Flourishing or Languishing? Predictors of Positive Mental Health in Medical Students during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Instruments
2.3. Statistical Analysis
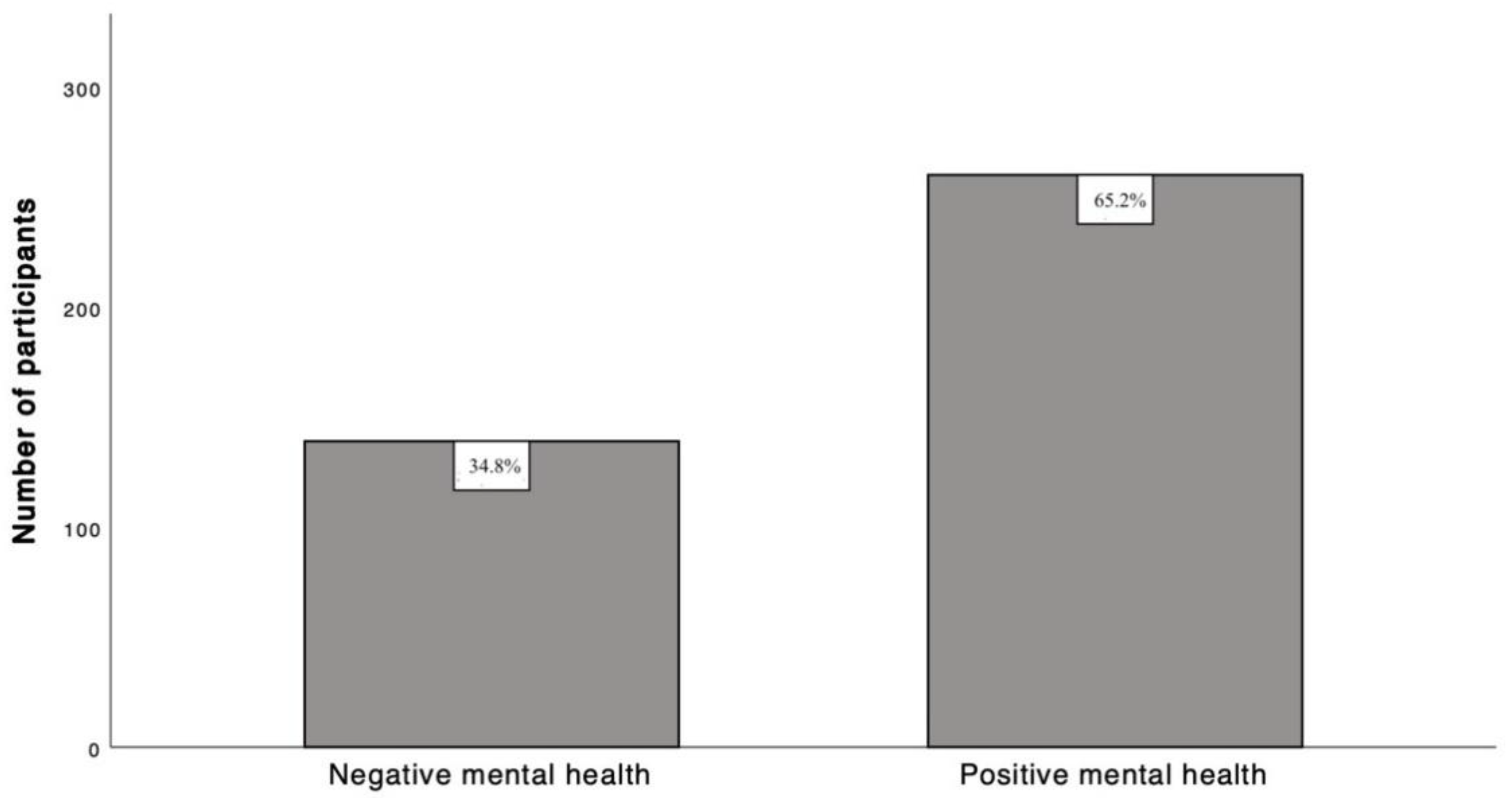
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Concerto, C.; Conti, C.; Muscatello, M.R.; Signorelli, M.S.; Zoccali, R.; Coira, D.; Aguglia, E.; Battaglia, F. Sleep Quality, Perceived Stress, and Caffeinated Drinks Intake in Psychiatry Residents: A Cross-Sectional Study. J. Caffeine Res. 2017, 7, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Sawah, M.A.; Ruffin, N.; Rimawi, M.; Concerto, C.; Aguglia, E.; Chusid, E.; Infortuna, C.; Battaglia, F. Perceived Stress and Coffee and Energy Drink Consumption Predict Poor Sleep Quality in Podiatric Medical Students A Cross-sectional Study. J. Am. Podiatr. Med. Assoc. 2015, 105, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Mineo, L.; Concerto, C.; Patel, D.; Mayorga, T.; Chusid, E.; Infortuna, C.; Aguglia, E.; Sarraf, Y.; Battaglia, F. Modulation of sensorimotor circuits during retrieval of negative Autobiographical Memories: Exploring the impact of personality dimensions. Neuropsychologia 2018, 110, 190–196. [Google Scholar] [CrossRef]
- Mineo, L.; Concerto, C.; Patel, D.; Mayorga, T.; Paula, M.; Chusid, E.; Aguglia, E.; Battaglia, F. Valeriana officinalis Root Extract Modulates Cortical Excitatory Circuits in Humans. Neuropsychobiology 2017, 75, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Infortuna, C.; Mineo, L.; Buffer, S.; Thomas, F.P.; Muscatello, M.R.A.; Aguglia, E.; Bruno, A.; Zoccali, R.A.; Sheikh, A.; Chusid, E.; et al. Acute social and somatic stress alters cortical metaplasticity probed with non-invasive brain stimulation in humans. Int. J. Psychophysiol. 2021, 170, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Concerto, C.; Patel, D.; Infortuna, C.; Chusid, E.; Muscatello, M.R.; Bruno, A.; Zoccali, R.; Aguglia, E.; Battaglia, F. Academic stress disrupts cortical plasticity in graduate students. Stress 2017, 20, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Concerto, C.; Infortuna, C.; Muscatello, M.R.A.; Bruno, A.; Zoccali, R.; Chusid, E.; Aguglia, E.; Battaglia, F. Exploring the effect of adaptogenic Rhodiola Rosea extract on neuroplasticity in humans. Complement Ther. Med. 2018, 41, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Dahlin, M.; Joneborg, N.; Runeson, B. Stress and depression among medical students: A cross-sectional study. Med. Educ. 2005, 39, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, C. Stress, coping and burn-out in nursing students. Int. J. Nurs. Stud. 2010, 47, 1299–1309. [Google Scholar] [CrossRef] [PubMed]
- Struthers, C.W.; Perry, R.P.; Menec, V.H. An examination of the relationship among academic stress, coping, motivation, and performance in college. Res. High. Educ. 2000, 41, 581–592. [Google Scholar] [CrossRef]
