Clinical Nutrition in Portuguese Gastroenterology Departments: A Multicentric Study
Abstract
1. Introduction
- Department characterization.
- Evaluation of departments engagement in medical training and in research.
- Characterization of inpatient nutrition interventions.
- Characterization of departments’ involvement in hospital nutritional counseling.
- Enteral and parenteral feeding techniques performed.
- Evaluation of the existence and characterization of outpatient nutrition clinics.
- Obtaining suggestions from the heads of the departments for developments in nutritional practice.
2. Materials and Methods
3. Results
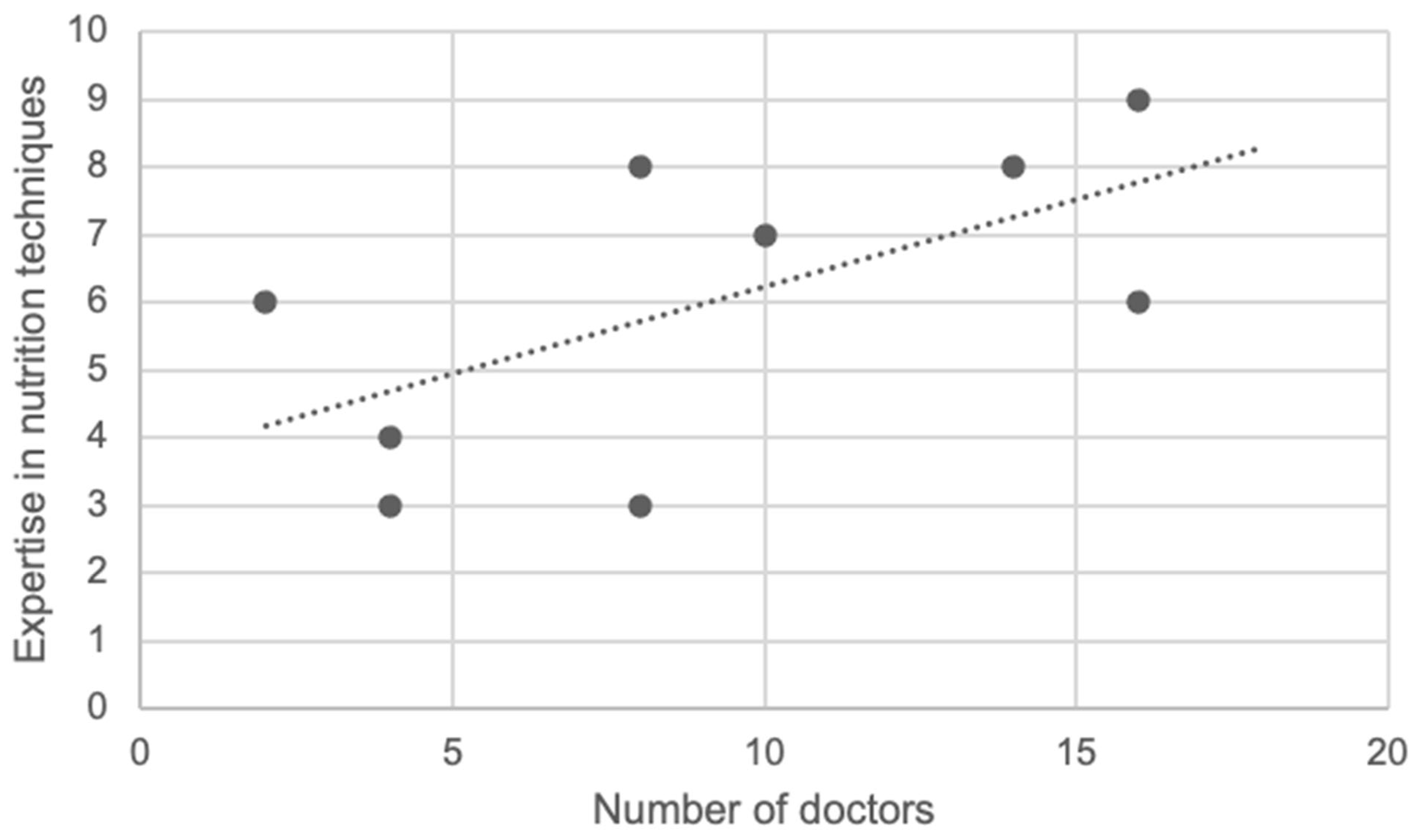
3.1. Department Characterization
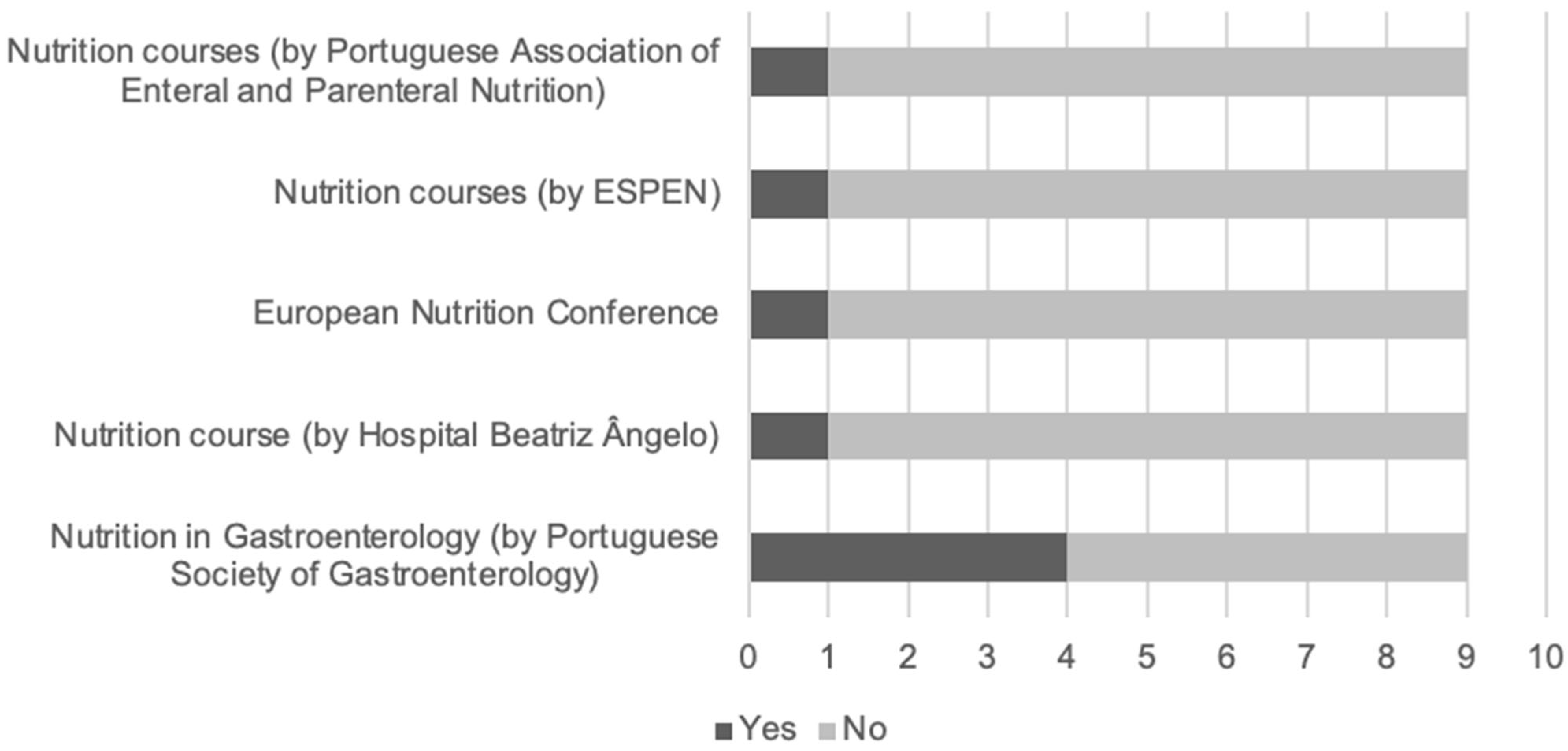
3.2. Nutrition Training and Research
3.3. Inpatient Nutrition Interventions
3.4. Department Involvement in Hospital Nutritional Counseling
3.5. Enteral and Parenteral Feeding Techniques Performed
3.6. Outpatient Nutrition Clinic
3.7. Future Development in the Nutritional Support Area
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sobotka, L. Basics in Clinical Nutrition, 4th ed.; Galen: Prague, Czech Republic, 2012. [Google Scholar]
- Bruun, L.; Bosaeus, I.; Bergstad, L.; Nygaard, K. Prevalence of undernutrition in surgical patients: Evaluation of nutritional support and documentation. Clin. Nutr. 1999, 18, 141–147. [Google Scholar] [CrossRef]
