Cognitive Defusion and Psychological Flexibility Predict Negative Body Image in the Chinese College Students: Evidence from Acceptance and Commitment Therapy
Abstract
1. Introduction
2. Method
2.1. Participants and Design
2.2. ACT Procedure
2.3. Measures
2.3.1. Psychological Flexibility
2.3.2. Cognitive Fusion
2.3.3. Negative Body Image
2.3.4. Implicit Association Test (IAT)
2.4. Analysis
3. Results
3.1. Pre-Test
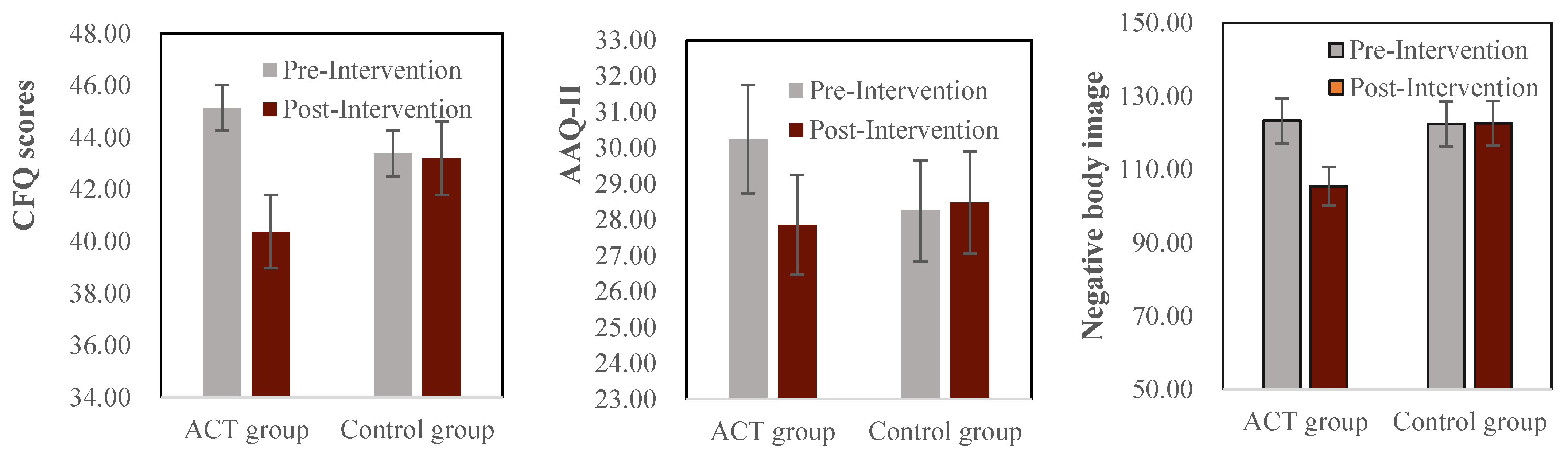
3.2. Post- vs. Pre-Test
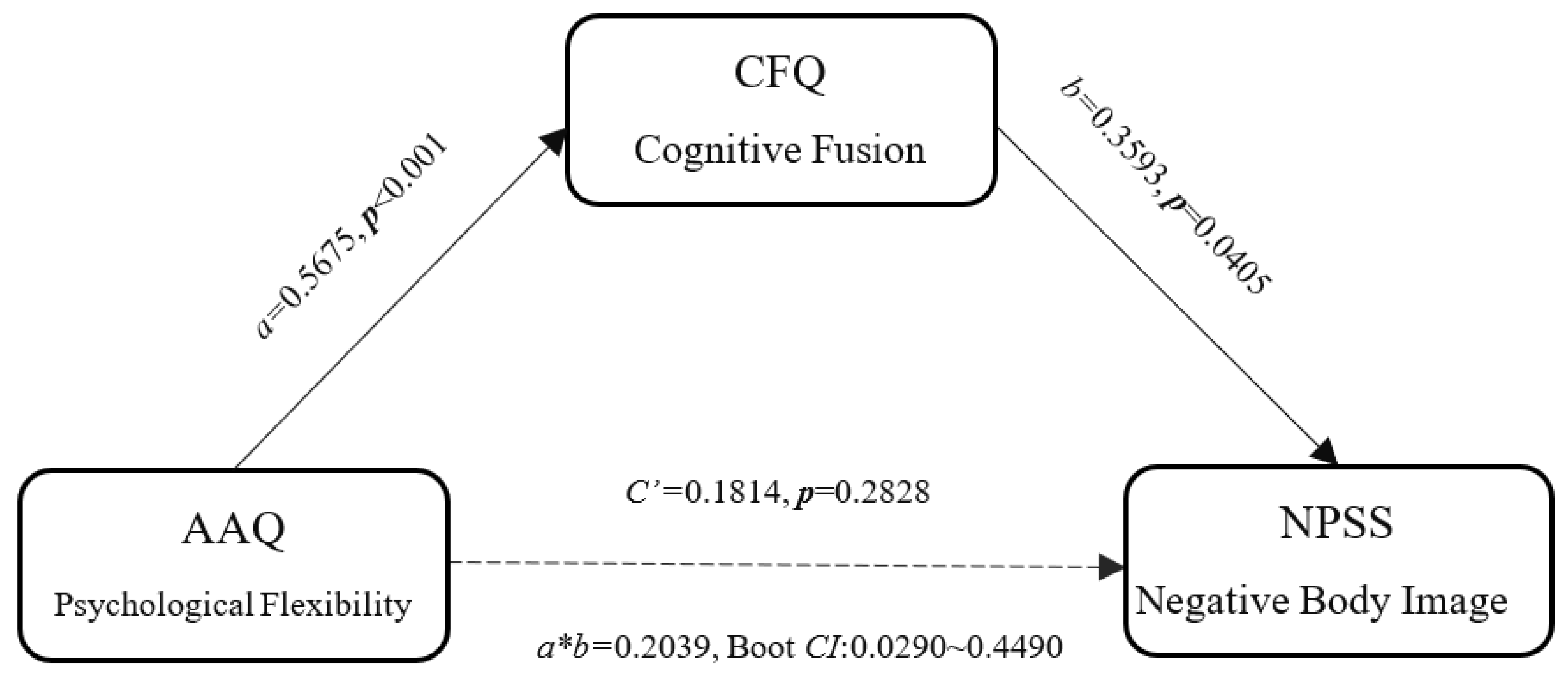
3.3. Post-Test
3.4. Cognitive Defusion during Intervention
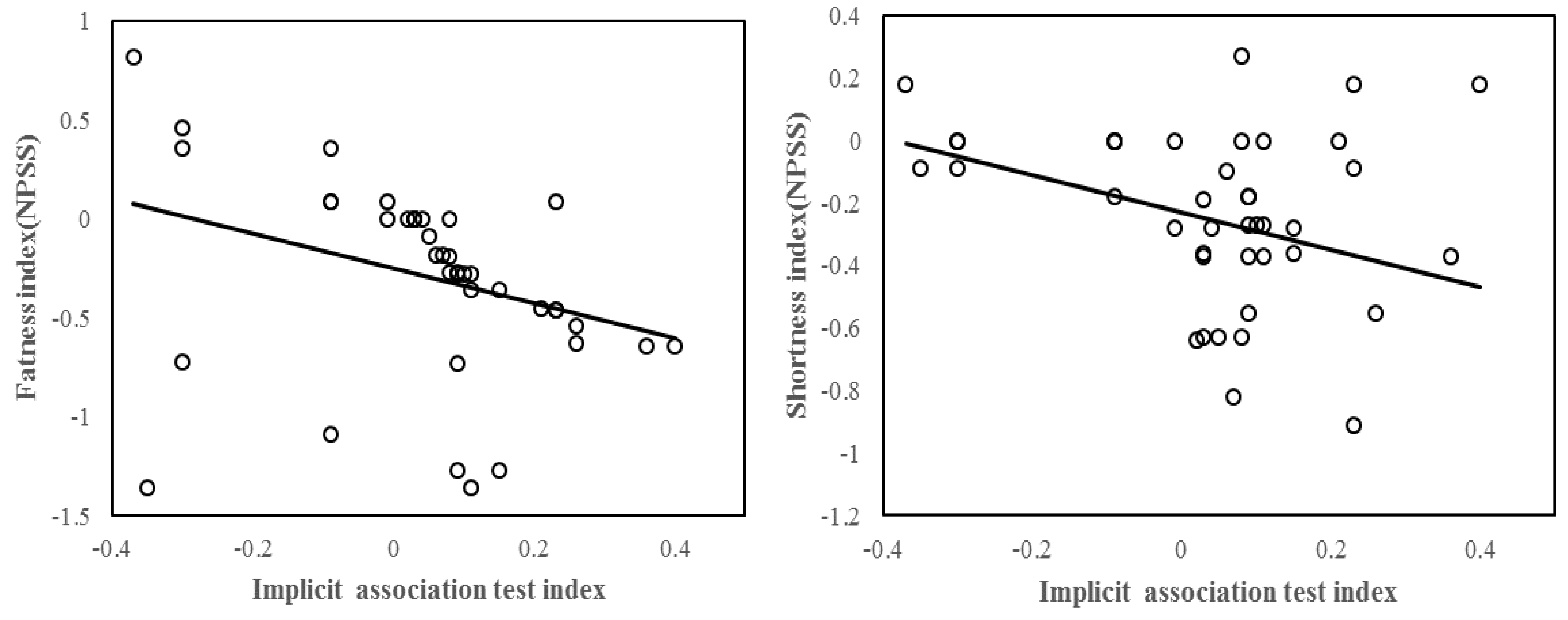
3.5. Individual Differences in Implicit Processing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cash, T.F.; Smolak, L. Body Image: A Handbook of Science, Practice, and Prevention; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Cash, T.F.; Smolak, L. Understanding Body Images: Historical and Contemporary Perspectives; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Grogan, S. Body Image: Understanding Body Dissatisfaction in Men, Women and Children; Routledge: London, UK, 2016. [Google Scholar]
- Stojcic, I.; Dong, X.; Ren, X. Body Image and Sociocultural Predictors of Body Image Dissatisfaction in Croatian and Chinese Women. Front. Psychol. 2020, 11, 731. [Google Scholar] [CrossRef] [PubMed]
- Swami, V.; Tran, U.S.; Stieger, S.; Voracek, M. Associations between women’s body image and happiness: Results of the YouBeauty.com Body Image Survey (YBIS). J. Happiness Stud. 2015, 16, 705–718. [Google Scholar] [CrossRef]
- Tiggemann, M. Body image across the adult life span: Stability and change. Body Image 2004, 1, 29–41. [Google Scholar] [CrossRef] [PubMed]
- Alharballeh, S.; Dodeen, H. Prevalence of body image dissatisfaction among youth in the United Arab Emirates: Gender, age, and body mass index differences. Curr. Psychol. 2021, 1–10. [Google Scholar] [CrossRef]
- Bucchianeri, M.M.; Arikian, A.J.; Hannan, P.J.; Eisenberg, M.E.; Neumark-Sztainer, D. Body dissatisfaction from adolescence to young adulthood: Findings from a 10-year longitudinal study. Body Image 2013, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Paxton, S.J.; Neumark-Sztainer, D.; Hannan, P.J.; Eisenberg, M.E. Body Dissatisfaction Prospectively Predicts Depressive Mood and Low Self-Esteem in Adolescent Girls and Boys. J. Clin. Child Adolesc. Psychol. 2006, 35, 539–549. [Google Scholar] [CrossRef]
- Rodgers, R.F.; DuBois, R.H. Cognitive biases to appearance-related stimuli in body dissatisfaction: A systematic review. Clin. Psychol. Rev. 2016, 46, 1–11. [Google Scholar] [CrossRef]
- Trindade, I.A.; Ferreira, C. The impact of body image-related cognitive fusion on eating psychopathology. Eat. Behav. 2014, 15, 72–75. [Google Scholar] [CrossRef]