- Wyatt, T.; Oswalt, S.B. Comparing mental health issues among undergraduate and graduate students. Am. J. Health Educ. 2013, 44, 96–107. [Google Scholar] [CrossRef]
- Consorti, F.; Familiari, G.; Lotti, A.; Torre, D. Medical education in Italy: Challenges and opportunities. Med. Teach. 2021, 43, 1242–1248. [Google Scholar] [CrossRef] [PubMed]
- Kavvadas, D.; Kavvada, A.; Karachrysafi, S.; Papaliagkas, V.; Cheristanidis, S.; Chatzidimitriou, M.; Papamitsou, T. Stress, Anxiety and Depression Prevalence among Greek University Students during COVID-19 Pandemic: A Two-Year Survey. J. Clin. Med. 2022, 11, 4263. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Chen, B.; Sun, J.; Feng, Y. How Have COVID-19 Isolation Policies Affected Young People’s Mental Health?—Evidence From Chinese College Students. Front. Psychol. 2020, 11, 1529. [Google Scholar] [CrossRef]
- Sahu, P. Closure of Universities Due to Coronavirus Disease 2019 (COVID-19): Impact on Education and Mental Health of Students and Academic Staff. Cureus 2020, 12, e7541. [Google Scholar] [CrossRef]
- Chakladar, J.; Diomino, A.; Li, W.T.; Tsai, J.C.; Krishnan, A.R.; Zou, A.E.; Kharidia, K.; Baig, F.A.; Householder, S.; Kuo, S.Z.; et al. Medical student’s perception of the COVID-19 pandemic effect on their education and well-being: A cross-sectional survey in the United States. BMC Med. Educ. 2022, 22, 149. [Google Scholar] [CrossRef] [PubMed]
- Grøtan, K.; Sund, E.R.; Bjerkeset, O. Mental Health, Academic Self-Efficacy and Study Progress Among College Students—The SHoT Study, Norway. Front. Psychol. 2019, 10, 45. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L. The mental health continuum: From languishing to flourishing in life. J. Health Soc. Behav. 2002, 43, 207–222. [Google Scholar] [CrossRef]
- Keyes, C.L. The mental health continuum: From languishing to flourishing in life (2002). Found. Psychol. Thought A Hist. Psychol. 2009, 601–617. [Google Scholar]
- Infortuna, C.; Gratteri, F.; Benotakeia, A.; Patel, S.; Fleischman, A.; Muscatello, M.R.A.; Bruno, A.; Zoccali, R.A.; Chusid, E.; Han, Z.; et al. Exploring the Gender Difference and Predictors of Perceived Stress among Students Enrolled in Different Medical Programs: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 6647. [Google Scholar] [CrossRef] [PubMed]
- Infortuna, C.; Silvestro, S.; Crenshaw, K.; Muscatello, M.R.A.; Bruno, A.; Zoccali, R.A.; Chusid, E.; Intrator, J.; Han, Z.; Battaglia, F. Affective Temperament Traits and Age-Predicted Recreational Cannabis Use in Medical Students: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 4836. [Google Scholar] [CrossRef] [PubMed]
- Mineo, L.; Sarraf, Y.; Ingram, C.; Hanauer, S.; Infortuna, C.; Chusid, E.; Coira, D.; Aguglia, E.; Battaglia, F. Affective temperaments and stimulant medications misuse for neuroenhancement in graduate students. J. Subst. Use 2018, 23, 124–129. [Google Scholar] [CrossRef]
