Abstract
Background: The aim of this study was to examine the attitudes, fears, and anxiety level of nursing students faced with a critical clinical simulation (cardiopulmonary reanimation) with and without personal protective equipment (PPE). Methods: A pilot before–after study as conducted from 21 to 25 June 2021, with 24 students registered in the nursing degree of the Faculty of Health Sciences of the Castilla-La Mancha University (UCLM) in the city of Talavera de la Reina (Toledo, Spain). From 520 possible participants, only 24 were selected according to the exclusion and inclusion criteria. The STAI Manual for the State-Trait Anxiety Inventory, a self-evaluation questionnaire, was used to study trait STAI (basal anxiety), trait STAI before CPR, state STAI after CPR, total STAI before CPR, and total STAI after CPR as the main variables. A t-test was used to study the STAI variables according to sex and the physiological values related to the anxiety level of participants. An ANOVA statistical test was used to perform a data analysis of the STAI variables. Results: A total of 54.2% of participants (IC 95% 35.1–72.1) suffered from global anxiety before the cardiopulmonary reanimation maneuvers (CPR). The results of the STAI before CPR maneuvers showed significant differences according to gender in state anxiety (p = 0.04), with a higher level of anxiety in women (22.38 ± 7.69 vs. 15.82 ± 7.18). Conclusions: This study demonstrates different levels of anxiety in terms of gender suffered by nursing students in high-pressure environments, such as a CPR situation.
1. Introduction
Nursing education has frequently been linked to anxiety among undergraduate students [1,2,3]. Anxiety helps prepare an individual to respond and act appropriately to a situation [4,5], which is crucial in health-assistance settings. Anxiety has been detailed previously in other studies [6,7,8], especially among women [9,10].
Furthermore, the clinical training taking place during nursing education is more stressful than other theoretical subjects [1,11] and more stressful than other clinical practices among undergraduates in different health degrees. Particularly, anxiety among nursing students has a negative effect on their quality of life [2] and may cause them to drop out of their programs [3]. It is also well-known that negative emotions and feelings such as fear and anxiety can influence the learning process in nursing students [12,13,14]. High levels of anxiety, fear, and other feelings can make learning difficult [15] and even influence decision making [16,17]. Three important aspects can influence decision making: experience, knowledge, and the emotional, mental, and physical state of the student or nurse [18]. Incorrect decision making can stem from a lack of knowledge and/or learning [19] and even from sociodemographic variables such as sex and age [20].
Due to the COVID pandemic, the scenario for health professionals has only gotten worse [21], particularly for recent nurses and students in practice [22]. On the one hand, age, expertise, and concerns about infection risk increase the risk of suffering anxiety among frontline healthcare workers fighting COVID-19 [23], and on the other hand, a lack of PPE and fear of infection can increase the risk of anxiety among nursing students [21]. There is also a gender association: there is a higher anxiety level in female students than in males [2,24,25,26,27].
Given the fact that females comprise most of the undergraduates in nursing careers worldwide, gender can in part explain the focus on the high prevalence of anxiety studies in many publications [9,10,21].
There are many studies on the prevalence of anxiety during clinical simulations that resemble life situations [22,28], outlining those individuals who were subjected to the pressure of the intervention, the critical state of the patient, and the aspects related to the patient’s death [29,30,31]. With respect to the effect of wearing personal protective equipment on CPR quality during the pandemic, Rauch et al. [32] have recently published the results from a sample of providers from the prehospital emergency medical service. In that study, the authors did not find any effect of wearing PPE with respect to compression depth, release, or rate or number of effective compressions.
However, there is no literature about the impact of wearing a PPE (personal protective equipment) on state or trait anxiety during a clinical simulation.
Since stress and anxiety affect the decision-making and learning process [17], it is necessary to conduct studies that include the factor of wearing PPE during clinical simulations with nursing students in order to enable for them to work in the COVID scenario or for others that require the same level of biosecurity.
