Prognostic Factors of New-Onset Hypertension in New and Traditional Hypertension Definition in a Large Taiwanese Population Follow-up Study
Abstract
1. Introduction
2. Methods
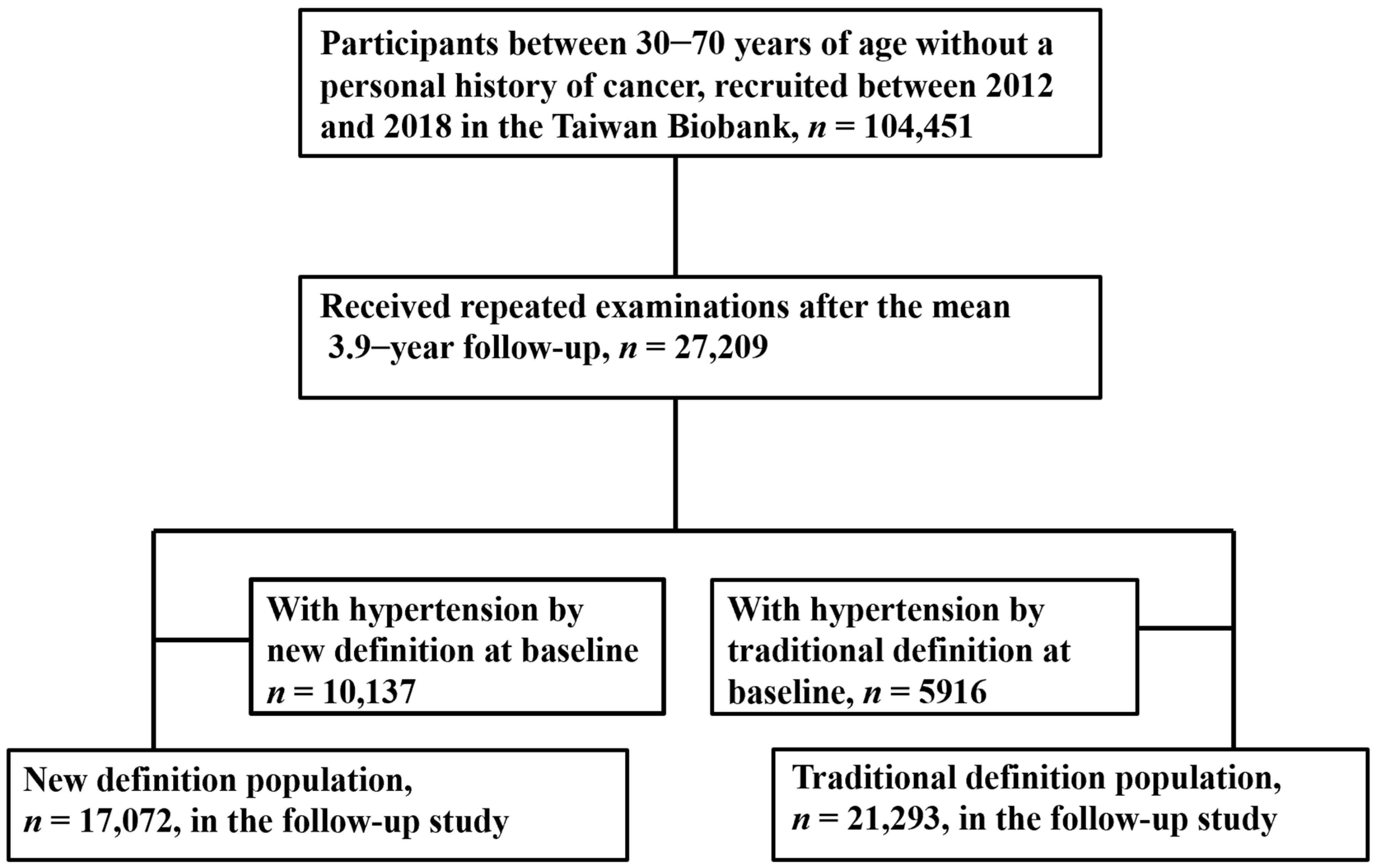
2.1. Study Participants
2.2. Definition of New-Onset Hypertension
2.3. Ethics Statement
2.4. Statistical Analysis
3. Results
3.1. Comparisons of Baseline Characteristics between the with and without New-Onset Hypertension Groups
3.2. Factors Associated with New-Onset Hypertension in the New and Traditional Definition Populations
3.3. Discussion
4. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Basu, S.; Millett, C. Social epidemiology of hypertension in middle-income countries: Determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension 2013, 62, 18–26. [Google Scholar] [CrossRef]
- Colafella, K.M.M.; Denton, K.M. Sex-specific differences in hypertension and associated cardiovascular disease. Nat. Rev. Nephrol. 2018, 14, 185–201. [Google Scholar] [CrossRef] [PubMed]
- Li, A.L.; Zhu, S.; Hu, Z.H.; Peng, Q.; Fang, X.; Zhang, Y.Y. The distribution and epidemic characteristics of cerebrovascular disease in followed-up hypertension patients. Sci. Rep. 2021, 11, 9366. [Google Scholar] [CrossRef] [PubMed]
- Duni, A.; Dounousi, E.; Pavlakou, P.; Eleftheriadis, T.; Liakopoulos, V. Hypertension in Chronic Kidney Disease: Novel Insights. Curr. Hypertens. Rev. 2020, 16, 45–54. [Google Scholar] [CrossRef]
- Zhou, B.; Perel, P.; Mensah, G.A.; Ezzati, M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat. Rev. Cardiol. 2021, 18, 785–802. [Google Scholar] [CrossRef] [PubMed]
- Devi, P.; Rao, M.; Sigamani, A.; Faruqui, A.; Jose, M.; Gupta, R.; Kerkar, P.; Jain, R.K.; Joshi, R.; Chidambaram, N.; et al. Prevalence, risk factors and awareness of hypertension in India: A systematic review. J. Hum. Hypertens. 2013, 27, 281–287. [Google Scholar] [CrossRef]
- The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch. Intern. Med. 1993, 153, 154–183. [CrossRef]
- Lewis, C.E.; Fine, L.J.; Beddhu, S.; Cheung, A.K.; Cushman, W.C.; Cutler, J.A.; Evans, G.W.; Johnson, K.C.; Kitzman, D.W.; Oparil, S.; et al. Final Report of a Trial of Intensive versus Standard Blood-Pressure Control. N. Engl. J. Med. 2021, 384, 1921–1930. [Google Scholar]
- Zhang, W.; Zhang, S.; Deng, Y.; Wu, S.; Ren, J.; Sun, G.; Yang, J.; Jiang, Y.; Xu, X.; Wang, T.D.; et al. Trial of Intensive Blood-Pressure Control in Older Patients with Hypertension. N. Engl. J. Med. 2021, 385, 1268–1279. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar]
- Wang, T.D.; Chiang, C.E.; Chao, T.H.; Cheng, H.M.; Wu, Y.W.; Wu, Y.J.; Lin, Y.H.; Chen, M.Y.; Ueng, K.C.; Chang, W.T.; et al. 2022 Guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the Management of Hypertension. Acta Cardiol. Sin. 2022, 38, 225–325. [Google Scholar] [PubMed]