- Krejcie, R.V.; Morgan, D.W. Determining sample size for research activities. Educ. Psychol. Meas. 1970, 30, 607–610. [Google Scholar] [CrossRef]
- Bottesi, G.; Ghisi, M.; Altoe, G.; Conforti, E.; Melli, G.; Sica, C. The Italian version of the Depression Anxiety Stress Scales-21: Factor structure and psychometric properties on community and clinical samples. Compr. Psychiatry 2015, 60, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Preti, A.; Vellante, M.; Zucca, G.; Tondo, L.; Akiskal, K.; Akiskal, H. The Italian version of the validated short TEMPS-A: The temperament evaluation of Memphis, Pisa, Paris and San Diego. J. Affect. Disord. 2010, 120, 207–212. [Google Scholar] [CrossRef]
- Petrillo, G.; Capone, V.; Caso, D.; Keyes, C.L.M. The Mental Health Continuum–Short Form (MHC–SF) as a Measure of Well-Being in the Italian Context. Soc. Indic. Res. 2014, 121, 291–312. [Google Scholar] [CrossRef]
- Peters, L.; Peters, A.; Andreopoulos, E.; Pollock, N.; Pande, R.L.; Mochari-Greenberger, H. Comparison of DASS-21, PHQ-8, and GAD-7 in a virtual behavioral health care setting. Heliyon 2021, 7, e06473. [Google Scholar] [CrossRef] [PubMed]
- Salanti, G.; Peter, N.; Tonia, T.; Holloway, A.; White, I.R.; Darwish, L.; Low, N.; Egger, M.; Haas, A.D.; Fazel, S.; et al. The Impact of the COVID-19 Pandemic and Associated Control Measures on the Mental Health of the General Population: A Systematic Review and Dose-Response Meta-analysis. Ann. Intern. Med. 2022, 175, 1560–1571. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scales, 2nd ed.; Psychology Foundation of Australia: Sydney, NSW, Australia, 1995. [Google Scholar]
- Antony, M.M.; Bieling, P.J.; Cox, B.J.; Enns, M.W.; Swinson, R.P. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol. Assess. 1998, 10, 176–181. [Google Scholar] [CrossRef]
- Akiskal, H.S.; Mendlowicz, M.V.; Jean-Louis, G.; Rapaport, M.H.; Kelsoe, J.R.; Gillin, J.C.; Smith, T.L. TEMPS-A: Validation of a short version of a self-rated instrument designed to measure variations in temperament. J. Affect. Disord. 2005, 85, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Placidi, G.F.; Signoretta, S.; Liguori, A.; Gervasi, R.; Maremmani, I.; Akiskal, H.S. The semi-structured affective temperament interview (TEMPS-I). Reliability and psychometric properties in 1010 14-26-year old students. J. Affect. Disord. 1998, 47, 1–10. [Google Scholar] [CrossRef]