Thus, the aim of this study was to examine the attitudes, fears, and anxiety level that nursing students experience when faced with a critical clinical simulation (cardiopulmonary reanimation) with and without personal protective equipment.
2. Materials and Methods
2.1. Study Design
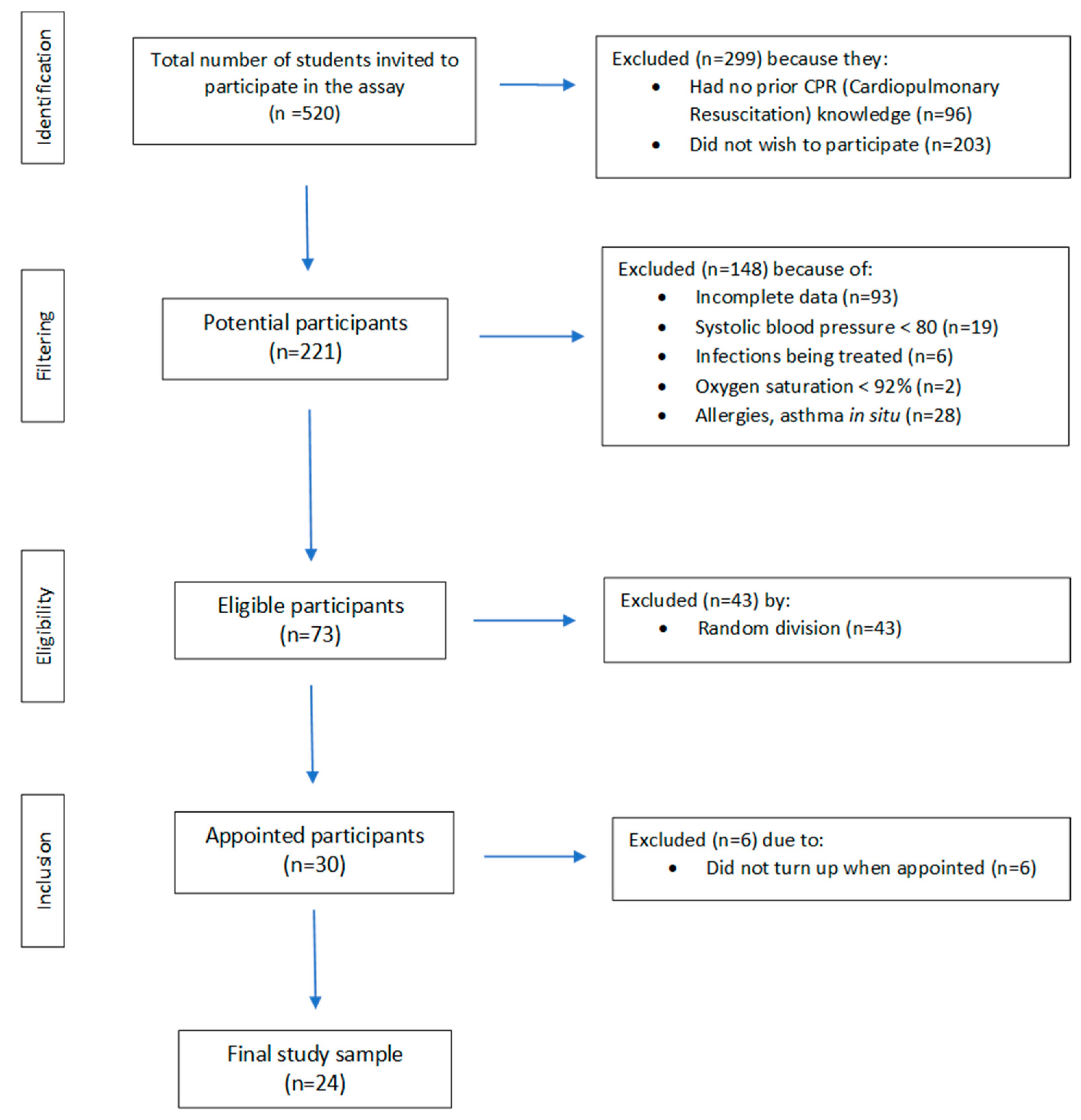
A pilot before–after study [22] was conducted from 21 to 25 June 2021, with 520 students registered in the nursing degree of the Faculty of Health Sciences of the Castilla-La Mancha University (UCLM) in the city of Talavera de la Reina (Toledo, Spain). Of 520 possible participants, only 73 were selected according to the inclusion criteria. Using random numbers generated by computer software XLSTAT ® BioMED 14.4.0 (Microsoft Inc., Redmond, WA, USA), we appointed a final sample of 24 participants (Figure 1).
Figure 1.
Flow chart of the selection of participants for this study.
Before performing the CPR simulation, all participants had received a CPR seminar with dummies. All selected participants were aged between 18 and 34. They all had basic knowledge of the maneuvers, according to the American Heart Association or European Resuscitation Council training.
2.2. Population
The eligible population were nursing students with accredited knowledge in basic cardiopulmonary resuscitation. We performed a random selection of subjects who showed interest in participating in the study and did not present any of the exclusion criteria. The exclusion criteria were similar to those considered in previous studies [28] (major surgery in the last 30 days; blood sugar levels < 65 mg/dL; electrocardiogram with alterations; resting heart rate of >120 beats/minute (bpm) or <35 bpm; body mass index > 40 kg/m2; temperature > 38 °C; systolic or diastolic blood pressure > 160 or <95 mmHg or systolic blood pressure < 80 mmHg, respectively; any type of functional disorder hindering cardiopulmonary resuscitation maneuvers; oxygen saturation < 92%; acute-phase skin diseases or systemic immunological diseases; severe visual or hearing impairment or epilepsy; diagnosed infections treated while the study was conducted).
The sample size was 24 subjects, 11 (45.8%) men and 13 (54.2%) women; it was calculated as accepting a 0.05 alpha risk. All participants signed the informed consent and carried out the study.
2.3. Study Protocol
In this pilot study, each subject carried out two interventions, with 24 h resting time in between: one intervention without the use of personal protective equipment (PPE) and another with complete PPE (that is, protective equipment for infection control including FFP2 mask, coverall, clothing, doble gloves, protective glasses, gown). To eliminate any compliance bias, all subjects had the same probability of being included in any group in the first intervention, as a randomization sequence was generated using random numbers according to the gender stratification created by the computer with Microsoft Excel® version 14.4.0. (Microsoft Inc., Redmond, WA, USA).
First, all students completed a State Trait Anxiety Inventory (STAI) (State Anxiety-SA and Trait Anxiety-TA) questionnaire and a “Pre-feelings and emotions” questionnaire thirty minutes before the performance of CPR. They continued on to the different scenarios in which they performed a test for 10 min with a high-quality CPR simulator: Real CPR Help software installed in an R Series monitor-defibrillator (ZOLL Medical Corporation, Chelmsford, MA, USA) and CPR-D-padz® defibrillation electrodes (ZOLL Medical Corporation, Chelmsford, MA, USA) (Real CPR Help® technology provides real-time feedback about the depth and frequency of CPR while it is applied, which provides guidance on improving the quality of the CPR).
At the end of the performance, the same State Trait Anxiety Inventory (STAI) and “Post-feelings and emotions” questionnaires were completed.
At no time was it reported that the students had to complete the questionnaires after completing the CPR test to avoid bias.
The State Trait Anxiety Inventory (STAI) is a self-administered questionnaire, validated for the Spanish population, and it has a Cronbach’s alpha of 0.93 for TA and 0.92 for SA [33]. This instrument measures anxiety in healthy adults. It has two scales: state anxiety (SA, reflects temporary anxiety about a particular event) and trait anxiety (TA, reflects anxious propensity that characterizes individuals), with 20 questions each. The questionnaire provides a numerical value for TA and another for SA [28]. The total STAI is the sum of SA and TA.
In addition, “Pre- and Post-feelings and emotions” questionnaires were anonymous, non-validated, and based on the model presented by Miquel Perez et al. [34] and Romo-Barrientos et al. [9]. These instruments were administered to characterize students’ feelings and emotions regarding the CPR maneuvers with/without PPE.
