The PRISMA 2020 Statement: A System Review of Hospital Preparedness for Bioterrorism Events
Abstract
1. Introduction
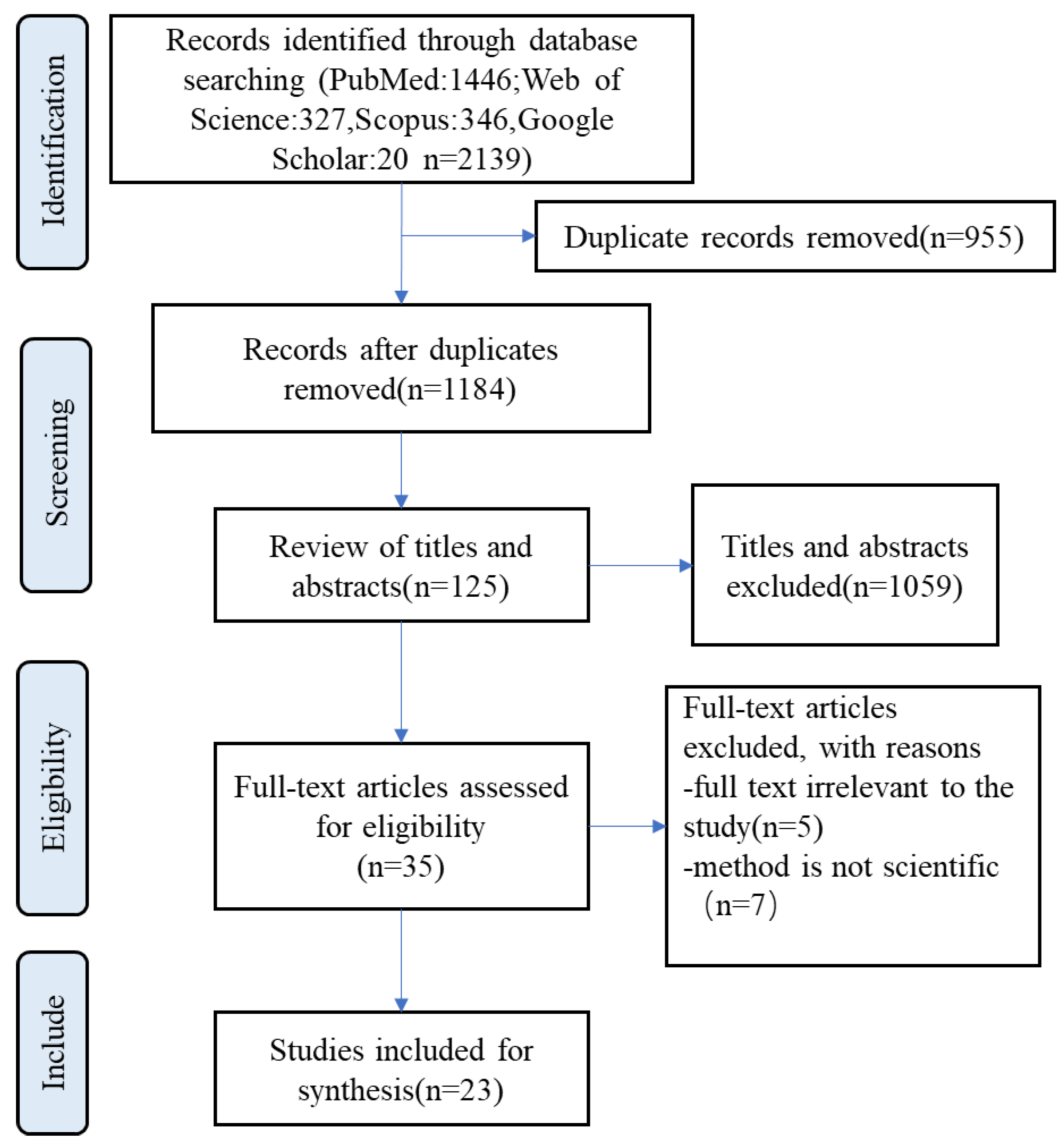
2. Methods
2.1. Search Strategies and Databases
2.2. Selection Process and Eligibility Criteria
2.3. Quality Assessment
3. Results
3.1. Quantitative Analysis
3.2. Qualitative Analysis
3.2.1. Emergency Management
Bioterrorism Response
Risk Communication
Training and Drills
Leadership
3.2.2. Medical Service Capacity
Monitoring and Warning
Emergency Medical Services
Patient Management
Prevention and Control of Infections
Corpse Disposal
3.2.3. Surge Capacity
Human Resources
Medical Equipment
Pharmaceutical Reserve
3.2.4. Laboratories
3.2.5. Regional Coordination
3.2.6. Logistical Support
4. Discussion
4.1. Emergency Management
4.2. Medical Service Capacity
4.3. Surge Capacity
4.4. Laboratories
4.5. Regional Coordination
4.6. Logistical Support
5. Limitation
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rathjen, N.A.; Shahbodaghi, S.D. Bioterrorism. Am. Fam. Physician 2021, 104, 376–385. [Google Scholar] [PubMed]
- Perry, R.W.; Lindell, M.K. Hospital planning for weapons of mass destruction incidents. J. Postgrad. Med. 2006, 52, 116–120. [Google Scholar] [PubMed]
- Williams, M.; Armstrong, L.; Sizemore, D.C. Biologic, Chemical, and Radiation Terrorism Review. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2022. [Google Scholar]
- Novossiolova, T.A.; Whitby, S.; Dando, M.; Pearson, G.S. The vital importance of a web of prevention for effective biosafety and biosecurity in the twenty-first century. One Health Outlook 2021, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- Schultz, C.H.; Mothershead, J.L.; Field, M. Bioterrorism preparedness. I: The emergency department and hospital. Emerg. Med. Clin. North Am. 2002, 20, 437–455. [Google Scholar] [CrossRef] [PubMed]
- Pearson, L.; Pelling, M. The UN Sendai Framework for Disaster Risk Reduction 2015–2030: Negotiation Process and Prospects for Science and Practice. J. Extrem. Events 2015, 2, 1571001. [Google Scholar] [CrossRef]
- Wang, Y.S.; Sun, H.J.; Zou, J.C.; Ning, J.; Du, Y. Evaluation Model for Hospital Response Capability for Public Health Emergency. Disaster Med. Public Health Prep. 2021, 15, 403–408. [Google Scholar] [CrossRef]
- Rapid Hospital Readiness Checklist. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-hospital-readiness-checklist-2020.1 (accessed on 30 April 2022).
- Dean, M.D.; Nair, S.K. Mass-casualty triage: Distribution of victims to multiple hospitals using the SAVE model. Eur. J. Oper. Res. 2014, 238, 363–373. [Google Scholar] [CrossRef]
- Levy, L.A.; Rokusek, C.F.; Bragg, S.M.; Howell, J.T. Interdisciplinary approach to all-hazards preparedness: Are you ready? How do we know? J. Public Health Manag. Pract. 2009, 15 (Suppl. 2), S8–S12. [Google Scholar] [CrossRef]