- Borkowska, A.; Rybakowski, J.K.; Drozdz, W.; Bielinski, M.; Kosmowska, M.; Rajewska-Rager, A.; Bucinski, A.; Akiskal, K.K.; Akiskal, H.S. Polish validation of the TEMPS-A: The profile of affective temperaments in a college student population. J. Affect. Disord. 2010, 123, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Hinić, D.; Akiskal, S.H.; Akiskal, K.K.; Jović, J.; Ignjatović Ristić, D. Validation of the Temps-A in university student population in Serbia. J. Affect. Disord. 2013, 149, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L. Mental health in adolescence: Is America’s youth flourishing? Am. J. Orthopsychiatry 2006, 76, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J. Consult. Clin. Psychol. 2005, 73, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Low, K.G. Flourishing, substance use, and engagement in students entering college: A preliminary study. J. Am. Coll. Health 2011, 59, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Harper, W.; Moutier, C.; Durning, S.J.; Power, D.V.; Massie, F.S.; Eacker, A.; Thomas, M.R.; Satele, D.; Sloan, J.A.; et al. A multi-institutional study exploring the impact of positive mental health on medical students’ professionalism in an era of high burnout. Acad. Med. 2012, 87, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Diener, E. Subjective well-being. The science of happiness and a proposal for a national index. Am. Psychol. 2000, 55, 34–43. [Google Scholar] [CrossRef]
- Iasiello, M.; Van Agteren, J. Mental health and/or mental illness: A scoping review of the evidence and implications of the dual-continua model of mental health. Evidence Base 2020, 1, 1–45. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Personal. Soc. Psychol. 1989, 57, 1069. [Google Scholar] [CrossRef]
- Antonovsky, A. The salutogenic model as a theory to guide health promotion. Health Promot. Int. 1996, 11, 11–18. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. On happiness and human potentials: A review of research on hedonic and eudaimonic well-being. Annu. Rev. Psychol. 2001, 52, 141. [Google Scholar] [CrossRef]
- Saraswathi, I.; Saikarthik, J.; Kumar, K.S.; Srinivasan, K.M.; Ardhanaari, M.; Gunapriya, R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: A prospective longitudinal study. PeerJ 2020, 8, e10164. [Google Scholar] [CrossRef] [PubMed]
- Bacchi, S.; Licinio, J. Resilience and Psychological Distress in Psychology and Medical Students. Acad. Psychiatry 2017, 41, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Liu, R.; Zhang, Y.; Zhang, R.; Liang, L.; Wang, Y.; Wei, Y.; Zhu, R.; Wang, F. Association between perceived stress and depression among medical students during the outbreak of COVID-19: The mediating role of insomnia. J. Affect. Disord. 2021, 292, 89–94. [Google Scholar] [CrossRef]
- Abullais, S.S.; Khan, A.A.; AlQahtani, S.A.; Al Zuhayr, A.Z.; Parveen, S.; Alassiri, A.S.; Alghamdi, K.A.; Mahmood, S.E. Coronavirus Disease (COVID-19) Associated Anxiety, Fear and Preparedness Among Healthcare Students at University Teaching Hospital in KSA. Psychol. Res. Behav. Manag. 2022, 15, 875–885. [Google Scholar] [CrossRef] [PubMed]