The “Pre-feelings and emotions” questionnaire consisted of 12 questions, and the “Post-feelings and emotions” questionnaire consisted of 16 questions (adding four new questions related to students’ satisfaction and emotional experience performing the CPR) (Supplementary Materials).
2.4. Data Analysis
Data were checked for meeting the normality condition with the Shapiro–Wilk test. Categorical variables were described using absolute frequencies with a 95% confidence interval (IC 95%), considering descriptive statistics, means, and standard deviation (SD). In the descriptive and inferential statistical analysis, the parameters were used according to the scale of the variable. The quantitative variables herein contemplated were as follows: trait STAI (basal anxiety), trait STAI before CPR, state STAI after CPR, total STAI before CPR, and total STAI after CPR.
With a t-test, we studied the STAI variables according to sex and the physiological values related to the anxiety level of participants. An ANOVA statistical test was used to perform a data analysis of the STAI variables according to the experimental group. A 95% confidence level was established. The SPSS statistical package, v. 24 (SPSS Inc., Chicago, IL, USA) and XLSTAT ® BioMED software were employed.
2.5. Ethical Considerations
The participants were informed about the general objectives of the study and gave their informed consent. The study was approved by the Clinical Research Ethics Committee of Talavera de la Reina (Toledo) with number 178013/113. Details of the study design, statistical analysis plan, and baseline data are available online (doi.org/10.1186/ISRCTN10222040 (accessed on 5 October 2022)).
3. Results
We included 24 subjects, of whom 54.2% were women and 45.8% were men, with a mean age of 22.12 years (SD 3.84). All participants belonged to the nursing degree according to the academic course. A total of 25% of the sample were students from the first course, 25% were from the second course, and 50% were from the fourth course (Figure 1).
Regarding the STAI questionnaire, in the first phase (PRE), the score for the STAI-TA was 22.46 ± 8.57 points. The STAI-SA decreased from the first phase (19.40 ± 8.03 points) to the second phase (16.04 ± 8.51 points) without statistically significant differences (p > 0.05). We found significant differences between STAI-state anxiety among males and females, where female participants showed a higher level of anxiety (p = 0.04).
Regarding to the STAI-SA, we found significant differences between the first phase (PRE) and the second phase (POST) in the female group (p = 0.016).
When studied with regard to PPE, there were no significant differences (Table 1).

Table 1.
Anxiety (pre- and post-intervention) categorized by gender and by personal protective equipment use.
According to Romo-Barrientos et al. [9], Spielberger et al. [33], Arraez-Aybar et al. [35], and Casado et al. [36], we consider that a subject suffers from global anxiety when their trait anxiety minus state anxiety is less than six points (TA-SA > 6). Therefore, in the sample, 54.2% (IC 95% 35.1–72.1) of participants suffered global anxiety before the CPR, and 62.5% (IC 95% 42.7–78.8) suffered global anxiety after the CPR, without significant differences. This means a relative increase of 8.3 points in percentage.
The results obtained from the questionnaire indicate that the main thoughts and feelings regarding the cardiopulmonary reanimation were uncertainty and curiosity, at 62.5% (n: 15) and 58.3% (n: 14), respectively. These were described with a frequency higher than other feelings, such as fear or anxiety.
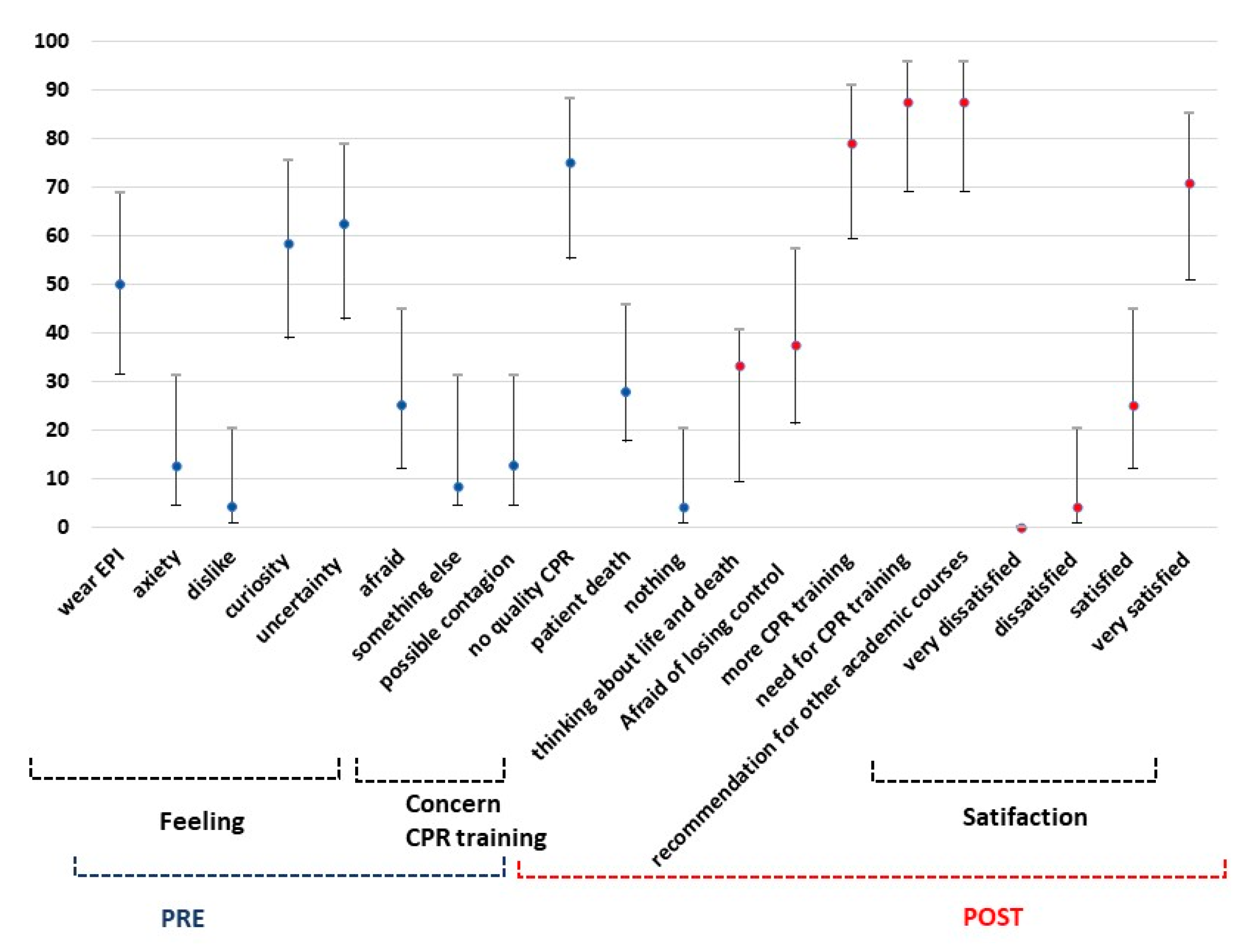
According to the question “What is your main concern about performing a CPR with PPE?”, the students answered that their greatest concern was not performing a quality CPR (75%, n: 18) and the patient’s death (45.8%, n: 11) vs. a possible contagion (12.5%, n: 3) (Figure 2), without significant differences (p > 0.05). When we studied differences according to gender, we found a significant difference for the answer uncertainty, with more males than females acknowledging this feeling (p = 0.035).