- Amaral, T.F.; Matos, L.C.; Teixeira, M.A.; Tavares, M.M.; Álvares, L.; Antunes, A. Undernutrition and associated factors among hospitalized patients. Clin. Nutr. 2010, 29, 580–585. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Romano, C.; Dipasquale, V. Nutrition in Pediatric Gastroenterology. Nutrients 2021, 13, 1965. [Google Scholar] [CrossRef]
- Jiang, J.; Hu, X.; Chen, J.; Wang, H.; Zhang, L.; Dong, B.; Yang, M. Predicting long-term mortality in hospitalized elderly patients using the new ESPEN definition. Sci. Rep. 2017, 7, 4067. [Google Scholar] [CrossRef]
- Kris-Etherton, P.M.; Akabas, S.R.; Bales, C.W.; Bistrian, B.; Braun, L.; Edwards, M.S.; Laur, C.; Lenders, C.M.; Levy, M.D.; Palmer, C.A.; et al. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Am. J. Clin. Nutr. 2014, 99, 1153s–1166s. [Google Scholar] [CrossRef]
- Harvey, J.A.H.; Neild, P.J. Nutritional training in gastroenterology. Frontline Gastroenterol. 2010, 1, 19–24. [Google Scholar] [CrossRef]
- Brett, A.; Godden, D.J.; Keenan, R. Nutritional knowledge of medical staff and students: Is present education adequate? Hum. Nutr. Appl. Nutr. 1986, 40, 217–222. [Google Scholar]
- Hopper, D.; Barker, M.E. Dietary advice, nutritional knowledge and attitudes towards nutrition in primary health care. J. Hum. Nutr. Diet. 1995, 8, 279–286. [Google Scholar] [CrossRef]
- Camburn, L.; Forbes, A. Junior doctors’ knowledge of clinical nutrition. Proc. Nutr. Soc. 2009, 68, E5. [Google Scholar] [CrossRef]
