How Do Shifts in Patients with Mental Health Problems’ Formal and Informal Care Utilization Affect Informal Caregivers?: A COVID-19 Case Study
Abstract
1. Introduction
Research Aim and Questions
- How were patients’ formal and informal care utilization and informal caregivers’ subjective burden, happiness, and psychological wellbeing affected by the COVID-19 pandemic?
- To what extent did shifts in patients’ formal and informal care utilization affect informal caregivers’ subjective burden, happiness, and psychological wellbeing?
- To what extent did shifts in patients’ informal care utilization mediate the relationship between shifts in patients’ formal care utilization and informal caregivers’ subjective burden, happiness, and psychological wellbeing?
2. Materials and Methods
2.1. Study Design and Participants
2.2. Ethical Approval
2.3. Measurements
2.3.1. Socio-Demographic Characteristics
2.3.2. Independent Variables
2.3.3. Dependent Variables
2.4. Procedure
2.5. Statistical Analyses
2.5.1. Sub-Question 1: How Did Patients’ Formal and Informal Care Utilization and Informal Caregivers’ Subjective Burden, Happiness, and Psychological Wellbeing Change during the COVID-19 Pandemic?
2.5.2. Sub-Question 2: How Did Shifts in Patients’ Formal and Informal Care Utilization Affect Informal Caregivers’ Subjective Burden, Happiness, and Psychological Wellbeing?
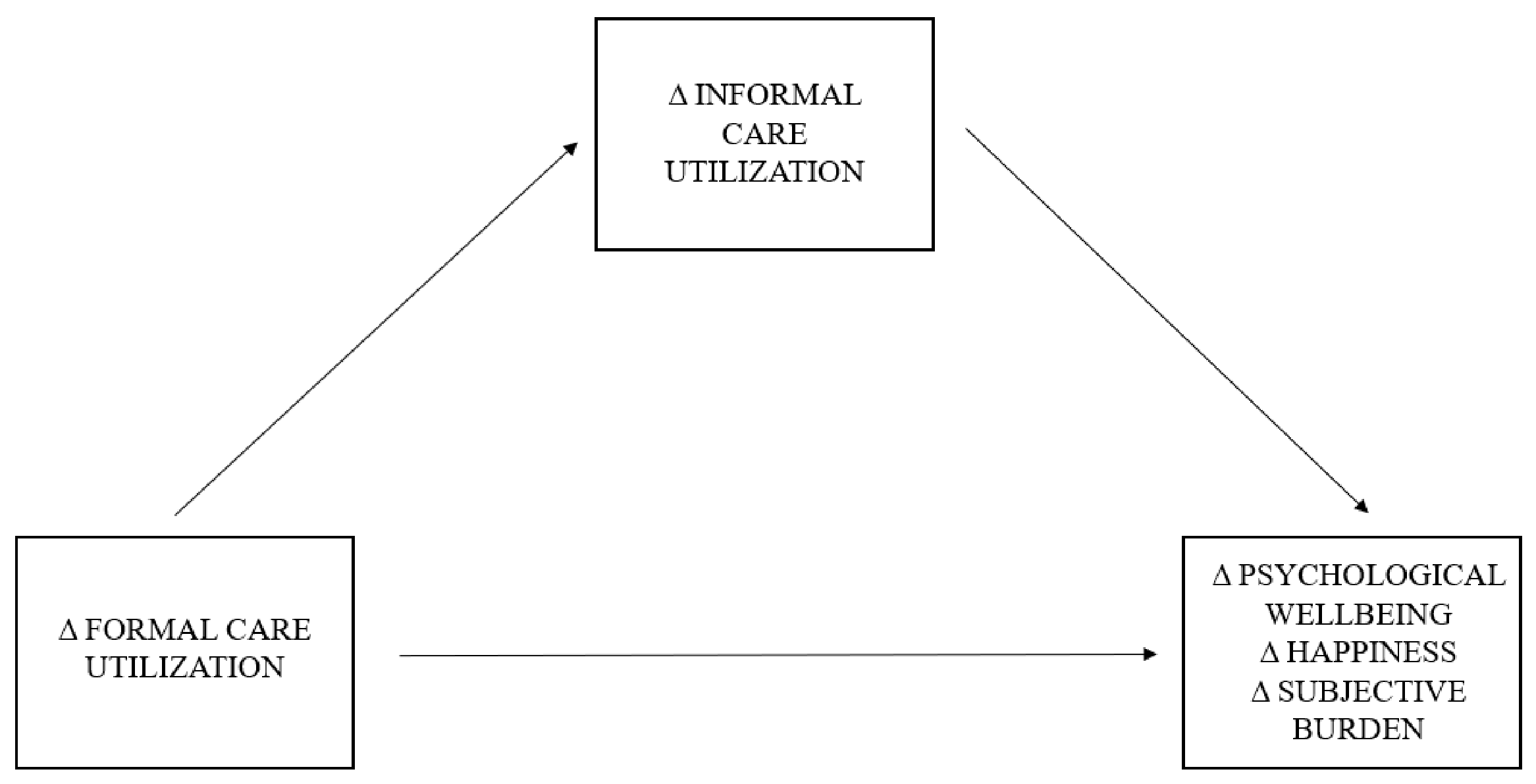
2.5.3. Sub-Question 3: To What Extent Did Shifts in Patients’ Informal Care Utilization Mediate the Relationship between Shifts in Patients’ Formal Care Utilization and Informal Caregivers’ Subjective Burden, Happiness, and Psychological Wellbeing?