- Choi, E.; Choi, I. The associations between body dissatisfaction, body figure, self-esteem, and depressed mood in adolescents in the United States and Korea: A moderated mediation analysis. J. Adolesc. 2016, 53, 249–259. [Google Scholar] [CrossRef]
- Niemeier, B.S.; Duan, Y.P.; Shang, B.; Yang, J. Parental influences on weight-Related health behaviors in western and eastern cultures. Child Care Health Dev. 2017, 43, 259–266. [Google Scholar] [CrossRef]
- Swami, V. Cultural influences on body size ideals. Eur. Psychol. 2015, 20, 44–51. [Google Scholar] [CrossRef]
- Wallner, C.; Kruber, S.; Adebayo, S.O.; Ayandele, O.; Namatame, H.; Olonisakin, T.T.; Olapegba, P.O.; Sawamiya, Y.; Suzuki, T.; Yamamiya, Y.; et al. Interethnic Influencing Factors Regarding Buttocks Body Image in Women from Nigeria, Germany, USA and Japan. Int. J. Environ. Res. Public Health 2022, 19, 13212. [Google Scholar] [CrossRef] [PubMed]
- Klaczynski, P.A.; Goold, K.W.; Mudry, J.J. Culture, obesity stereotypes, self-esteem, and the “thin ideal”: A social identity perspective. J. Youth Adolesc. 2004, 33, 307–317. [Google Scholar] [CrossRef]
- Wang, K.; Liang, R.; Ma, Z.-L.; Chen, J.; Cheung, E.F.C.; Roalf, D.R.; Gur, R.C.; Chan, R.C.K. Body image attitude among Chinese college students. PsyCh J. 2018, 7, 31–40. [Google Scholar] [CrossRef]
- Lee, S.; Lee, A.M. Disordered eating in three communities of China: A comparative study of female high school students in Hong Kong, Shenzhen, and rural Hunan. Int. J. Eat. Disord. 2000, 27, 317–327. [Google Scholar] [CrossRef]
- Cash, T.F.; Pruzinsky, T. Body Image: A Handbook of Theory, Research, and Clinical Practice; Guilford Press: New York, NY, USA, 2004. [Google Scholar]
- Kawamura, K.Y. Asian American body images. In Body Image: A Handbook of Science, Practice, and Presentation; Cash, T.F., Smolak, L., Eds.; Guilford Press: New York, NY, USA, 2011; pp. 229–236. [Google Scholar]
- Luo, Y.; Parish, W.L.; Laumann, E.O. A population-based study of body image concerns among urban Chinese adults. Body Image 2005, 2, 333–345. [Google Scholar] [CrossRef]
- Matsumoto, D.; Juang, L. Culture and Psychology; Nelson Education: Toronto, ON, Canada, 2016. [Google Scholar]
- Soh, N.L.; Touyz, S.W.; Surgenor, L.J. Eating and body image disturbances across cultures: A review. Eur. Eat. Disord. Rev. Prof. J. Eat. Disord. Assoc. 2006, 14, 54–65. [Google Scholar] [CrossRef]
- Spector, R.E. Cultural Diversity in Health and Illness. J. Transcult. Nurs. 2002, 13, 197–199. [Google Scholar] [CrossRef]
- Thompson, J.K.; Heinberg, L.J.; Altabe, M.; Tantleff-Dunn, S. Exacting Beauty: Theory, Assessment, and Treatment of Body Image Disturbance; American Psychological Association: Washington, DC, USA, 1999.