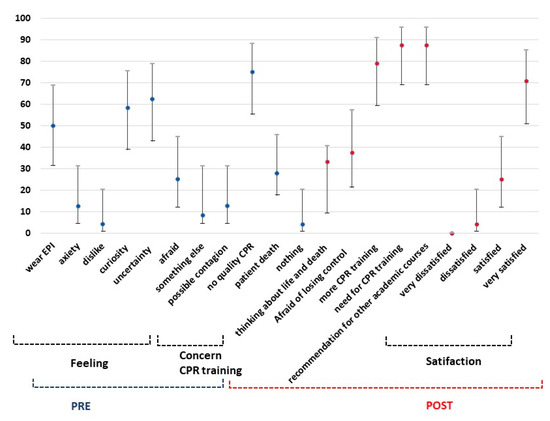
Figure 2.
Prevalence of students’ thoughts and feelings (with IC 95%) regarding to the cardiopulmonary reanimation.
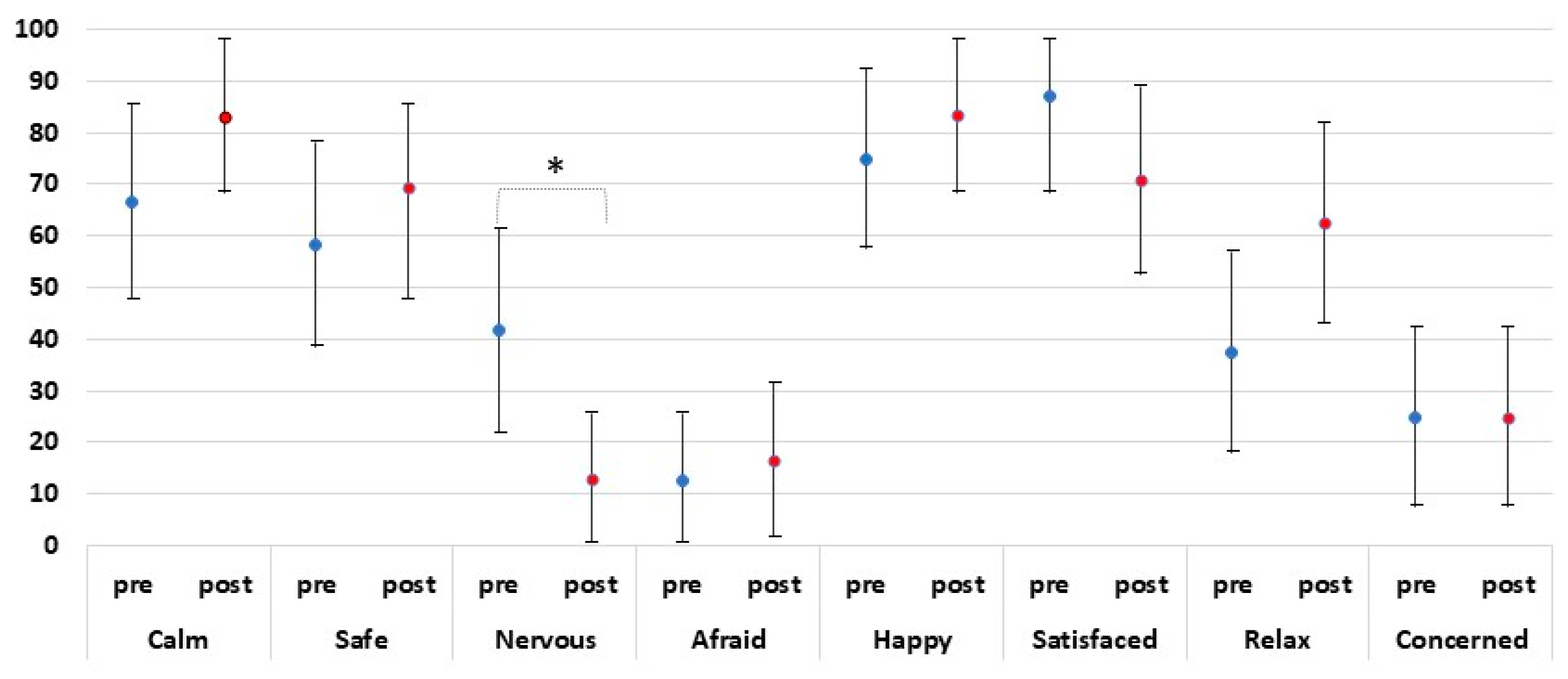
In general, during the first phase (PRE), the students were “calm” (n: 16; 66.7%) and felt “safety” (n: 14; 58.3%) more than “nervous” (n: 13; 41.7%), “worried” (n: 6, 25.0%), or “afraid” (n: 3, 12.5%).