- Jha, A.; Lin, L.; Short, S.M.; Argentini, G.; Gamhewage, G.; Savoia, E. Integrating emergency risk communication (ERC) into the public health system response: Systematic review of literature to aid formulation of the 2017 WHO Guideline for ERC policy and practice. PLoS ONE 2018, 13, e0205555. [Google Scholar] [CrossRef]
- Olivieri, C.; Ingrassia, P.L.; Della Corte, F.; Carenzo, L.; Sapori, J.M.; Gabilly, L.; Segond, F.; Grieger, F.; Arnod-Prin, P.; Larrucea, X.; et al. Hospital preparedness and response in CBRN emergencies: TIER assessment tool. Eur. J. Emerg. Med. 2017, 24, 366–370. [Google Scholar] [CrossRef]
- Alexander, G.C.; Larkin, G.L.; Wynia, M.K. Physicians’ preparedness for bioterrorism and other public health priorities. Acad. Emerg. Med. 2006, 13, 1238–1241. [Google Scholar] [CrossRef]
- Beyramijam, M.; Farrokhi, M.; Ebadi, A.; Masoumi, G.; Khankeh, H.R. Disaster preparedness in emergency medical service agencies: A systematic review. J. Educ. Health Promot. 2021, 10, 258. [Google Scholar]
- Morgan, O. Infectious disease risks from dead bodies following natural disasters. Rev. Panam. Salud Publica 2004, 15, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Al-Shareef, A.S.; Alsulimani, L.K.; Bojan, H.M.; Masri, T.M.; Grimes, J.O.; Molloy, M.S.; Ciottone, G.R. Evaluation of Hospitals’ Disaster Preparedness Plans in the Holy City of Makkah (Mecca): A Cross-Sectional Observation Study. Prehospital Disaster Med. 2017, 32, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Aminizadeh, M.; Farrokhi, M.; Ebadi, A.; Masoumi, G.R.; Kolivand, P.; Khankeh, H.R. Hospital management preparedness tools in biological events: A scoping review. J. Educ. Health Promot. 2019, 8, 234. [Google Scholar] [PubMed]
- Bennett, R.L. Chemical or Biological Terrorist Attacks: An Analysis of the Preparedness of Hospitals for Managing Victims Affected by Chemical or Biological Weapons of Mass Destruction. Int. J. Environ. Res. Public Health 2006, 3, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Monfared, Y.K.; Jamaly, Z.; Keykale, M.S.; Asgary, J.; Khoshghadam, M.; Farzam, S.A.; Gholami, S. How is training hospitals of Qazvin preparedness against disaster in 2015? Ann. Trop. Med. Public Health 2017, 10, 1205–1214. [Google Scholar]
- Kalish, B.T.; Gaydos, C.A.; Hsieh, Y.H.; Christensen, B.E.; Carroll, K.C.; Cannons, A.; Cattani, J.A.; Rothman, R.E. National survey of Laboratory Response Network sentinel laboratory preparedness. Disaster Med. Public Health Prep. 2009, 3 (Suppl. 2), S17–S23. [Google Scholar] [CrossRef]
- Hick, J.L.; Hanfling, D.; Burstein, J.L.; DeAtley, C.; Barbisch, D.; Bogdan, G.M.; Cantrill, S. Health care facility and community strategies for patient care surge capacity. Ann. Emerg. Med. 2004, 44, 253–256. [Google Scholar] [CrossRef]
- Toyokawa, T.; Hori, N.; Kato, Y. Preparedness at Japan’s Hospitals Designated for Patients with Highly Infectious Diseases. Health Secur. 2017, 15, 97–103. [Google Scholar] [CrossRef]