3. Results
3.1. Characteristics of Respondents
3.2. Reported Changes during The COVID-19 Pandemic: Patients’ Care Utilization and Informal Caregiver Outcomes (Sub-Question 1)
3.2.1. Patients’ Care Utilization
3.2.2. Informal Caregiver Outcomes
3.3. Differences between Caregiver Groups Reporting Shifts in Their Patients’ Formal and Informal Care Utilization (Sub-Question 2)
3.3.1. Subjective Burden
3.3.2. Happiness
3.3.3. Psychological Wellbeing
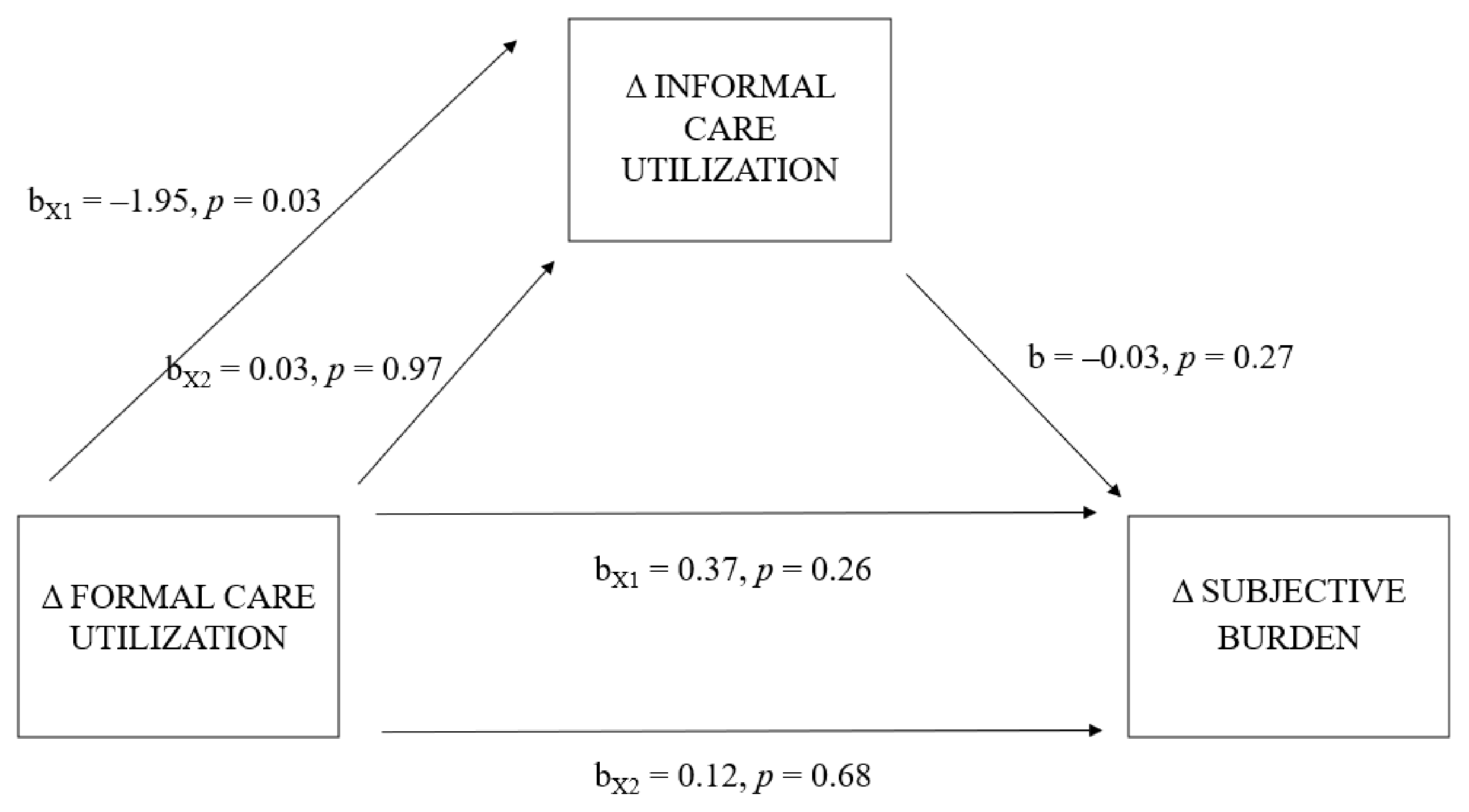
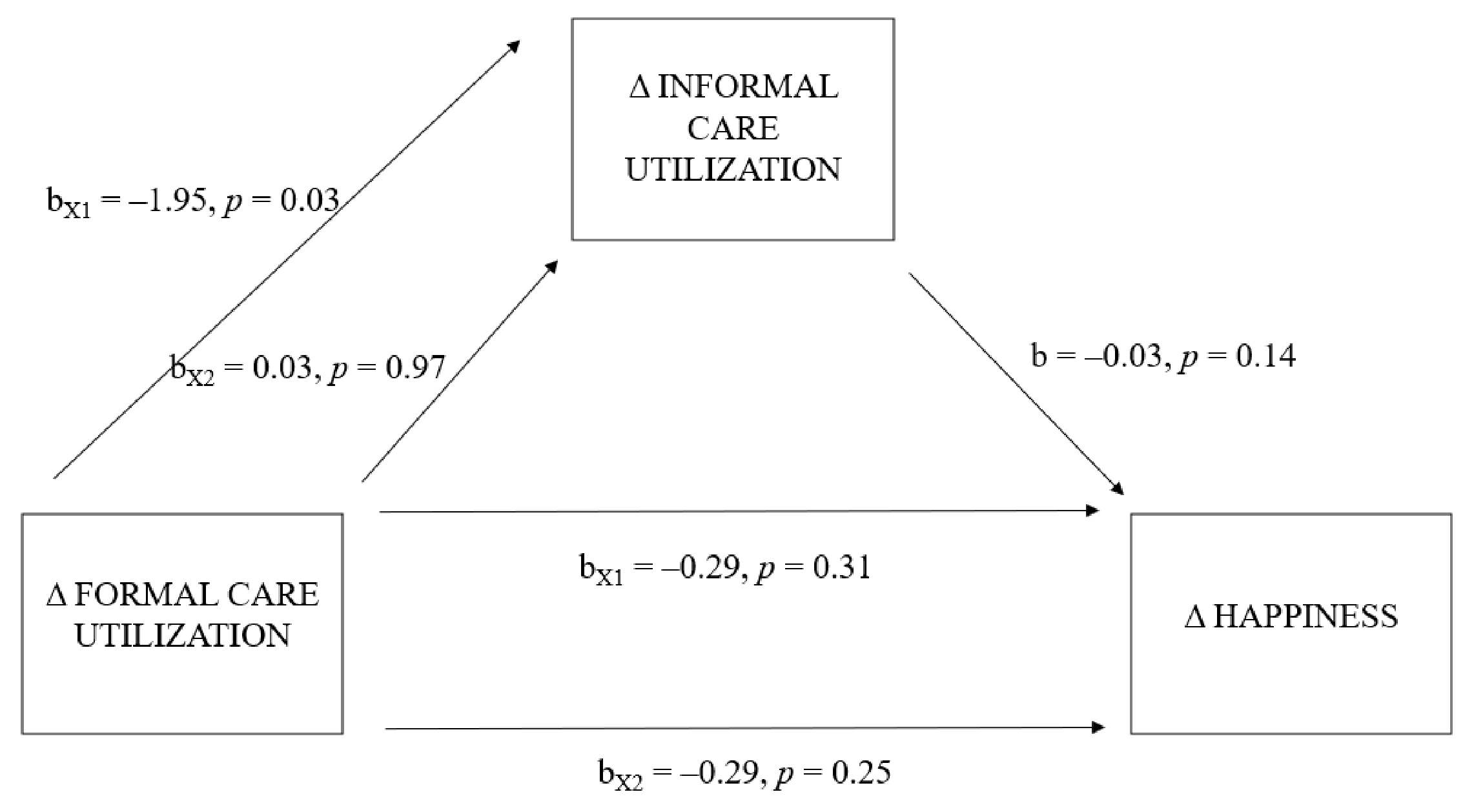
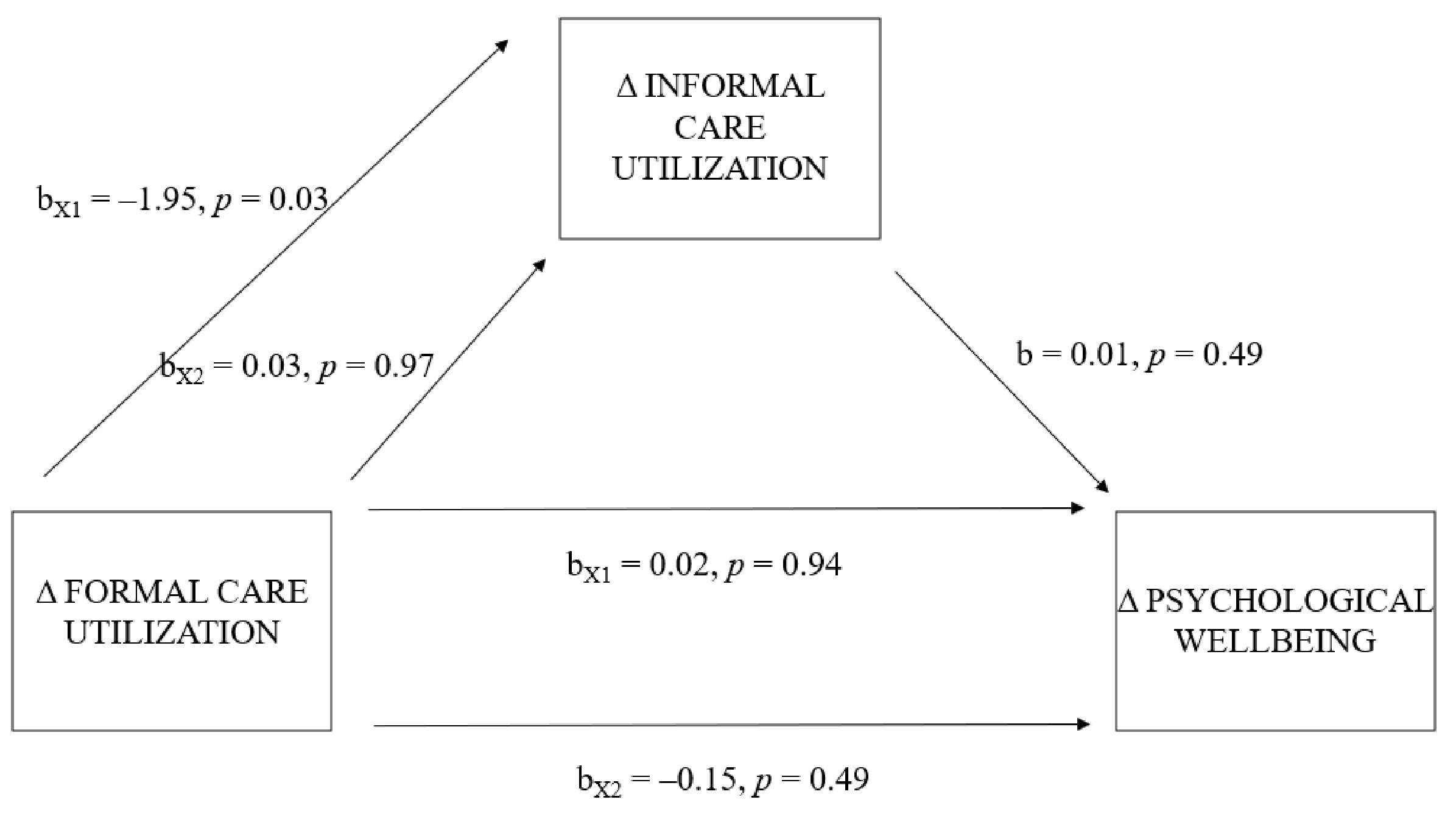
3.4. Effect of Shifts in Patients’ Formal Care Utilization on Informal Caregivers and Mediation by Shifts in Patients’ Informal Care Utilization (Sub-Question 3)
3.4.1. Change in Subjective Burden
3.4.2. Change in Happiness
3.4.3. Change in Psychological Wellbeing
4. Discussion
4.1. Reflection on Main Findings
4.1.1. Minimal Shifts in Patients’ Care Utilization during the COVID-19 Pandemic
4.1.2. No Substitution of Formal Care
4.1.3. COVID-19 Context
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ravelli, D.P. Deinstitutionalisation of mental health care in the Netherlands: Towards an integrative approach. Int. J. Integr. Care 2006, 6, e04. [Google Scholar] [CrossRef] [PubMed]
- Schene, A.H.; Faber, A.M.E. Mental health care reform in the Netherlands. Acta Psychiatr. Scand. 2001, 104, 74–81. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The World Health Report 2001–Mental Health: New Understanding, New Hope; World Health Organization: Geneva, Switzerland, 2001; Available online: https://apps.who.int/iris/handle/10665/42390 (accessed on 11 October 2022).