After the intervention (POST), there was an increase in the average of “calm”, “safety”, and “relaxed” (n: 20, 83.0%; n: 16, 69.6%; n: 15, 62.5%, respectively). The students were less “nervous” (n: 3; 65.2%) and felt a slight increase in being “afraid” (16.7%, n: 4) compared with the feelings perceived in the first phase. Nevertheless, 70.8% were satisfied with themselves (n: 17) (Figure 3).
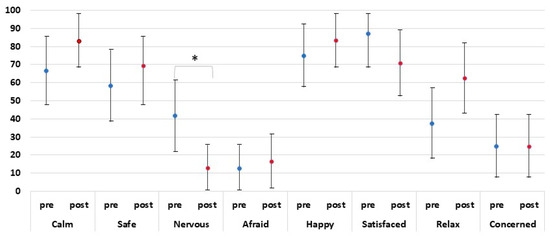
Figure 3.
Comparison among self-perceived feelings pre- and post-CPR (IC 95%). * Statistically significant differences (p < 0.01 before vs. after) are shown.
Regarding the comparison among the self-perceived feelings questionnaire PRE- and POST-intervention, there were no statistically significant differences (p > 0.05) in any variable except nervousness (p < 0.01 before vs. after) (Figure 3).
The perception of the participants towards performing the CPR maneuvers was the main outcome of this study. In the first phase, students were asked about the feelings they experience when performing CPR under biological risk conditions or during a pandemic, in which case the answers were “uncertainty” and “curiosity” (62.50% and 58.30%, respectively) and facing “anxiety” and “dislike” (12.50% and 4.20%, respectively) (Figure 2).
When performing the maneuvers with the PPE kit, the participants worried about the patient’s death (27.90%) and not performing a quality CPR (75%), whereas a possible contagion was only a worry of 12.5% of the sample, considering that 50% of the participants had worn a PPE kit before this study (Figure 2).
Regarding the evaluation of training in the second phase, the students answered that they needed more training to improve their proper technique and concentration to complete a quality CPR (79.2%, n: 19). A percentage of 87.5% (n: 21) considered that it was necessary to carry out more training in CPR throughout the nursing degree, and 87.5% recommended this training activity for other courses (n: 21) (Figure 2).
The score given by the students in this training was 8.62 ± 1.04 points over ten points, and 95.8% (n: 23) were satisfied or very satisfied with the training activity.
4. Discussion
This study attempted to examine the attitudes, fears, and anxiety level that nursing students experience when faced with a critical clinical simulation (cardiopulmonary resuscitation) with and without a personal protective equipment (PPE). The literature shows that simulation scenarios facilitate objective teaching models, which would otherwise be limited by ethical, social, administrative, and legal parameters [37]. Several studies have described a lack of confidence, a transfer of experienced emotions to the simulation environment, as well as a lack of evidence compared with traditional methods [38]. However, this is the first time that anxiety, emotions, and attitudes during a critical clinical simulation have been studied according to the context of the COVID pandemic, using a PPE kit.
The STAI questionnaire was found to be a useful tool in the evaluation of state and trait anxiety level. The results of the statistical analysis for the STAI before the CPR maneuvers showed significant differences by gender on state anxiety, with a higher level of anxiety in females before the CPR. This is consistent with studies in which differences between men and women have been observed in critical care residents in CPR simulation scenarios [39]; in extreme conditions, gender differences have been observed after CPR simulations, with a higher level of anxiety in women [28]. During the first wave of the COVID pandemic, an increase in anxiety in female health professionals was evidenced [40,41,42,43,44,45]. Concurrently, other studies with undergraduates have shown higher levels of trait anxiety in women [9,10].
In addition, we found that the female group showed a higher level of anxiety in the first phase of the simulation. These results raise the question as to whether the higher anxiety scores occurred before the CPR maneuvers. What is known is that the measurement of stress is related to a transient event, and that once it ends, anxiety values decrease quickly [46]. These data are consistent with our study. In addition, this prior anxiety can affect learning, decision making, and CPR execution, confirming studies that show that anxiety affects learning and decision making [12,14].
Our results suggest an increase in anxiety at the final phase due to the doubts of the participants about the real outcomes of their performance, as the feeling of being observed or the anticipatory anxiety is diminished, which coincides with recent findings [47].
The outcomes of this pilot study indicate that the main concern about the use of a PPE kit during a cardiopulmonary resuscitation is not only the patient’s death but also the quality of the maneuvers, relegating the fear of a possible contagion to a secondary place. Recently, other factors such as the effectiveness of time, the perception of a safe environment in contrast to the real context, or findings of making a mistake while being observed have been related to stress and anxiety during a CPR [48].
This pilot study also indicates that knowing how to perform CPR does not presume calm, comfort, or an ability to control state anxiety in critical situations. The psychological response of health professionals in emergency situations is a frequently discussed issue. It has been suggested that PPE use is a stressor for all response personnel; other authors suggest that the trait anxiety is most affected by using PPE. Dunbar’s works are the precedents that describe how the stable psychological traits of anxiety and the expression of anger mitigate against performance in using PPE [49].
Nursing education has traditionally been a female discipline [50], and this election depends on the gender roles and social factors [51]. Nursing studies currently have a higher percentage of female undergraduates, surprisingly, with statistical differences in stress by gender with worse results in women [52], which could affect the learning process and academic scores and self-esteem, even the decision-making process [53,54].
Recent studies have examined job stress-coping strategies among nurses. These results could be used to develop specific training in nursing students. Some of the most emotion-oriented coping strategies used by nurses include positive reappraisal [55], which demonstrates higher psychological competences and significantly better professional behavior and personality traits [56]. Positive reappraisal has demonstrated benefits in terms of psychological health [57] and, in general, females are more likely to use positive reappraisal [58]. We agree that specific emotional training when facing to a critical clinical scenario would improve the results in making decisions and also the performance of quality resuscitation maneuvers.
