International Survey of Specialist Fetal Alcohol Spectrum Disorder Diagnostic Clinics: Comparison of Diagnostic Approach and Considerations Regarding the Potential for Unification
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Questionnaire
2.3. Data Analysis
3. Results
3.1. Clinic Demographics and Criteria Usage
3.2. Barriers to a Unified Diagnostic Approach
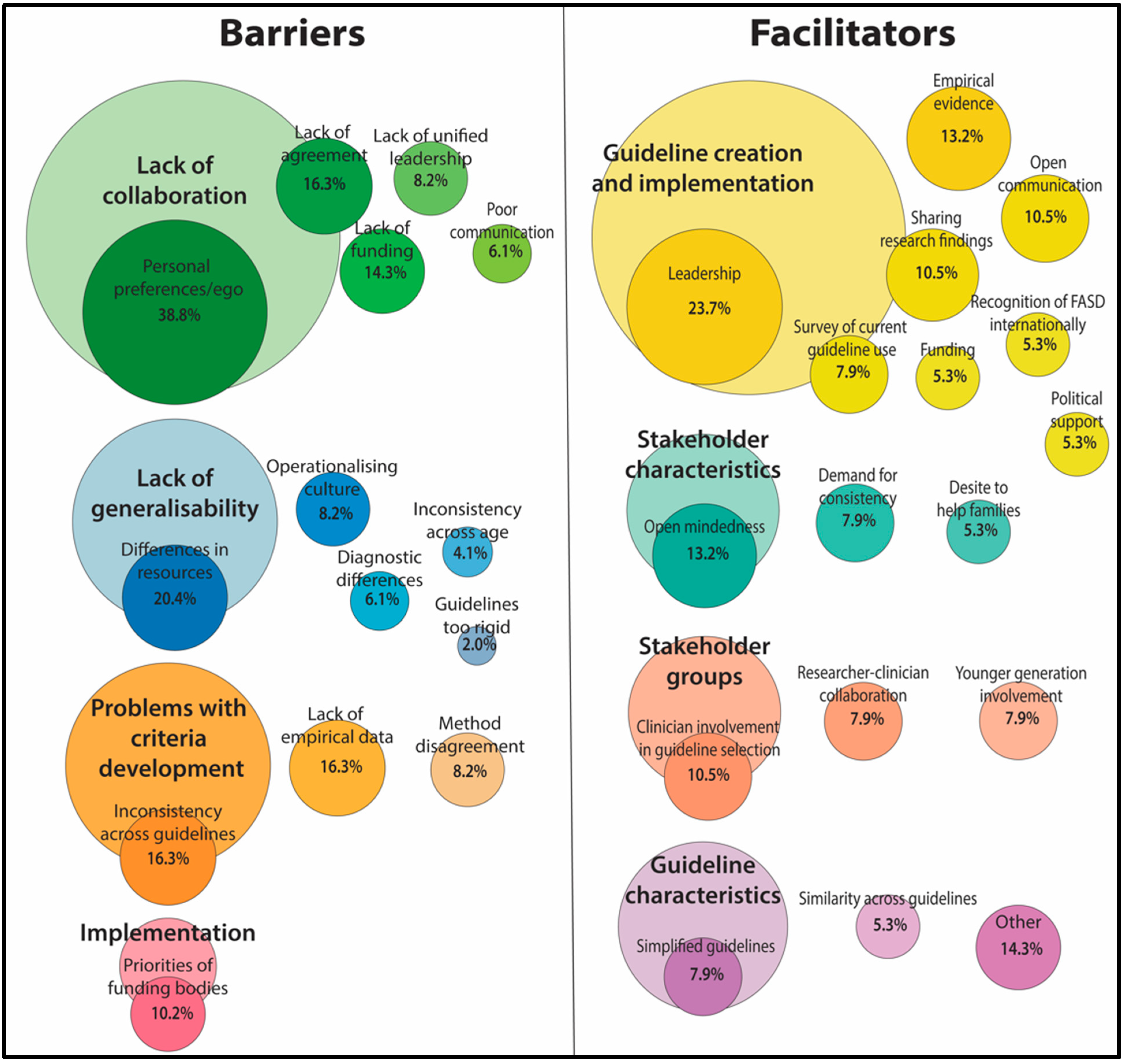
3.3. Facilitators to a Unified Diagnostic Approach
4. Discussion
4.1. Diagnostic Criteria
4.2. Barriers to a Unified Diagnostic Approach
4.3. Facilitators to a Unified Diagnostic Approach
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Clinic Country | Australian Guidelines (Bower & Elliott, 2016) | Canadian Diagnostic Guidelines (Chudley et al., 2005) | Revised Canadian Diagnostic Guideline (Cook et al., 2016) | Revised United States Institute of Medicine Criteria (Hoyme et al., 2005) | 4-Digit Diagnostic Code (Astley, 2004) | Centers for Disease Control and Prevention (Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis, 2004) | Emory Clinic Diagnostic Guidelines | Other | Total Number of Guidelines |
|---|---|---|---|---|---|---|---|---|---|
| AUS | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 2 |
| CAN | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 2 |
| OTH | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 2 |
| OTH | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 2 |
| NZ | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 3 |
| NZ | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 2 |
| UK | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 2 |
| UK | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 4 |
| UK | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 4 |
| USA | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 3 |
| USA | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| USA | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 2 |
| USA | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 2 |
| USA | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 3 |
| USA | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 3 |
| USA | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 2 |
| USA | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 3 |
References
- Cook, J.L.; Green, C.R.; Lilley, C.M.; Anderson, S.M.; Baldwin, M.E.; Chudley, A.E.; Conry, J.L.; LeBlanc, N.; Loock, C.A.; Lutke, J.; et al. Fetal alcohol spectrum disorder: A guideline for diagnosis across the lifespan. CMAJ 2016, 188, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Banerji, A.; Shah, C. Ten-year experience of fetal alcohol spectrum disorder; diagnostic and resource challenges in Indigenous children. Paediatr. Child