- Szmukler, G.I.; Wykes, T.; Parkman, S. Care-giving and the impact on carers of a community mental health service: PRiSM Psychosis Study 6. Br. J. Psychiatry 1998, 173, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Hoefman, R.J.; Van Exel, N.J.A.; Brouwer, W.B.F. iVICQ: iMTA Valuation of Informal Care Questionnaire; Erasmus Universiteit Rotterdam: Rotterdam, The Netherlands, 2013; Available online: https://www.imta.nl/questionnaires/ivicq/documents/ (accessed on 11 October 2022).
- Pavolini, E.; Ranci, C. Restructuring the welfare state: Reforms in long-term care in Western European countries. J. Eur. Soc. Policy 2008, 18, 246–259. [Google Scholar] [CrossRef]
- Triantafillou, J.; Naiditch, M.; Repkova, K.; Stiehr, K.; Carretero, S.; Emilsson, T.; Vlantoni, D. Informal Care in the Long-Term Care System European Overview Paper; European Centre for Social Welfare Policy and Research: Vienna, Austria, 2010; Available online: https://www.euro.centre.org/downloads/detail/768 (accessed on 11 October 2022).
- World Health Organization. World Mental Health Report: Transforming Mental Health for All; WHO Press: Geneva, Switzerland, 2022; Available online: https://www.who.int/publications/i/item/9789240049338 (accessed on 11 October 2022).
- Scheffler, R.M.; Arnold, D.R. Projecting shortages and surpluses of doctors and nurses in the OECD: What looms ahead. Health Econ. Policy Law 2019, 14, 274–290. [Google Scholar] [CrossRef]
- Barbieri, D.; Ghibelli, P. Formal vs. Informal Long-Term Care: Economic Social Impacts; SPRINT Working Paper; SPRINT: Brussels, Belgium, 2018; Volume 4, Available online: http://sprint-project.eu/wp-content/uploads/2018/09/SPRINT_D4.4_Formal_vs_Informal-LTC_Econocmic_Social_Impacts.pdf (accessed on 11 October 2022).
- Verbakel, E. Informal caregiving and well-being in Europe: What can ease the negative consequences for caregivers? J. Eur. Soc. Policy 2014, 24, 424–441. [Google Scholar] [CrossRef]
- Hastrup, L.H.; van den Berg, B.; Gyrd-Hansen, D. Do informal caregivers in mental illness feel more burdened? A comparative study of mental versus somatic illnesses. Scand. J. Public Health 2011, 39, 598–607. [Google Scholar] [CrossRef]
- De Boer, A.; Plaisier, I.; de Klerk, M. Mantelzorgers in Het Vizier: Beleidssignalement Mantelzorg [Informal Caregivers in the Crosshairs: Policy Statement Informal Care]; Sociaal en Cultureel Planbureau: Den Haag, The Netherlands, 2019; Available online: https://www.scp.nl/publicaties/publicaties/2019/11/08/mantelzorgers-in-het-vizier (accessed on 11 October 2022).
- Plaisier, I.; Schyns, P. Hulp Delen [Sharing Help]. In Informele Hulp: Wie Doet Er Wat? Omvang, Aard En Kenmerken Van Mantelzorg En Vrijwilligerswerk in De Zorg En Ondersteuning in 2014 [Informal Care: Who Does What? Scope, Nature and Characteristics of Informal Care and Volunteer Work in Healthcare and Support in 2014]; de Klerk, M., de Boer, A., Plaisier, I., Schyns, P., Kooiker, S., Eds.; Sociaal en Cultureel Planbureau: Den Haag, The Netherlands, 2014; pp. 110–128. Available online: https://www.scp.nl/publicaties/publicaties/2015/12/15/informele-hulp-wie-doet-er-wat (accessed on 11 October 2022).