- Alsoufi, A.; Alsuyihili, A.; Msherghi, A.; Elhadi, A.; Atiyah, H.; Ashini, A.; Ashwieb, A.; Ghula, M.; Hasan, H.B.; Abudabuos, S.; et al. Impact of the COVID-19 pandemic on medical education: Medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS ONE 2020, 15, e0242905. [Google Scholar] [CrossRef] [PubMed]
- Lyons, Z.; Wilcox, H.; Leung, L.; Dearsley, O. COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australas. Psychiatry 2020, 28, 649–652. [Google Scholar] [CrossRef] [PubMed]
- Bali, H.; Rai, V.; Khanduri, N.; Tripathi, R.; Adhikari, K.; Sapkota, B. Perceived Stress and Stressors among Medical and Dental Students of Bhairhawa, Nepal: A Descriptive Cross-sectional Study. JNMA J. Nepal. Med. Assoc. 2020, 58, 383–389. [Google Scholar] [CrossRef]
- Iqbal, S.; Gupta, S.; Venkatarao, E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J. Med. Res. 2015, 141, 354–357. [Google Scholar] [CrossRef] [PubMed]
- Baba, H.; Kohno, K.; Inoue, T.; Nakai, Y.; Toyomaki, A.; Suzuki, T.; Hatano, K.; Arai, H.; Terao, T. The effects of mental state on assessment of bipolar temperament. J. Affect. Disord. 2014, 161, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Terao, T.; Shirahama, M.; Hatano, K.; Hirakawa, H.; Kohno, K.; Shiotsuki, I.; Ishii, N. Relationship between hyperthymic temperament, self-directedness, and self-transcendence in medical students and staff members. Psychiatry Clin. Neurosci. 2019, 73, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Shirahama, M.; Terao, T.; Ishii, N.; Hatano, K.; Hirakawa, H.; Kohno, K. Relationship between anxious temperament and harm avoidance in medical students and staff. Psychiatry Clin. Neurosci. 2018, 72, 322–328. [Google Scholar] [CrossRef]
- Dembinska-Krajewska, D.; Rybakowski, J. The Temperament Evaluation of Memphis, Pisa and San Diego Autoquestionnaire (TEMPS-A)—An important tool to study affective temperaments. Psychiatr. Pol. 2014, 48, 261–276. [Google Scholar] [PubMed]
- Bassi, M.; Negri, L.; Delle Fave, A.; Accardi, R. The relationship between post-traumatic stress and positive mental health symptoms among health workers during COVID-19 pandemic in Lombardy, Italy. J. Affect. Disord. 2021, 280, 1–6. [Google Scholar] [CrossRef] [PubMed]
| Severity | Depression | Anxiety | Stress |
|---|---|---|---|
| Normal | 0–9 | 0–7 | 0–14 |
| Mild | 10–13 | 8–9 | 15–18 |
| Moderate | 14–20 | 10–14 | 19–25 |
| Severe | 21–27 | 15–19 | 26–33 |
| Extremely severe | 28+ | 20+ | 34+ |
| Variable | ||
|---|---|---|
| Age | 23 [21–25] 1 | |
| Gender | Male | 279 (70.1%) |
| Female | 120 (29.9%) | |
| Relationship status | Single | 163 (40.9%) |
| Partnered | 236 (50.1%) | |
| Academic year | 1st year | 36 (9%) |
| 2nd year | 39 (9.8%) | |
| 3rd year | 50 (12.5%) | |
| 4th year | 71 (17.8%) | |
| 5th year | 57 (14.3%) | |
| 6th year | 146 (36.6%) | |
| Psychoactive drugs | No | 370 (92.7%) |
| Yes | 29 (7.3%) | |
| Smoking | No | 329 (82.5%) |
| Yes | 70 (17.5%) | |
| Alcohol | No | 165 (41.4%) |