Health 2017, 22, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Brownell, M.; Enns, J.E.; Hanlon-Dearman, A.; Chateau, D.; Phillips-Beck, W.; Singal, D.; MacWilliam, L.; Longstaffe, S.; Chudley, A.; Elias, B.; et al. Health, Social, Education, and Justice Outcomes of Manitoba First Nations Children Diagnosed with Fetal Alcohol Spectrum Disorder: A Population-Based Cohort Study of Linked Administrative Data. Can. J. Psychiatry 2019, 64, 611–620. [Google Scholar] [CrossRef]
- Sessa, F.; Salerno, M.; Esposito, M.; Di Nunno, N.; Rosi, G.L.; Roccuzzo, S.; Pomara, C. Understanding the Relationship between Fetal Alcohol Spectrum Disorder (FASD) and Criminal Justice: A Systematic Review. Healthcare 2022, 10, 84. [Google Scholar] [CrossRef] [PubMed]
- Kambeitz, C.; Klug, M.G.; Greenmyer, J.; Popova, S.; Burd, L. Association of adverse childhood experiences and neurodevelopmental disorders in people with fetal alcohol spectrum disorders (FASD) and non-FASD controls. BMC Pediatr. 2019, 19, 498. [Google Scholar]
- Spohr, H.L.; Willms, J.; Steinhausen, H.C. Fetal alcohol spectrum disorders in young adulthood. J. Pediatr. 2007, 150, 175–179.e1. [Google Scholar] [CrossRef] [PubMed]
- Streissguth, A.P.; Bookstein, F.L.; Barr, H.M.; Sampson, P.D.; O’Malley, K.; Young, J.K. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J. Dev. Behav. Pediatr. 2004, 25, 228–238. [Google Scholar] [CrossRef]
- Lange, S.; Probst, C.; Gmel, G.; Rehm, J.; Burd, L.; Popova, S. Global Prevalence of Fetal Alcohol Spectrum Disorder Among Children and Youth: A Systematic Review and Meta-analysis. JAMA Pediatr. 2017, 171, 948–956. [Google Scholar] [CrossRef]
- Popova, S.; Lange, S.; Shield, K.; Burd, L.; Rehm, J. Prevalence of fetal alcohol spectrum disorder among special subpopulations: A systematic review and meta-analysis. Addiction 2019, 114, 1150–1172. [Google Scholar] [CrossRef]
- Lupton, C.; Burd, L.; Harwood, R. Cost of fetal alcohol spectrum disorders. Am. J. Med. Genet. C Semin. Med. Genet. 2004, 127c, 42–50. [Google Scholar] [CrossRef]
- Greenmyer, J.R.; Klug, M.G.; Kambeitz, C.; Popova, S.; Burd, L. A Multicountry Updated Assessment of the Economic Impact of Fetal Alcohol Spectrum Disorder: Costs for Children and Adults. J. Addict. Med. 2018, 12, 466–473. [Google Scholar] [CrossRef] [PubMed]
- Astley, S.J. Validation of the fetal alcohol spectrum disorder (FASD) 4-Digit Diagnostic Code. J. Popul. Ther. Clin. Pharmacol. 2013, 20, e416–e467. [Google Scholar] [PubMed]
- Gerberding, J.L.; Cordero, J.; Floyd, R.L. Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis; National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, and the Department of Health and Human Services: Atlanta, GA, USA, 2004.