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Fang, S.; Ding, D. A meta-analysis of the efficacy of acceptance and commitment therapy for children. J. Context. Behav. Sci. 2020, 15, 225–234. [Google Scholar] [CrossRef]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and Commitment Therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef]
- Twohig, M.P. Acceptance and commitment therapy: Introduction. Cogn. Behav. Pract. 2012, 19, 499–507. [Google Scholar] [CrossRef]
- Kashdan, T.B.; Rottenberg, J. Psychological flexibility as a fundamental aspect of health. Clin. Psychol. Rev. 2010, 30, 865–878. [Google Scholar] [CrossRef] [PubMed]
- Fogelkvist, M.; Gustafsson, S.A.; Kjellin, L.; Parling, T. Acceptance and commitment therapy to reduce eating disorder symptoms and body image problems in patients with residual eating disorder symptoms: A randomized controlled trial. Body Image 2020, 32, 155–166. [Google Scholar] [CrossRef]
- Griffiths, C.; Williamson, H.; Zucchelli, F.; Paraskeva, N.; Moss, T. A Systematic Review of the Effectiveness of Acceptance and Commitment Therapy (ACT) for Body Image Dissatisfaction and Weight Self-Stigma in Adults. J. Contemp. Psychother. 2018, 48, 189–204. [Google Scholar] [CrossRef] [PubMed]
- Moradi, F.; Ghadiri-Anari, A.; Dehghani, A.; Vaziri, S.R.; Enjezab, B. The effectiveness of counseling based on acceptance and commitment therapy on body image and self-esteem in polycystic ovary syndrome: An RCT. Int. J. Reprod. Biomed. (IJRM) 2020, 18, 243–252. [Google Scholar] [CrossRef] [PubMed]
- Selvi, K.; Parling, T.; Ljótsson, B.; Welch, E.; Ghaderi, A. Two randomized controlled trials of the efficacy of acceptance and commitment therapy-based educational course for body shape dissatisfaction. Scand. J. Psychol. 2021, 62, 249–258. [Google Scholar] [CrossRef]
- Shepherd, L.; Turner, A.; Reynolds, D.P.; Thompson, A.R. Acceptance and commitment therapy for appearance anxiety: Three case studies. Scars Burn. Health 2020, 6, 2059513120967584. [Google Scholar] [CrossRef]
- Bardeen, J.R.; Fergus, T.A. The interactive effect of cognitive fusion and experiential avoidance on anxiety, depression, stress and posttraumatic stress symptoms. J. Context. Behav. Sci. 2016, 5, 1–6. [Google Scholar] [CrossRef]
- Finger, I.D.R.; de Freitas, B.I.; Oliveira, M.D.S. Psychological inflexibility in overweight and obese people from the perspective of acceptance and commitment therapy (ACT). Eat. Weight Disord. Stud. Anorexia Bulim. Obes. 2018, 25, 169–175. [Google Scholar] [CrossRef]
- Hayes, S.C.; Pankey, J. Experiential avoidance, cognitive fusion, and an ACT approach to anorexia nervosa. Cogn. Behav. Pract. 2002, 9, 243–247. [Google Scholar] [CrossRef]