- Sun, D.; Liu, J.; Xiao, L.; Liu, Y.; Wang, Z.; Li, C.; Jin, Y.; Zhao, Q.; Wen, S. Recent development of risk-prediction models for incident hypertension: An updated systematic review. PLoS ONE 2017, 12, e0187240. [Google Scholar] [CrossRef]
- Lee, B.J.; Kim, J.Y. A comparison of the predictive power of anthropometric indices for hypertension and hypotension risk. PLoS ONE 2014, 9, e84897. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Lim, N.K.; Baek, T.H.; Park, S.H.; Park, H.Y. Anthropometric indices as predictors of hypertension among men and women aged 40–69 years in the Korean population: The Korean Genome and Epidemiology Study. BMC Public Health 2015, 15, 140. [Google Scholar] [CrossRef] [PubMed]
- Chien, K.L.; Hsu, H.C.; Su, T.C.; Chang, W.T.; Sung, F.C.; Chen, M.F.; Lee, Y.T. Prediction models for the risk of new-onset hypertension in ethnic Chinese in Taiwan. J. Hum. Hypertens. 2011, 25, 294–303. [Google Scholar] [CrossRef]
- Chowdhury, M.Z.I.; Naeem, I.; Quan, H.; Leung, A.A.; Sikdar, K.C.; O’Beirne, M.; Turin, T.C. Prediction of hypertension using traditional regression and machine learning models: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0266334. [Google Scholar] [CrossRef]
- Kawasoe, M.; Kawasoe, S.; Kubozono, T.; Ojima, S.; Kawabata, T.; Ikeda, Y.; Oketani, N.; Miyahara, H.; Tokushige, K.; Miyata, M.; et al. Development of a risk prediction score for hypertension incidence using Japanese health checkup data. Hypertens. Res. Off. J. Jpn. Soc. Hypertens. 2022, 45, 730–740. [Google Scholar] [CrossRef]
- Chen, C.H.; Yang, J.H.; Chiang, C.W.K.; Hsiung, C.N.; Wu, P.E.; Chang, L.C.; Chu, H.W.; Chang, J.; Song, I.W.; Yang, S.L.; et al. Population structure of Han Chinese in the modern Taiwanese population based on 10,000 participants in the Taiwan Biobank project. Hum. Mol. Genet. 2016, 25, 5321–5331. [Google Scholar] [CrossRef]
- Fan, C.T.; Hung, T.H.; Yeh, C.K. Taiwan Regulation of Biobanks. J. Law Med. Ethics 2015, 43, 816–826. [Google Scholar] [CrossRef]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef]
- Fryar, C.D.; Ostchega, Y.; Hales, C.M.; Zhang, G.; Kruszon-Moran, D. Hypertension Prevalence and Control Among Adults: United States, 2015–2016. NCHS Data Brief 2017, 289, 1–8. [Google Scholar]
- Skeete, J.; Ramsey, E.; Battle, S.; DiPette, D.J. Sex-based differences in hypertension: Understanding the trends. J. Clin. Hypertens. 2021, 23, 1129–1132. [Google Scholar] [CrossRef]
- Sabbatini, A.R.; Kararigas, G. Estrogen-related mechanisms in sex differences of hypertension and target organ damage. Biol. Sex Differ. 2020, 11, 31. [Google Scholar] [CrossRef]