- Fekete, C.; Tough, H.; Siegrist, J.; Brinkhof, M.W. Health impact of objective burden, subjective burden and positive aspects of caregiving: An observational study among caregivers in Switzerland. BMJ Open 2017, 7, e017369. [Google Scholar] [CrossRef]
- Kuzuya, M.; Enoki, H.; Hasegawa, J.; Izawa, S.; Hirakawa, Y.; Shimokata, H.; Akihisa, I. Impact of caregiver burden on adverse health outcomes in community-dwelling dependent older care recipients. Am. J. Geriatr. Psychiatry 2011, 19, 382–391. [Google Scholar] [CrossRef]
- Hughes, S.L.; Giobbie-Hurder, A.; Weaver, F.M.; Kubal, J.D.; Henderson, W. Relationship between caregiver burden and health-related quality of life. Gerontologist 1999, 39, 534–545. [Google Scholar] [CrossRef]
- Kate, N.; Grover, S.; Kulhara, P.; Nehra, R. Relationship of caregiver burden with coping strategies, social support, psychological morbidity, and quality of life in the caregivers of schizophrenia. Asian J. Psychiatr 2013, 6, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Pickett-Schenk, S.A.; Cook, J.A.; Steigman, P.; Lippincott, R.; Bennett, C.; Grey, D.D. Psychological well-being and relationship outcomes in a randomized study of family-led education. Arch. Gen. Psychiatry 2006, 63, 1043–1050. [Google Scholar] [CrossRef] [PubMed]
- Suro, G.; Weisman de Mamani, A.G. Burden, interdependence, ethnicity, and mental health in caregivers of patients with schizophrenia. Fam. Process 2013, 52, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Van Campen, C.; de Boer, A.H.; Iedema, J. Are informal caregivers less happy than noncaregivers? Happiness and the intensity of caregiving in combination with paid and voluntary work. Scand. J. Caring. Sci. 2013, 27, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Broese van Groenou, M.I.; De Boer, A. Providing informal care in a changing society. Eur. J. Ageing 2016, 13, 271–279. [Google Scholar] [CrossRef]
- Litwak, E. Helping the Elderly: The Complementary Roles of Informal Networks and Formal Systems; The Guilford Press: New York, NY, USA, 1985. [Google Scholar]
- Hatfield, A.B.; Lefley, H.P. Families of the Mentally Ill: Coping and Adaption; The Guilford Press: New York, NY, USA, 1987. [Google Scholar]
- Greene, V.L. Substitution between formally and informally provided care for the impaired elderly in the community. Med. Care 1983, 21, 609–619. [Google Scholar] [CrossRef]
- Clark, R.E.; Xie, H.; Adachi-Meija, A.M.; Sengupta, A. Substitution between Formal and Informal Care for Persons with Severe Mental Illness and Substance Use Disorders. J. Mental. Health Policy Econ. 2001, 4, 123–132. [Google Scholar]
- Perdrix, E.; Roquebert, Q. Does the amount of formal care affect informal care? Evidence among over-60s in France. Eur. J. Health Econ. 2022, 23, 453–465. [Google Scholar] [CrossRef]
- Lindt, N.; van Berkel, J.; Mulder, B.C. Determinants of overburdening among informal carers: A systematic review. BMC Geriatr. 2020, 20, 304. [Google Scholar] [CrossRef]
- Verbakel, E.; Tamlagsrønning, S.; Winstone, L.; Fjær, E.L.; Eikemo, T.A. Informal care in Europe: Findings from the European Social Survey (2014) special module on the social determinants of health. Eur. J. Public Health 2017, 27 (Suppl. 1), 90–95. [Google Scholar] [CrossRef]
- Lauber, C.; Eichenberger, A.; Luginbühl, P.; Keller, C.; Rössler, W. Determinants of burden in caregivers of patients with exacerbating schizophrenia. Eur. Psychiatry 2003, 18, 285–289. [Google Scholar] [CrossRef]
- Rodríguez-González, A.M.; Rodríguez-Míguez, E.; Claveria, A. Determinants of caregiving burden among informal caregivers of adult care recipients with chronic illness. J. Clin. Nurs. 2021, 30, 1335–1346. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 Significantly Impacts Health Services for Noncommunicable Diseases. Available online: https://www.who.int/news/item/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases (accessed on 4 December 2022).
- Chan, E.Y.Y.; Gobat, N.; Kim, J.H.; Newnham, A.E.; Huang, Z.; Hung, H.; Dubois, C.; Hung, K.K.C.; Wong, E.L.Y.; Wong, S.Y.S. Informal home care providers: The forgotten health-care workers during the COVID-19 pandemic. Lancet 2020, 395, 1957–1959. [Google Scholar] [CrossRef]
- De Boer, A.; Hoefman, R.; de Klerk, M.; Plaisier, I.; de Roos, S. Beleidssignalement Maatschappelijk Gevolgen Coronamaatregelen: Mantelzorgers [Policy Statement Societal Consequences of Corona Measures]; Sociaal en Cultureel Planbureau: Den Haag, The Netherlands, 2020; Available online: https://www.scp.nl/publicaties/publicaties/2020/07/14/beleidssignalement-maatschappelijke-gevolgen-coronamaatregelen-mantelzorgers (accessed on 11 October 2022).
- Park, S.S. Caregivers’ mental health and somatic symptoms during COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 76, e235–e240. [Google Scholar] [CrossRef]
- Veer, I.; Riepenhausen, A.; Zerban, M.; Wackerhagen, C.; Engen, H.; Puhlmann, L.; Kalisch, R. Mental Resilience in the Corona Lockdown: First Empirical Insights from Europe; ORBi: Liege, Belgium, 2020; Available online: https://orbi.uliege.be/2268/247055 (accessed on 11 October 2022).
- Central Government of the Netherlands. Maart 2020: Maatregelen Tegen Verspreiding Coronavirus, Intelligente Lockdown [March 2020: Measures against the Spread of the Coronavirus, Intelligent Lockdown]. Available online: https://www.rijksoverheid.nl/onderwerpen/coronavirus-tijdlijn/maart-2020-maatregelen-tegen-verspreiding-coronavirus (accessed on 22 August 2022).
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- iMTA Productivity and Health Research Group. Manual iMTA Medical Cost Questionnaire (iMCQ); Erasmus University Rotterdam: Rotterdam, The Netherlands, 2018; Available online: https://www.imta.nl/questionnaires/imcq/ (accessed on 11 October 2022).