- Zettle, R.D.; Hayes, S.C. Rule-Governed behavior: A potential theoretical framework for cognitive-behavioral therapy. In The Act in Context; Routledge: London, UK, 2015; pp. 33–63. [Google Scholar]
- Hayes, S.K.; Wilson, K. Acceptance and Commitment Therapy: An Experimental Approach to Behavior Change; Guilford Press: New York, NY, USA, 1999. [Google Scholar]
- Zucchelli, F.; White, P.; Williamson, H. Experiential avoidance and cognitive fusion mediate the relationship between body evaluation and unhelpful body image coping strategies in individuals with visible differences. Body Image 2020, 32, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Fang, S. Effects of Internet-Based Acceptance and Commitment Therapy (IACT) on Adolescents: A Systematic Review and Meta-Analysis. Int. J. Ment. Health Promot. 2022, 1–16. [Google Scholar] [CrossRef]
- Arch, J.J.; Wolitzky-Taylor, K.B.; Eifert, G.H.; Craske, M.G. Longitudinal treatment mediation of traditional cognitive behavioral therapy and acceptance and commitment therapy for anxiety disorders. Behav. Res. Ther. 2012, 50, 469–478. [Google Scholar] [CrossRef] [PubMed]
- Luoma; Hayes, S.C. Cognitive defusion. In Cognitive Behavior Therapy: Applying Empirically Supported Techniques in Your Practice; O’Donohue, W.T., Fisher, J.E., Eds.; Wiley: New York, NY, USA, 2003; pp. 71–78. [Google Scholar]
- Barney, J.L.; Barrett, T.S.; Lensegrav-Benson, T.; Quakenbush, B.; Twohig, M.P. Examining a mediation model of body image-related cognitive fusion, intuitive eating, and eating disorder symptom severity in a clinical sample. Eat. Weight Disord. Stud. Anorexia Bulim. Obes. 2022, 27, 2181–2192. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M.; Barker, E.; Chilcot, J. Decentering, rumination, cognitive defusion, and psychological flexibility in people with chronic pain. J. Behav. Med. 2014, 37, 1215–1225. [Google Scholar] [CrossRef] [PubMed]
- McCracken, L.M.; Gutiérrez-Martínez, O.; Smyth, C. “Decentering” reflects psychological flexibility in people with chronic pain and correlates with their quality of functioning. Health Psychol. 2013, 32, 820–823. [Google Scholar] [CrossRef]
- Barrera, T.L.; Szafranski, D.D.; Ratcliff, C.G.; Garnaat, S.L.; Norton, P.J. An Experimental Comparison of Techniques: Cognitive Defusion, Cognitive Restructuring, and in-vivo Exposure for Social Anxiety. Behav. Cogn. Psychother. 2016, 44, 249–254. [Google Scholar] [CrossRef]
- Fang, S.; Ding, D. The efficacy of group-based acceptance and commitment therapy on psychological capital and school engagement: A pilot study among Chinese adolescents. J. Context. Behav. Sci. 2020, 16, 134–143. [Google Scholar] [CrossRef]
