Changes in Alcohol Consumption and Risk of Heart Failure: A Nationwide Population-Based Study in Korea
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Study Setting
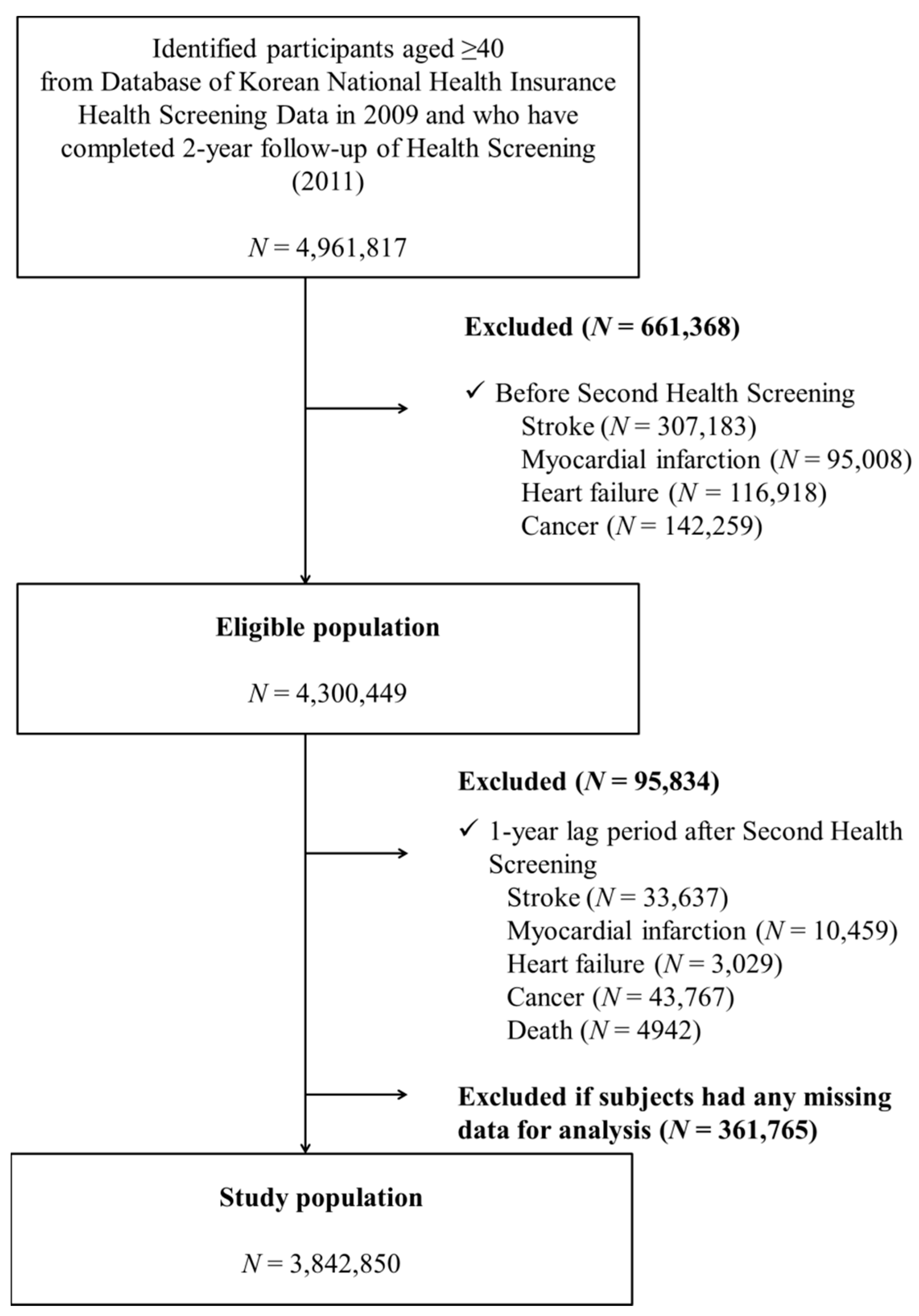
2.2. Study Population
2.3. Definition of Change in Alcohol-Intake Level
2.4. Covariates
2.5. Definition of Heart Failure and Follow-Up
2.6. Statistical Analyses
3. Results
3.1. Baseline Characteristics
3.2. Risk of Heart Failure by Change in Alcohol Consumption: Comparisons with Abstainers
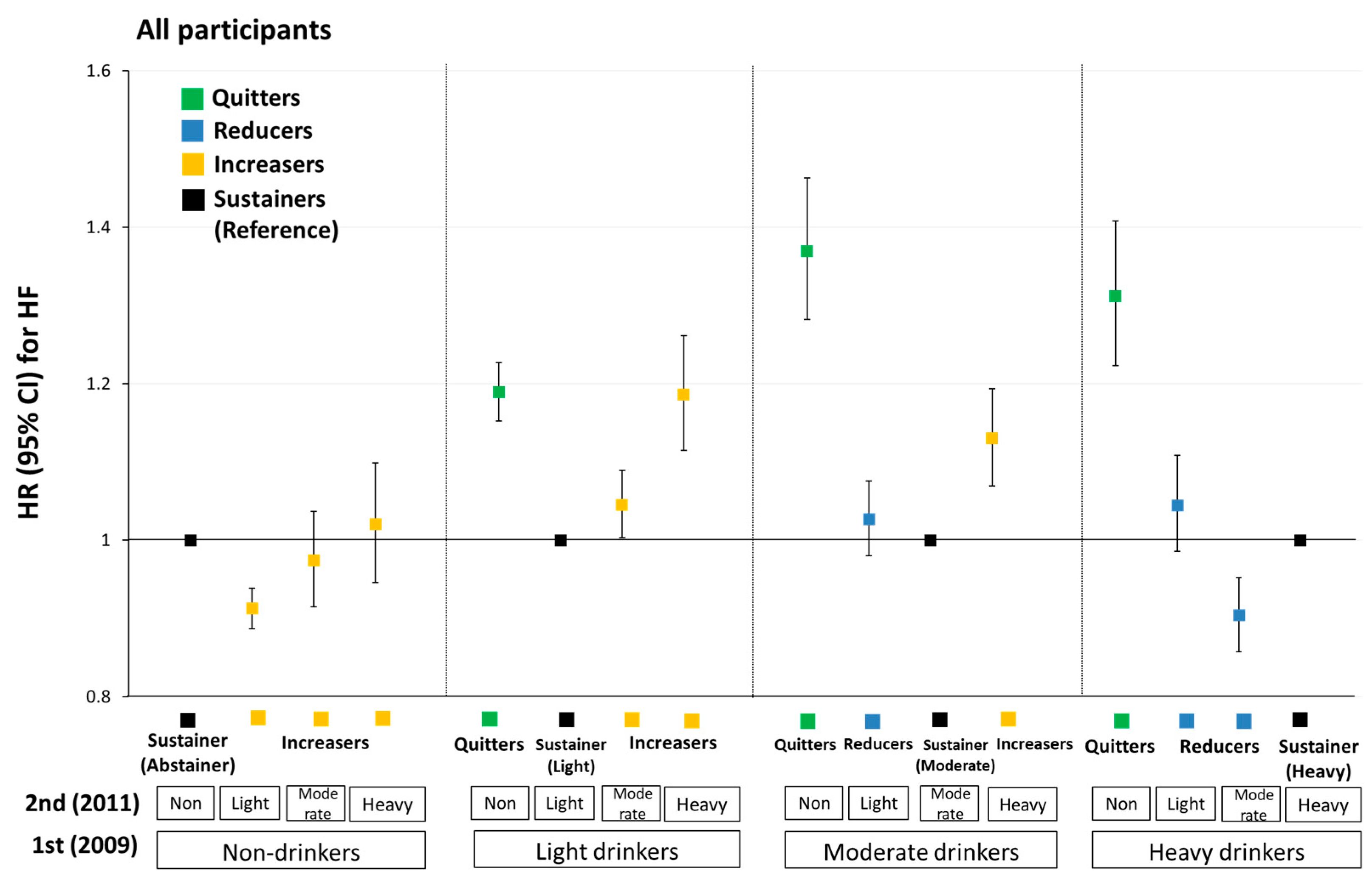
3.3. Risk of Heart Failure by Change in Alcohol Consumption: Comparison with Sustainers
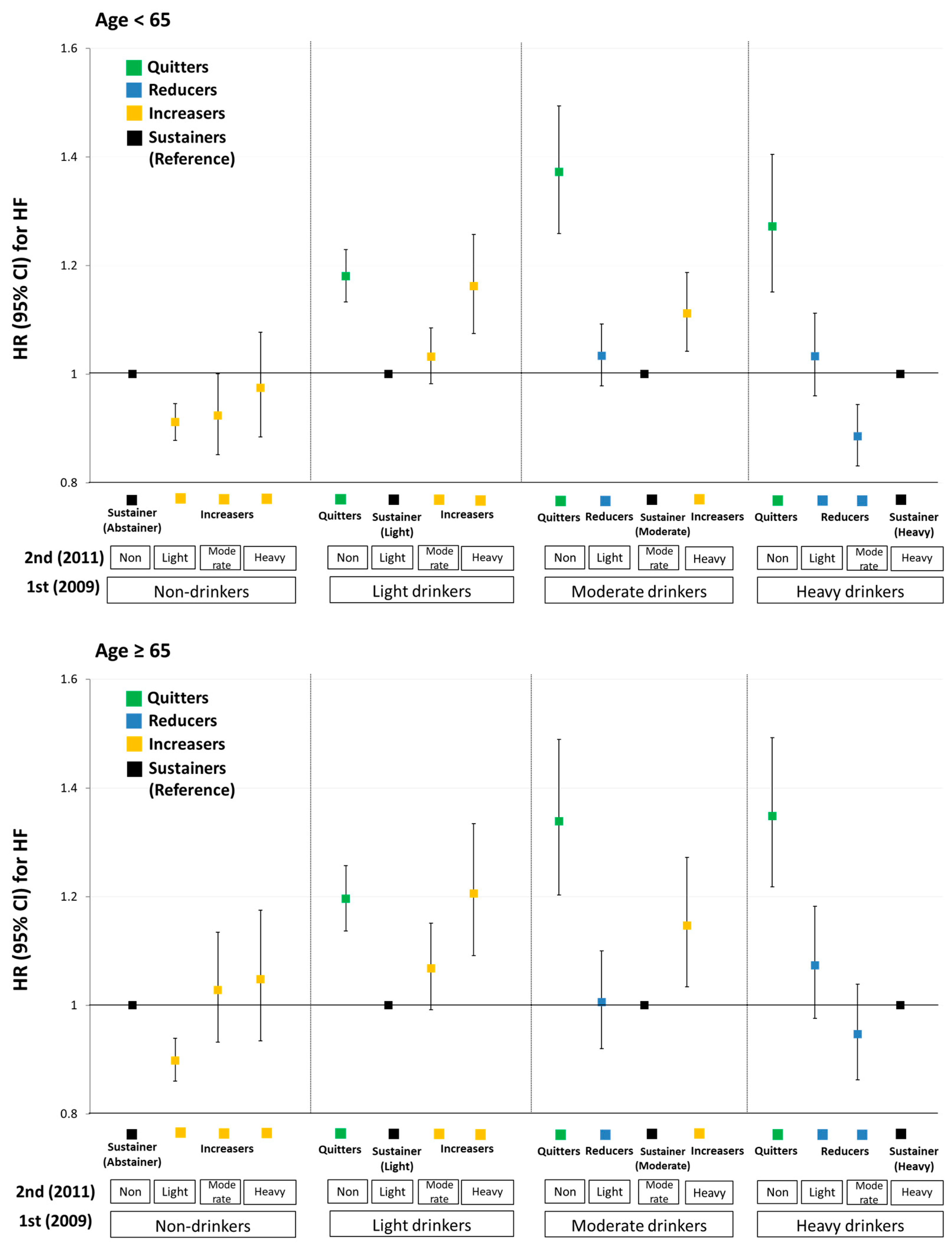
3.4. Stratified Analyses by Age, Sex, and Smoking Status
4. Discussion
4.1. Harmful Effects of Heavy Drinking
4.2. Quitting Alcohol Intake
4.3. Age Differences
4.4. Gender Differences