| Yes | 234 (58.6%) | |
| Coffee | No | 108 (27.1%) |
| Yes | 291 (72.9%) | |
| Energy Drinks | No | 382 (95.7%) |
| Yes | 17 (4.3%) |
| Variable | Value 1 |
|---|---|
| DASS stress | 26 [18–32] |
| DASS anxiety | 12 [8–20] |
| DASS depression | 20 [14–30] |
| Cyclothymic (TEMPS-A) | 0.58 [0.75–0.29] |
| Depressive (TEMPS-A) | 0.44 [0.22–0.67] |
| Irritable (TEMPS-A) | 0.13 [0–0.25] |
| Hyperthymic (TEMPS-A) | 0.5 [0.15–0.63] |
| Anxious (TEMPS-A) | 0.67 [0.33–1] |
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | — | |||||||||||||||||||||||||||||||
| 2. Gender | 0.062 | — | ||||||||||||||||||||||||||||||
| 3. Relationship | 0.093 | −0.070 | — | |||||||||||||||||||||||||||||
| 4. Academic year | 0.836 | *** | 0.031 | 0.072 | — | |||||||||||||||||||||||||||
| 5. Drugs | 0.182 | *** | −0.035 | −0.042 | 0.160 | ** | — | |||||||||||||||||||||||||
| 6. Smoking | 0.066 | 0.145 | ** | −0.005 | 0.032 | 0.049 | — | |||||||||||||||||||||||||
| 7. Drinking coffee | 0.067 | 0.004 | 0.136 | ** | 0.069 | −0.090 | 0.192 | ** | — | |||||||||||||||||||||||
| 8. Consuming energy drink | −0.058 | 0.006 | 0.074 | −0.034 | 0.037 | 0.001 | 0.073 | — | ||||||||||||||||||||||||
| 9. GPA | −0.107 | * | −0.164 | ** | 0.037 | 0.033 | −0.005 | −0.001 | 0.027 | −0.040 | — | |||||||||||||||||||||
| 10. MHC–SF | −0.094 | 0.101 | * | 0.083 | −0.059 | −0.244 | *** | −0.050 | 0.002 | −0.032 | 0.051 | — | ||||||||||||||||||||
| 11. DASS-21 Stress | 0.056 | −0.221 | *** | −0.001 | 0.015 | 0.264 | *** | 0.079 | 0.036 | 0.033 | −0.025 | −0.480 | ** | — | ||||||||||||||||||
| 12. DASS-21 Anxiety | −0.068 | −0.253 | *** | 0.061 | −0.088 | 0.228 | *** | 0.056 | −0.026 | 0.030 | 0.006 | −0.416 | ** | 0.661 | ** | — | ||||||||||||||||
| 13. DASS-21 Depression | 0.082 | −0.121 | * | −0.047 | 0.062 | 0.320 | *** | 0.041 | −0.039 | 0.031 | −0.082 | −0.651 | ** | 0.696 | ** | 0.620 | ** | — | ||||||||||||||
| 14. Cyclothymic (TEMPS-A) | −0.132 | ** | −0.165 | ** | −0.022 | −0.182 | ** | 0.068 | 0.157 | ** | −0.008 | 0.037 | −0.132 | ** | −0.408 | ** | 0.444 | ** | 0.423 | ** | 0.493 | ** | — | |||||||||
| 15. Depressive (TEMPS-A) | 0.010 | −0.083 | −0.057 | 0.010 | 0.161 | ** | 0.035 | 0.038 | 0.050 | −0.076 | −0.570 | ** | 0.518 | ** | 0.423 | ** | 0.564 | ** | 0.401 | ** | — | |||||||||||
| 16. Irritable (TEMPS-A) | −0.085 | 0.023 | 0.071 | −0.085 | 0.007 | 0.203 | *** | 0.082 | 0.052 | −0.084 | −0.159 | ** | 0.270 | ** | 0.167 | ** | 0.145 | ** | 0.243 | ** | 0.297 | ** | — | |||||||||
| 17. Hyperthymic (TEMPS-A) | −0.039 | 0.105 | * | −0.015 | −0.093 | −0.027 | 0.146 | ** | −0.042 | 0.022 | −0.095 | 0.275 | ** | −0.069 | −0.115 | * | −0.242 | ** | 0.062 | −0.204 | ** | 0.146 | ** | — | ||||||||
| 18. Anxious (TEMPS-A) | −0.135 | ** | −0.249 | ** | 0.145 | ** | −0.156 | ** | −0.002 | −0.004 | −0.065 | −0.004 | 0.005 | −0.183 | ** | 0.225 | ** | 0.300 | ** | 0.187 | ** | 0.326 | ** | 0.236 | ** | 0.079 | 0.000 | — | ||||