- Khan, R.F. Continuing medical education in nutrition. Am. J. Clin. Nutr. 2006, 83, 981S–984S. [Google Scholar] [CrossRef] [PubMed]
- Johansson, U.; Rasmussen, H.H.; Mowé, M.; Staun, M. Clinical nutrition in medical gastroenterology: Room for improvement. Clin. Nutr. 2009, 28, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Mowe, M.; Bosaeus, I.; Rasmussen, H.H.; Kondrup, J.; Unosson, M.; Irtun, Ø. Nutritional routines and attitudes among doctors and nurses in Scandinavia: A questionnaire based survey. Clin. Nutr. 2006, 25, 524–532. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J. Hepatol. 2019, 70, 172–193. [Google Scholar] [CrossRef]
- Raman, M.; Ghosh, S. Diet and Nutrition in IBD—Progress and Gaps. Nutrients 2019, 11, 1740. [Google Scholar] [CrossRef]
- Marriot, B.P.; Birt, D.F.; Stallings, V.A.; Yates, A.A. Present Knowledge in Nutrition, 11th ed.; Academic Press: Cambridge, MA, USA, 2020. [Google Scholar]
- Shepherd, S.J.; Gibson, P.R. Nutritional inadequacies of the gluten-free diet in both recently-diagnosed and long-term patients with coeliac disease. J. Hum. Nutr. Diet. 2013, 26, 349–358. [Google Scholar] [CrossRef]
- The European Section and Board of Gastroenterology and Hepatology. The Blue Book. Speciality Training Programme and Curriculum for Gastroenterology and Hepatology. 2017. Available online: https://www.eubogh.org/blue-book (accessed on 16 May 2022).