Finally, as strengths, this study has included a specific scenario with a PPE kit for COVID, which involved the complex use of resources and organization, and results are revealed that have not been published previously. Further, other clinical simulation studies have used different questionnaires to measure anxiety, such as Nursing Anxiety and Self-confidence with Clinical Decision-Making (NASC-CDM), although the most frequently used measure in these cases is the STAI, as a validated and effective tool for measuring self-perceived anxiety. In addition, we measured physiological variables that strengthen the results regarding the effects of anxiety. However, this preliminary study limits a generalization of findings owing to the small sample size. More studies with larger sample sizes that also consider additional variables, such as culture, socioeconomic level, and beliefs, are required to provide in-depth understanding.
One of the weaknesses of the study is the sample size, which was based on an opportunity sample, meeting the inclusion and exclusion criteria method.
5. Conclusions
This study has demonstrated the different levels of stress and anxiety in terms of gender that nursing students in high-pressure environments perceive, such as a CPR situation. Future stress-management interventions and training should be developed using positive coping strategies to enhance supportive working environments to enable nurses to provide better quality care to critical patients.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192315713/s1.
Author Contributions
Conceptualization, A.M.-M. and J.L.M.-C.; methodology, F.M.-R.; software, F.T.-F. and J.J.C.-Á.; validation, B.P.-L., F.M.-R., C.R.-B. and J.J.C.-Á.; formal analysis, C.D.-F. and C.R.-B.; investigation, F.M.-R.; resources, C.J.-S., A.V. and F.T.-F.; data curation, A.V. and C.J.-S.; writing—original draft preparation, C.M.-M.; writing—review and editing, A.M.-M., R.C.-S. and C.D.-F.; visualization, A.V.; supervision, C.M.-M. and A.V.; project administration, F.M.-R.; funding acquisition, J.L.M.-C. and R.C.-S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Clinical Research Ethics Committee of Talavera de la Reina (Toledo) (protocol code 178013/113 and date of approval 4 April 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
doi.org/10.1186/ISRCTN10222040 (accessed on 5 October 2022).
Acknowledgments
The authors would like to thank the students of health sciences for their participation in the study.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- John, B.; Al-Sawad, M. Perceived stress in clinical areas andemotional intelligence among baccalaureate nursing students. J. Indian Acad. Appl. Psychol. 2015, 41, 75–84. [Google Scholar]
- Sanad, H.M. Stress and Anxiety among Junior Nursing Students during the Initial Clinical Training: A Descriptive Study at College of Health Sciences, University of Bahrain. Am. J. Nurs. Res. 2019, 7, 995–999. [Google Scholar]
- Rafati, F.; Nouhi, E.; Sabzehvari, S.; Dehghan-Nayyeri, N. Iranian Nursing Students’ Experience of Stressors in Their First Clinical Experience. J. Prof. Nurs. 2017, 33, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Gilbertson, A.D. Sex bias in diagnosis. Hosp. Community Psychiatry 1992, 43, 406–407. [Google Scholar] [CrossRef] [PubMed]
- De Benedittis, G. Neural mechanisms of hypnosis and meditation. J. Physiol. 2015, 109, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Derrick, K.; Green, T.; Wand, T. Assessing and responding to anxiety and panic in the Emergency Department. Australas. Emerg. Care 2019, 22, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Al-Ghareeb, A.; Cooper, S.; McKenna, L. Anxiety and clinical performance in simulated setting in undergraduate health professionals education: An integrative review. Clin. Simul. Nurs. 2017, 13, 478–491. [Google Scholar] [CrossRef]
- Kenny, G.; Bray, I.; Pontin, D.; Jeeries, R.; Albarran, J. A randomized controlled trial of student nurse performance of cardiopulmonary resuscitation in a simulated family-witnessed resuscitation scenario. Nurse Educ. Pract. 2017, 24, 21–26. [Google Scholar] [CrossRef]
- Romo Barrientos, C.; José Criado-Álvarez, J.; González-González, J.; Ubeda-Bañon, I.; Saiz-Sanchez, D.; Flores-Cuadrado, A.; Martín-Conty, J.L.; Viñuela, A.; Martinez-Marcos, A.; Mohedano-Moriano, A. Anxiety among Medical Students when Faced with the Practice of Anatomical Dissection. Anat. Sci. Educ. 2019, 12, 300–309. [Google Scholar] [CrossRef]
- Romo-Barrientos, C.; Viñuela, A.; Mohedano-Moriano, A.; Ubeda-Bañon, I.; Saiz-Sánchez, D.; Aceituno-Gómez, J.; Pavón, M.J.G.; Crespo, M.L.; Martín, D.T.; Martinez-Marcos, A.; et al. What emotions do physical therapy students feel during their first visit to the dissection room? Ann. Anat. 2022, 239, 151777. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J. Stress, stressors, and stress responses of student nurses in a government nursing school. Health Sci. J. 2013, 7, 424–435. [Google Scholar]