- Van Exel, N.J.A.; op Reimer, W.J.S.; Brouwer, W.B.F.; van den Berg, B.; Koopmanschap, M.A.; van den Bos, G.A. Instruments for assessing the burden of informal caregiving for stroke patients in clinical practice: A comparison of CSI, CRA, SCQ and self-rated burden. Clin. Rehabil. 2004, 18, 203–214. [Google Scholar] [CrossRef]
- Van Exel, N.J.A.; Bobinac, A.; Koopmanschap, M.; Brouwer, W.B.F. The invisible hands made visible: Recognizing the value of informal care in healthcare decision-making. Expert Rev. Pharmacoecon Outcomes Res. 2008, 8, 557–561. [Google Scholar] [CrossRef]
- Brouwer, W.B.F.; Van Exel, N.J.A.; Van Gorp, B.; Redekop, W.K. The CarerQol instrument: A new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual. Life Res. 2006, 15, 1005–1021. [Google Scholar] [CrossRef]
- Hoefman, R.J.; Van Exel, N.J.A.; Foets, M.; Brouwer, W.B.F. Sustained informal care: The feasibility, construct validity and test–retest reliability of the CarerQol-instrument to measure the impact of informal care in long-term care. Aging Ment. Health 2011, 15, 1018–1027. [Google Scholar] [CrossRef]
- van Krugten, F.C.W.; Busschbach, J.J.V.; Versteegh, M.M.; Hakkaart-van Roijen, L.; Brouwer, W.B.F. The Mental Health Quality of Life Questionnaire (MHQoL): Development and first psychometric evaluation of a new measure to assess quality of life in people with mental health problems. Qual. Life Res. 2022, 31, 633–643. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; The Guilford Press: New York, NY, USA, 2017. [Google Scholar]
- Bass, D.M.; Noelker, L.S.; Rechlin, L.R. The moderating influence of service use on negative caregiving consequences. J. Gerontol. B Psychol. Sci. Soc. Sci. 1996, 51, S121–S131. [Google Scholar] [CrossRef] [PubMed]
- Hirst, M. Carer distress: A prospective, population-based study. Soc. Sci. Med. 2005, 61, 697–708. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, N. Distinct impacts of high intensity caregiving on caregivers’ mental health and continuation of caregiving. Health Econ. Rev. 2017, 7, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lerner, D.; Chang, H.; Rogers, W.H.; Benson, C.; Lyson, M.C.; Dixon, L.B. Psychological distress among caregivers of individuals with a diagnosis of schizophrenia or schizoaffective disorder. Psychiatr. Serv. 2018, 69, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Pompili, M.; Harnic, D.; Gonda, X.; Forte, A.; Dominici, G.; Innamorati, M.; Fountoulakis, K.N.; Serafini, G.; Sher, L.; Janiri, L.; et al. Impact of living with bipolar patients: Making sense of caregivers’ burden. World J. Psychiatry 2014, 4, 1–12. [Google Scholar] [CrossRef]
- Biddle, B.J. Recent development in role theory. Annu. Rev. Sociol. 1986, 12, 67–92. [Google Scholar] [CrossRef]
- Goode, W.J. A theory of role strain. Am. Sociol. Rev. 1960, 25, 483–496. [Google Scholar] [CrossRef]
- Chow, M.W.; Noorthoorn, E.O.; Wierdsma, A.I.; Van Der Horst, M.; De Boer, N.; Guloksuz, S.; Luykx, J.J. Impact of the first COVID-19 outbreak on mental health service utilisation at a Dutch mental health centre: Retrospective observational study. Br. J. Psychiatry Open 2021, 7, E213. [Google Scholar] [CrossRef]
- Raiber, K.; Verbakel, E. Are the gender gaps in informal caregiving intensity and burden closing due to the COVID-19 pandemic? Evidence from the Netherlands. Gend. Work. Organ. 2021, 28, 1926–1936. [Google Scholar] [CrossRef]
- Tur-Sinai, A.; Bentur, N.; Fabbietti, P.; Lamura, G. Impact of the outbreak of the COVID-19 pandemic on formal and informal care of community-dwelling older adults: Cross-national clustering of empirical evidence from 23 countries. Sustainability 2021, 13, 7277. [Google Scholar] [CrossRef]
- Verbakel, E.; Raiber, K.; de Boer, A. Verandering in de intensiteit van mantelzorg tijdens de eerste COVID-19 lockdown in 2020 in Nederland [Change in the intensity of informal care during the first COVID-19 lockdown in 2020 in the Netherlands]. Mens Maatsch. 2021, 96, 411–439. [Google Scholar] [CrossRef]
- Sugiura, K.; Pertega, E.; Holmberg, C. Experiences of involuntary psychiatric admission decision-making: A systematic review and meta-synthesis of the perspectives of service users, informal carers, and professionals. Int. J. Law Psychiatry 2020, 73, 101645. [Google Scholar] [CrossRef]
- Keuper, J.; Batenburg, R.; Verheij, R.; Van Tuyl, L. Use of E-health in Dutch general practice during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 12479. [Google Scholar] [CrossRef]
- Feijt, M.; De Kort, Y.; Bongers, I.; Bierbooms, J.; Westerink, J.; IJsselsteijn, W. Mental health care goes online: Practitioners’ experiences of providing mental health care during the COVID-19 pandemic. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 860–864. [Google Scholar] [CrossRef]
- Bolin, K.; Lindgren, B.; Lundborg, P. Informal and formal care among single-living elderly in Europe. Health Econ. 2008, 17, 393–409. [Google Scholar] [CrossRef]
- Bremer, P.; Challis, D.; Hallberg, I.R.; Leino-Kilpi, H.; Saks, K.; Vellas, B.; Zwakhalen, S.M.; Sauerland, D.; RightTimePlaceCare Consortium. Informal and formal care: Substitutes or complements in care for people with dementia? Empirical evidence for 8 European countries. Health Policy 2017, 121, 613–622. [Google Scholar] [CrossRef]
- Zhang, W.; Sun, H.; L’Heureux, J. Substitutes or complements between informal and formal home care in the Canadian longitudinal study on aging: Functional impairment as an effect modifier. Health Policy 2021, 125, 1267–1275. [Google Scholar] [CrossRef]
- Diminic, S.; Lee, Y.Y.; Hielscher, E.; Harris, M.G.; Kealton, J.; Whiteford, H.A. Quantifying the size of the informal care sector for Australian adults with mental illness: Caring hours and replacement cost. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 387–400. [Google Scholar] [CrossRef]
- Hielscher, E.; Diminic, S.; Kealton, J.; Harris, M.; Lee, Y.Y.; Whiteford, H. Hours of care and caring tasks performed by Australian carers of adults with mental illness: Results from an online survey. Community Ment. Health J. 2019, 55, 279–295. [Google Scholar] [CrossRef]
- Lyons, K.S.; Zarit, S.H. Formal and informal support: The great divide. Int. J. Geriatr. Psychiatry 1999, 14, 183–192. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Netherlands Statistics. Coronavirus Crisis FAQs. Available online: https://www.cbs.nl/en-gb/dossier/coronavirus-crisis-cbs-figures (accessed on 7 September 2022).