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Bohm, M.; Burri, H.; Butler, J.; Celutkiene, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Smeets, M.; Vaes, B.; Mamouris, P.; Van Den Akker, M.; Van Pottelbergh, G.; Goderis, G.; Janssens, S.; Aertgeerts, B.; Henrard, S. Burden of heart failure in Flemish general practices: A registry-based study in the Intego database. BMJ Open 2019, 9, e022972. [Google Scholar] [CrossRef] [PubMed]
- McManus, D.D.; Yin, X.; Gladstone, R.; Vittinghoff, E.; Vasan, R.S.; Larson, M.G.; Benjamin, E.J.; Marcus, G.M. Alcohol Consumption, Left Atrial Diameter, and Atrial Fibrillation. J. Am. Heart Assoc. 2016, 5, e004060. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Drca, N.; Wolk, A. Alcohol consumption and risk of atrial fibrillation: A prospective study and dose-response meta-analysis. J. Am. Coll. Cardiol. 2014, 64, 281–289. [Google Scholar] [CrossRef]
- Ruidavets, J.-B.; Ducimetière, P.; Evans, A.; Montaye, M.; Haas, B.; Bingham, A.; Yarnell, J.; Amouyel, P.; Arveiler, D.; Kee, F.; et al. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: The Prospective Epidemiological Study of Myocardial Infarction (PRIME). Br. Med. J. 2010, 341, c6077. [Google Scholar] [CrossRef]
- McMurray, J.J.; Pfeffer, M.A. Heart failure. Lancet 2005, 365, 1877–1889. [Google Scholar] [CrossRef]
- Briasoulis, A.; Agarwal, V.; Messerli, F.H. Alcohol consumption and the risk of hypertension in men and women: A systematic review and meta-analysis. J. Clin. Hypertens. 2012, 14, 792–798. [Google Scholar] [CrossRef]
- Long, M.J.; Jiang, C.Q.; Lam, T.H.; Lin, J.M.; Chan, Y.H.; Zhang, W.S.; Jin, Y.L.; Liu, B.; Thomas, G.N.; Cheng, K.K. Alcohol consumption and electrocardiographic left ventricular hypertrophy and mediation by elevated blood pressure in older Chinese men: The Guangzhou Biobank Cohort Study. Alcohol 2013, 47, 473–480. [Google Scholar] [CrossRef]
- Li, Z.; Guo, X.; Bai, Y.; Sun, G.; Guan, Y.; Sun, Y.; Roselle, A.M. The Association Between Alcohol Consumption and Left Ventricular Ejection Fraction: An Observational Study on a General Population. Medicine 2016, 95, e3763. [Google Scholar] [CrossRef]
- Larsson, S.C.; Orsini, N.; Wolk, A. Alcohol consumption and risk of heart failure: A dose-response meta-analysis of prospective studies. Eur. J. Heart Fail. 2015, 17, 367–373. [Google Scholar] [CrossRef]
- Wannamethee, S.G.; Whincup, P.H.; Lennon, L.; Papacosta, O.; Shaper, A.G. Alcohol consumption and risk of incident heart failure in older men: A prospective cohort study. Open Heart 2015, 2, e000266. [Google Scholar] [CrossRef] [PubMed]
- Walsh, C.R.; Larson, M.G.; Evans, J.C.; Djousse, L.; Ellison, R.C.; Vasan, R.S.; Levy, D. Alcohol consumption and risk for congestive heart failure in the Framingham Heart Study. Ann. Intern. Med. 2002, 136, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Global Status Report on Alcohol and Health 2018; CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2018.
