What Works to Improve Wellbeing? A Rapid Systematic Review of 223 Interventions Evaluated with the Warwick-Edinburgh Mental Well-Being Scales
Abstract
1. Introduction
- What WEMWBS-based evaluation research has been carried out to assess the effectiveness of programmes and pilots on mental wellbeing?
- What are the key findings from the evaluation research?
- What is the strength of evidence of the evaluation research?
2. Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection
2.4. Critical Appraisal
2.5. Data Extraction
2.6. Synthesis
3. Results
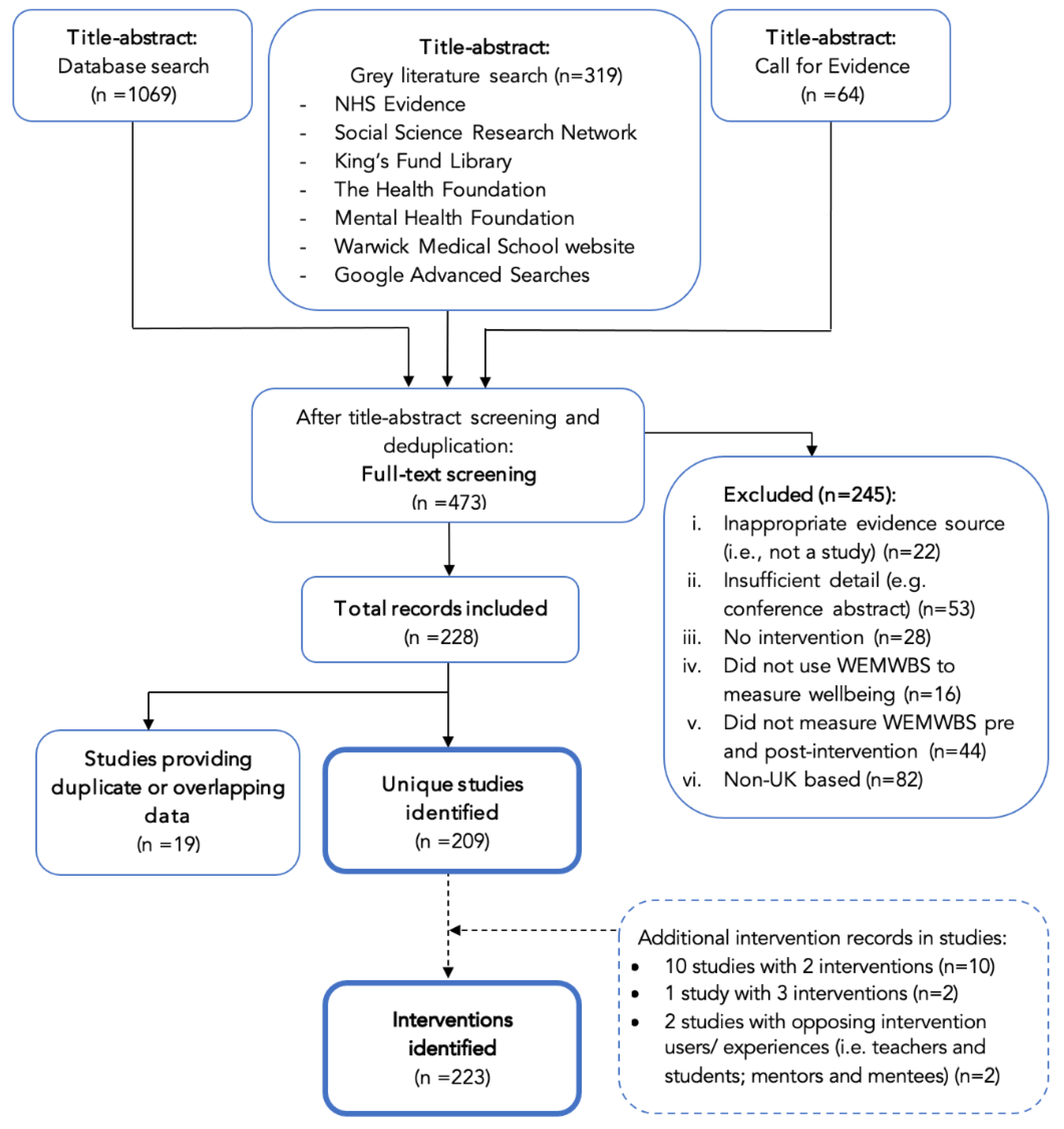
3.1. Search Results
3.2. Study Characteristics
3.3. Key Findings by Theme
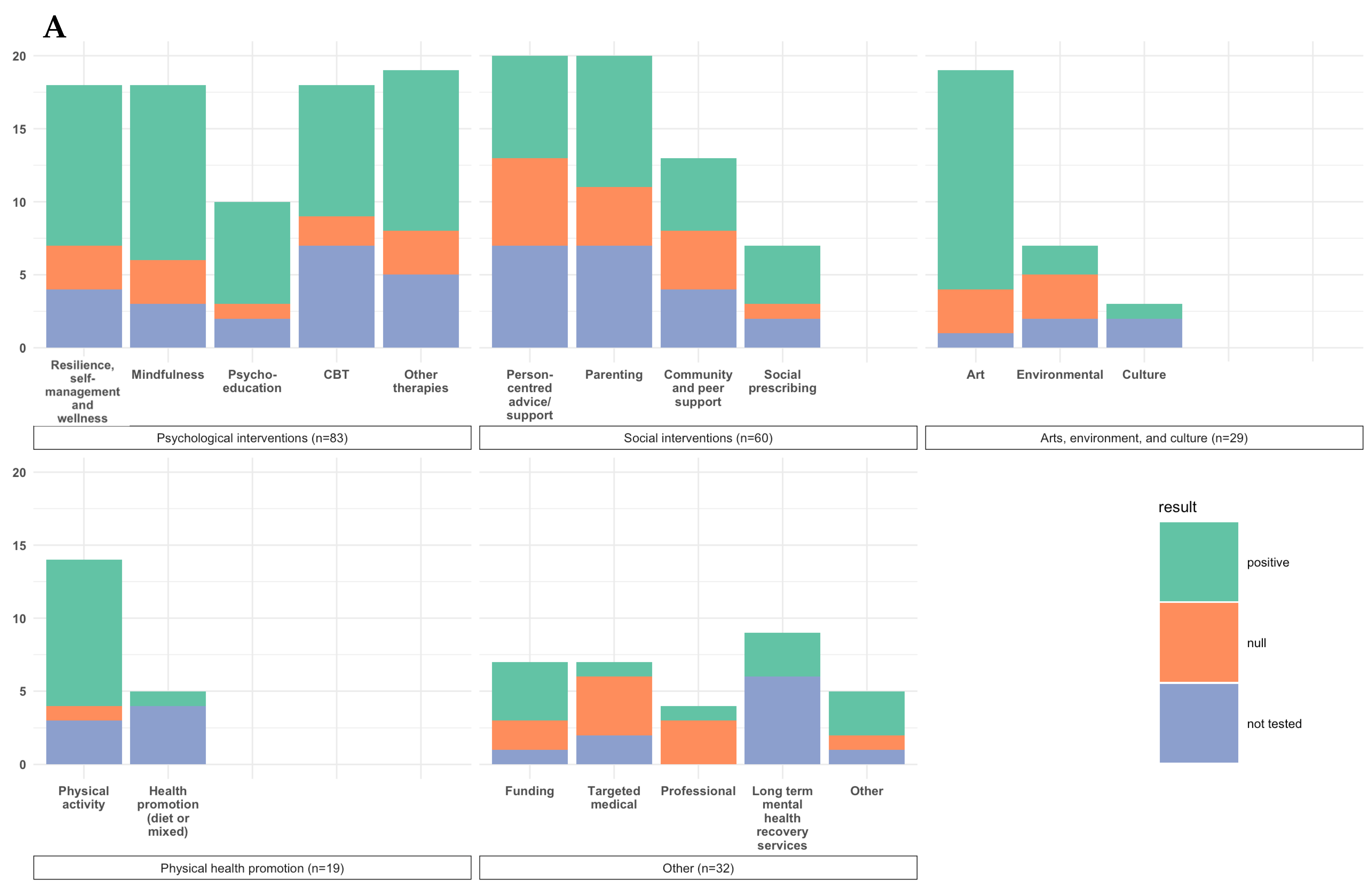
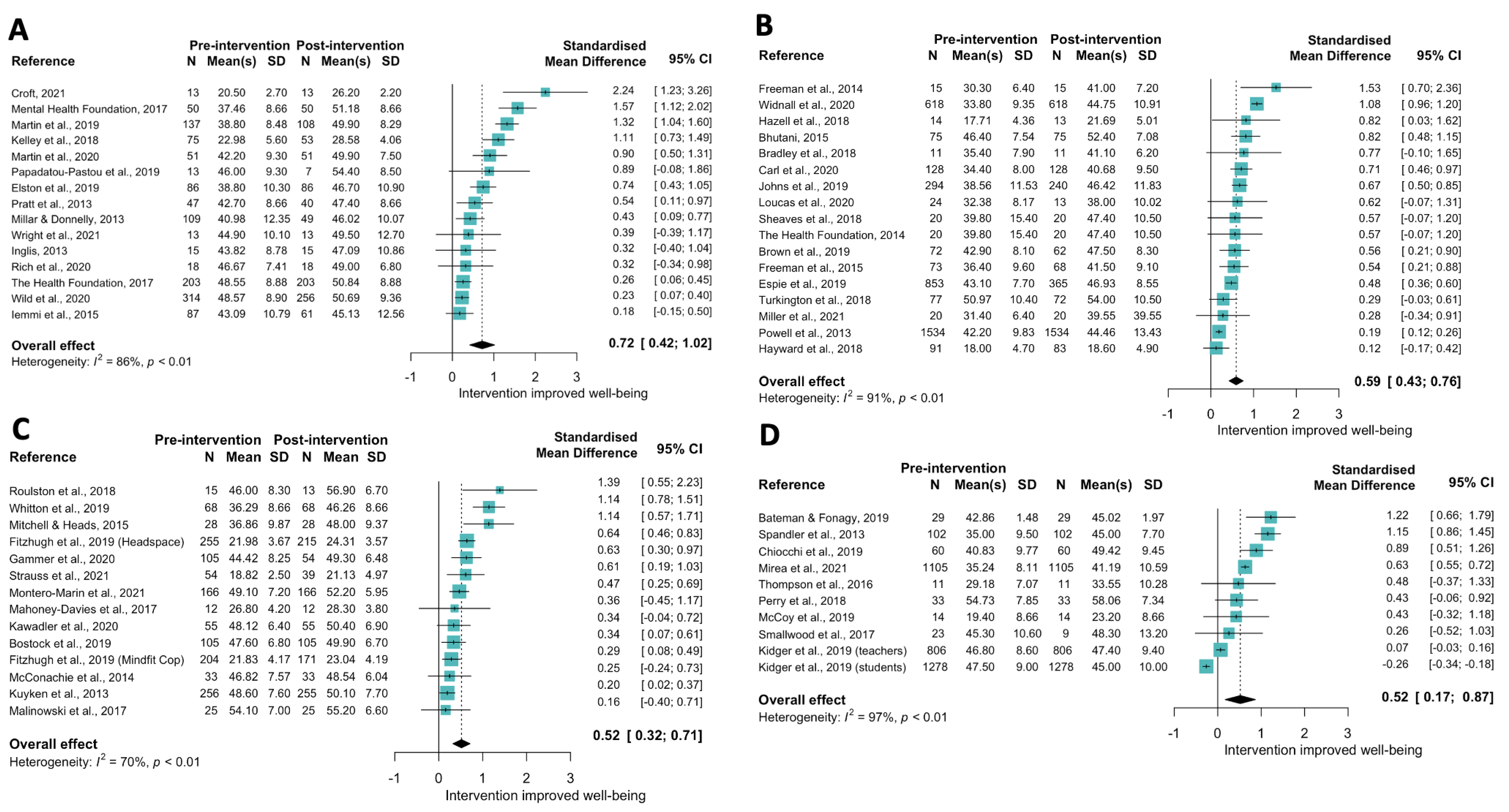
3.3.1. Theme 1: Psychological (n = 80)
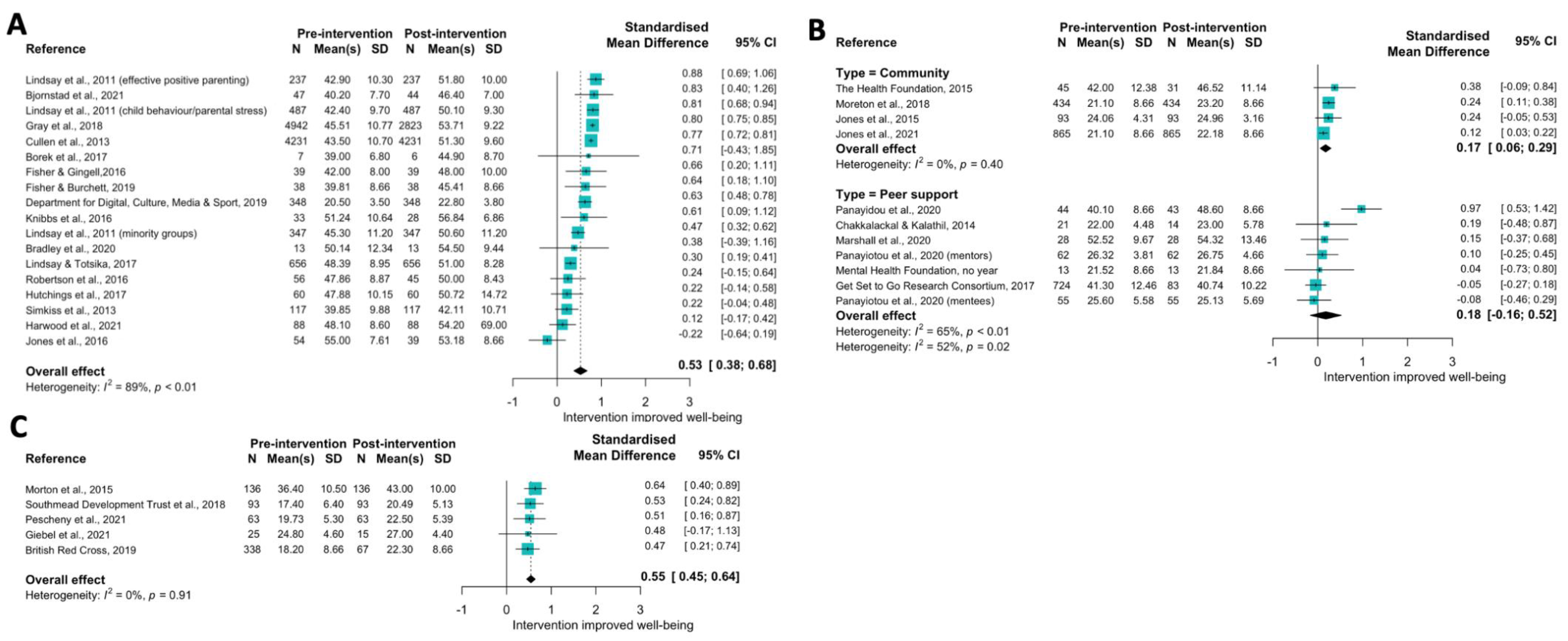
3.3.2. Theme 2: Social (n = 54)
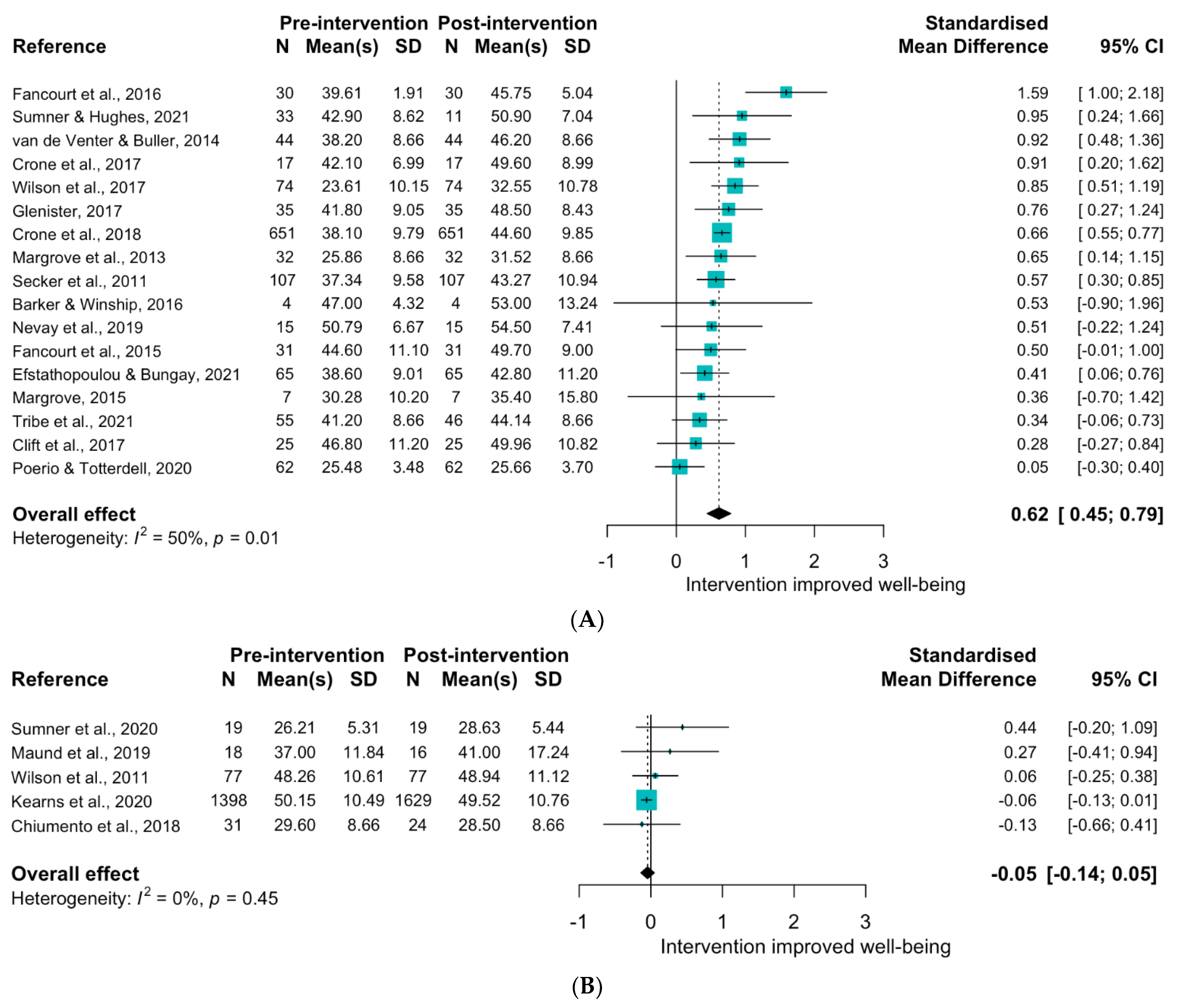
3.3.3. Theme 3: Arts, Environment and Culture (n = 29)
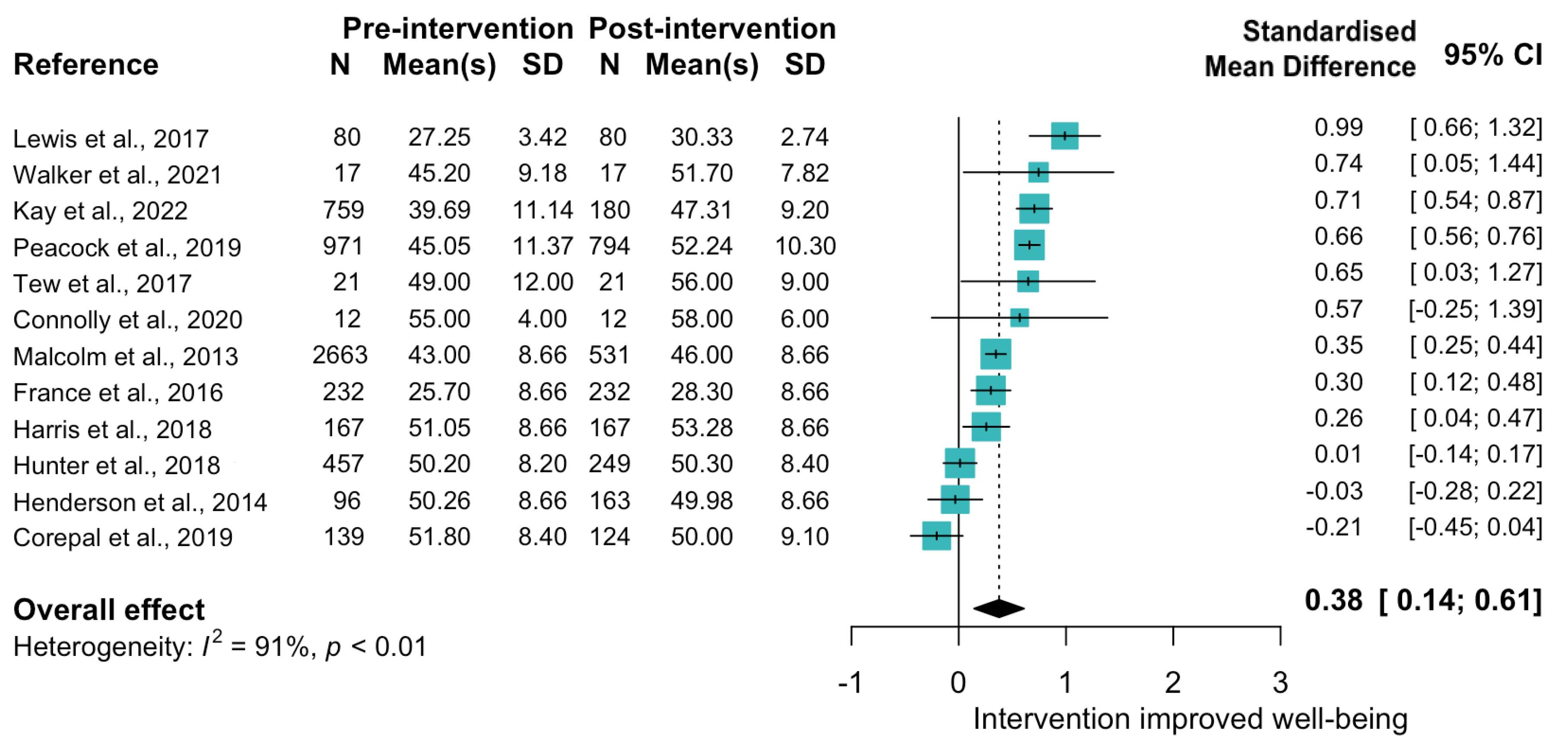
3.3.4. Theme 4: Physical Health Promotion (n = 18)
3.3.5. Theme 5 Other (n = 28)
3.4. Critical Appraisal
4. Discussion
4.1. Key Findings
4.2. Comparison to Other Reviews
4.3. Sources and Explanations of Heterogeneity
4.4. Implications for Research and Policy
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- van Agteren, J.; Iasiello, M.; Lo, L.; Bartholomaeus, J.; Kopsaftis, Z.; Carey, M.; Kyrios, M. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat. Hum. Behav. 2021, 5, 631–652. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh mental well-being scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Warwick Medical School. the Warwick-Edinburgh Mental Wellbeing Scales—WEMWBS. Available online: https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs/ (accessed on 15 November 2021).
- Stewart-Brown, S.; Platt, S.; Tennant, A.; Maheswaran, H.; Parkinson, J.; Weich, S.; Taggart, F.; Clarke, A. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): A valid and reliable tool for measuring mental well-being in diverse populations and projects. J. Epidemiol. Community Health 2011, 65 (Suppl. 2), A38–A39. [Google Scholar] [CrossRef]
- Clarke, A.; Friede, T.; Putz, R.; Ashdown, J.; Martin, S.; Blake, A.; Adi, Y.; Parkinson, J.; Flynn, P.; Platt, S.; et al. Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health 2011, 11, 487. [Google Scholar] [CrossRef] [PubMed]
- Koushede, V.; Lasgaard, M.; Hinrichsen, C.; Meilstrup, C.; Nielsen, L.; Rayce, S.B.; Torres-Sahli, M.; Gudmundsdottir, D.G.; Stewart-Brown, S.; Santini, Z.I. Measuring mental well-being in Denmark: Validation of the original and short version of the Warwick-Edinburgh mental well-being scale (WEMWBS and SWEMWBS) and cross-cultural comparison across four European settings. Psychiatry Res. 2018, 271, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Shah, N.; Steiner, D.; Petrou, S.; Johnson, R.; Stewart Brown, S. Exploring the impact of the Warwick-Edinburgh Mental Well-being scales on public health research and practice. Health Serv. Res. Policy, 2018, in press.