- Pan, K.-Y.; Kok, A.A.L.; Eikelenboom, M.; Horsfall, M.; Jörg, F.; Luteijn, R.A.; Rhebergen, D.; van Oppen, P.; Giltay, E.J.; Penninx, B.W.J.H. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry 2021, 8, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Douglas, M.; Katikireddi, S.V.; Taulbut, M.; McKee, M.; McCartney, G. Mitigating the wider health effects of covid-19 pandemic response. BMJ 2020, 369, m1557. [Google Scholar] [CrossRef] [PubMed]
- Gräler, L.; Bremmers, L.; Bakx, P.; van Exel, J.; van Bochove, M. Informal care in times of a public health crisis: Objective burden, subjective burden and quality of life of caregivers in the Netherlands during the COVID-19 pandemic. Health Soc. Care Community 2022, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Chadha, J.; Khullar, L.; Mittal, N. Facing the wrath of enigmatic mutations: A review on the emergence of severe acute respiratory syndrome coronavirus 2 variants amid coronavirus disease-19 pandemic. Environ. Microbiol. 2021, 24, 2615–2629. [Google Scholar] [CrossRef]
- Van den Berg, B.; Spauwen, P. Measurement of informal care: An empirical study into the valid measurement of time spent on informal caregiving. Health Econ. 2006, 15, 447–460. [Google Scholar] [CrossRef]
- Chen, C.Y.; Liu, C.Y.; Liang, H.Y. Comparison of patient and caregiver assessments of depressive symptoms in elderly patients with depression. Psychiatry Res. 2009, 166, 69–75. [Google Scholar] [CrossRef]
| Informal Caregivers | |
|---|---|
| Gender | |
| Male n (%) | 88 (40.2) |
| Age mean years (min.-max.; SD) | 47.4 (18–84; 16.1) |
| Employment status | |
| Full- or part-time employment n (%) | 133 (60.7) |
| Overall COVID-19-related concerns | |
| No concerns n (%) | 19 (8.9) |
| Some concerns n (%) | 77 (36.0) |
| Very concerned n (%) | 118 (55.1) |
| Child caregiving responsibility | |
| Not caring for a child under the age of 18 n (%) | 154 (70.3) |
| Care Recipients | |
| Comorbidity status | |
| Yes, has at least one comorbidity n (%) | 147 (67.1) |
| Living situation | |
| Lives with caregiver n (%) | 60 (27.4) |
| Patients’ Weekly Utilization Hours | |||||||
|---|---|---|---|---|---|---|---|
| T0 (SD) | T1 (SD) | Δ (SD) | Wilcoxon Signed-Rank Test z Score | n Care Recipients (%) | |||
| Total informal care | 41.9 (76.8) | 41.3 (77.0) | −0.6 (4.7) | −1.8 | Less care | 23 (10.5) | |
| No change | 138 (63.0) | ||||||
| More care | 58 (26.5) | ||||||
| Support with household tasks | 10.7 (22.1) | 10.5 (22.0) | −0.2 (1.6) | −1.2 | Less care | 16 (7.3) | |
| No change | 193 (88.1) | ||||||
| More care | 10 (4.6) | ||||||
| Support with self-care tasks | 11.0 (24.1) | 11.0 (24.1) | 0.1 (1.4) | 0.0 | Less care | 9 (4.1) | |
| No change | 201 (91.8) | ||||||
| More care | 9 (4.1) | ||||||
| Practical support | 8.8 (16.1) | 8.5 (16.0) | −0.2 (1.7) | −1.9 * | Less care | 19 (8.7) | |
| No change | 191 (87.2) | ||||||
| More care | 9 (4.1) | ||||||
| Emotional support | 11.5 (25.2) | 11.2 (25.4) | −0.2 (3.0) | −2.0 * | Less care | 22 (10.1) | |
| No change | 186 (84.9) | ||||||
| More care | 11 (5.0) | ||||||
| Total formal care | n.a. | n.a. | n.a. | n.a. | Less care | 49 (22.4) | |
| No change | 135 (61.6) | ||||||
| More care | 35 (16.0) | ||||||
| Informal Caregiver Outcomes Mean (SD) | Paired t-Test t | |||
|---|---|---|---|---|
| T0 | T1 | Δ | ||
| Subjective burden a | 5.1 (2.4) | 5.5 (2.4) | 0.4 (1.7) | 3.2 ** |
| Happiness b | 7.0 (1.9) | 6.4 (1.9) | −0.6 (1.5) | −6.2 *** |
| Psychological wellbeing c | 7.3 (1.8) | 7.2 (1.8) | −0.1 (1.3) | −1.6 |