- He, D.; Fan, F.; Jia, J.; Jiang, Y.; Sun, P.; Wu, Z.; Li, J.; Huo, Y.; Zhang, Y. Lipid profiles and the risk of new-onset hypertension in a Chinese community-based cohort. Nutr. Metab. Cardiovasc. Dis. NMCD 2021, 31, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Borghi, C.; Veronesi, M.; Cosentino, E.; Cicero, A.F.; Kuria, F.; Dormi, A.; Ambrosioni, E. Interaction between serum cholesterol levels and the renin-angiotensin system on the new onset of arterial hypertension in subjects with high-normal blood pressure. J. Hypertens. 2007, 25, 2051–2057. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Deng, Z.; Se, Z.; Bai, Y.; Yan, C.; Zhan, Q.; Zeng, Q.; Ouyang, P.; Dai, M.; Xu, D. Combined impact of risk factors on the subsequent development of hypertension. J. Hypertens. 2019, 37, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Dai, M.; Deng, Z.; Huang, X.; Li, H.; Bai, Y.; Yan, C.; Zhan, Q.; Zeng, Q.; Ouyang, P. Clustering of risk factors and the risk of new-onset hypertension defined by the 2017 ACC/AHA Hypertension Guideline. J. Hum. Hypertens. 2020, 34, 372–377. [Google Scholar] [CrossRef]
- Wang, C.; Yuan, Y.; Zheng, M.; Pan, A.; Wang, M.; Zhao, M.; Li, Y.; Yao, S.; Chen, S.; Wu, S.; et al. Association of Age of Onset of Hypertension With Cardiovascular Diseases and Mortality. J. Am. Coll. Cardiol. 2020, 75, 2921–2930. [Google Scholar] [CrossRef]
- Lin, C.C.; Li, C.I.; Liu, C.S.; Lin, C.H.; Wang, M.C.; Yang, S.Y.; Li, T.C. A risk scoring system to predict the risk of new-onset hypertension among patients with type 2 diabetes. J. Clin. Hypertens. 2021, 23, 1570–1580. [Google Scholar] [CrossRef]
- Franklin, S.S.; Pio, J.R.; Wong, N.D.; Larson, M.G.; Leip, E.P.; Vasan, R.S.; Levy, D. Predictors of new-onset diastolic and systolic hypertension: The Framingham Heart Study. Circulation 2005, 111, 1121–1127. [Google Scholar] [CrossRef]
- Liu, J.; Cheng, N.N.; Zhou, Z.Y.; Zhang, Y.; Yang, J.; Liu, L.S.; Song, Y.; Huang, X.; Tang, G.F.; Wang, B.Y.; et al. Effect of fasting blood glucose on risk of new-onset hypertension in rural Chinese population: A 15-year follow-up cohort. BMC Cardiovasc. Disord. 2021, 21, 531. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Participants with New-Onset Hypertension (n = 3641) | Participants without New-Onset Hypertension (n = 13,431) | p Value | All Participants (n = 17,072) |
|---|---|---|---|---|
| Age (year) | 53 ± 10 | 48 ± 10 | <0.001 | 49 ± 10 |
| Male sex (%) | 39 | 24 | <0.001 | 27 |
| Smoking history (%) | 28 | 20 | <0.001 | 21 |
| Diabetes mellitus (%) | 5.3 | 2.7 | <0.001 | 3.3 |
| Systolic blood pressure (mmHg) | 115 ± 9 | 106 ± 10 | <0.001 | 108 ± 11 |