- Everett, G. Measuring National Well-Being: A UK Perspective. Rev. Income Wealth 2015, 61, 34–42. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Trudel-Fitzgerald, C.; Allin, P.; Farrelly, C.; Fletcher, G.; Frederick, D.E.; Hall, J.; Helliwell, J.F.; Kim, E.S.; Lauinger, W.A.; et al. Current recommendations on the selection of measures for well-being. Prev. Med. 2020, 133, 106004. [Google Scholar] [CrossRef] [PubMed]
- Linton, M.-J.; Dieppe, P.; Medina-Lara, A. Review of 99 self-report measures for assessing well-being in adults: Exploring dimensions of well-being and developments over time. BMJ Open 2016, 6, e010641. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Garritty, C.; Gartlehner, G.; Nussbaumer-Streit, B.; King, V.J.; Hamel, C.; Kamel, C.; Affengruber, L.; Stevens, A. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J. Clin. Epidemiol. 2020, 130, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Warwick Medical School. Examples of Research Using WEMWBS. Available online: https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs/research/research/ (accessed on 15 November 2021).
- Snape, D.; Meads, C.; Bagnall, A.; Tregaskis, O.; Mansfield, L. What Works Wellbeing: A Guide to Our Evidence Review Methods; What Works Centre for Wellbeing: London, UK, 2019. [Google Scholar]
- Solutions for Public Health. Rapid Evidence Assessment of Wellbeing Impact Evaluations Using ONS4 Personal Wellbeing Measures; What Works Centre for Wellbeing: London, UK, 2020. [Google Scholar]
- Rohatgi, A. WebPlotDigitalizer: HTML5 Based Online Tool to Extract Numerical Data from Plot Images, Version 4.3. 2020. Available online: http://arohatgi.info/WebPlotDigitizer/app/ (accessed on 15 January 2022).
- Popay, J.; Roberts, H.; Sowden, A.; Petticrew, M.; Arai, L.; Rodgers, M.; Britten, N.; Roen, K.; Duffy, S. Guidance on the conduct of narrative synthesis in systematic reviews. A Prod. ESRC Methods Programme Version 2006, 1, b92. [Google Scholar]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Brydges, C.R. Effect size guidelines, sample size calculations, and statistical power in gerontology. Innov. Aging 2019, 3, igz036. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.J.; Butcher, I.; Assi, V.; Lewis, S.C.; Murray, G.D.; Langhorne, P.; Brady, M.C. Dealing with missing standard deviation and mean values in meta-analysis of continuous outcomes: A systematic review. BMC Med. Res. Methodol. 2018, 18, 25. [Google Scholar] [CrossRef] [PubMed]
- Croft, G. Reconnect to Innate Resilience. 2021. Available online: https://us.simplerousercontent.net/uploads/asset/file/5486471/Reconnect-to-Resilience-Report-May-2021.pdf (accessed on 31 May 2021).
- Elston, J.; Gradinger, F.; Asthana, S.; Lilley-Woolnough, C.; Wroe, S.; Harman, H.; Byng, R. Does a social prescribing ‘holistic’ link-worker for older people with complex, multimorbidity improve well-being and frailty and reduce health and social care use and costs? A 12-month before-and-after evaluation. Prim. Health Care Res. Dev. 2019, 20, e135. [Google Scholar] [CrossRef] [PubMed]
- Iemmi, V.; Crepaz-Keay, D.; Cyhlarova, E.; Knapp, M. Peer-led self-management for people with severe mental disorders: An economic evaluation. J. Ment. Health Train. Educ. Pract. 2015, 10, 14–25. [Google Scholar] [CrossRef]
- Inglis, J. Social Assets in Action Evaluation Report. 2013. Available online: https://www.iriss.org.uk/sites/default/files/social-assets-in-action-evaluation-report.pdf (accessed on 16 October 2022).
- Kelley, T.M.; Hollows, J.; Lambert, E.G.; Savard, D.M.; Pransky, J. Teaching health versus treating illness: The efficacy of three principles correctional counseling with people in an English prison. Int. J. Offender Ther. Comp. Criminol. 2018, 62, 2831–2856. [Google Scholar] [CrossRef] [PubMed]
- Martin, F.; Clyne, W.; Pearce, G.; Turner, A. Self-Management Support Intervention for Parents of Children with Developmental Disorders: The Role of Gratitude and Hope. J. Child Fam. Stud. 2019, 28, 980–992. [Google Scholar] [CrossRef]
- Martin, F.; Wright, H.; Moody, L.; Whiteman, B.; McGillion, M.; Clyne, W.; Pearce, G.; Turner, A. Help to Overcome Problems Effectively for Cancer Survivors: Development and Evaluation of a Digital Self-Management Program. J. Med Internet Res. 2020, 22, e17824. [Google Scholar] [CrossRef] [PubMed]
- Mental Health Foundation. Parc Prison. An Evaluation of Peer-Led Self-Management Training within A Prison Setting; Mental Health Foundation: Wales, UK, 2017. [Google Scholar]
- Millar, S.L.; Donnelly, M. Promoting mental wellbeing: Developing a theoretically and empirically sound complex intervention. J. Public Health 2013, 36, 275–284. [Google Scholar] [CrossRef] [PubMed]
- Mind Cymru, Age Cymru. Our work in Wales: My Generation. Improving the Mental Resilience and Wellbeing of People over 50 Years Old in Wales. Cardiff. 2018. Available online: https://www.mind.org.uk/media-a/4355/my-generation-report_-english.pdf (accessed on 16 October 2022).
- Papadatou-Pastou, M.; Campbell-Thompson, L.; Barley, E.; Haddad, M.; Lafarge, C.; McKeown, E.; Simeonov, L.; Tzotzoli, P. Exploring the feasibility and acceptability of the contents, design, and functionalities of an online intervention promoting mental health, wellbeing, and study skills in Higher Education students. Int. J. Ment. Health Syst. 2019, 13, 51. [Google Scholar] [CrossRef] [PubMed]
- Pratt, R.; MacGregor, A.; Reid, S.; Given, L. Experience of Wellness Recovery Action Planning in Self-Help and Mutual Support Groups for People with Lived Experience of Mental Health Difficulties. Sci. World J. 2013, 2013, 180587. [Google Scholar] [CrossRef] [PubMed]
- Rich, A.; Aly, A.; Cecchinato, M.E.; Lascau, L.; Baker, M.; Viney, R.; Cox, A.L. Evaluation of a novel intervention to reduce burnout in doctors-in-training using self-care and digital wellbeing strategies: A mixed-methods pilot. BMC Med. Educ. 2020, 20, 294. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.; Hanna, E.; Raine, G.; Robertson, S. Extending the Comfort Zone: Building Resilience in Older People With Long-Term Conditions. J. Appl. Gerontol. 2017, 38, 825–848. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.; Robertson, S.; Steen, M.; Raine, G.; Day, R. Doing and rethinking. Building resilience with men. Ment. Health Rev. J. 2015, 20, 185–198. [Google Scholar] [CrossRef]
- The Health Foundation. Optimising Strength and Resilience: Integrated Physical and Psychological Health Programme for Patients, Families and NHS Staff; The Health Foundation: London, UK, 2017. [Google Scholar]
- Wild, J.; El-Salahi, S.; Degli Esposti, M.; Thew, G.R. Evaluating the effectiveness of a group-based resilience intervention versus psychoeducation for emergency responders in England: A randomised controlled trial. PLoS ONE 2020, 15, e0241704. [Google Scholar] [CrossRef]
- Wright, H.; Martin, F.; Clyne, W.; Clark, C.C.T.; Matouskova, G.; McGillion, M.; Turner, A. A Digital Self-management Program (Help to Overcome Problems Effectively) for People Living With Cancer: Feasibility Randomized Controlled Trial. J. Med Internet Res. 2021, 23, e28322. [Google Scholar] [CrossRef]
- Beshai, S.; McAlpine, L.; Weare, K.; Kuyken, W. A Non-Randomised Feasibility Trial Assessing the Efficacy of a Mindfulness-Based Intervention for Teachers to Reduce Stress and Improve Well-Being. Mindfulness 2015, 7, 198–208. [Google Scholar] [CrossRef]
- Bostock, S.; Crosswell, A.D.; Prather, A.A.; Steptoe, A. Mindfulness on-the-go: Effects of a mindfulness meditation app on work stress and well-being. J. Occup. Health Psychol. 2019, 24, 127–138. [Google Scholar] [CrossRef]
- Fitzhugh, H.; Michaelides, G.; Connolly, S.; Daniels, K. Mindfulness in Policing: A Randomised Controlled Trial of Two Online Mindfulness Resources Across Five Forces in England and Wales; College of Policing: Coventry, UK, 2019. [Google Scholar]
- Flynn, S.; Hastings, R.P.; Burke, C.; Howes, S.; Lunsky, Y.; Weiss, J.A.; Bailey, T. Online Mindfulness Stress Intervention for Family Carers of Children and Adults with Intellectual Disabilities: Feasibility Randomized Controlled Trial. Mindfulness 2020, 11, 2161–2175. [Google Scholar] [CrossRef]
- Gammer, I.; Hartley-Jones, C.; Jones, F.W. A Randomized Controlled Trial of an Online, Compassion-Based Intervention for Maternal Psychological Well-Being in the First Year Postpartum. Mindfulness 2020, 11, 928–939. [Google Scholar] [CrossRef]
- Kawadler, J.M.; Hemmings, N.R.; Ponzo, S.; Morelli, D.; Bird, G.; Plans, D. Effectiveness of a Smartphone App (BioBase) for Reducing Anxiety and Increasing Mental Well-Being: Pilot Feasibility and Acceptability Study. JMIR Form. Res. 2020, 4, e18067. [Google Scholar] [CrossRef] [PubMed]
- Kuyken, W.; Weare, K.; Ukoumunne, O.C.; Vicary, R.; Motton, N.; Burnett, R.; Cullen, C.; Hennelly, S.; Huppert, F. Effectiveness of the Mindfulness in Schools Programme: Non-randomised controlled feasibility study. Br. J. Psychiatry 2013, 203, 126–131. [Google Scholar] [CrossRef]
- Mahoney-Davies, G.; Dixon, C.; Tynan, H.; Mann, S. An evaluation of the effectiveness of a ‘Five Ways to Well-being’ group run with people with learning disabilities. Br. J. Learn. Disabil. 2016, 45, 56–63. [Google Scholar] [CrossRef]
- Malinowski, P.; Moore, A.W.; Mead, B.R.; Gruber, T. Mindful Aging: The Effects of Regular Brief Mindfulness Practice on Electrophysiological Markers of Cognitive and Affective Processing in Older Adults. Mindfulness 2015, 8, 78–94. [Google Scholar] [CrossRef]
- McConachie, D.A.J.; McKenzie, K.; Morris, P.; Walley, R.M. Acceptance and mindfulness-based stress management for support staff caring for individuals with intellectual disabilities. Res. Dev. Disabil. 2014, 35, 1216–1227. [Google Scholar] [CrossRef]
- Millar, A.; Tip, L.; Lennon, R.; Macinnes, M.; Michalska, B.; Lawrie, S.M.; Schwannauer, M. The introduction of mindfulness groups to a psychiatric rehabilitation in-patient setting: A feasibility study. BMC Psychiatry 2020, 20, 322. [Google Scholar] [CrossRef]
- Mitchell, M.; Heads, G. Staying Well: A Follow Up of a 5-Week Mindfulness Based Stress Reduction Programme for a Range of Psychological Issues. Community Ment. Health J. 2015, 51, 897–902. [Google Scholar] [CrossRef]
- Montero-Marin, J.; Taylor, L.; Crane, C.; Greenberg, M.T.; Ford, T.J.; Williams, J.M.G.; García-Campayo, J.; Sonley, A.; Lord, L.; Dalgleish, T.; et al. Teachers “finding peace in a frantic world”: An experimental study of self-taught and instructor-led mindfulness program formats on acceptability, effectiveness, and mechanisms. J. Educ. Psychol. 2021, 113, 1689. [Google Scholar] [CrossRef]
- Roulston, A.; Montgomery, L.; Campbell, A.; Davidson, G. Exploring the impact of mindfulnesss on mental wellbeing, stress and resilience of undergraduate social work students. Soc. Work Educ. 2017, 37, 157–172. [Google Scholar] [CrossRef]
- Strauss, C.; Dunkeld, C.; Cavanagh, K. Is clinician-supported use of a mindfulness smartphone app a feasible treatment for depression? A mixed-methods feasibility study. Internet Interv. 2021, 25, 100413. [Google Scholar] [CrossRef] [PubMed]