| B | S.E. | p | OR | 95% CI OR | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age | −0.14 | 0.05 | 0.009 | 0.867 | 0.78 | 0.96 |
| Gender (Female) | 0.20 | 0.32 | 0.53 | 1.218 | 0.65 | 2.27 |
| Relationship (Partnered) | −0.44 | 0.29 | 0.12 | 0.641 | 0.37 | 1.12 |
| Academic year | 0.10 | 0.12 | 0.38 | 1.107 | 0.88 | 1.39 |
| Takes drugs (Yes) | 0.24 | 0.54 | 0.66 | 1.27 | 0.44 | 3.63 |
| Smoke (Yes) | −0.24 | 0.39 | 0.54 | 0.789 | 0.37 | 1.69 |
| Drink alcohol (Yes) | −0.02 | 0.29 | 0.94 | 0.978 | 0.56 | 1.72 |
| Drink coffee (Yes) | 0.05 | 0.32 | 0.88 | 1.05 | 0.56 | 1.97 |
| Consume ED (Yes) | 0.30 | 0.62 | 0.62 | 1.356 | 0.40 | 4.60 |
| GPA | −0.01 | 0.02 | 0.62 | 0.988 | 0.94 | 1.04 |
| DASS-21 Stress | 0.004 | 0.02 | 0.87 | 1.004 | 0.96 | 1.05 |
| DASS-21 Anxiety | 0.003 | 0.02 | 0.91 | 1.003 | 0.96 | 1.05 |
| DASS-21 Depression | −0.08 | 0.02 | <0.001 | 0.925 | 0.89 | 0.96 |
| TEMPS-A Cyclothymic | −1.36 | 0.62 | 0.03 | 0.256 | 0.08 | 0.86 |
| TEMPS-A Depressive | −2.19 | 0.58 | <0.001 | 0.112 | 0.04 | 0.35 |
| TEMPS-A Irritable | 0.12 | 0.72 | 0.87 | 1.123 | 0.27 | 4.60 |
| TEMPS-A Hyperthymic | 0.93 | 0.54 | 0.08 | 2.547 | 0.88 | 7.36 |
| TEMPS-A Anxious | −0.03 | 0.41 | 0.94 | 0.972 | 0.44 | 2.16 |
| Constant | 6.74 | 1.72 | 0 | 847.293 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Concerto, C.; Rodolico, A.; La Rosa, V.L.; Aiello, B.; Martinez, M.; Stuto, S.; Infortuna, C.; Fusar-Poli, L.; Signorelli, M.S.; Commodari, E.; et al. Flourishing or Languishing? Predictors of Positive Mental Health in Medical Students during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 15814. https://doi.org/10.3390/ijerph192315814
Concerto C, Rodolico A, La Rosa VL, Aiello B, Martinez M, Stuto S, Infortuna C, Fusar-Poli L, Signorelli MS, Commodari E, et al. Flourishing or Languishing? Predictors of Positive Mental Health in Medical Students during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(23):15814. https://doi.org/10.3390/ijerph192315814
Chicago/Turabian StyleConcerto, Carmen, Alessandro Rodolico, Valentina Lucia La Rosa, Barbara Aiello, Miriam Martinez, Sebastiano Stuto, Carmenrita Infortuna, Laura Fusar-Poli, Maria Salvina Signorelli, Elena Commodari, and et al. 2022. "Flourishing or Languishing? Predictors of Positive Mental Health in Medical Students during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 23: 15814. https://doi.org/10.3390/ijerph192315814
APA StyleConcerto, C., Rodolico, A., La Rosa, V. L., Aiello, B., Martinez, M., Stuto, S., Infortuna, C., Fusar-Poli, L., Signorelli, M. S., Commodari, E., Battaglia, F., & Aguglia, E. (2022). Flourishing or Languishing? Predictors of Positive Mental Health in Medical Students during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(23), 15814. https://doi.org/10.3390/ijerph192315814