| Diastolic blood pressure (mmHg) | 71 ± 6 | 66 ± 7 | <0.001 | 67 ± 7 |
| Heart rate (beat/min) | 70 ± 9 | 69 ± 9 | 0.031 | 69 ± 9 |
| Body mass index (kg/m2) | 24.5 ± 3.3 | 22.9 ± 3.2 | <0.001 | 23.3 ± 3.3 |
| Fasting glucose (g/dL) | 97.7 ± 23.7 | 92.4 ± 15.1 | <0.001 | 94 ± 17 |
| Total cholesterol (mg/dL) | 198 ± 35 | 193 ± 35 | <0.001 | 194 ± 35 |
| Triglycerides (mg/dL) | 121 ± 93 | 97 ± 66 | <0.001 | 102 ± 74 |
| eGFR (mL/min/1.73 m2) | 108 ± 26 | 114 ± 25 | <0.001 | 112 ± 25 |
| Characteristics | Participants with New-Onset Hypertension (n = 3002) | Participants without New-Onset Hypertension (n = 18,291) | p Value | All Participants (n = 21,293) |
|---|---|---|---|---|
| Age (year) | 55 ± 9 | 49 ± 10 | <0.001 | 50 ± 10 |
| Male sex (%) | 43 | 30 | <0.001 | 32 |
| Smoking history (%) | 18 | 13 | <0.001 | 14 |
| Diabetes mellitus (%) | 6.6 | 3.0 | <0.001 | 3.5 |
| Systolic blood pressure (mmHg) | 124 ± 10 | 110 ± 12 | <0.001 | 112 ± 13 |
| Diastolic blood pressure (mmHg) | 76 ± 8 | 69 ± 9 | <0.001 | 70 ± 9 |
| Heart rate (beat/min) | 70 ± 9 | 69 ± 9 | 0.001 | 69.± 9 |
| Body mass index (kg/m2) | 24.9 ± 3.4 | 23.4 ± 3.3 | <0.001 | 23.6 ± 3.4 |
| Fasting glucose (g/dL) | 99 ± 25 | 94 ± 17 | <0.001 | 94 ± 19 |
| Total cholesterol (mg/dL) | 200 ± 36 | 194 ± 35 | <0.001 | 195 ± 35 |
| Triglycerides (mg/dL) | 129 ± 98 | 104 ± 76 | <0.001 | 108 ± 80 |
| eGFR (mL/min/1.73 m2) | 105 ± 25 | 112 ± 25 | <0.001 | 111 ± 25 |
| Parameter | Univariable | Multivariable | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age (per 1 year) | 1.051 (1.047–1.055) | <0.001 | 1.035 (1.030–1.039) | <0.001 |
| Male (vs. female) | 2.044 (1.892–2.209) | <0.001 | 1.332 (1.194–1.486) | <0.001 |
| Smoking history | 1.558 (1.432–1.695) | <0.001 | 1.030 (0.920–1.154) | 0.605 |
| Diabetes mellitus | 2.015 (1.686–2.409) | <0.001 | 0.863 (0.686–1.085) | 0.208 |
| Systolic blood pressure (per 1 mmHg) | 1.103 (1.098–1.107) | <0.001 | 1.067 (1.062–1.073) | <0.001 |
| Diastolic blood pressure (per 1 mmHg) | 1.122 (1.115–1.129) | <0.001 | 1.048 (1.040–1.056) | <0.001 |
| Heart rate (per 1 beat/min) | 1.005 (1.000–1.009) | 0.031 | 1.007 (1.002–1.012) | 0.004 |
| Body mass index (per 1 kg/m2) | 1.155 (1.142–1.168) | <0.001 | 1.091 (1.077–1.106) | <0.001 |
| Fasting glucose (per 1 g/dL) | 1.015 (1.013–1.017) | <0.001 | 1.004 (1.001–1.006) | 0.002 |
| Total cholesterol (per 1 mg/dL) | 1.004 (1.003–1.005) | <0.001 | 0.999 (0.998–1.000) | 0.058 |
| Triglyceride (per 1 mg/dL) | 1.004 (1.003–1.005) | <0.001 | 1.001 (1.000–1.001) | 0.004 |
| eGFR (per 1 mL/min/1.73 m2) | 0.990 (0.988–0.991) | <0.001 | 0.998 (0.996–1.000) | 0.051 |
| Parameter | Univariable | Multivariable | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age (per 1 year) | 1.064 (1.060–1.069) | <0.001 | 1.038 (1.032–1.043) | <0.001 |