- Whitton, T.; Buchanan, G.; Smith, S. How a mindfulness intervention can improve patients’ mental wellbeing. Nurs. Times 2019, 115, 48–51. [Google Scholar]
- Bateman, A.; Fonagy, P. A randomized controlled trial of a mentalization-based intervention (MBT-FACTS) for families of people with borderline personality disorder. Pers. Disord. Theory, Res. Treat. 2019, 10, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Chiocchi, J.; Lamph, G.; Slevin, P.; Fisher-Smith, D.; Sampson, M. Can a carer (peer) led psychoeducation programme improve mental health carers well-being, reduce burden and enrich empowerment: A service evaluation study. J. Ment. Health Train. Educ. Pract. 2019, 14, 131–140. [Google Scholar] [CrossRef]
- Kidger, J.; Turner, N.; Hollingworth, W.; Evans, R.; Bell, S.; Brockman, R.; Copeland, L.; Fisher, H.; Harding, S.; Powell, J.; et al. An intervention to improve teacher well-being support and training to support students in UK high schools (the WISE study): A cluster randomised controlled trial. PLOS Med. 2021, 18, e1003847. [Google Scholar] [CrossRef] [PubMed]
- McCoy, E.; Harrison, R.; Butler, N.; Kinsella, K.; Oyston, J.; Timpson, H.; Quigg, Z. Evaluation of the Rock Pool Adverse Childhood Experiences (ACEs) Recovery Toolkit Programme; Liverpool John Moores University Public Health Institute: Liverpool, UK, 2019. [Google Scholar]
- Mirea, D.-M.; A Martin-Key, N.; Barton-Owen, G.; Olmert, T.; Cooper, J.D.; Han, S.Y.S.; Farrag, L.P.; Bell, E.; Friend, L.V.; Eljasz, P.; et al. Impact of a Web-Based Psychiatric Assessment on the Mental Health and Well-Being of Individuals Presenting With Depressive Symptoms: Longitudinal Observational Study. JMIR Ment. Health 2021, 8, e23813. [Google Scholar] [CrossRef]
- Perry, A.; Gardener, C.; Dove, J.; Eiger, Y.; Loewenthal, K. Improving mental health knowledge of the Charedi Orthodox Jewish Community in North London: A partnership project. Int. J. Soc. Psychiatry 2018, 64, 235–247. [Google Scholar] [CrossRef] [PubMed]
- Smallwood, J.; Jolley, S.; Makhijani, J.; Grice, S.; O’Donoghue, E.; Bendon, P.; Greenaway, L.P.; Onwumere, J. Implementing specialist psychological support for caregivers in psychosis services: A preliminary report. Psychosis 2016, 9, 119–128. [Google Scholar] [CrossRef]
- Spandler, H.; McKeown, M.; Roy, A.; Hurley, M. Football metaphor and mental well-being: An evaluation of the It’s a Goal! programme. J. Ment. Health 2013, 22, 544–554. [Google Scholar] [CrossRef]
- Thompson, C.; Fern ez de la Cruz, L.; Mataix-Cols, D.; Onwumere, J. Development of a brief psychoeducational group intervention for carers of people with hoarding disorder: A proof-of-concept study. J. Obs.-Compuls. Relat. Disord. 2016, 9, 66–72. [Google Scholar] [CrossRef]
- Bhutani, G.E. Looking After Me Looking After You: Using positive cognitive behavioural techniques to improve emotional well-being. Cogn. Behav. Ther. 2015, 8, 13. [Google Scholar] [CrossRef]
- Bradley, J.; Freeman, D.; Chadwick, E.; Harvey, A.G.; Mullins, B.; Johns, L.; Sheaves, B.; Lennox, B.; Broome, M.; Waite, F. Treating Sleep Problems in Young People at Ultra-High Risk of Psychosis: A Feasibility Case Series. Behav. Cogn. Psychother. 2017, 46, 276–291. [Google Scholar] [CrossRef]
- Brown, J.S.; Blackshaw, E.; Stahl, D.; Fennelly, L.; McKeague, L.; Sclare, I.; Michelson, D. School-based early intervention for anxiety and depression in older adolescents: A feasibility randomised controlled trial of a self-referral stress management workshop programme (“DISCOVER”). J. Adolesc. 2019, 71, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Carl, J.R.; Miller, C.B.; Henry, A.L.; Davis, M.L.; Stott, R.; Smits, J.A.J.; Emsley, R.; Gu, J.; Shin, O.; Otto, M.W.; et al. Efficacy of digital cognitive behavioral therapy for moderate-to-severe symptoms of generalized anxiety disorder: A randomized controlled trial. Depress. Anxiety 2020, 37, 1168–1178. [Google Scholar] [CrossRef]
- Espie, C.A.; Emsley, R.; Kyle, S.; Gordon, C.; Drake, C.; Siriwardena, A.N.; Cape, J.; Ong, J.C.; Sheaves, B.; Foster, R.; et al. Effect of Digital Cognitive Behavioral Therapy for Insomnia on Health, Psychological Well-being, and Sleep-Related Quality of Life: A Randomized Clinical Trial. JAMA Psychiatry 2019, 76, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Dunn, G.; Startup, H.; Pugh, K.; Cordwell, J.; Mander, H.; Cernis, E.; Wingham, G.; Shirvell, K.; Kingdon, D. Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT): A parallel, single-blind, randomised controlled trial with a mediation analysis. Lancet Psychiatry 2015, 2, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Pugh, K.; Dunn, G.; Evans, N.; Sheaves, B.; Waite, F.; Černis, E.; Lister, R.; Fowler, D. An early Phase II randomised controlled trial testing the effect on persecutory delusions of using CBT to reduce negative cognitions about the self: The potential benefits of enhancing self confidence. Schizophr. Res. 2014, 160, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Hayward, M.; Edgecumbe, R.; Jones, A.-M.; Berry, C.; Strauss, C. Brief Coping Strategy Enhancement for Distressing Voices: An Evaluation in Routine Clinical Practice. Behav. Cogn. Psychother. 2017, 46, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Hazell, C.M.; Hayward, M.; Cavanagh, K.; Jones, A.-M.; Strauss, C. Guided self-help cognitive-behaviour Intervention for VoicEs (GiVE): Results from a pilot randomised controlled trial in a transdiagnostic sample. Schizophr. Res. 2018, 195, 441–447. [Google Scholar] [CrossRef]
- Johns, L.; Jolley, S.; Garety, P.; Khondoker, M.; Fornells-Ambrojo, M.; Onwumere, J.; Peters, E.; Milosh, C.; Brabban, A.; Byrne, M. Improving Access to psychological therapies for people with severe mental illness (IAPT-SMI): Lessons from the South London and Maudsley psychosis demonstration site. Behav. Res. Ther. 2019, 116, 104–110. [Google Scholar] [CrossRef]
- Loucas, C.E.; Sclare, I.; Stahl, D.; Michelson, D. Feasibility randomized controlled trial of a one-day CBT workshop (‘DISCOVER’) for 15- to 18-year-olds with anxiety and/or depression in clinic settings. Behav. Cogn. Psychother. 2019, 48, 142–159. [Google Scholar] [CrossRef] [PubMed]
- Miller, C.B.; Gu, J.; Henry, A.L.; Davis, M.L.; Espie, C.A.; Stott, R.; Heinz, A.J.; Bentley, K.H.; Goodwin, G.M.; Gorman, B.S.; et al. Feasibility and efficacy of a digital CBT intervention for symptoms of Generalized Anxiety Disorder: A randomized multiple-baseline study. J. Behav. Ther. Exp. Psychiatry 2020, 70, 101609. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.; Hamborg, T.; Stallard, N.; Burls, A.; McSorley, J.; Bennett, K.; Griffiths, K.M.; Christensen, H. Effectiveness of a Web-Based Cognitive-Behavioral Tool to Improve Mental Well-Being in the General Population: Randomized Controlled Trial. J. Med. Internet Res. 2012, 15, e2. [Google Scholar] [CrossRef]
- Powell, J.; Williams, V.; Atherton, H.; Bennett, K.; Yang, Y.; Davoudianfar, M.; Hellsing, A.; Martin, A.; Mollison, J.; Shanyinde, M.; et al. Effectiveness and cost-effectiveness of a self-guided internet intervention for social anxiety symptoms in a general population sample: Randomized controlled trial. J. Med. Internet Res. 2020, 22, e16804. [Google Scholar] [CrossRef] [PubMed]
- Sheaves, B.; Freeman, D.; Isham, L.; McInerney, J.; Nickless, A.; Yu, L.-M.; Rek, S.; Bradley, J.; Reeve, S.; Attard, C.; et al. Stabilising sleep for patients admitted at acute crisis to a psychiatric hospital (OWLS): An assessor-blind pilot randomised controlled trial. Psychol. Med. 2017, 48, 1694–1704. [Google Scholar] [CrossRef]
- The Health Foundation. Stabilising Sleep for Patients Admitted at Acute Crisis to Psychiatric Hospital: A Pilot Ranomised Controlled Trial; The Health Foundation: London, UK, 2016. [Google Scholar]
- Turkington, D.; Gega, L.; Lebert, L.; Douglas-Bailey, M.; Rustom, N.; Alberti, M.; Deighton, S.; Naeem, F. A training model for relatives and friends in cognitive behaviour therapy (CBT) informed care for psychosis. Cogent Psychol. 2018, 5, 1497749. [Google Scholar] [CrossRef]
- Widnall, E.; Price, A.; Trompetter, H.; Dunn, B.D. Routine Cognitive Behavioural Therapy for Anxiety and Depression is More Effective at Repairing Symptoms of Psychopathology than Enhancing Wellbeing. Cogn. Ther. Res. 2019, 44, 28–39. [Google Scholar] [CrossRef]
- Allward, C.; Dunn, R.; Forshaw, G.; Rewston, C.; Wass, N. Mental wellbeing in people with dementia following Cognitive Stimulation Therapy: Innovative practice. Dementia 2017, 19, 496–504. [Google Scholar] [CrossRef]
- Bacon, T.; Doughty, C.; Summers, A.; Wiffen, B.; Stanley, Z.; McAlpine, S. The Emotional Resources Group: Provisional outcome data for a pilot six-session emotion regulation programme for secondary care. Br. J. Clin. Psychol. 2018, 57, 223–239. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.; Hooper, N.; James, P.; Scott, D.; Bodger, O.; John, A. A Web-Delivered Acceptance and Commitment Therapy Intervention With Email Reminders to Enhance Subjective Well-Being and Encourage Engagement With Lifestyle Behavior Change in Health Care Staff: Randomized Cluster Feasibility Stud. JMIR Form. Res. 2020, 4, e18586. [Google Scholar] [CrossRef] [PubMed]
- Cheshire, A.; Peters, D.; Ridge, D. How do we improve men’s mental health via primary care? An evaluation of the Atlas Men’s Well-being Pilot Programme for stressed/distressed men. BMC Fam. Pract. 2016, 17, 13. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Collins, J.; Gibson, A.; Parkin, S.; Parkinson, R.; Shave, D.; Dyer, C. Counselling in the workplace: How time-limited counselling can effect change in well-being. Couns. Psychother. Res. 2012, 12, 84–92. [Google Scholar] [CrossRef]
- Dunn, B.D.; Widnall, E.; Reed, N.; Owens, C.; Campbell, J.; Kuyken, W. Bringing light into darkness: A multiple baseline mixed methods case series evaluation of Augmented Depression Therapy (ADepT). Behav. Res. Ther. 2019, 120, 103418. [Google Scholar] [CrossRef]
- Durcan, G. Restoring something lost. In The Mental Health Impact of Therapy Dogs in Prison; Centre for Mental Health: London, UK, 2018. [Google Scholar]
- Flaherty-Jones, G.M.; Carne, A.S.; Dexter-Smith, S. The steps to recovery program: Evaluation of a group-based intervention for older individuals receiving mental health services. Psychiatr. Rehabilitation J. 2016, 39, 68–70. [Google Scholar] [CrossRef] [PubMed]
- Grajfoner, D.; Harte, E.; Potter, L.M.; McGuigan, N. The effect of dog-assisted intervention on student well-being, mood, and anxiety. Int. J. Environ. Res. Public Health 2017, 14, 483. [Google Scholar] [CrossRef]
- Hartley, S.E. Service Users’ Perceptions of an Outreach Wellbeing Service: A Social Enterprise for Promoting Mental Health. Community Ment. Health J. 2017, 53, 842–851. [Google Scholar] [CrossRef][Green Version]