- Klatsky, A.L.; Chartier, D.; Udaltsova, N.; Gronningen, S.; Brar, S.; Friedman, G.D.; Lundstrom, R.J. Alcohol drinking and risk of hospitalization for heart failure with and without associated coronary artery disease. Am. J. Cardiol. 2005, 96, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Bryson, C.L.; Mukamal, K.J.; Mittleman, M.A.; Fried, L.P.; Hirsch, C.H.; Kitzman, D.W.; Siscovick, D.S. The association of alcohol consumption and incident heart failure: The Cardiovascular Health Study. J. Am. Coll. Cardiol. 2006, 48, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Djoussé, L.; Gaziano, J.M. Alcohol consumption and risk of heart failure in the Physicians’ Health Study I. Circulation 2007, 115, 34–39. [Google Scholar] [CrossRef]
- Gemes, K.; Janszky, I.; Ahnve, S.; Laszlo, K.D.; Laugsand, L.E.; Vatten, L.J.; Mukamal, K.J. Light-to-moderate drinking and incident heart failure--the Norwegian HUNT study. Int. J. Cardiol. 2016, 203, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Wallin, A.; Wolk, A. Contrasting association between alcohol consumption and risk of myocardial infarction and heart failure: Two prospective cohorts. Int. J. Cardiol. 2017, 231, 207–210. [Google Scholar] [CrossRef] [PubMed]
- Dorans, K.S.; Mostofsky, E.; Levitan, E.B.; Hakansson, N.; Wolk, A.; Mittleman, M.A. Alcohol and incident heart failure among middle-aged and elderly men: Cohort of Swedish men. Circ. Heart Fail. 2015, 8, 422–427. [Google Scholar] [CrossRef]
- Goncalves, A.; Claggett, B.; Jhund, P.S.; Rosamond, W.; Deswal, A.; Aguilar, D.; Shah, A.M.; Cheng, S.; Solomon, S.D. Alcohol consumption and risk of heart failure: The Atherosclerosis Risk in Communities Study. Eur. Heart J. 2015, 36, 939–945. [Google Scholar] [CrossRef]
- Abramson, J.L.; Williams, S.A.; Krumholz, H.M.; Vaccarino, V. Moderate alcohol consumption and risk of heart failure among older persons. J. Am. Med. Assoc. 2001, 285, 1971–1977. [Google Scholar] [CrossRef]
- Janszky, I.; Ljung, R.; Ahnve, S.; Hallqvist, J.; Bennet, A.M.; Mukamal, K.J. Alcohol and long-term prognosis after a first acute myocardial infarction: The SHEEP study. Eur. Heart J. 2008, 29, 45–53. [Google Scholar] [CrossRef]
- Wang, Y.; Tuomilehto, J.; Jousilahti, P.; Antikainen, R.; Mähönen, M.; Katzmarzyk, P.T.; Hu, G. Lifestyle factors in relation to heart failure among Finnish men and women. Circ. Heart Fail. 2011, 4, 607–612. [Google Scholar] [CrossRef]
- Aguilar, D.; Skali, H.; Moyé, L.A.; Lewis, E.F.; Gaziano, J.M.; Rutherford, J.D.; Hartley, L.H.; Randall, O.S.; Geltman, E.M.; Lamas, G.A.; et al. Alcohol consumption and prognosis in patients with left ventricular systolic dysfunction after a myocardial infarction. J. Am. Coll. Cardiol. 2004, 43, 2015–2021. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Cho, J.; Park, J.H.; Cho, B. National General Health Screening Program in Korea: History, current status, and future direction. Precis. Future Med. 2022, 6, 9–31. [Google Scholar] [CrossRef]
- Kim, Y.G.; Han, K.-D.; Choi, J.-I.; Boo, K.Y.; Kim, D.Y.; Lee, K.-N.; Shim, J.; Kim, J.S.; Kim, Y.-H. Frequent drinking is a more important risk factor for new-onset atrial fibrillation than binge drinking: A nationwide population-based study. EP Eur. 2019, 22, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Dietary Guidelines for Americans 2015–2020, 8th ed.; U.S. Department of Health and Human Services: Washington, DC, USA; U.S. Department of Agriculture: Washington, DC, USA, 2015. Available online: http://health.gov/dietaryguidelines/2015/guidelines (accessed on 9 August 2020).