- Fang, S.; Ding, D. Which outcome variables are associated with psychological inflexibility/flexibility for chronic pain patients? A three level meta-Analysis. Front. Psychol. 2022, 13, 1069748. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Mandavia, A.; Masuda, A.; Moore, M.; Mendoza, H.; Donati, M.R.; Cohen, L.L. The application of a cognitive defusion technique to negative body image thoughts: A preliminary analogue investigation. J. Context. Behav. Sci. 2015, 4, 86–95. [Google Scholar] [CrossRef]
- Fang, S.; Wang, W. Act in Practice: Case Conceptualization in Acceptance and Commitment Therapy; Chongqing University Press: Chongqing, China, 2011. [Google Scholar]
- Cao, J.; Ji, Y.; Zhu, Z.H. Reliability and validity of the Chinese version of the Acceptance and Action Questionnaire-(AAQ-II) in college students. Chin. Ment. Health J. 2013, 27, 873–877. [Google Scholar] [CrossRef]
- Lee, E.B.; Homan, K.J.; Morrison, K.L.; Ong, C.W.; Levin, M.E.; Twohig, M.P. Acceptance and Commitment Therapy for Trichotillomania: A Randomized Controlled Trial of Adults and Adolescents. Behav. Modif. 2018, 44, 70–91. [Google Scholar] [CrossRef] [PubMed]
- Wei-Chen, Z.; Yang, J.; Li, X.; Hui-Na, G.; Zhuo-Hong, Z. Reliability and validity of the Chinese version of the Cognitive Fusion Questionnaire. Chin. Ment. Health J. 2014, 28, 40–44. [Google Scholar] [CrossRef]
- Chen, H.; Jackson, T.; Huang, X. The Negative Physical Self Scale: Initial development and validation in samples of Chinese adolescents and young adults. Body Image 2006, 3, 401–412. [Google Scholar] [CrossRef]
- Greenwald, A.G.; McGhee, D.E.; Schwartz, J.L.K. Measuring individual differences in implicit cognition: The implicit association test. J. Personal. Soc. Psychol. 1998, 74, 1464. [Google Scholar] [CrossRef]
- Karpinski, A.; Hilton, J.L. Attitudes and the implicit association test. J. Personal. Soc. Psychol. 2001, 81, 774. [Google Scholar] [CrossRef]
- Kou, H.; Su, Y.; Luo, X.; Chen, H. Attentional Bias Toward Face-related Words among Females with Facial Negative Physical Self: Evidence from An Eye-movement Study. Acta Psychol. Sin. 2015, 47, 1213. [Google Scholar] [CrossRef]
- Youyun, X.U.; Qian, Y.; Kan, H.E. Explicit physical self and its correlation with their implicit physical self in college students. Chin. Ment. Health J. 2017, 31, 162–167. [Google Scholar] [CrossRef]
- Cai, H. A review on implicit association test. Adv. Psychol. Sci. 2003, 11, 339–344. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.B. Estimating Effect Sizes From Pretest-Posttest-Control Group Designs. Organ. Res. Methods 2008, 11, 364–386. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The Moderator-Mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium. Commun. Monogr. 2009, 76, 408–420. [Google Scholar] [CrossRef]
- MacKinnon, D.P.; Fairchild, A.J.; Fritz, M.S. Mediation analysis. Annu. Rev. Psychol. 2007, 58, 593–614. [Google Scholar] [CrossRef]