- Hemmings, N.R.; Kawadler, J.M.; Whatmough, R.; Ponzo, S.; Rossi, A.; Morelli, D.; Bird, G.; Plans, D. Development and Feasibility of a Digital Acceptance and Commitment Therapy–Based Intervention for Generalized Anxiety Disorder: Pilot Acceptability Study. JMIR Form. Res. 2021, 5, e21737. [Google Scholar] [CrossRef]
- Jolley, S.; Johns, L.C.; O’Donoghue, E.; Oliver, J.; Khondoker, M.; Byrne, M.; Butler, L.; De Rosa, C.; Leal, D.; McGovern, J.; et al. Group acceptance and commitment therapy for patients and caregivers in psychosis services: Feasibility of training and a preliminary randomized controlled evaluation. Br. J. Clin. Psychol. 2020, 59, 524–551. [Google Scholar] [CrossRef]
- Kevern, P.; Hill, L. ‘Chaplains for well-being’ in primary care: Analysis of the results of a retrospective study. Prim. Health Care Res. Dev. 2014, 16, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, G. The efficacy of primary care chaplaincy compared with antidepressants: A retrospective study comparing chaplaincy with antidepressants. Prim. Health Care Res. Dev. 2017, 18, 354–365. [Google Scholar] [CrossRef]
- Majumdar, S.; Morris, R. Brief group-based acceptance and commitment therapy for stroke survivors. Br. J. Clin. Psychol. 2018, 58, 70–90. [Google Scholar] [CrossRef]
- Northcott, S.; Thomas, S.; James, K.; Simpson, A.; Hirani, S.; Barnard, R.; Hilari, K. Solution Focused Brief Therapy in Post-Stroke Aphasia (SOFIA): Feasibility and acceptability results of a feasibility randomised wait-list controlled trial. BMJ Open 2021, 11, e050308. [Google Scholar] [CrossRef] [PubMed]
- Priebe, S.; Kelley, L.; Omer, S.; Golden, E.; Walsh, S.; Khanom, H.; Kingdon, D.; Rutterford, C.; McCrone, P.; McCabe, R. The Effectiveness of a Patient-Centred Assessment with a Solution-Focused Approach (DIALOG+) for Patients with Psychosis: A Pragmatic Cluster-Randomised Controlled Trial in Community Care. Psychother. Psychosom. 2015, 84, 304–313. [Google Scholar] [CrossRef]
- Schrank, B.; Brownell, T.; Jakaite, Z.; Larkin, C.; Pesola, F.; Riches, S.; Tylee, A.; Slade, M. Evaluation of a positive psychotherapy group intervention for people with psychosis: Pilot randomised controlled trial. Epidemiology Psychiatr. Sci. 2015, 25, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Strauss, C.; Lea, L.; Hayward, M.; Forrester, E.; Leeuwerik, T.; Jones, A.-M.; Rosten, C. Mindfulness-based exposure and response prevention for obsessive compulsive disorder: Findings from a pilot randomised controlled trial. J. Anxiety Disord. 2018, 57, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Battrick, T.; Crook, L.; Edwards, K.; Moselle, B. Evaluation of the MEAM Pilots—Update on Our Findings; FTI Consulting: London, UK, 2014. [Google Scholar]
- Beynon, P.; Burdis, G.; Hoadley, J.; Jensen, A.; Beardmore, A.; Jones, M. Bristol Ageing Better Community Navigators Service: Final Evaluation Report of a Social Prescribing Initiative Addressing Loneliness and Social Isolation Amongst Older People; Bristol Ageing Better Community: Bristol, UK, 2020. [Google Scholar]
- Borschmann, R.; Barrett, B.; Hellier, J.; Byford, S.; Henderson, C.; Rose, D.; Slade, M.; Sutherby, K.; Szmukler, G.; Thornicroft, G.; et al. Joint crisis plans for people with borderline personality disorder: Feasibility and outcomes in a randomised controlled trial. Br. J. Psychiatry 2013, 202, 357–364. [Google Scholar] [CrossRef]
- British Red Cross. Hope for the Future: Support for Survivors of Trafficking after the National Referral Mechanism; British Red Cross: London, UK, 2019. [Google Scholar]
- Cheshire, P.C.; Gibbons, S.; Mouland, J. Social tenants’ health: Evaluating the effectiveness of landlord interventions. J. Epidemiology Community Health 2018, 72, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Dalkin, S.M.; Forster, N.; Hodgson, P.; Lhussier, M.; Philipson, P.; Carr, S.M. Exposing the impact of intensive advice services on health: A realist evaluation. Health Soc. Care Community 2018, 27, 767–776. [Google Scholar] [CrossRef] [PubMed]
- Family Mosaic. Health Begins at Home; Final report; Family Mosaic: London, UK, 2016. [Google Scholar]
- Fisk, M.J. The health behaviour and wellbeing of older seafarers on Merseyside—Indicated changes through brief interventions. Int. Marit. Health 2017, 68, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Bradley, J.; Waite, F.; Sheaves, B.; DeWeever, N.; Bourke, E.; McInerney, J.; Evans, N.; Černis, E.; Lister, R.; et al. Targeting Recovery in Persistent Persecutory Delusions: A Proof of Principle Study of a New Translational Psychological Treatment (the Feeling Safe Programme). Behav. Cogn. Psychother. 2016, 44, 539–552. [Google Scholar] [CrossRef]
- Fullwood, Y. Blended evaluation of Phase 2 of the Age UK Personalised Integrated Care Programme; Age UK: London, UK, 2018. [Google Scholar]
- Hill-Dixon, A.; Solley, S.; Davis, H. Building Bridges, Building Health. In An Evaluation of SPEAR’s Homeless Health Link Service; The Young Foundation: London, UK, 2018. [Google Scholar]
- Lloyd-Evans, B.; Frerichs, J.; Stefanidou, T.; Bone, J.; Pinfold, V.; Lewis, G.; Billings, J.; Barber, N.; Chhapia, A.; Chipp, B.; et al. The Community Navigator Study: Results from a feasibility randomised controlled trial of a programme to reduce loneliness for people with complex anxiety or depression. PLoS ONE 2020, 15, e0233535. [Google Scholar] [CrossRef] [PubMed]
- Lovell, K.; Bee, P.; Brooks, H.; Cahoon, P.; Callaghan, P.; Carter, L.-A.; Cree, L.; Davies, L.; Drake, R.; Fraser, C.; et al. Embedding shared decision-making in the care of patients with severe and enduring mental health problems: The EQUIP pragmatic cluster randomised trial. PLoS ONE 2018, 13, e0201533. [Google Scholar] [CrossRef]
- Maxwell, M.; Hibberd, C.; Aitchison, P.; Calveley, E.; Pratt, R.; Dougall, N.; Hoy, C.; Mercer, S.; Cameron, I. The Patient Centred Assessment Method for improving nurse-led biopsychosocial assessment of patients with long-term conditions: A feasibility RCT. Health Serv. Deliv. Res. 2018, 6, 1–119. [Google Scholar] [CrossRef]
- Reidy, H.; Webber, M.; Rayner, S.; Jones, M. Evaluation of the Southwark Reablement Service; Kings College: London, UK, 2013. [Google Scholar]
- Smith, H.; Eckley, L.; Whelen, G. Evaluation of the Advocacy in Wirral’s Independent Mental Health Act and Psychiatric Liaison Advocacy Services; Liverpool John Moores University: Liverpool, UK, 2012. [Google Scholar]
- Thiel, V.; Sonola, L.; Goodwin, N.; Kodner, D.L. Co-Ordinated Care in the Sandwell Integrated Primary Care Mental Health and Wellbeing Service; The Esteem Team: London, UK, 2013. [Google Scholar]
- Woodhead, C.; Khondoker, M.; Lomas, R.; Raine, R. Impact of co-located welfare advice in healthcare settings: Prospective quasi-experimental controlled study. Br. J. Psychiatry 2017, 211, 388–395. [Google Scholar] [CrossRef]
- Bjornstad, G.; Cuffe-Fuller, B.; Ukoumunne, O.C.; Fredlund, M.; McDonald, A.; Wilkinson, K.; Lloyd, J.; Hawton, A.; Berry, V.; Tarrant, M.; et al. Healthy Parent Carers: Feasibility randomised controlled trial of a peer-led group-based health promotion intervention for parent carers of disabled children. Pilot Feasibility Stud. 2021, 7, 144. [Google Scholar] [CrossRef]
- Borek, A.; McDonald, B.; Fredlund, M.; Logan, S.; Morris, C. Healthy parent carers programme: Testing feasibility of a novel group-based intervention to improve the health and wellbeing of parents of disabled children. Dev. Med. Child Neurol. 2017, 59, 46. [Google Scholar]
- Bradley, C.; Day, C.; Penney, C.; Michelson, D. ‘Every day is hard, being outside, but you have to do it for your child’: Mixed-methods formative evaluation of a peer-led parenting intervention for homeless families. Clin. Child Psychol. Psychiatry 2020, 25, 860–876. [Google Scholar] [CrossRef]
- Cullen, S.M.; Cullen, M.-A.; Lindsay, G.; Str, S. The Parenting Early Intervention Programme in England, 2006-2011, A classed experience? Br. Educ. Res. J. 2013, 39, 1025–1043. [Google Scholar] [CrossRef][Green Version]
- Department for Digital Culture Media & Sport. Nesta/DCMS Centre for Social Action Innovation Fund Phase 2 Evaluation Report Summary Sheet; Department for Digital Culture Media & Sport: London, UK, 2019.
- Fisher, J.; Burchett, N. An Evaluation of Five Wellbeing Workshops in South Wales Created and Facilitated by Single Parents Wellbeing for Single Parents; Single Parents Wellbeing: Cardiff, UK, 2019. [Google Scholar]
- Fisher, J.; Gingell, R. Creating Connections Impact Report 2014–2016; Mental Health Foundation: Wales, UK, 2016. [Google Scholar]
- Gray, G.R.; Totsika, V.; Lindsay, G. Sustained Effectiveness of Evidence-Based Parenting Programs After the Research Trial Ends. Front. Psychol. 2018, 9, 2035. [Google Scholar] [CrossRef]
- Harwood, J.; Fernandez, L.; Vallejo, V.; Day, C. Baby and Us: Community-based, feasibility trial of a psychosocial intervention for new parents and their infants. J. Prev. 2022, 43, 589–604. [Google Scholar] [CrossRef] [PubMed]
- Hutchings, J.; Griffith, N.; Bywater, T.; Williams, M.E. Evaluating the Incredible Years Toddler Parenting Programme with parents of toddlers in disadvantaged (Flying Start) areas of Wales. Child Care Health Dev. 2016, 43, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.H.; Erjavec, M.; Viktor, S.; Hutchings, J. Outcomes of a Comparison Study into a Group-Based Infant Parenting Programme. J. Child Fam. Stud. 2016, 25, 3309–3321. [Google Scholar] [CrossRef] [PubMed]
- Knibbs, S.; Mollidor, C.; Bierman, R. KEEP Standard Evaluation; Department for Education: London, UK, 2016. [Google Scholar]
- Lindsay, G.; Strand, S.; Davis, H. A comparison of the effectiveness of three parenting programmes in improving parenting skills, parent mental-well being and children’s behaviour when implemented on a large scale in community settings in 18 English local authorities: The parenting early intervention pathfinder (PEIP). BMC Public Health 2011, 11, 962. [Google Scholar]
- Lindsay, G.; Totsika, V. The effectiveness of universal parenting programmes: The CANparent trial. BMC Psychol. 2017, 5, 35. [Google Scholar] [CrossRef] [PubMed]
- Robertson, W.; Fleming, J.; Kamal, A.; Hamborg, T.; A Khan, K.; Griffiths, F.; Stewart-Brown, S.; Stallard, N.; Petrou, S.; Simkiss, D.; et al. Randomised controlled trial and economic evaluation of the ‘Families for Health’ programme to reduce obesity in children. Arch. Dis. Child. 2016, 102, 416–426. [Google Scholar] [CrossRef] [PubMed]
- Simkiss, D.E.; A Snooks, H.; Stallard, N.; Kimani, P.K.; Sewell, B.; Fitzsimmons, D.; Anthony, R.; Winstanley, S.; Wilson, L.; Phillips, C.J.; et al. Effectiveness and cost-effectiveness of a universal parenting skills programme in deprived communities: Multicentre randomised controlled trial. BMJ Open 2013, 3, e002851. [Google Scholar] [CrossRef] [PubMed]
- Roadmap Evaluation Final Report; Connect Centre University of Central Lancashire, University of East London, Manchester Metropolitan University, Bangor University. 2021. Available online: https://www.womensaid.org.uk/wp-content/uploads/2021/10/Roadmap_Report_280921.pdf (accessed on 16 October 2022).