- Aminizadeh, M.; Farrokhi, M.; Ebadi, A.; Masoumi, G.; Kolivand, P.; Khankeh, H. Hospital Preparedness Challenges in Biological Disasters: A Qualitative Study. Disaster Med. Public Health Prep. 2020, 16, 956–960. [Google Scholar] [CrossRef] [PubMed]
- Aghabeigi, M.; Taghinejad, H.; Mozafari, M.; Khorshidi, A. Effect of Bioterrorism Management Education on Nurses’ Knowledge. Pak. J. Med. Health Sci. 2020, 14, 1550–1554. [Google Scholar]
- Jasper, E.; Miller, M.; Sweeney, B.; Berg, D.; Feuer, E.; Reganato, D. Preparedness of hospitals to respond to a radiological terrorism event as assessed by a full-scale exercise. J. Public Health Manag. Pract. 2005, 11, S11–S16. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, R.L.; Battaglia, A.; Perpetua, Z.; Wojtaszek, K.; Campbell, G. The Clinical Nurse Leader and COVID-19: Leadership and quality at the point of care. J. Prof. Nurs. 2020, 36, 178–180. [Google Scholar]
- Bogucki, S.; Jubanyik, K. Triage, rationing, and palliative care in disaster planning. Biosecur. Bioterror. 2009, 7, 221–224; discussion 224. [Google Scholar] [CrossRef]
- Caldicott, D.G.; Edwards, N.A.; Tingey, D.; Bonnin, R. Medical response to a terrorist attack and weapons of mass destruction. Emerg. Med. 2002, 14, 230–239. [Google Scholar] [CrossRef]
- Mackie, B.R.; Weber, S.; Mitchell, M.L.; Crilly, J.; Wilson, B.; Handy, M.; Wullschleger, M.; Sharpe, J.; McCaffery, K.; Lister, P.; et al. Chemical, Biological, Radiological, or Nuclear Response in Queensland Emergency Services: A Multisite Study. Health Secur. 2022, 20, 222–229. [Google Scholar] [CrossRef]
- Kwon, N.; Raven, M.C.; Chiang, W.K.; Moran, G.J.; Jui, J.; Carter, R.A.; Goldfrank, L.; EMERGEncy ID Net Study Group. Emergency Physicians Perspectives on Smallpox Vaccination. Acad. Emerg. Med. 2003, 10, 599–605. [Google Scholar] [CrossRef]
- Mortelmans, L.J.M.; Gaakeer, M.I.; Dieltiens, G.; Anseeuw, K.; Sabbe, M.B. Are Dutch Hospitals Prepared for Chemical, Biological, or Radionuclear Incidents? A Survey Study. Prehosp. Disaster. Med. 2017, 32, 483–491. [Google Scholar] [CrossRef]
- Shearer, D.A. Management styles and motivation. Radiol. Manag. 2012, 34, 47–52. [Google Scholar]
- Niska, R.W.; Burt, C.W. Emergency response planning in hospitals, United States: 2003–2004. Adv. Data 2007, 391, 1–13. [Google Scholar]
- Asefzadeh, S.; Varyani, A.S.; Gholami, S. Disaster Risk Assessment in Educational Hospitals of Qazvin Based on WHO Pattern in 2015. Electron. Physician 2016, 8, 1770–1775. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rebmann, T. Assessing hospital emergency management plans: A guide for infection preventionists. Am. J. Infect. Control 2009, 37, 708–735. [Google Scholar] [CrossRef] [PubMed]
- Bentley, J.D. Hospital preparedness for bioterrorism. Public Health Rep. 2001, 116 (Suppl. 2), 36–39. [Google Scholar] [CrossRef]
| Search Terms | |||
|---|---|---|---|
| PubMed | Web of Science | Scopus | |