- Jeong, S.M.; Lee, H.R.; Han, K.; Jeon, K.H.; Kim, D.; Yoo, J.E.; Cho, M.H.; Chun, S.; Lee, S.P.; Nam, K.W.; et al. Association of Change in Alcohol Consumption With Risk of Ischemic Stroke. Stroke 2022, 53, 2488–2496. [Google Scholar] [CrossRef]
- Yoo, J.E.; Han, K.; Shin, D.W.; Kim, D.; Kim, B.S.; Chun, S.; Jeon, K.H.; Jung, W.; Park, J.; Park, J.H.; et al. Association Between Changes in Alcohol Consumption and Cancer Risk. JAMA Netw. Open 2022, 5, e2228544. [Google Scholar] [CrossRef]
- Hendriks, H.F.J. Moderate Alcohol Consumption and Insulin Sensitivity: Observations and Possible Mechanisms. Ann. Epidemiol. 2007, 17, S40–S42. [Google Scholar] [CrossRef]
- Bui, A.L.; Horwich, T.B.; Fonarow, G.C. Epidemiology and risk profile of heart failure. Nat. Rev. Cardiol. 2011, 8, 30–41. [Google Scholar] [CrossRef]
- Brien, S.E.; Ronksley, P.E.; Turner, B.J.; Mukamal, K.J.; Ghali, W.A. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: Systematic review and meta-analysis of interventional studies. Br. Med. J. 2011, 342, d636. [Google Scholar] [CrossRef]
- O’Keefe, J.H.; Bybee, K.A.; Lavie, C.J. Alcohol and cardiovascular health: The razor-sharp double-edged sword. J. Am. Coll. Cardiol. 2007, 50, 1009–1014. [Google Scholar] [CrossRef] [PubMed]
- Gianoulakis, C.; Guillaume, P.; Thavundayil, J.; Gutkowska, J. Increased plasma atrial natriuretic peptide after ingestion of low doses of ethanol in humans. Alcohol. Clin. Exp. Res. 1997, 21, 162–170. [Google Scholar] [CrossRef] [PubMed]
- Piano, M.R.; Phillips, S.A. Alcoholic cardiomyopathy: Pathophysiologic insights. Cardiovasc. Toxicol. 2014, 14, 291–308. [Google Scholar] [CrossRef] [PubMed]
- Lewer, D.; Meier, P.; Beard, E.; Boniface, S.; Kaner, E. Unravelling the alcohol harm paradox: A population-based study of social gradients across very heavy drinking thresholds. BMC Public Health 2016, 16, 599. [Google Scholar] [CrossRef] [PubMed]
- Fillmore, K.M.; Stockwell, T.; Chikritzhs, T.; Bostrom, A.; Kerr, W. Moderate alcohol use and reduced mortality risk: Systematic error in prospective studies and new hypotheses. Ann. Epidemiol. 2007, 17, S16–S23. [Google Scholar] [CrossRef]
- Meier, P.; Seitz, H.K. Age, alcohol metabolism and liver disease. Curr. Opin. Clin. Nutr. Metab. Care 2008, 11, 21–26. [Google Scholar] [CrossRef]
- Oneta, C.M.; Pedrosa, M.; Rüttimann, S.; Russell, R.M.; Seitz, H.K. Age and bioavailability of alcohol. Z. Gastroenterol. 2001, 39, 783–788. [Google Scholar] [CrossRef]
- Gärtner, U.; Schmier, M.; Bogusz, M.; Seitz, H.K. Blood alcohol concentrations after oral alcohol administration—Effect of age and sex. Z. Gastroenterol. 1996, 34, 675–679. [Google Scholar]
- Fernández-Solà, J.; Estruch, R.; Nicolás, J.M.; Paré, J.C.; Sacanella, E.; Antúnez, E.; Urbano-Márquez, A. Comparison of alcoholic cardiomyopathy in women versus men. Am. J. Cardiol. 1997, 80, 481–485. [Google Scholar] [CrossRef]
- Ikehara, S.; Iso, H.; Toyoshima, H.; Date, C.; Yamamoto, A.; Kikuchi, S.; Kondo, T.; Watanabe, Y.; Koizumi, A.; Wada, Y.; et al. Alcohol consumption and mortality from stroke and coronary heart disease among Japanese men and women: The Japan collaborative cohort study. Stroke 2008, 39, 2936–2942. [Google Scholar] [CrossRef]