- Institute of Public Care Oxford Brookes University. Barnardo’s Cymru. In Opening Closed Doors Programme Evaluation; Final report; Institute of Public Care Oxford Brookes University: Oxford, UK, 2020. [Google Scholar]
- Tavistock Relationship. Tavistock Relationships project report; Tavistock Relationship: London, UK, 2019. [Google Scholar]
- Panayiotou, M.; Ville, E.; Poole, L.; Gill, V.; Humphrey, N. Learning from HeadStart: Does Cross-Age Peer Mentoring Help Young People with Emerging Mental Health Difficulties? Evidence Based Practice Unit: London, UK, 2020. [Google Scholar]
- Panayidou, F.; Priest, B. Enhancing postgraduate researcher wellbeing through support groups. Stud. Grad. Postdr. Educ. 2021, 12, 42–57. [Google Scholar] [CrossRef]
- Mental Health Foundation. An Evaluation of the Standing together Project; Mental Health Foundation: London, UK, 2018. [Google Scholar]
- Chakkalackal, L.; Kalathil, J. Peer Support Groups to Facilitate Self-Help Coping Strategies for People with Dementia in Extra Care Housing; Evaluation Report; Mental Health Foundation: London, UK, 2014. [Google Scholar]
- Marshall, J.; Devane, N.; Talbot, R.; Caute, A.; Cruice, M.; Hilari, K.; MacKenzie, G.; Maguire, K.; Patel, A.; Roper, A.; et al. A randomised trial of social support group intervention for people with aphasia: A Novel application of virtual reality. PLoS ONE 2020, 15, e0239715. [Google Scholar] [CrossRef] [PubMed]
- Get Set to Go Research Consortium. Get Set to Go: Research findings; Mind: London, UK, 2017. [Google Scholar]
- Jones, M.; Beardmore, A.; White, J. Effects of Bristol Ageing Better Projects for Older People; UWE Bristol: Bristol, UK, 2021. [Google Scholar]
- Jones, R.B.; Ashurst, E.J.; Atkey, J.; Duffy, B.; Helsper, E.; Bouwman, T. Older People Going Online: Its Value and Before-After Evaluation of Volunteer Support. J. Med Internet Res. 2015, 17, e122. [Google Scholar] [CrossRef] [PubMed]
- The Health Foundation. RIPPLE. Respiratory Innovation: Promoting Positive Life Experience; Shine 2014 final report; The Health Foundation: London, UK, 2015. [Google Scholar]
- Parsfield, M.; Morris, D.; Bola, M.; Knapp, M.; Yoshioka, M.; Marcus, G. Community Capital: The Valua of Connected Communities. 2015. Available online: https://www.thersa.org/globalassets/pdfs/reports/rsaj3718-connected-communities-report_web.pdf (accessed on 16 October 2022).
- Moreton, R.; Slutz, A.; Richards, S.; Choudhoury, A.; Mulia, I.; Daly, G. Evaluation of Ageing Better in Birmingham; Birmingham Voluntary Service Council: Leicester, UK, 2018. [Google Scholar]
- Bromley by Bow Centre. Macmillan Social Prescribing Service; Bromley by Bow Centre: London, UK, 2017. [Google Scholar]
- Dayson, C.; Leather, D. Evaluation of HALE Community Connectors Social Prescribing Service 2017; Sheffield Hallam University Centre for Regional Economic and Social Research: Sheffield, UK, 2018. [Google Scholar]
- Giebel, C.; Morley, N.; Komuravelli, A. A socially prescribed community service for people living with dementia and family carers and its long-term effects on well-being. Health Soc. Care Community 2021, 29, 1852–1857. [Google Scholar] [CrossRef] [PubMed]
- Pescheny, J.V.; Gunn, L.H.; Pappas, Y.; Randhawa, G. The impact of the Luton social prescribing programme on mental well-being: A quantitative before-and-after study. J. Public Health 2019, 43, e69–e76. [Google Scholar] [CrossRef]
- Southmead Development Trust; BS3 Community; UWE Bristol; Bristol City Council; NHS Bristol Clinical Commissioning Group. Community Webs. In Final Evaluation Report. Bristol, UK. 2018. Available online: https://www.bvsc.org/Handlers/Download.ashx?IDMF=baa5c034-f8eb-4dc2-a748-d22e439cbc0a (accessed on 16 October 2022).
- Morton, L.; Ferguson, M.; Baty, F. Improving wellbeing and self-efficacy by social prescription. Public Health 2015, 129, 286–289. [Google Scholar] [CrossRef]
- British Red Cross. Tackling Loneliness and Isolation: Findings from the Evaluation of Our Connecting Communities Service; British Red Cross: London, UK, 2019. [Google Scholar]
- Barker, A.B.; Winship, G. Recovery is no laughing matter–Or is it? Ment. Health Soc. Incl. 2016, 20, 167–173. [Google Scholar] [CrossRef]
- Clift, S.; Manship, S.; Stephens, L. Further evidence that singing fosters mental health and wellbeing: The West Kent and Medway project. Ment. Health Soc. Incl. 2017, 21, 53–62. [Google Scholar] [CrossRef]
- Crone, D.; Ellis, L.; Sumner, R. Flourish. Mixed Method Evaluation Final Report; ResearchGate GmbH: Berlin, Germany, 2017. [Google Scholar]
- Crone, D.M.; Sumner, R.C.; Baker, C.M.; A Loughren, E.; Hughes, S.; James, D.V.B. ‘Artlift’ arts-on-referral intervention in UK primary care: Updated findings from an ongoing observational study. Eur. J. Public Health 2018, 28, 404–409. [Google Scholar] [CrossRef]
- Efstathopoulou, L.; Bungay, H. Mental health and resilience: Arts on Prescription for children and young people in a school setting. Public Health 2021, 198, 196–199. [Google Scholar] [CrossRef]
- Fancourt, D.; Perkins, R.; Ascenso, S.; Atkins, L.; Kilfeather, S.; Carvalho, L.; Steptoe, A.; Williamon, A. Group Drumming Modulates Cytokine Response in Mental Health Services Users: A Preliminary Study. Psychother. Psychosom. 2015, 85, 53–55. [Google Scholar] [CrossRef]
- Fancourt, D.; Perkins, R.; Ascenso, S.; de Carvalho, L.A.; Steptoe, A.; Williamon, A. Effects of Group Drumming Interventions on Anxiety, Depression, Social Resilience and Inflammatory Immune Response among Mental Health Service Users. PLoS ONE 2016, 11, e0151136. [Google Scholar] [CrossRef]
- Fancourt, D.; Warran, K.; Finn, S.; Wiseman, T. Psychosocial singing interventions for the mental health and well-being of family carers of patients with cancer: Results from a longitudinal controlled study. BMJ Open 2019, 9, e026995. [Google Scholar] [CrossRef]
- Glenister, S. A Study of Stakeholder Perceptions of Noise Solution’s Practices: Measuring Impact on the Well-Being of Youth Facing Challenging Circumstances; University of Cambridge: Cambridge, UK, 2017. [Google Scholar]
- Margrove, K. Promoting the wellbeing and social inclusion of students through visual art at university: An Open Arts pilot project. J. Furth. High. Educ. 2013, 39, 147–162. [Google Scholar] [CrossRef]
- Margrove, K.L.; Heydinrych, K.; Secker, J. SE-SURG (South Essex Service User Research Group) Waiting list-controlled evaluation of a participatory arts course for people experiencing mental health problems. Perspect. Public Health 2012, 133, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Nevay, S.; Robertson, L.; Lim, C.S.; Moncur, W. Crafting Textile Connections: A mixed-methods approach to explore traditional and e-textile crafting for wellbeing. Des. J. 2019, 22, 487–501. [Google Scholar] [CrossRef]
- Poerio, G.; Totterdell, P. The Effect of Fiction on the Well-Being of Older Adults: A Longitudinal RCT Intervention Study Using Audiobooks. Psychosoc. Interv. 2020, 29, 29–38. [Google Scholar] [CrossRef]
- Ribbans, D.; Glenister, S. Noise Solution Impact Report 18/19. 2019. Available online: https://issuu.com/noisesolutionuk/docs/ns_impact_report_2019 (accessed on 15 December 2021).