- Hu, K. Neural activity to threat in ventromedial prefrontal cortex correlates with individual differences in anxiety and reward processing. Neuropsychologia 2018, 117, 566–573. [Google Scholar] [CrossRef]
- Hu, K. Investigations into ventral prefrontal cortex using mediation models. J. Neurosci. Res. 2019, 98, 632–642. [Google Scholar] [CrossRef]
- Striegel-Moore, R.H.; Bulik, C.M. Risk factors for eating disorders. Am. Psychol. 2007, 62, 181–198. [Google Scholar] [CrossRef]
- Chen, H.; Jackson, T. Are cognitive biases associated with body image concerns similar between cultures? Body Image 2005, 2, 177–186. [Google Scholar] [CrossRef]
- Hardman, C.A.; Rogers, P.J.; Etchells, K.A.; Houstoun, K.V.E.; Munafò, M. The effects of food-Related attentional bias training on appetite and food intake. Appetite 2013, 71, 295–300. [Google Scholar] [CrossRef]
- Vitousek, K.B.; Hollon, S.D. The investigation of schematic content and processing in eating disorders. Cogn. Ther. Res. 1990, 14, 191–214. [Google Scholar] [CrossRef]
- Williamson, D.A. Body image disturbance in eating disorders: A form of cognitive bias? Eat. Disord. 1996, 4, 47–58. [Google Scholar] [CrossRef]
- Masuda, A.; Hayes, S.C.; Sackett, C.F.; Twohig, M.P. Cognitive defusion and self-relevant negative thoughts: Examining the impact of a ninety year old technique. Behav. Res. Ther. 2004, 42, 477–485. [Google Scholar] [CrossRef]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary Psychometric Properties of the Acceptance and Action Questionnaire–II: A Revised Measure of Psychological Inflexibility and Experiential Avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef] [PubMed]
- Bennett, B.L.; Wagner, A.F.; Latner, J.D. Body Checking and Body Image Avoidance as Partial Mediators of the Relationship between Internalized Weight Bias and Body Dissatisfaction. Int. J. Environ. Res. Public Health 2022, 19, 9785. [Google Scholar] [CrossRef]
- Romano, K.A.; Heron, K.E.; Ebener, D. Associations among weight suppression, self-acceptance, negative body image, and eating disorder behaviors among women with eating disorder symptoms. Women Health 2021, 61, 791–799. [Google Scholar] [CrossRef]
- Gillanders, D.T.; Bolderston, H.; Bond, F.W.; Dempster, M.; Flaxman, P.E.; Campbell, L.; Kerr, S.; Tansey, L.; Noel, P.; Ferenbach, C.; et al. The Development and Initial Validation of the Cognitive Fusion Questionnaire. Behav. Ther. 2014, 45, 83–101. [Google Scholar] [CrossRef]
- Juarascio, A.; Shaw, J.; Forman, E.M.; Timko, A.; Herbert, J.D.; Butryn, M.L.; Lowe, M. Acceptance and Commitment Therapy for eating disorders: Clinical applications of a group treatment. J. Context. Behav. Sci. 2013, 2, 85–94. [Google Scholar] [CrossRef]