| 1. Set of entry criteria | TS = (hospital preparedness) OR TS = (emergency trauma) | TITLE-ABS-KEY (“bioterrorism prevention”) OR TITLE-ABS-KEY (“bioterrorism control”) OR TITLE-ABS-KEY (biological) | |
| 2. Set of entry criteria | TS = (“bioterrorism”) OR TS = (terrorism, biological) OR TS = (biological terrorism) | TITLE-ABS-KEY (hospital) OR TITLE-ABS-KEY (“emergency trauma”) OR | |
| 3. Set of entry criteria | TS = (emergency) OR TS = (emergency preparedness) OR TS = (disaster planning) | TITLE-ABS-KEY (disaster planning) OR TITLE-ABS-KEY (disaster preparedness) | |
| Final search | (“bioterrorism/prevention and control” [Mesh]) OR (“bioterrorism/organization and administration” [Mesh]) AND/OR (“emergency service, hospital/organization and administration” [Mesh]) OR (“trauma centers/organization and administration” [Mesh]) | 1 AND 2 AND 3 | 1 AND 2 OR 3 |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| 1. Study the hospital’s ability to respond to bioterrorism incidents by investigating or constructing indicators; including a review of events that have occurred and work processes. | 1. The research direction consists of biological warfare agents, pathogens, etc., that are not related to management. |
| 2. The content involves prevention and response methods, tools, and legislation related to bioterrorism, which are not focused on hospitals. | |
| 3. The content focuses on the quality and delivery of medical staff surveys, education, and training. | |
| 2. Any type of studies (observational, cross-sectional, longitudinal). | 4. Reviews, letters, communications, notes, editorials, and conference reports. |
| 5. Abstract missing; full text not found. | |
| 3. Studies published in English. | 6. Not published in English. |
| 4. Studies published from 2012 to 2022. | 7. Studies published before January 2012 or after September 2022. |
| No. | Title | Academic Journal | Publication Date | Regional Study |
|---|---|---|---|---|
| 1 | Evidence-based support for the all-hazards approach to emergency preparedness | Israel Journal of Health Policy Research | 25 October 2012 | Israel |
| 2 | Construction of evaluation systems for the ability to respond to bioterrorism in military hospitals | Military Medical Sciences | 25 October 2012 | China |
| 3 | Suggestions about the ability to respond to bioterrorism in military hospitals | Military Medical Sciences | 25 February 2014 | China |
| 4 | Hospital disaster preparedness in Switzerland | Swiss Medical Weekly | 2 October 2014 | Switzerland |
| 5 | Evaluation and Analysis of Hospital Disaster Preparedness in Jeddah | Scientific Research | 10 November 2014 | Saudi Arabia |
| 6 | A Comprehensive Evaluation System for Military Hospitals’ Response Capability to Bioterrorism | Cell Biochemistry and Biophysics | 22 January 2015 | China |
| 7 | Hospital Disaster Preparedness in Italy: a preliminary study utilizing the World Health Organization Hospital Emergency Response Evaluation Toolkit. | Minerva Anestesiologica | 7 June 2016 | Italy |
