 257 (0.3%) | 138 (0.2%) | 202 (0.2%) | 16,448 (19.6%) |
| 2003 | 10,345 (12.2%) | 8559 (10.1%) | 8643 (10.2%) | 35 (0%) | 269 (0.3%) | 267 (0.3%) | 28,361 (33.5%) | 9557 (11.3%) | 3774 (4.5%) | 240 (0.3%) | 110 (0.1%) | 129 (0.2%) | 14,250 (16.9%) |
| 2004 | 11,445 (13.4%) | 8868 (10.4%) | 8303 (9.7%) | 42 (0%) | 248 (0.3%) | 228 (0.3%) | 29,277 (34.3%) | 9016 (10.5%) | 4019 (4.7%) | 229 (0.3%) | 120 (0.1%) | 154 (0.2%) | 13,512 (15.8%) |
| 2005 | 12,965 (14.4%) | 9717 (10.8%) | 8345 (9.3%) | 52 (0.1%) | 249 (0.3%) | 206 (0.2%) | 30,535 (34%) | 9539 (10.6%) | 4275 (4.8%) | 314 (0.3%) | 145 (0.2%) | 147 (0.2%) | 13,406 (14.9%) |
| 2006 | 13,490 (14.8%) | 9697 (10.7%) | 8103 (8.9%) | 35 (0%) | 198 (0.2%) | 209 (0.2%) | 31,438 (34.5%) | 9667 (10.6%) | 4569 (5%) | 271 (0.3%) | 211 (0.2%) | 158 (0.2%) | 12,991 (14.3%) |
| 2007 | 13,855 (14.9%) | 10,107 (10.8%) | 7724 (8.3%) | 51 (0.1%) | 253 (0.3%) | 254 (0.3%) | 32,344 (34.7%) | 10,161 (10.9%) | 5101 (5.5%) | 305 (0.3%) | 231 (0.2%) | 171 (0.2%) | 12,703 (13.6%) |
| 2008 | 13,978 (14.4%) | 10,269 (10.6%) | 7961 (8.2%) | 49 (0.1%) | 302 (0.3%) | 321 (0.3%) | 33,799 (34.9%) | 10,741 (11.1%) | 5173 (5.3%) | 369 (0.4%) | 266 (0.3%) | 188 (0.2%) | 13,323 (13.8%) |
| 2009 | 14,038 (14.4%) | 10,518 (10,8%) | 7432 (7.6%) | 45 (0%) | 360 (0.4%) | 251 (0.3%) | 34,103 (35.1%) | 11,352 (11.7%) | 5369 (5.5%) | 433 (0.4%) | 309 (0.3%) | 185 (0.2%) | 12,786 (13.2%) |
| 2010 | 14,771 (15.3%) | 11,005 (11.4%) | 6871 (7.1%) | 76 (0.1%) | 413 (0.4%) | 186 (0.2%) | 34,333 (35.6%) | 10,657 (11%) | 5596 (5.8%) | 396 (0.4%) | 312 (0.3%) | 153 (0.2%) | 11,704 (12.1%) |
| 2011 | 15,075 (15.9%) | 10,964 (11.6%) | 6685 (7.1%) | 117 (0.1%) | 435 (0.5%) | 165 (0.2%) | 33,158 (35%) | 10,583 (11.2%) | 5457 (5.8%) | 312 (0.3%) | 357 (0.4%) | 165 (0.2%) | 11,225 (11.9%) |
| 2012 | 15,512 (15.9%) | 10,739 (11%) | 6671 (6.8%) | 144 (0.1%) | 534 (0.5%) | 198 (0.2%) | 34,192 (35%) | 11,737 (12%) | 5400 (5.5%) | 306 (0.3%) | 393 (0.4%) | 185 (0.2%) | 11,593 (11.9%) |
| 2013 | 15,733 (16.2%) | 11,360 (11.7%) | 6297 (6.5%) | 170 (0.2%) | 556 (0.6%) | 160 (0.2%) | 33,698 (34.6%) | 11,988 (12.3%) | 5386 (5.5%) | 332 (0.3%) | 361 (0.4%) | 146 (0.1%) | 11,214 (11.5%) |
| 2014 | 16,177 (16.5%) | 11,238 (11.4%) | 6155 (6.3%) | 109 (0.1%) | 717 (0.7%) | 176 (0.2%) | 33,930 (34.5%) | 11,966 (12.2%) | 5511 (5.6%) | 301 (0.3%) | 523 (0.5%) | 172 (0.2%) | 11,322 (11.5%) |
| 2015 | 16,430 (16.2%) | 11,677 (11.5%) | 6051 (6%) | 144 (0.1%) | 808 (0.8%) | 234 (0.2%) | 34,033 (33.6%) | 13,152 (13%) | 5939 (5.9%) | 370 (0.4%) | 564 (0.6%) | 208 (0.2%) | 11,538 (11.4%) |
| 2016 | 15,748 (15.6%) | 11,760 (11.6%) | 5867 (5.8%) | 242 (0.2%) | 809 (0.8%) | 283 (0.3%) | 34,177 (33.8%) | 13,338 (13.2%) | 5620 (5.6%) | 419 (0.4%) | 594 (0.6%) | 239 (0.2%) | 11,902 (11.8%) |
| HA | THA | CRwIF | CRw/oIF | ORwIF | ORw/oIF | Other | Non-Surgical | |
|---|---|---|---|---|---|---|---|---|
| 82,001 | 117,300 (55.2%) | 43,928 (20.7%) | 2706 (1.3%) | 394 (0.2%) | 14,297 (6.7%) | 18 (0%) | 1491 (0.7%) | 32,374 (15.2%) |
| 82,002 | 85,760 (53.2%) | 30,232 (18.7%) | 4963 (3.1%) | 271 (0.2%) | 13,817 (8.6%) | 28 (0%) | 1414 (0.9%) | 24,762 (15.4%) |