- Micic, D.; McDonald, E.K.; Stein, A.C.; Semrad, C.E. How to Obtain Training in Nutrition During the Gastroenterology Fellowship. Gastroenterology 2018, 154, 467–470. [Google Scholar] [CrossRef]
- Reber, E.; Messerli, M.; Stanga, Z.; Mühlebach, S. Pharmaceutical Aspects of Artificial Nutrition. J. Clin. Med. 2019, 8, 2017. [Google Scholar] [CrossRef]
- Hvas, C.L.; Farrer, K.; E Donaldson, E.; Blackett, B.; Lloyd, H.; Forde, C.; Garside, G.; Paine, P.; Lal, S. Quality and safety impact on the provision of parenteral nutrition through introduction of a nutrition support team. Eur. J. Clin. Nutr. 2014, 68, 1294–1299. [Google Scholar] [CrossRef]
- Grammatikopoulou, M.G.; Katsouda, A.; Lekka, K.; Tsantekidis, K.; Bouras, E.; Kasapidou, E.; Poulia, K.-A.; Chourdakis, M. Is continuing medical education sufficient? Assessing the clinical nutrition knowledge of medical doctors. Nutrition 2019, 57, 69–73. [Google Scholar] [CrossRef]
- Awad, S.; Herrod, P.J.; Forbes, E.; Lobo, D.N. Knowledge and attitudes of surgical trainees towards nutritional support: Food for thought. Clin. Nutr. 2010, 29, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Mowe, M.; Bosaeus, I.; Rasmussen, H.H.; Kondrup, J.; Unosson, M.; Rothenberg, E.; Irtun, Ø. Insufficient nutritional knowledge among health care workers? Clin. Nutr. 2008, 27, 196–202. [Google Scholar] [CrossRef]
- Wirth, R.; Smoliner, C.; Spamer, C.; Marburger, C.; Schreiber, F.S.; Willschrei, H.P.; Lenzen-Großimlinghaus, R.; Schäfer, R.; Volkert, D. Do doctors know how much nutrition patients need? A survey from Germany. Eur. J. Clin. Nutr. 2014, 68, 840–843. [Google Scholar] [CrossRef]
- Kamran, U.; Lee, P.C.; Coupland, B.; Abbasi, A.; Steed, H.; Ispoglou, S.; Varyani, F.; Trudgill, N. Improving 30-day mortality after PEG tube placement in England from 2007 to 2019: A retrospective national cohort analysis of 87,862 patients. Gastrointest Endosc. 2022, 96, 943–953.e11. [Google Scholar] [CrossRef]
- Nutrition Support in Adults: NICE Guideline. 2006. Available online: http://guidance.nice.org.uk/CG32/NiceGuidance/pdf/English (accessed on 18 January 2022).