| 8 | Evaluation of Hospitals’ Disaster Preparedness Plans in the Holy City of Makkah (Mecca): A Cross-Sectional Observation Study | Prehospital and Disaster Medicine | 22 June 2016 | Saudi Arabia |
| 9 | Are Dutch Hospitals Prepared for Chemical, Biological or Radio Nuclear Incidents? A Survey Study | Prehospital and Disaster Medicine | 9 December 2016 | Netherlands |
| 10 | Survey of Biological Incidents Preparedness of Hospitals in Markazi Province in 2016 | Journal of Military Medicine | 24 June 2017 | Iran |
| 11 | How is training hospitals of Qazvin preparedness against disaster in 2015 | Annals of Tropical Medicine and Parasitology | September 2017 | Iran |
| 12 | A Study of Hospital Disaster Preparedness in South Yemen | Prehospital and Disaster Medicine | April 2018 | Yemen |
| 13 | Hospital management preparedness tools in biological events: A scoping review | Journal of Education and Health Promotion | 29 September 2019 | Iran |
| 14 | Evaluation of hospital disaster preparedness by a multi-criteria decision-making approach: The case of Turkish hospitals | International Journal of Disaster Risk Reduction | 22 June 2020 | Turkey |
| 15 | Factors affecting hospital response in biological disasters: A qualitative study | Medical Journal of the Islamic Republic of Iran | 16 March 2020 | Iran |
| 16 | Hospital Preparedness Challenges in Biological Disasters: A Qualitative Study | Disaster Medicine and Public Health Preparedness | 5 November 2020 | Iran |
| 17 | Assessing the preparedness of hospitals facing disasters using the rough set theory: guidelines for more preparedness to cope with the COVID-19 | International Journal of Systems Science: Operations&Logistics | 24 March 2021 | Iran |
| 18 | Hospital Disaster Preparedness in Iranian Province: A Cross-sectional Study Using A Standard Tool | American Journal of Disaster Medicine | 6 April 2021 | Iran |
| 19 | Disaster preparedness in emergency medical service agencies: A systematic review | Journal of Education and Health Promotion | 30 July 2021 | Iran |
| 20 | COSMIN Checklist for Systematic Reviews of the Hospital Preparedness Instruments in Biological Events | Journal of Nursing Measurement | 1 December 2021 | Iran |
| 21 | Investigating the level of functional preparedness of selected Tehran hospitals in the face of biological events: a focus on COVID-19 | International Journal of Disaster Resilience in the Built Environment | 10 January 2022 | Iran |
| 22 | Chemical, Biological, Radiological, or Nuclear Response in Queensland Emergency Services: A Multisite Study | Health Security | 24 May 2022 | Australia |
| 23 | Establishing the Domains of a Hospital Disaster Preparedness Evaluation Tool: A Systematic Review | Prehospital and Disaster Medicine | 17 July 2022 | China |
| Main Subcategories | Contains Subcategories |
|---|---|