- Secker, J.; Loughran, M.; Heydinrych, K.; Kent, L. Promoting mental well-being and social inclusion through art: Evaluation of an arts and mental health project. Arts Health 2011, 3, 51–60. [Google Scholar] [CrossRef]
- Sumner, R.; Hughes, S. See with Fresh Eyes: Mindful Photography for Improved Mental Health; A mixed-methods evaluation; University of Gloucestershire: Gloucestershire, UK, 2021. [Google Scholar]
- Tribe, R.H.; Alcock, K.; Scior, K.; Huddy, V. A mixed methods exploration of “Creativity in Mind”, an online creativity-based intervention for low mood and anxiety. J. Ment. Health 2021, 30, 734–742. [Google Scholar] [CrossRef] [PubMed]
- van de Venter, E.; Buller, A.M. Arts on referral interventions: A mixed-methods study investigating factors associated with differential changes in mental well-being. J. Public Health 2014, 37, 143–150. [Google Scholar] [CrossRef]
- Wilson, C.; Secker, J.; Kent, L.; Keay, J. Promoting mental wellbeing and social inclusion through art: Six month follow-up results from Open Arts Essex. Int. J. Ment. Health Promot. 2017, 19, 268–277. [Google Scholar] [CrossRef]
- Khan, L.; Saini, G.; Augustine, A.; Palmer, K.; Johnson, M.; Donald, R. Against the Odds: Evaluation of the Mind Birmingham Up My Street Programme; Centre for Mental Health: London, UK, 2017. [Google Scholar]
- Heaslip, V.; Darvill, T. Human Henge Wellbeing Research: Final Report; Bournemouth University: Bournemouth, UK, 2018. [Google Scholar]
- Ecorys. Arts for Wellbeing: Unlocking Social Energy to Increase Wellbeing; Ecorys UK: Birmingham, UK, 2017. [Google Scholar]
- Beishon, J.; Munoz, N. “I Feel Fitter and Better Being Outside”; Green Gym Evaluation Report; Royal Society for Public Health: Doncaster, UK, 2016. [Google Scholar]
- Chiumento, A.; Mukherjee, I.; Chandna, J.; Dutton, C.; Rahman, A.; Bristow, K. A haven of green space: Learning from a pilot pre-post evaluation of a school-based social and therapeutic horticulture intervention with children. BMC Public Health 2018, 18, 836. [Google Scholar] [CrossRef]
- Farrier, A.; Baybutt, M.; Dooris, M. Mental health and wellbeing benefits from a prisons horticultural programme. Int. J. Prison. Health 2019, 15, 91–104. [Google Scholar] [CrossRef]
- Kearns, A.; Ghosh, S.; Mason, P.; Egan, M. Urban regeneration and mental health: Investigating the effects of an area-based intervention using a modified intention to treat analysis with alternative outcome measures. Health Place 2020, 61, 102262. [Google Scholar] [CrossRef]
- Maund, P.R.; Irvine, K.N.; Reeves, J.; Strong, E.; Cromie, R.; Dallimer, M.; Davies, Z.G. Wetlands for Wellbeing: Piloting a Nature-Based Health Intervention for the Management of Anxiety and Depression. Int. J. Environ. Res. Public Health 2019, 16, 4413. [Google Scholar] [CrossRef] [PubMed]
- Sumner, R.; Sitch, M.; Stonebridge, N. A Mixed Method Evaluation of the Nature on Prescription Social Prescribing Programme; University of Gloucestershire: Gloucestershire, UK, 2020. [Google Scholar]
- Wilson, N.W.; Jones, R.; Fleming, S.; Lafferty, K.; Knifton, L.; Cathrine, K.; McNish, H. Branching Out: The Impact of a Mental Health Ecotherapy Program. Ecopsychology 2011, 3, 51–57. [Google Scholar] [CrossRef]
- Connolly, L.J.; Scott, S.; Morencos, C.M.; Fulford, J.; Jones, A.M.; Knapp, K.; Krustrup, P.; Bailey, S.J.; Bowtell, J.L. Impact of a novel home-based exercise intervention on health indicators in inactive premenopausal women: A 12-week randomised controlled trial. Eur. J. Appl. Physiol. 2020, 120, 771–782. [Google Scholar] [CrossRef]
- Corepal, R.; Best, P.; O’Neill, R.; Kee, F.; Badham, J.; Dunne, L.; Miller, S.; Connolly, P.; Cupples, M.E.; Van Sluijs, E.M.F.; et al. A feasibility study of ‘The StepSmart Challenge’ to promote physical activity in adolescents. Pilot Feasibility Stud. 2019, 5, 132. [Google Scholar] [CrossRef]
- France, J.; Sennett, J.; Jones, A.; Fordham, R.; Williams, J.; Burke, A.; Meierkord, A.; Fong Soe Khioe, R.; Suhroke, M. Evaluation of Walking for Health; Final report to Macmillan and the Ramblers; Ecorys: Birmingham, UK, 2016. [Google Scholar]
- Gray, R.; Gow, A.J. Cycling Without Age: Assessing the Impact of a Cycling-Based Initiative on Mood and Wellbeing. Gerontol. Geriatr. Med. 2020, 6, 2333721420946638. [Google Scholar] [CrossRef] [PubMed]
- Hadley, R.; Eastwood-Gray, O.; Kiddier, M.; Rose, D.; Ponzo, S. “Dance Like Nobody’s Watching”: Exploring the Role of Dance-Based Interventions in Perceived Well-Being and Bodily Awareness in People With Parkinson’s. Front. Psychol. 2020, 11, 531567. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.A. The relationship between physical inactivity and mental wellbeing: Findings from a gamification-based community-wide physical activity intervention. Health Psychol. Open 2018, 5. [Google Scholar] [CrossRef]
- Henderson, C.; O’Hara, S.; Thornicroft, G.; Webber, M. Corporate social responsibility and mental health: The Premier League football Imagine Your Goals programme. Int. Rev. Psychiatry 2014, 26, 460–466. [Google Scholar] [CrossRef]
- Hunter, R.F.; on behalf of the Physical Activity Loyalty (PAL) Study team; Murray, J.M.; Gough, A.; Tang, J.; Patterson, C.C.; French, D.P.; McIntosh, E.; Xin, Y.; Kee, F. Effectiveness and cost-effectiveness of a loyalty scheme for physical activity behaviour change maintenance: Results from a cluster randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 127. [Google Scholar] [CrossRef] [PubMed]
- Kay, C.W.P.; McKenna, J. The enduring well-being impacts of attending the Battle Back Multi Activity Course for the lives of recovering UK armed forces personnel. Mil. Psychol. 2022, 34, 410–421. [Google Scholar] [CrossRef]
- Lewis, C.J.; Reeves, M.J.; Roberts, S.J. Improving the physical and mental well-being of typically hard-to-reach men: An investigation of the impact of the Active Rovers project. Sport Soc. 2017, 20, 258–268. [Google Scholar] [CrossRef]
- Malcolm, E.; Evans-Lacko, S.; Little, K.; Henderson, C.; Thornicroft, G. The impact of exercise projects to promote mental wellbeing. J. Ment. Health 2013, 22, 519–527. [Google Scholar] [CrossRef]
- Peacock, S.M.; McKenna, J.; Carless, D.; Cooke, C. Outcomes from a One-Week Adapted Sport and Adapted Adventure Recovery Programme for Military Personnel. Sports 2019, 7, 135. [Google Scholar] [CrossRef]
- Tew, G.A.; Howsam, J.; Hardy, M.; Bissell, L. Adapted yoga to improve physical function and health-related quality of life in physically-inactive older adults: A randomised controlled pilot trial. BMC Geriatr. 2017, 17, 131. [Google Scholar] [CrossRef]
- Walker, L.; Smith, N.; Delon, C. Weight loss, hypertension and mental well-being improvements during COVID-19 with a multicomponent health promotion programme on Zoom: A service evaluation in primary care. BMJ Nutr. Prev. Health 2021, 4, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Newbury-Birch, D.; Scott, S.; O’Donnell, A.; Coulton, S.; Howel, D.; McColl, E.; Stamp, E.; Graybill, E.; Gilvarry, E.; Laing, K.; et al. A pilot feasibility cluster randomised controlled trial of screening and brief alcohol intervention to prevent hazardous drinking in young people aged 14–15 years in a high school setting (SIPS JR-HIGH). Public Health Res. 2014, 5, 2055102917753853. [Google Scholar] [CrossRef]
- Giles, E.L.; McGeechan, G.J.; Coulton, S.; Deluca, P.; Drummond, C.; Howel, D.; Kaner, E.; McColl, E.; McGovern, R.; Scott, S. Brief alcohol intervention for risky drinking in young people aged 14 15 years in secondary schools: The SIPS JR-HIGH RCT. Public Health Res. 2019, 7. Available online: https://pubmed.ncbi.nlm.nih.gov/31067018/ (accessed on 16 October 2022). [CrossRef] [PubMed]
- Johnson, R.; Robertson, W.; Towey, M.; Stewart-Brown, S.; Clarke, A. Changes over time in mental well-being, fruit and vegetable consumption and physical activity in a community-based lifestyle intervention: A before and after study. Public Health 2017, 146, 118–125. [Google Scholar] [CrossRef]
- Callaghan, L.; Thompson, T.P.; Creanor, S.; Quinn, C.; Senior, J.; Green, C.; Hawton, A.; Byng, R.; Wallace, G.; Sinclair, J.; et al. Individual health trainers to support health and well-being for people under community supervision in the criminal justice system: The STRENGTHEN pilot RCT. Public Health Res. 2019, 7. Available online: https://www.ncbi.nlm.nih.gov/books/NBK551448/ (accessed on 16 October 2022). [CrossRef] [PubMed]
- CLES Consulting, New Economics Foundation. Big Lottery Fund National Well-Being Evaluation: The Big Lottery Fund; CLES: Manchester, UK, 2013. [Google Scholar]
- Scott, L.; Williams, J.; Molyneux, J.; Whitley, J. Wellbeing 2 Programme Evaluation: A final Report to the Big Lottery Fund; Ecorys: Birmingham, UK, 2014. [Google Scholar]
- Age UK. Fit as a Fiddle. Final Evaluation Report—Community Network Engaging Isolated Older Adults for Improved Health and Well-Being; Age UK: London, UK, 2013. [Google Scholar]
- Wigfield, A.; Kispeter, E.; Alden, A.; Turner, R. Age UK’s Fit for the Future Project: Evaluation Report; Centre for International Research on Care, Labour and Equalities, University of Leeds: Leeds, UK, 2015. [Google Scholar]
- Scanlon, K.; Bradshaw-Walsh, K.; McNeil, B.; Bryson, C.; Purdon, S.; Fischer, J.; Piazza, R.; Fowler, B. The Youth Investment Fund: Learning and Insight Paper Seven: Findings from A Shared Evaluation of Open Access Youth Provision; Technical report; NPC: London, UK, 2021. [Google Scholar]
- Day, L.; Campbell-Jack, D.; Bertolotto, E. Evaluation of the Peer Support for Mental Health and Wellbeing Pilots; Depatment for Education: London, UK, 2020.
- Ministry of Housing Communities and Local Government. National Evaluation of the Troubled Families Programme 2015–2020: Findings; Ministry of Housing Communities and Local Government: London, UK, 2019.
- Acton, J.H.; Molik, B.; Court, H.; Margrain, T.H. Effect of a Home Visit–Based Low Vision Rehabilitation Intervention on Visual Function Outcomes: An Exploratory Randomized Controlled Trial. Investig. Opthalmology Vis. Sci. 2016, 57, 6662–6667. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Watson, R.; Wright, B.; Baggaley, J.; Rapley, T.; Pearse, J. Early therapy in perinatal stroke: Pilot feasibility trial. Dev. Med. Child Neurol. 2018, 60, 9. [Google Scholar]
- Elnazer, H.Y.; Sampson, A.P.; Baldwin, D.S. Effects of celecoxib augmentation of antidepressant or anxiolytic treatment on affective symptoms and inflammatory markers in patients with anxiety disorders: Exploratory study. Int. Clin. Psychopharmacol. 2021, 36, 126–132. [Google Scholar] [CrossRef]
- Evans, C.; Banissy, M.J.; Charlton, R.A. The efficacy of transcranial random noise stimulation (tRNS) on mood may depend on individual differences including age and trait mood. Clin. Neurophysiol. 2018, 129, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Osborn, D.; Burton, A.; Hunter, R.; Marston, L.; Atkins, L.; Barnes, T.; Blackburn, R.; Craig, T.; Gilbert, H.; Heinkel, S.; et al. Clinical and cost-effectiveness of an intervention for reducing cholesterol and cardiovascular risk for people with severe mental illness in English primary care: A cluster randomised controlled trial. Lancet Psychiatry 2018, 5, 145–154. [Google Scholar] [CrossRef]
- Steel, C.; Korrelboom, K.; Baksh, M.F.; Kingdon, D.; Simon, J.; Wykes, T.; Phiri, P.; van der Gaag, M. Positive memory training for the treatment of depression in schizophrenia: A randomised controlled trial. Behav. Res. Ther. 2020, 135, 103734. [Google Scholar] [CrossRef]
- Stuttard, L.; Boyle, P.; Fairhurst, C.; Hewitt, C.; Longo, F.; Walker, S.; Weatherly, H.; Mayhew, E.; Beresford, B. Hearing dogs for people with severe and profound hearing loss: A wait-list design randomised controlled trial investigating their effectiveness and cost-effectiveness. Trials 2021, 22, 700. [Google Scholar] [CrossRef] [PubMed]
- Slade, M.; Bird, V.; Clarke, E.; Le Boutillier, C.; McCrone, P.; Macpherson, R.; Pesola, F.; Wallace, G.; Williams, J.; Leamy, M. Supporting recovery in patients with psychosis through care by community-based adult mental health teams (REFOCUS): A multisite, cluster, randomised, controlled trial. Lancet Psychiatry 2015, 2, 503–514. [Google Scholar] [CrossRef]