- Frezza, M.; di Padova, C.; Pozzato, G.; Terpin, M.; Baraona, E.; Lieber, C.S. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N. Engl. J. Med. 1990, 322, 95–99. [Google Scholar] [CrossRef] [PubMed]

| Change in Alcohol Consumption on Subsequent Two Health Examinations | ||||||
|---|---|---|---|---|---|---|
| Variables | Abstainers | Quitters | Reducers | Sustainers | Increasers | p Value |
| (N = 1,801,711) | (N = 305,487) | (N = 279,756) | (N = 921,802) | (N = 534,094) | ||
| Mean age, years (mean ± SD) | 57.1 ± 9.9 | 54.7 ± 9.51 | 52.7 ± 8.5 | 52.1 ± 8.4 | 53.0 ± 8.8 | <0.001 |
| Men (N, %) | 465,296 (25.8) | 168,267 (55.1) | 254,748 (91.1) | 731,139 (79.3) | 381,938 (71.5) | <0.001 |
| Alcohol consumption in 2009 † (N, %) | ||||||
| None | 1,801,711 (100.0) | NA | NA | NA | 293,439 (54.9) | <0.001 |
| Light (<15 g/day) | NA | 248,072 (81.2) | NA | 616,935 (66.9) | 166,672 (31.2) | |
| Moderate (15–29 g/day) | NA | 35,445 (11.6) | 148,992 (53.3) | 166,252 (18.0) | 73,983 (13.9) | |
| Heavy (≥30 g/day) | NA | 21,970 (7.2) | 130,764 (46.7) | 138,615 (15.1) | NA | |
| Alcohol frequency in 2009 † (N, %) | ||||||
| None | 1,801,711 (100.0) | NA | NA | NA | 293,439 (54.9) | <0.001 |
| 1–2 days/week | NA | 252,159 (82.5) | 107,267 (38.3) | 663,079 (71.9) | 170,129 (31.9) | |
| 3–4 days/week | NA | 33,549 (11.0) | 115,054(41.1) | 177,049 (19.2) | 58,549 (11.0) | |
| 5–7 days/week | NA | 19,779 (6.5) | 57,435 (20.5) | 81,674 (8.9) | 11,977 (2.2) | |
| Alcohol consumption amount per occasion in 2009 † (N, %) | ||||||
| None | 1,801,711 (100.0) | NA | NA | NA | 293,439 (54.9) | <0.001 |
| 1–2 drinks | NA | 108,462 (35.5) | 2265 (0.8) | 140,926 (15.3) | 23,152 (4.3) | |
| 3–4 drinks | NA | 92,875 (30.4) | 15,593 (5.6) | 254,419 (27.6) | 59,146 (11.1) | |
| 5–7 drinks | NA | 69,679 (22.8) | 119,126 (42.6) | 313,865 (34.1) | 104,709 (19.6) | |
| ≥8 drinks | NA | 34,459 (11.3) | 142,772 (51.0) | 212,557 (23.0) | 53,635 (10.1) | |
| Smoking status (N, %) | ||||||
| None | 1,523,503 (84.6) | 214,390 (70.2) | 72,942 (26.1) | 345,310 (37.5) | 233,659 (43.7) | <0.001 |
| Former smoker | 143,938 (8.0) | 46,060 (15.1) | 88,245 (31.5) | 272,373 (29.5) | 136,563 (25.6) | |
| Current, <10 cigarettes/day | 16,888 (0.9) | 6355 (2.0) | 12,424 (4.4) | 32,551 (3.5) | 17,042 (3.2) | |
| Current, 10–19 cigarettes/day | 49,823 (2.8) | 17,405 (5.7) | 47,488 (17.0) | 122,194 (13.3) | 60,155 (11.3) | |
| Current, ≥20 cigarettes/day | 67,559 (3.7) | 21,277 (7.0) | 58,657 (21.0) | 149,374 (16.2) | 86,675 (16.2) | |
| Physical activity (N, %) | <0.001 | |||||
| None | 1,435,610 (79.7) | 242,945 (79.5) | 210,334 (75.2) | 695,520 (75.4) | 405,783 (76.0) | |
| Moderate or vigorous intensity | 271,384 (15.1) | 45,502 (14.9) | 52,538 (18.8) | 172,323 (18.7) | 95,913 (18.0) | |
| Moderate and vigorous intensity | 94,717 (5.3) | 17,040 (5.6) | 16,884 (6.0) | 53,959 (5.9) | 32,398 (6.0) | |
| Anthropometrics (mean ± SD) | ||||||
| Body mass index, kg/m2 | 23.8 ± 3.1 | 23.9 ± 2.9 | 24.3 ± 2.9 | 24.0 ± 2.8 | 24.1 ± 2.9 | <0.001 |