- Palmeira, L.; Cunha, M.; Pinto-Gouveia, J. Processes of change in quality of life, weight self-stigma, body mass index and emotional eating after an acceptance-, mindfulness-and compassion-Based group intervention (Kg-Free) for women with overweight and obesity. J. Health Psychol. 2019, 24, 1056–1069. [Google Scholar] [CrossRef]
- Strandskov, S.W.; Ghaderi, A.; Andersson, H.; Parmskog, N.; Hjort, E.; Wärn, A.S.; Jannert, M.; Andersson, G. Effects of Tailored and ACT-Influenced Internet-Based CBT for Eating Disorders and the Relation between Knowledge Acquisition and Outcome: A Randomized Controlled Trial. Behav. Ther. 2017, 48, 624–637. [Google Scholar] [CrossRef]
- Rosen, J.C.; Orosan, P.; Reiter, J. Cognitive behavior therapy for negative body image in obese women. Behav. Ther. 1995, 26, 25–42. [Google Scholar] [CrossRef]
- Rosen, J.C.; Saltzberg, E.; Srebnik, D. Cognitive behavior therapy for negative body image. Behav. Ther. 1989, 20, 393–404. [Google Scholar] [CrossRef]
- Pilecki, B.C.; McKay, D. An Experimental Investigation of Cognitive Defusion. Psychol. Rec. 2012, 62, 19–40. [Google Scholar] [CrossRef]
- Cheng, C.Y.; Bunnin, N. Contemporary Chinese Philosophy; John Wiley & Sons: Hoboken, NJ, USA, 2008. [Google Scholar]
| Baseline Characteristics | All (n = 86) | ACT (n = 42) | Control (n = 44) |
|---|---|---|---|
| Age M (SD) | 19.57 (1.32) | 19.93 (0.92) | 20.04 (1.18) |
| Gender | |||
| male | 40 (46.5%) | 19 (45.2%) | 21 (47.7%) |
| Female | 46 (53.5%) | 23 (54.8%) | 23 (52.3%) |
| College Grade | |||
| Freshmen | 26 (30.2%) | 13 (30.9%) | 13 (29.5%) |
| Sophomores | 21 (24.4%) | 12 (28.6%) | 9 (20.5%) |
| Junior | 20 (23.2%) | 10 (23.8%) | 10 (22.7%) |
| Senior | 19 (22.2%) | 7 (16.7%) | 12 (27.3%) |
| Session | Brief Description |
|---|---|
| 1. First meeting |
|
| |
| |
| 2. Live in the present |
|
| |
| |
| |
| 3. Self-acceptance |
|
| |
| |
| |
| |
| |
| 4. Cognitive defusion |
|
| |
| |
| |
| |
| |
| |
| 5. Self-as-context |
|
| |
| |
| |
| |
| 6. Watch your thoughts |
|
| |
| |
| |
| |
| 7. Values |
|
| |
| |
| |
| |
| |
| 8. Committed action |
|
| |
| |
| |
| |
| |
| |
| 9. Do your best |
|
| |
| |
| |
| 10. Summary |
|
| |
|
| Trial Blocks | Tasks Description | Q Key | P Key |
|---|---|---|---|
| 1 | Attitude discrimination | Positive body image | Negative body image |
| 2 | Concept discrimination | Self | Non-self |
| 3 | Compatible combined task (excise) | Self + Positive body image | Non-self + Negative body image |
| 4 | Compatible combined task (formal) | Self + Positive body image | Non-self + Negative body image |
| 5 | Reversed concept discrimination | Non-self | Self |
| 6 | Reversed combined task (excise) | Non-self + Positive body image | Self + Negative body image |
| 7 | Reversed combined task (formal) | Non-self + Positive body image | Self + Negative body image |