| Emergency management | organizational management 2,3,16, command and coordination 2,6,7,12,18,22, training and education 1,2,3,6,7,8,12,13,14,15,16,19,22, plan 4,5,8,9,11,12,13,19,22, communication systems 5,7,8,12,13,14,15,16,19,21, information management 14,17, lock down the facility 6, transport 23, vehicles 2,5,14,19, safety and security 7,12,18,23 |
| Medical service capacity | prehospital first aid (prehospital team) 2,3,6, electronic medical records 22, patient management 16,22, triage 7,12,15,16,18, on-site disposal 2,3,6, personal protective equipment (PPE) 3,8,9,13,16,19, monitoring and warning 2,6,12,13,15,19, decontamination 2,8,9,13,15,16,19,20,22, body storage/disposal 8,23, morgue facilities 23, anti-infective therapy and vaccines 15,19,23, standard operating procedure (SOP) 1,13,19, isolation 6,9,15, treatment and infection control 15, continuity of essential services 12,18 |
| Surge capacity | material supply 6,14,19, infrastructure and equipment 1,2,3,5,6,11,13,14,17,19, stockpiling 23, pharmaceuticals (antidotes 9, vaccines 10) 11,14,17,22, human resource 4,5,7,12,13,14,18,19, staff support policies 13,15,16,22,23, surge bed capacity 4,7,12,14,17,18,21,22, psychological counselling 19, additional staff 4,13,23, surge discharge plan 8 |
| Laboratory | scientific research 2,6,17, surveillance system 12,15,16 |
| Regional coordination | integration with local or regional systems 5,13,22, inter-organizational coordination 15,19, cooperative plan3, health facility networking 5, referral procedure 5, infectious disease control centers 15 |
| Logistical support | Funding 2,6,7,12,14,15,19, legal 19, architecture and furnishings 5,13,15,16, safety of Lifeline Facilities (water 14, electricity 23) 5,7,13,14, location and areas 5,14, emergency supply kit 3,17, waste management 16, post-disaster recovery 7,12,18,21, logistics and management supply 7,12,18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yao, L.; Zhang, Y.; Zhao, C.; Zhao, F.; Bai, S. The PRISMA 2020 Statement: A System Review of Hospital Preparedness for Bioterrorism Events. Int. J. Environ. Res. Public Health 2022, 19, 16257. https://doi.org/10.3390/ijerph192316257
Yao L, Zhang Y, Zhao C, Zhao F, Bai S. The PRISMA 2020 Statement: A System Review of Hospital Preparedness for Bioterrorism Events. International Journal of Environmental Research and Public Health. 2022; 19(23):16257. https://doi.org/10.3390/ijerph192316257
Chicago/Turabian StyleYao, Lulu, Yongzhong Zhang, Chao Zhao, Feida Zhao, and Song Bai. 2022. "The PRISMA 2020 Statement: A System Review of Hospital Preparedness for Bioterrorism Events" International Journal of Environmental Research and Public Health 19, no. 23: 16257. https://doi.org/10.3390/ijerph192316257
APA StyleYao, L., Zhang, Y., Zhao, C., Zhao, F., & Bai, S. (2022). The PRISMA 2020 Statement: A System Review of Hospital Preparedness for Bioterrorism Events. International Journal of Environmental Research and Public Health, 19(23), 16257. https://doi.org/10.3390/ijerph192316257