| WC, cm | 79.4 ± 8.5 | 81.0 ±8.5 | 84.0 ± 7.6 | 82.5 ± 8.0 | 82.3 ±8.3 | <0.001 |
| SBP, mmHg | 122.8 ± 15.2 | 122.9 ± 14.7 | 126.4 ± 14.2 | 124.5 ± 14.3 | 124.6 ± 14.7 | <0.001 |
| DBP, mmHg | 75.7 ± 9.8 | 76.5 ± 9.8 | 79.4 ± 9.8 | 78.2 ± 9.8 | 78.1 ± 10.0 | <0.001 |
| Comorbidity (N, %) | ||||||
| Hypertension | 599,286 (33.4) | 97,494 (31.9) | 102,788 (36.7) | 292,549 (31.7) | 175,562 (32.9) | <0.001 |
| Diabetes mellitus | 192,576 (10.7) | 33,787 (11.1) | 36,364 (13.0) | 95,973 (10.4) | 60,210 (11.3) | <0.001 |
| Dyslipidemia | 462,493 (25.7) | 67,774 (22.2) | 58,547 (20.9) | 181,123 (19.7) | 108,434 (20.3) | <0.001 |
| CKD | 119,568 (6.6) | 15,407 (5.0) | 10,775 (3.9) | 36,648 (4.0) | 22,126 (4.1) | <0.001 |
| Laboratory findings (mean ± SD) | ||||||
| Glucose, mg/dL | 97.9 ± 22.2 | 99.3 ± 23.7 | 102.9 ± 25.7 | 100.6 ± 23.7 | 101.0 ± 24.9 | <0.001 |
| Total cholesterol, mg/dL | 199.9 ± 36.9 | 197.9 ± 36.5 | 197.8 ± 35.7 | 198.0 ± 35.1 | 198.2 ±35.6 | <0.001 |
| HDL, mg/dL | 54.8 ± 16.6 | 54.5 ± 17.4 | 54.8 ± 17.4 | 55.3 ± 17.4 | 55.9 ± 18.3 | <0.001 |
| LDL, mg/dL | 120.7 ± 33.8 | 117.9 ± 33.8 | 112.4 ± 34.7 | 114.7± 33.8 | 114.6 ± 34.0 | <0.001 |
| GFR, mL/min/1.73 m2 | 86.9 ± 31.0 | 87.9 ± 32.4 | 89.0 ± 38.1 | 88.3 ± 37.5 | 88.7 ± 35.2 | <0.001 |
| Urban residency, (N, %) | 798,440 (44.3) | 138,208 (45.2) | 127,960 (45.7) | 438,405 (47.6) | 242,026 (45.3) | <0.001 |
| Income, (N, %) | ||||||
| Q1 (lowest) | 472,769 (26.2) | 74,015 (24.2) | 50,931 (18.2) | 172,525 (18.7) | 114,141 (21.4) | <0.001 |
| Q2 | 341,643 (19.0) | 58,962 (19.3) | 46,497 (16.6) | 151,333 (16.4) | 94,576 (17.7) | |
| Q3 | 411,182 (22.8) | 71,332 (23.4) | 70,834 (25.3) | 217,490 (23.6) | 126,751 (23.7) | |
| Q4 (highest) | 576,117 (32.0) | 101,178 (33.1) | 111,494 (39.9) | 380,454 (41.3) | 198,626 (37.2) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeo, Y.; Jeong, S.-M.; Shin, D.W.; Han, K.; Yoo, J.; Yoo, J.E.; Lee, S.-P. Changes in Alcohol Consumption and Risk of Heart Failure: A Nationwide Population-Based Study in Korea. Int. J. Environ. Res. Public Health 2022, 19, 16265. https://doi.org/10.3390/ijerph192316265
Yeo Y, Jeong S-M, Shin DW, Han K, Yoo J, Yoo JE, Lee S-P. Changes in Alcohol Consumption and Risk of Heart Failure: A Nationwide Population-Based Study in Korea. International Journal of Environmental Research and Public Health. 2022; 19(23):16265. https://doi.org/10.3390/ijerph192316265
Chicago/Turabian StyleYeo, Yohwan, Su-Min Jeong, Dong Wook Shin, Kyungdo Han, Juhwan Yoo, Jung Eun Yoo, and Seung-Pyo Lee. 2022. "Changes in Alcohol Consumption and Risk of Heart Failure: A Nationwide Population-Based Study in Korea" International Journal of Environmental Research and Public Health 19, no. 23: 16265. https://doi.org/10.3390/ijerph192316265
APA StyleYeo, Y., Jeong, S.-M., Shin, D. W., Han, K., Yoo, J., Yoo, J. E., & Lee, S.-P. (2022). Changes in Alcohol Consumption and Risk of Heart Failure: A Nationwide Population-Based Study in Korea. International Journal of Environmental Research and Public Health, 19(23), 16265. https://doi.org/10.3390/ijerph192316265