| Subjective Burden a | Happiness b | Psychological Wellbeing c | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 (SD) | T1 (SD) | Δ (SD) | Paired t-Test t | T0 (SD) | T1 (SD) | Δ (SD) | Paired t-Test t | T0 (SD) | T1 (SD) | Δ (SD) | Paired t-Test t | |
| No change in formal care hours, Decrease in informal care hours (n = 11) | 4.9 (2.2) | 5.8 (3.0) | 0.9 (1.8) | 1.7 | 6.0 (2.9) | 5.2 (1.9) | −0.8 (2.4) | −1.1 | 6.5 (2.3) | 6.2 (2.5) | −0.4 (0.9) | −1.3 |
| Increase in formal care hours, Decrease in informal care hours (n = 4) | 3.5 (3.7) | 4.5 (3.0) | 1.0 (1.8) | 1.1 | 8.8 (0.5) | 6.3 (1.7) | −2.5 (1.7) | −2.9 | 7.5 (1.3) | 7.5 (1.0) | 0.0 (0.8) | 0.0 |
| Decrease in formal care hours, Decrease in informal care hours (n = 8) | 4.3 (2.0) | 4.8 (2.0) | 0.5 (1.6) | 0.9 | 7.1 (1.7) | 6.1 (2.1) | −1.0 (0.8) | −3.7 ** | 7.9 (1.6) | 7.1 (2.6) | −0.8 (1.2) | −1.8 |
| No change in formal care hours, No change in informal care hours (n = 93) | 5.1 (2.4) | 5.4 (2.4) | 0.3 (1.5) | 1.7 | 7.0 (1.9) | 6.6 (1.8) | −0.4 (1.4) | −2.6 * | 7.3 (1.9) | 7.3 (1.9) | 0.0 (1.1) | 0.3 |
| Increase in formal care hours, No change in informal care hours (n = 16) | 4.5 (2.0) | 4.6 (2.1) | 0.1 (1.0) | 0.5 | 7.3 (1.6) | 7.2 (1.7) | −0.1 (0.7) | −0.7 | 7.4 (1.3) | 7.4 (1.4) | 0.0 (0.6) | 0.0 |
| Decrease in formal care hours, No change in informal care hours (n = 29) | 5.7 (2.5) | 6.6 (2.5) | 0.9 (2.0) | 2.5 * | 6.8 (2.4) | 5.5 (2.5) | −1.3 (1.6) | −4.3 *** | 7.2 (1.7) | 6.8 (1.9) | −0.4 (1.2) | −1.9 |
| No change in formal care hours, Increase in informal care hours (n = 31) | 5.5 (2.1) | 5.5 (2.3) | −0.1 (1.7) | −0.3 | 7.1 (1.4) | 6.6 (1.6) | −0.5 (1.3) | −2.3 * | 7.5 (1.8) | 7.3 (1.4) | −0.2 (2.0) | −0.5 |
| Increase in formal care hours, Increase in informal care hours (n= 15) | 4.9 (2.1) | 6.2 (2.3) | 1.3 (1.5) | 3.2 ** | 6.9 (2.0) | 5.7 (1.9) | −1.3 (1.8) | −2.7 * | 7.5 (1.6) | 7.1 (1.8) | −0.4 (1.1) | −1.5 |
| Decrease in formal care hours, Increase in informal care hours (n= 12) | 5.3 (2.6) | 4.6 (2.6) | −0.7 (1.9) | −1.2 | 6.8 (1.6) | 6.8 (1.8) | −0.1 (1.2) | −0.2 | 6.9 (1.9) | 7.0 (1.7) | 0.1 (1.4) | 0.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bremmers, L.G.M.; Hakkaart-van Roijen, L.; Gräler, E.S.; Uyl-de Groot, C.A.; Fabbricotti, I.N. How Do Shifts in Patients with Mental Health Problems’ Formal and Informal Care Utilization Affect Informal Caregivers?: A COVID-19 Case Study. Int. J. Environ. Res. Public Health 2022, 19, 16425. https://doi.org/10.3390/ijerph192416425
Bremmers LGM, Hakkaart-van Roijen L, Gräler ES, Uyl-de Groot CA, Fabbricotti IN. How Do Shifts in Patients with Mental Health Problems’ Formal and Informal Care Utilization Affect Informal Caregivers?: A COVID-19 Case Study. International Journal of Environmental Research and Public Health. 2022; 19(24):16425. https://doi.org/10.3390/ijerph192416425
Chicago/Turabian StyleBremmers, Leonarda G. M., Leona Hakkaart-van Roijen, Eleonora S. Gräler, Carin A. Uyl-de Groot, and Isabelle N. Fabbricotti. 2022. "How Do Shifts in Patients with Mental Health Problems’ Formal and Informal Care Utilization Affect Informal Caregivers?: A COVID-19 Case Study" International Journal of Environmental Research and Public Health 19, no. 24: 16425. https://doi.org/10.3390/ijerph192416425
APA StyleBremmers, L. G. M., Hakkaart-van Roijen, L., Gräler, E. S., Uyl-de Groot, C. A., & Fabbricotti, I. N. (2022). How Do Shifts in Patients with Mental Health Problems’ Formal and Informal Care Utilization Affect Informal Caregivers?: A COVID-19 Case Study. International Journal of Environmental Research and Public Health, 19(24), 16425. https://doi.org/10.3390/ijerph192416425