- Fitzgerald, A.; Konrad, S. Transition in learning during COVID-19: Student nurse anxiety, stress, and resource support. Nurs. Forum 2021, 56, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Tastan, S.; Iyigun, E.; Ayhan, H.; Hatipoglu, S. Experiences of Turkish undergraduate nursing students in the intensive care unit. Collegian 2015, 22, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.K.; Long, A.; Tseng, Y.S.; Huang, H.M.; You, J.H.; Chiang, C.Y. Undergraduate student nurses’ lived experiences of anxiety during their first clinical practicum: A phenomenological study. Nurse Educ. Today 2016, 37, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Hembree, R. Correlates, Causes, Effects, and Treatment of Test Anxiety. Rev. Educ. Res. 1988, 58, 47–77. [Google Scholar] [CrossRef]
- Ropeik, D. The consequences of fear. EMBO Rep. 2004, 5 (Suppl. S1), S56–S60. [Google Scholar] [CrossRef] [PubMed]
- Schlosser, T.; Dunning, D.; Fetchenhauer, D. What a Feeling: The Role of Immediate and Anticipated Emotions in Risky Decisions. J. Behav. Decis. Mak. 2013, 26, 13–30. [Google Scholar] [CrossRef]
- Tanner, C.A. Factors influcencing the diagnostic process. In Diagnostic Reasoninig in Nursing; Carnevali, D.L., Mitchell, P.H., Woods, N.F., Tarne, C.A., Eds.; Lippincott: Philadelphia, PA, USA, 1984. [Google Scholar]
- Carnevali, D.L. The diagnostiv reasoing process. In Diagnostic Reasoninig in Nursing; Carnevali, D.L., Mitchell, P.H., Woods, N.F., Tarne, C.A., Eds.; Lippincott: Philadelphia, PA, USA, 1984. [Google Scholar]
- Hamers, J.P.; Huijer Abu-Saad, H.; Halfens, R.J. Diagnostic process and decision making in nursing: A literature review. J. Prof. Nurs. 1994, 10, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Stavitsky, B.; Findling, Y.; Ereli, A.; Hendel, T. Anxiety and coping strategies among nursing students during the COVID pandemic. Nurse Educ. Pract. 2020, 46, 102809. [Google Scholar] [CrossRef] [PubMed]
- Mauriz, E.; Caloca-Amber, S.; Córdoba-Murga, L.; Vázquez-Casares, A.M. Effect of Psychophysiological Stress and Socio-Emotional Competencies on the Clinical Performance of Nursing Students during a Simulation Practice. Int. J. Environ. Res. Public Health 2021, 18, 5448. [Google Scholar] [CrossRef] [PubMed]
- Th’Ng, F.; Rao, K.A.; Ge, L.; Mao, D.; Neo, H.N.; De Molina, J.A.; Seow, E. A One-Year Longitudinal Study: Changes in Depression and Anxiety in Frontline Emergency Department Healthcare Workers in the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 11228. [Google Scholar] [CrossRef] [PubMed]
- McLean, C.P.; Asnaani, A.; Litz, B.T.; Hofmann, S.G. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J. Psychiatr. Res. 2011, 45, 1027–1035. [Google Scholar] [CrossRef] [PubMed]
- Lun, K.W.; Chan, C.K.; Ip, P.K.; Ma, S.Y.; Tsai, W.W.; Wong, C.S.; Wong, C.H.; Wong, T.W.; Yan, D. Depression and anxiety among university students in Hong Kong. Hong Kong Med. J. 2018, 24, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Miron, J.; Goldberg, X.; López-Sola, C.; Nadal, R.; Armario, A.; Andero, R.; Giraldo, J.; Ortiz, J.; Cardoner, N.; Palao, D. Perceived stress, anxiety and depression among undergraduate Students: An online survey study. J. Depress. Anxiety 2019, 8, 1–5. [Google Scholar]
- Quek, T.T.-C.; Tam, W.W.-S.; Tran, B.X.; Zhang, M.; Ho, C.S.-H. The Global Prevalence of Anxiety among Medical Students: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 2735. [Google Scholar] [CrossRef]
- Martin-Conty, J.L.; Martin-Rodríguez, F.; Criado-Álvarez, J.J.; Romo Barrientos, C.; Maestre-Miquel, C.; Viñuela, A.; Polonio-López Durantez-Fernández, C.; Marcos-Tejedor, F.; Mohedano-Moriano, A. Do Rescuers’ Physiological Responses and Anxiety Influence Quality Resuscitation under Extreme Temperatures? Int. J. Environ. Res. Public Health 2020, 17, 4241. [Google Scholar] [CrossRef] [PubMed]
- Munroe, B.; Curtis, K.; Murphy, M.; Strachan, L.; Buckley, T. HIRAID: An evidence-informed emergency nursing assessment framework. Australas. Emerg. Nurs. J. 2015, 18, 83–97. [Google Scholar] [CrossRef] [PubMed]
- Larsen, T.; Beier-Holgersen, R.; Østergaard, D.; Dieckmann, P. Training residents to lead emergency teams: A qualitative review of barriers, challenges and learning goals. Heliyon 2018, 4, e01037. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.; Barnett, M. Aspects of caring for dying patients which cause anxiety to first year student nurses. Int. J. Palliat. Nurs. 2005, 11, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Rauch, S.; van Veelen, M.J.; Oberhammer, R.; Dal Cappello, T.; Roveri, G.; Gruber, E.; Strapazzon, G. Effect of Wearing Personal Protective Equipment (PPE) on CPR Quality in Times of the COVID-19 Pandemic-A Simulation, Randomised Crossover Trial. J. Clin. Med. 2021, 10, 1728. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.E. STAI Cuestionario de Ansiedad Estado-Rasgo, 6th ed.; TEA Ediciones: Madrid, Spain, 2002. [Google Scholar]
- Miguel Pérez, M.; Porta-Riba, N.; Ortiz-Sagristà, J.C.; Martínez, A.; Götzens-García, V. Human anatomy: Reactions of first year medical students to the dissection room. Educ. Méd. 2007, 10, 105–113. [Google Scholar]
- Arráez-Aybar, L.A.; Castaño-Collado, G.; Casado-Morales, M.I. Dissection from the Spanish anatomist’s perspective: Aims, attitudes, and related aspects. Anat. Rec. 2004, 281, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Casado, M.I.; Castaño, G.; Arráez-Aybar, L.A. Audiovisual material as educational innovation strategy to reduce anxiety response in students of human anatomy. Adv. Health Sci. Educ. Theory Pract. 2012, 17, 431–440. [Google Scholar] [CrossRef]