| ACT Group (n = 42) | Control Group (n = 44) | Effect Size | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | F | Cohen’s d | |||||
| M | SD | M | SD | M | SD | M | SD | |||
| AAQ-II | 30.80 | 8.44 | 21.07 | 4.53 | 28.07 | 6.89 | 27.53 | 5.88 | 4.18 * | 0.32 |
| CFQ-F | 45.93 | 14.22 | 33.20 | 8.38 | 42.27 | 10.24 | 43.67 | 9.56 | 7.67 * | 0.43 |
| General Appearance | 3.27 | 0.90 | 2.25 | 0.61 | 2.96 | 0.75 | 2.75 | 0.82 | 38.51 *** | 0.96 |
| Facial Appearance | 2.52 | 0.65 | 1.74 | 0.53 | 2.18 | 0.55 | 2.23 | 0.56 | 34.99 *** | 0.91 |
| Fatness | 2.44 | 1.09 | 1.79 | 0.77 | 2.33 | 0.80 | 2.41 | 0.90 | 18.93 *** | 0.67 |
| Shortness | 2.66 | 0.86 | 1.81 | 0.77 | 2.19 | 0.74 | 2.33 | 0.70 | 16.45 *** | 0.63 |
| Thinness | 1.82 | 0.84 | 1.33 | 0.39 | 2.19 | 0.59 | 2.25 | 0.50 | 20.32 *** | 0.70 |
| Variables | β | T | R2 | ΔR2 |
|---|---|---|---|---|
| Fatness (post-pre) | ||||
| Step1 | 0.01 | |||
| age | 0.09 | 0.54 | ||
| gender | −0.01 | −0.05 | ||
| Step2 | 0.16 * | 0.15 * | ||
| age | 0.12 | 0.78 | ||
| gender | 0.02 | 0.14 | ||
| IAT (post-pre) | −0.39 * | −2.54 | ||
| Shortness (post-pre) | ||||
| Step1 | 0.01 | |||
| age | 0.01 | 0.08 | ||
| gender | 0.01 | 0.06 | ||
| Step2 | 0.13 * | 0.12 * | ||
| age | 0.04 | 0.26 | ||
| gender | 0.04 | 0.23 | ||
| IAT (post-pre) | −0.36 * | −2.30 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fang, S.; Ding, D.; Ji, P.; Huang, M.; Hu, K. Cognitive Defusion and Psychological Flexibility Predict Negative Body Image in the Chinese College Students: Evidence from Acceptance and Commitment Therapy. Int. J. Environ. Res. Public Health 2022, 19, 16519. https://doi.org/10.3390/ijerph192416519
Fang S, Ding D, Ji P, Huang M, Hu K. Cognitive Defusion and Psychological Flexibility Predict Negative Body Image in the Chinese College Students: Evidence from Acceptance and Commitment Therapy. International Journal of Environmental Research and Public Health. 2022; 19(24):16519. https://doi.org/10.3390/ijerph192416519
Chicago/Turabian StyleFang, Shuanghu, Dongyan Ding, Pingping Ji, Mingjie Huang, and Kesong Hu. 2022. "Cognitive Defusion and Psychological Flexibility Predict Negative Body Image in the Chinese College Students: Evidence from Acceptance and Commitment Therapy" International Journal of Environmental Research and Public Health 19, no. 24: 16519. https://doi.org/10.3390/ijerph192416519
APA StyleFang, S., Ding, D., Ji, P., Huang, M., & Hu, K. (2022). Cognitive Defusion and Psychological Flexibility Predict Negative Body Image in the Chinese College Students: Evidence from Acceptance and Commitment Therapy. International Journal of Environmental Research and Public Health, 19(24), 16519. https://doi.org/10.3390/ijerph192416519