- Webber, M.; Morris, D.; Howarth, S.; Fendt-Newlin, M.; Treacy, S.; McCrone, P. Effect of the Connecting People Intervention on Social Capital: A Pilot Study. Res. Soc. Work Pract. 2018, 29, 483–494. [Google Scholar] [CrossRef]
- Stansfeld, S.A.; Kerry, S.; Chandola, T.; Russell, J.; Berney, L.; Hounsome, N.; Lanz, D.; Costelloe, C.; Smuk, M.; Bhui, K. Pilot study of a cluster randomised trial of a guided e-learning health promotion intervention for managers based on management standards for the improvement of employee well-being and reduction of sickness absence: GEM Study. BMJ Open 2015, 5, e007981. [Google Scholar] [CrossRef] [PubMed]
- Ebrahim, S.; Glascott, A.; Mayer, H.; Gair, E. Recovery Colleges; how effective are they? J. Ment. Health Train. Educ. Pract. 2018, 13, 209–218. [Google Scholar] [CrossRef]
- Foundation, M.H. Progression Together: An Evaluation of A Model of Personalised Residential Care Developed by together for Mental Wellbeing; Mental Health Foundation: London, UK, 2016. [Google Scholar]
- Harrison, R.; Cochrane, M.; Pendlebury, M.; Noonan, R.; Eckley, L.; Sumnall, H.; Timpson, H. Evaluation of Four Recovery Communities across England: Final Report for the Give It Up Project; Liverpool John Moores University: Liverpool, UK, 2017. [Google Scholar]
- Lamb, D.; Steare, T.; Marston, L.; Canaway, A.; Johnson, S.; Kirkbride, J.B.; Lloyd-Evans, B.; Morant, N.; Pinfold, V.; Smith, D.; et al. A comparison of clinical outcomes, service satisfaction and well-being in people using acute day units and crisis resolution teams: Cohort study in England. BJPsych Open 2021, 7, e68. [Google Scholar] [CrossRef]
- Wilson, C.; King, M.; Russell, J. A mixed-methods evaluation of a Recovery College in South East Essex for people with mental health difficulties. Health Soc. Care Community 2019, 27, 1353–1362. [Google Scholar] [CrossRef] [PubMed]
- Naruse, S.M.; Moss, M. Effects of couples positive massage programme on wellbeing, perceived stress and coping, and relation satisfaction. Health Psychol. Behav. Med. 2019, 7, 328–347. [Google Scholar] [CrossRef] [PubMed]
- Elphick, H.E.; Lawson, C.; Ives, A.; Siddall, S.; Kingshott, R.N.; Reynolds, J.; Dawson, V.; Hall, L. Pilot study of an integrated model of sleep support for children: A before and after evaluation. BMJ Paediatr Open 2019, 3, e000551. [Google Scholar] [CrossRef]
- Gensler, The Helen Hamlyn Centre for Design. Workplace & Wellbeing: What Aspects of Workplace Design Are Most Important to People’s Wellbeing; Gensler, The Helen Hamlyn Centre for Design: London, UK, 2016. [Google Scholar]
- Collis, A.; Eggers, F. Effects of Restricting Social Media Usage; Sloan School of Management, Massachusetts Institute of Technology Faculty of Economics and Business, University of Groningen: Groningen, The Netherlands, 2020. [Google Scholar]
- Evans, S.; Waller, S.; Bray, J.; Atkinson, T. Making Homes More Dementia-Friendly through the Use of Aids and Adaptations. Healthcare 2019, 7, 43. [Google Scholar] [CrossRef]
- Sumner, R.; Crone, D.; Hughes, S.; James, D. Arts on prescription: Observed changes in anxiety, depression, and well-being across referral cycles. Public Health 2021, 192, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Sumner, R.C.; Crone, D.M.; Baker, C.; Hughes, S.; A Loughren, E.; James, D.V.B. Factors associated with attendance, engagement and wellbeing change in an arts on prescription intervention. J. Public Health 2020, 42, e88–e95. [Google Scholar] [CrossRef]
- Stansfeld, S.A.; Berney, L.; Bhui, K.; Chandola, T.; Costelloe, C.; Hounsome, N.; Kerry, S.; Lanz, D.; Russell, J. Pilot study of a randomised trial of a guided e-learning health promotion intervention for managers based on management standards for the improvement of employee well-being and reduction of sickness absence: The GEM (Guided E-learning for Managers) study. Public Health Res. 2015, 3. [Google Scholar] [CrossRef] [PubMed]
- Robertson, W.; Fleming, J.; Kamal, A.; Hamborg, T.; A Khan, K.; Griffiths, F.; Stewart-Brown, S.; Stallard, N.; Petrou, S.; Simkiss, D.; et al. Randomised controlled trial evaluating the effectiveness and cost-effectiveness of ‘Families for Health’, a family-based childhood obesity treatment intervention delivered in a community setting for ages 6 to 11 years. Health Technol. Assess. 2017, 21. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, G. Primary care chaplaincy: A valid talking therapy? Br. J. Gen. Pract. 2017, 67, 77. [Google Scholar] [CrossRef]
- Luik, A.I.; Marsden, A.; Emsley, R.; Henry, A.; Stott, R.; Miller, C.B.; Espie, C.A. Long-term benefits of digital cognitive behavioural therapy for insomnia: Follow-up report from a randomized clinical trial. J. Sleep Res. 2020, 29, e13018. [Google Scholar] [CrossRef] [PubMed]
- Leeds Beckett University. Carnegie Great Outdoors; Leeds Beckett University: Leeds, UK, 2021. [Google Scholar]
- Kay, C.W.P.; McKenna, J. Battle Back: Adaptive Adventure Sports and Military Recovery; Royal British Legion: London, UK, 2019. [Google Scholar]
- The Carnegie School of Sport Leeds Beckett University. Battle Back Veterans Courses: Well-Being Impact Research 2019; The Carnegie School of Sport Leeds Beckett University: Leeds, UK, 2019. [Google Scholar]
- The Carnegie School of Sport Leeds Beckett University. Battle Back Multi Activity Course Impact Report; The Carnegie School of Sport Leeds Beckett University: Leeds, UK, 2018. [Google Scholar]
- Glenister, S. Changes in well-being of youth in challenging circumstances: Evaluation after a 10-week intervention combining music mentoring and digital storytelling. Transform. New Voice Community Music. 2018, 1, 59–80. [Google Scholar]
- Dawson, V.; Elphick, H. Behavioural intervention to improve sleep for children: Aiming to improve physical, mental and emotional wellbeing. Perspect. Public Health 2019, 139, 66–67. [Google Scholar] [CrossRef]
- Crone, D.M.; O’Connell, E.E.; Tyson, P.J.; Clark-Stone, F.; Opher, S.; James, D.V. ‘Art Lift’ intervention to improve mental well-being: An observational study from U.K. general practice. Int. J. Ment. Health Nurs. 2013, 22, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Crone, D.; Hughes, S.; Sumner, R.; Darch, J. Mixed Method Evaluation Final Report; Flourish 2; University of Gloucestershire: Cheltenham, UK, 2018. [Google Scholar]
- British Red Cross. Tackling Loneliness Together: British Red Cross and Co-Op End of Partnership Report; British Red Cross: London, UK, 2020. [Google Scholar]
- Ecorys UK, University of Keele Centre for Social Gerontology. Fit as a Fiddle: Final Evaluation Report; Ecorys: Birmingham, UK, 2013. [Google Scholar]
- Warwick Medical School. Collect, Score, Analyse and Interpret WEMWBS. Available online: https://warwick.ac.uk/fac/sci/med/research/platform/wemwbs/using/howto/ (accessed on 15 January 2022).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Brown, M.; Glendenning, A.; E Hoon, A.; John, A. Effectiveness of Web-Delivered Acceptance and Commitment Therapy in Relation to Mental Health and Well-Being: A Systematic Review and Meta-Analysis. J. Med Internet Res. 2016, 18, e221. [Google Scholar] [CrossRef] [PubMed]
- Chakhssi, F.; Kraiss, J.T.; Sommers-Spijkerman, M.; Bohlmeijer, E.T. The effect of positive psychology interventions on well-being and distress in clinical samples with psychiatric or somatic disorders: A systematic review and meta-analysis. BMC Psychiatry 2018, 18, 211. [Google Scholar] [CrossRef]
- Weiss, L.A.; Westerhof, G.J.; Bohlmeijer, E.T. Can We Increase Psychological Well-Being? The Effects of Interventions on Psychological Well-Being: A Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2016, 11, e0158092. [Google Scholar] [CrossRef]
- Sakuraya, A.; Imamura, K.; Watanabe, K.; Asai, Y.; Ando, E.; Eguchi, H.; Nishida, N.; Kobayashi, Y.; Arima, H.; Iwanaga, M.; et al. What Kind of Intervention Is Effective for Improving Subjective Well-Being Among Workers? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Psychol. 2020, 11, 528656. [Google Scholar] [CrossRef]
- MacKenzie, K.; Williams, C. Universal, school-based interventions to promote mental and emotional well-being: What is being done in the UK and does it work? A systematic review. BMJ Open 2018, 8, e022560. [Google Scholar] [CrossRef] [PubMed]
- Naghieh, A.; Montgomery, P.; Bonell, C.P.; Thompson, M.; Aber, J.L. Organisational interventions for improving wellbeing and reducing work-related stress in teachers. Cochrane Database Syst. Rev. 2015, 4, Cd010306. [Google Scholar] [CrossRef] [PubMed]
- Naehrig, D.; Schokman, A.; Hughes, J.K.; Epstein, R.; Hickie, I.B.; Glozier, N. Effect of interventions for the well-being, satisfaction and flourishing of general practitioners-a systematic review. BMJ Open 2021, 11, e046599. [Google Scholar] [CrossRef] [PubMed]

| N (%) | |
|---|---|
| Evidence type | |
| Peer-reviewed publication | 150 (71.8) |
| Report | 53 (25.4) |
| Other (e.g., evaluation summaries and evidence briefings) | 6 (2.0) |
| Age group a | |
| Children (0–10) | 3 (1.4) |
| Adolescents (11–18) | 22 (10.5) |
| Young adults (19–25) | 76 (36.4) |
| Adults (26–59) | 175 (83.7) |
| Older adults (60+) | 63 (30.1) |
| Control group | |
| No | 132 (63.2) |
| Yes | 77 (36.8) |
| Randomisation (for studies with control group) | |
| Individual randomisation | 33 (44.0) |
| No randomisation nor wait-list | 18 (24.0) |
| Wait-list control group | 13 (17.3) |
| Cluster randomisation | 11 (14.7) |
| Wellbeing measure | |
| 14-item WEMWBS | 145 (69.4) |
| 7-item SWEMWBS | 64 (30.6) |
| Examined WEMWBS scores by subgroup | |
| No | 174 (83.3) |
| Yes | 35 (16.7) |
| Assessment at additional follow-up points | |
| No | 143 (68.4) |
| Yes | 66 (31.6) |
| Theme | Intervention Subtheme | SMD (95% Confidence Intervals) a |
|---|---|---|
| Psychological | Resilience, self-management and wellness | 0.72 (0.42, 1.02) |
| Arts, Environment & Culture | Art | 0.62 (0.45, 0.79) |
| Social | Person-centred support and advice | 0.58 (0.14, 1.02) |
| Psychological | CBT | 0.58 (0.42, 0.75) |
| Social | Social prescribing | 0.55 (0.45, 0.64) |
| Social | Parenting | 0.53 (0.38, 0.68) |
| Psychological | Psychoeducation | 0.52 (0.17, 0.87) |
| Psychological | Mindfulness | 0.51 (0.33, 0.72) |
| Physical health promotion | Physical activity | 0.38 (0.14, 0.61) |
| Social | Peer-support | 0.18 (−0.16, 0.52) |
| Community-based | 0.17 (0.06, 0.29) | |
| Arts, Environment & Culture | Environment | −0.05 (−0.14, 0.05) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blodgett, J.M.; Birch, J.M.; Musella, M.; Harkness, F.; Kaushal, A. What Works to Improve Wellbeing? A Rapid Systematic Review of 223 Interventions Evaluated with the Warwick-Edinburgh Mental Well-Being Scales. Int. J. Environ. Res. Public Health 2022, 19, 15845. https://doi.org/10.3390/ijerph192315845
Blodgett JM, Birch JM, Musella M, Harkness F, Kaushal A. What Works to Improve Wellbeing? A Rapid Systematic Review of 223 Interventions Evaluated with the Warwick-Edinburgh Mental Well-Being Scales. International Journal of Environmental Research and Public Health. 2022; 19(23):15845. https://doi.org/10.3390/ijerph192315845
Chicago/Turabian StyleBlodgett, Joanna M., Jack M. Birch, Margherita Musella, Frances Harkness, and Aradhna Kaushal. 2022. "What Works to Improve Wellbeing? A Rapid Systematic Review of 223 Interventions Evaluated with the Warwick-Edinburgh Mental Well-Being Scales" International Journal of Environmental Research and Public Health 19, no. 23: 15845. https://doi.org/10.3390/ijerph192315845
APA StyleBlodgett, J. M., Birch, J. M., Musella, M., Harkness, F., & Kaushal, A. (2022). What Works to Improve Wellbeing? A Rapid Systematic Review of 223 Interventions Evaluated with the Warwick-Edinburgh Mental Well-Being Scales. International Journal of Environmental Research and Public Health, 19(23), 15845. https://doi.org/10.3390/ijerph192315845