- Hernández Ruipérez, T.; Adánez Martínez, M.G.; Díaz Agea, J.L.; García Pérez, B.; Leal Costa, C. Diseño y validación de un modelo pedagógico basado en simulación clínica dirigido a la formación de enfermería en el sistema de triaje estadounidense Emergency Severity Index. Emergencias 2015, 27, 155–160. [Google Scholar] [PubMed]
- Weidman, E.K.; Bell, G.; Walsh, D.; Small, S.; Edelson, D.P. Assessing the impact of immersive simulation on clinical performance during actual in-hospital cardiac arrest with CPR-sensing technology: A randomized feasibility study. Resuscitation 2010, 81, 1556–1561. [Google Scholar] [CrossRef]
- Bauer, C.; Rimmelé, T.; Duclos, A.; Prieto, N.; Cejka, J.-C.; Carry, P.-Y.; Grousson, S.; Friggeri, A.; Secco, J.; Bui-Xuan, B.; et al. Anxiety and stress among anaesthesiology and critical care residents during high-fidelity simulation sessions. Anaesth. Crit. Care Pain Med. 2016, 35, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Cléophat, J.E.; Simon, P.; Chiniara, G.; St-Pierre, L.; Ahossi, E.; Dogba, M.J.; Chénier, C.; Dubuc, E.; Landry, C.; Vonarx, N.; et al. How anxious were Quebec healthcare professionals during the first wave of the COVID-19 pandemic? A web-based cross-sectional survey. Work 2021, 70, 701–712. [Google Scholar] [CrossRef] [PubMed]
- Milgrom, Y.; Tal, Y.; Finestone, A.S. Comparison of hospital worker anxiety in COVID-19 treating and non-treating hospitals in the same city during theCOVID-19 pandemic. Isr. J. Health Policy Res. 2020, 9, 55. [Google Scholar] [CrossRef]
- Giusti, E.M.; Pedroli, E.; D’Aniello, G.E.; Badiale, C.S.; Pietrabissa, G.; Manna, C.; Badiale, M.S.; Riva, G.; Castelnuovo, G.; Molinari, E. The Psychological Impact of the COVID-19 Outbreak on Health Professionals: A Cross-Sectional Study. Front. Psychol. 2020, 11, 1684. [Google Scholar] [CrossRef] [PubMed]
- Hacimusalar, Y.; Kahve, A.C.; Yasar, A.B.; Aydin, M.S. Anxiety and hopelessness levels in COVID-19 pandemic: A comparative study of healthcare professionals and other community sample in Turkey. J. Psychiatr. Res. 2020, 129, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Di Tella, M.; Romeo, A.; Benfante, A.; Castelli, L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J. Eval. Clin. Pract. 2020, 26, 1583–1587. [Google Scholar] [CrossRef] [PubMed]
- Bahadir-Yilmaz, E.; Yüksel, A. State anxiety levels of nurses providing care to patients with COVID-19 in Turkey. Perspect. Psychiatr. Care 2021, 57, 1088–1094. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Ayuso, D.; Fernández-Ayuso, R.; Del-Campo-Cazallas, C.; Pérez-Olmo, J.L.; Matías-Pompa, B.; Fernández-Carnero, J.; Calvo-Lobo, C. The Modification of Vital Signs According to Nursing Students’ Experiences Undergoing Cardiopulmonary Resuscitation Training via High-Fidelity Simulation: Quasi-Experimental Study. JMIR Serious Games 2018, 6, e11061. [Google Scholar] [CrossRef]
- Megel, M.E.; Black, J.; Clark, L.; Carstens, P.; Jenkins, L.D.; Promes, J.; Snelling, M.; Zander, K.E.; Bremer, A.; Goodman, T. Effect of High-Fidelity Simulation on Pediatric Nursing Students’ Anxiety. Clin. Simul. Nurs. 2012, 8, e419–e428. [Google Scholar] [CrossRef]
- Khadivzadeh, T.; Erfanian, F. The effects of simulated patients and simulated gynecologic models on student anxiety in providing IUD services. Simul. Healthc. 2012, 7, 282–287. [Google Scholar] [CrossRef]
- Dunbar, E. The Role of Psychological stress and Prior experience in the use of Personal Protective Equipment. J. Saf. Res. 1993, 24, 181–187. [Google Scholar] [CrossRef]
- Okrainec, G.D. Perceptions of nursing education held by male nursing students. West. J. Nurs. Res. 1994, 16, 94–107. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Jung, S.Y.; Jang, S. Who enters nursing schools and why do they choose nursing? A comparison with female non-nursing students using longitudinal data. Nurse Educ. Today 2010, 30, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Vega Martínez, M.C.; Rodriguez García, B.; Arenal Gota, T. Estresores académicos percibidos por estudiantes del grado de enfermería en una universidad española. Rev. Enfermería CyL 2019, 11, 16. [Google Scholar]
- Chust-Hernández, P.; Castellano-Rioja, E.; Fernández-García, D.; Chust-Torrent, J.I. Ansiedad ante los exámenes en estudiantes de Enfermería: Factores de riesgo emocionales y de sueño. Ansiedad Y Estrés 2019, 25, 125–131. [Google Scholar] [CrossRef]
- Chávez Parillo, J.R.; Peralta Gómez, R.Y. Estrés académico y autoestima en estudiantes de enfermería, Arequipa-Perú. Rev. De Cienc. Soc. (RCS) 2019, 25, 384–399. [Google Scholar]
- Isa, K.Q.; Ibrahim, M.A.; Abdul-Manan, H.H.; Mohd-Salleh, Z.H.; Abdul-Mumin, K.H.; Rahman, H.A. Strategies used to cope with stress by emergency and critical care nurses. Br. J. Nurs. 2019, 28, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Shirey, M.R. Stress and coping in nurse managers: Two decades of research. Nurs. Econ. 2006, 24, 193–203. [Google Scholar]
- Shiota, M.N.; Levenson, R.W. Turn down the volume or change the channel? Emotional effects of detached versus positive reappraisal. J. Pers. Soc. Psychol. 2012, 103, 416–429. [Google Scholar] [CrossRef] [PubMed]
- Deklava, L.; Circenis, K.; Millere, I. Stress mechanisms and professional burnout among Latvian nurses. Procedia: Soc. Behav. Sci. 2014, 159, 261–267. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).