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017, 36, 11–48. [Google Scholar] [CrossRef]
| Population | Ward (Beds) | Gastro Doctors | Ratio Patient/ Doctor | Type of Outpatient Clinic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AN | IBD | Hepatology | Proctology | Oncology | Pancreatic Diseases | |||||
| A | 150,000 | No | 2 | 75,000 | No | Yes | Yes | No | No | No |
| B | 120,000 | Yes (10) | 10 | 12,000 | No | Yes | Yes | Yes | No | Yes |
| C | 150,000 | No | 8 | 18,750 | Yes | Yes | Yes | Yes | No | No |
| D | 350,000 | Yes (16) | 16 | 21,975 | No | Yes | Yes | Yes | Yes | No |
| E | 295,000 | No | 4 | 73,750 | No | Yes | Yes | Yes | No | No |
| F | 130,000 | Yes (12) | 8 | 16,250 | No | Yes | Yes | Yes | No | No |
| G | 350,000 | Yes (12) | 14 | 25,000 | Yes | Yes | Yes | Yes | Yes | No |
| H | 380,000 | No | 4 | 95,000 | No | Yes | No | No | Yes | No |
| I | 278,000 | Yes (15) | 16 | 17,375 | No | Yes | Yes | Yes | Yes | Yes |
| Enteral Nutrition | Parenteral Nutrition | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| NGT | NET | PEG | PEG-J | PEJ | PVC | PICC | CVC | T-CVC | |
| A | Y (0) | Y (10) | Y (30) | Y (0) | N | Y (0) | N | Y (0) | N |
| B | Y (10) | Y (8) | Y (24) | N | N | Y (0) | Y (0) | Y (0) | Y (0) |
| C | Y (38) | Y (25) | Y (44) | Y (0) | N | Y (0) | Y (0) | Y (0) | Y (1) |
| D | Y (50) | Y (10) | Y (20) | Y (0) | Y (0) | Y (20) | N | N | N |
| E | Y (2) | Y (1) | Y (15) | N | N | N | N | N | N |
| F | Y (0) | Y (0) | Y (34) | N | N | N | N | N | N |
| G | Y (4) | Y (11) | Y (82) | Y (1) | Y (0) | Y (14) | N | Y (25) | Y (4) |
| H | Y (15) | Y (22) | Y (12) | N | N | N | N | Y (0) | N |
| I | Y (5) | Y (12) | Y (26) | Y (0) | Y (0) | Y (7) | Y (2) | Y (12) | Y (3) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vara-Luiz, F.; Glória, L.; Mocanu, I.; Curado, A.; Medeiros, I.; Duarte, M.A.; Banhudo, A.; Ferreira, S.; Vaz, A.M.; Bastos, I.; et al. Clinical Nutrition in Portuguese Gastroenterology Departments: A Multicentric Study. Int. J. Environ. Res. Public Health 2022, 19, 16333. https://doi.org/10.3390/ijerph192316333
Vara-Luiz F, Glória L, Mocanu I, Curado A, Medeiros I, Duarte MA, Banhudo A, Ferreira S, Vaz AM, Bastos I, et al. Clinical Nutrition in Portuguese Gastroenterology Departments: A Multicentric Study. International Journal of Environmental Research and Public Health. 2022; 19(23):16333. https://doi.org/10.3390/ijerph192316333
Chicago/Turabian StyleVara-Luiz, Francisco, Luísa Glória, Irina Mocanu, António Curado, Isabel Medeiros, Maria Antónia Duarte, António Banhudo, Susana Ferreira, Ana Margarida Vaz, Isabel Bastos, and et al. 2022. "Clinical Nutrition in Portuguese Gastroenterology Departments: A Multicentric Study" International Journal of Environmental Research and Public Health 19, no. 23: 16333. https://doi.org/10.3390/ijerph192316333
APA StyleVara-Luiz, F., Glória, L., Mocanu, I., Curado, A., Medeiros, I., Duarte, M. A., Banhudo, A., Ferreira, S., Vaz, A. M., Bastos, I., & Fonseca, J. (2022). Clinical Nutrition in Portuguese Gastroenterology Departments: A Multicentric Study. International Journal of Environmental Research and Public Health, 19(23), 16333. https://doi.org/10.3390/ijerph192316333