| 82,003 | 42,792 (35.7%) | 12,651 (10.6%) | 6220 (5.2%) | 822 (0.7%) | 29,366 (24.5%) | 61 (0.1%) | 1643 (1.4%) | 26,310 (21.9%) |
| 82,011 | 694 (47.6%) | 194 (13.3%) | 52 (3.6%) | 2 (0.1%) | 188 (12.9%) | 1 (0.1%) | 27 (1.9%) | 300 (20.6%) |
| 82,012 | 3727 (55%) | 1095 (16.2%) | 366 (5.4%) | 18 (0.3%) | 444 (6.6%) | 0 (0%) | 60 (0.9%) | 1061 (15.7%) |
| 82,013 | 954 (25.2%) | 346 (9.1%) | 269 (7.1%) | 18 (0.5%) | 578 (15.3%) | 2 (0.1%) | 38 (1%) | 1579 (41.7%) |
| 82,020 | 10,670 (2.1%) | 4724 (0.9%) | 58,525 (11.5%) | 2542 (0.5%) | 322,283 (63.3%) | 452 (0.1%) | 12,134 (2.4%) | 98,169 (19.3%) |
| 82,021 | 2892 (1.7%) | 1057 (0.6%) | 39,046 (22.4%) | 656 (0.4%) | 96,433 (55.4%) | 154 (0.1%) | 3059 (1.8%) | 30,818 (17.7%) |
| 82,022 | 1650 (2.1%) | 769 (1%) | 8967 (11.6%) | 374 (0.5%) | 52,284 (67.4%) | 67 (0.1%) | 1747 (2.3%) | 11,713 (15.1%) |
| 82,030 | 231 (4.4%) | 95 (1.8%) | 565 (10.9%) | 21 (0.4%) | 2108 (40.5%) | 5 (0.1%) | 186 (3.6%) | 1988 (38.2%) |
| 82,031 | 81 (1.7%) | 43 (0.9%) | 1164 (24%) | 99 (2%) | 2634 (54.3%) | 9 (0.2%) | 104 (2.1%) | 719 (14.8%) |
| 82,032 | 56 (2%) | 41 (1.5%) | 458 (16.3%) | 18 (0.6%) | 1332 (47.4%) | 10 (0.4%) | 86 (3.1%) | 812 (28.9%) |
| unspecified | 79,621 (37.8%) | 26,885 (12.8%) | 8113 (3.9%) | 683 (0.3%) | 20,301 (9.6%) | 114 (0.1%) | 2654 (1.3%) | 72,088 (34.3%) |
| Associated Diagnosis | |||
|---|---|---|---|
| Acute Posthemorrhagic Anemia | 16.3% | 20.7% | 19.7% |
| Hypertension | 14.9% | 18.2% | 17.5% |
| Heart Disease | 11.3% | 8.2% | 8.9% |
| Diabetes | 8.3% | 8.3% | 8.3% |
| Dementia | 5.7% | 5.8% | 5.8% |
| Respiratory Disease | 7.0% | 2.8% | 3.8% |
| Osteoporosis | 1.1% | 2.3% | 2.1% |
| Parkinson Disease | 2.7% | 1.4% | 1.6% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, U.G.; Viganò, M.; de Girolamo, L.; Banfi, G.; Salvatore, G.; Denaro, V. Epidemiology and Management of Proximal Femoral Fractures in Italy between 2001 and 2016 in Older Adults: Analysis of the National Discharge Registry. Int. J. Environ. Res. Public Health 2022, 19, 16985. https://doi.org/10.3390/ijerph192416985
Longo UG, Viganò M, de Girolamo L, Banfi G, Salvatore G, Denaro V. Epidemiology and Management of Proximal Femoral Fractures in Italy between 2001 and 2016 in Older Adults: Analysis of the National Discharge Registry. International Journal of Environmental Research and Public Health. 2022; 19(24):16985. https://doi.org/10.3390/ijerph192416985
Chicago/Turabian StyleLongo, Umile Giuseppe, Marco Viganò, Laura de Girolamo, Giuseppe Banfi, Giuseppe Salvatore, and Vincenzo Denaro. 2022. "Epidemiology and Management of Proximal Femoral Fractures in Italy between 2001 and 2016 in Older Adults: Analysis of the National Discharge Registry" International Journal of Environmental Research and Public Health 19, no. 24: 16985. https://doi.org/10.3390/ijerph192416985
APA StyleLongo, U. G., Viganò, M., de Girolamo, L., Banfi, G., Salvatore, G., & Denaro, V. (2022). Epidemiology and Management of Proximal Femoral Fractures in Italy between 2001 and 2016 in Older Adults: Analysis of the National Discharge Registry. International Journal of Environmental Research and Public Health, 19(24), 16985. https://doi.org/10.3390/ijerph192416985