| Male (vs. female) | 1.750 (1.617–1.894) | <0.001 | 0.948 (0.845–1.064) | 0.364 |
| Smoking history | 1.441 (1.322–1.570) | <0.001 | 1.057 (0.939–1.190) | 0.360 |
| Diabetes mellitus | 2.304 (1.948–2.724) | <0.001 | 1.195 (0.962–1.482) | 0.107 |
| Systolic blood pressure (per 1 mmHg) | 1.109 (1.104–1.113) | <0.001 | 1.078 (1.072–1.084) | <0.001 |
| Diastolic blood pressure (per 1 mmHg) | 1.114 (1.108–1.120) | <0.001 | 1.039 (1.031–1.046) | <0.001 |
| Heart rate (per 1 beat/min) | 1.007 (1.003–1.012) | 0.001 | 1.005 (1.000–1.010) | 0.032 |
| Body mass index (per 1 kg/m2) | 1.139 (1.126–1.151) | <0.001 | 1.072 (1.058–1.087) | <0.001 |
| Fasting glucose (per 1 g/dL) | 1.012 (1.010–1.014) | <0.001 | 1.003 (1.000–1.005) | 0.020 |
| Total cholesterol (per 1 mg/dL) | 1.004 (1.003–1.005) | <0.001 | 0.998 (0.997–0.999) | 0.004 |
| Triglyceride (per 1 mg/dL) | 1.003 (1.003–1.004) | <0.001 | 1.001 (1.000–1.001) | 0.001 |
| eGFR (per 1 mL/min/1.73 m2) | 0.987 (0.985–0.988) | <0.001 | 0.995 (0.993–0.997) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.-H.; Chen, S.-C.; Lee, W.-H.; Chen, Y.-C.; Hsu, P.-C.; Tsai, W.-C.; Lee, C.-S.; Lin, T.-H.; Hung, C.-H.; Kuo, C.-H.; et al. Prognostic Factors of New-Onset Hypertension in New and Traditional Hypertension Definition in a Large Taiwanese Population Follow-up Study. Int. J. Environ. Res. Public Health 2022, 19, 16525. https://doi.org/10.3390/ijerph192416525
Liu Y-H, Chen S-C, Lee W-H, Chen Y-C, Hsu P-C, Tsai W-C, Lee C-S, Lin T-H, Hung C-H, Kuo C-H, et al. Prognostic Factors of New-Onset Hypertension in New and Traditional Hypertension Definition in a Large Taiwanese Population Follow-up Study. International Journal of Environmental Research and Public Health. 2022; 19(24):16525. https://doi.org/10.3390/ijerph192416525
Chicago/Turabian StyleLiu, Yi-Hsueh, Szu-Chia Chen, Wen-Hsien Lee, Ying-Chih Chen, Po-Chao Hsu, Wei-Chung Tsai, Chee-Siong Lee, Tsung-Hsien Lin, Chih-Hsing Hung, Chao-Hung Kuo, and et al. 2022. "Prognostic Factors of New-Onset Hypertension in New and Traditional Hypertension Definition in a Large Taiwanese Population Follow-up Study" International Journal of Environmental Research and Public Health 19, no. 24: 16525. https://doi.org/10.3390/ijerph192416525
APA StyleLiu, Y.-H., Chen, S.-C., Lee, W.-H., Chen, Y.-C., Hsu, P.-C., Tsai, W.-C., Lee, C.-S., Lin, T.-H., Hung, C.-H., Kuo, C.-H., & Su, H.-M. (2022). Prognostic Factors of New-Onset Hypertension in New and Traditional Hypertension Definition in a Large Taiwanese Population Follow-up Study. International Journal of Environmental Research and Public Health, 19(24), 16525. https://doi.org/10.3390/ijerph192416525