- Hoyme, H.E.; Kalberg, W.O.; Elliott, A.J.; Blankenship, J.; Buckley, D.; Marais, A.S.; Manning, M.A.; Robinson, L.K.; Adam, M.P.; Abdul-Rahman, O.; et al. Updated Clinical Guidelines for Diagnosing Fetal Alcohol Spectrum Disorders. Pediatrics 2016, 138, e20154256. [Google Scholar] [CrossRef] [PubMed]
- Landgraf, M.N.; Nothacker, M.; Kopp, I.B.; Heinen, F. The diagnosis of fetal alcohol syndrome. Dtsch. Arztebl. Int. 2013, 110, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Hagan, J.F., Jr.; Balachova, T.; Bertrand, J.; Chasnoff, I.; Dang, E.; Fernandez-Baca, D.; Kable, J.; Kosofsky, B.; Senturias, Y.N.; Singh, N.; et al. Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure. Pediatrics 2016, 138, e20151553. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5); American Psychiatric Pub.: Washington, DC, USA, 2013. [Google Scholar]
- Brown, J.M.; Bland, R.; Jonsson, E.; Greenshaw, A.J. The Standardization of Diagnostic Criteria for Fetal Alcohol Spectrum Disorder (FASD): Implications for Research, Clinical Practice and Population Health. Can. J. Psychiatry 2019, 64, 169–176. [Google Scholar] [CrossRef]
- Peadon, E.; Fremantle, E.; Bower, C.; Elliott, E.J. International survey of diagnostic services for children with Fetal Alcohol Spectrum Disorders. BMC Pediatr. 2008, 8, 12. [Google Scholar] [CrossRef]
- Brouwers, M.C.; Kerkvliet, K.; Spithoff, K. AGREE Next Steps Consortium the AGREE Reporting Checklist: A tool to improve reporting of clinical practice guidelines. BMJ 2016, 352, i1152. [Google Scholar] [CrossRef]
- Grol, R.; Dalhuijsen, J.; Thomas, S.; Veld, C.I.; Rutten, G.; Mokkink, H. Attributes of clinical guidelines that influence use of guidelines in general practice: Observational study. BMJ 1998, 317, 858–861. [Google Scholar] [CrossRef]
- Hayes, N.; Akison, L.K.; Goldsbury, S.; Hewlett, N.; Elliott, E.J.; Finlay-Jones, A.; Shanley, D.C.; Bagley, K.; Crawford, A.; Till, H.; et al. Key Stakeholder Priorities for the Review and Update of the Australian Guide to Diagnosis of Fetal Alcohol Spectrum Disorder: A Qualitative Descriptive Study. Int. J. Environ. Res. Public Health 2022, 19, 5823. [Google Scholar] [CrossRef]
- Petkovic, J.; Riddle, A.; Akl, E.A.; Khabsa, J.; Lytvyn, L.; Atwere, P.; Campbell, P.; Chalkidou, K.; Chang, S.M.; Crowe, S.; et al. Protocol for the development of guidance for stakeholder engagement in health and healthcare guideline development and implementation. Syst. Rev. 2020, 9, 21. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Chambers, T.; Chiang, C.-H. Understanding undergraduate students’ experience: A content analysis using NSSE open-ended comments as an example. Qual. Quant. 2012, 46, 1113–1123. [Google Scholar] [CrossRef]
- Hsieh, H.-F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Coles, C.D.; Gailey, A.R.; Mulle, J.G.; Kable, J.A.; Lynch, M.E.; Jones, K.L. A Comparison Among 5 Methods for the Clinical Diagnosis of Fetal Alcohol Spectrum Disorders. Alcohol. Clin. Exp. Res. 2016, 40, 1000–1009. [Google Scholar] [CrossRef]
- Hemingway, U.J.A.; Bledsoe, J.; Brooks, A.; Davies, J.; Jirikowic, T.; Olson, E.; Thorne, J. Comparison of the 4-Digit Code, Canadian 2015, Australian 2016 and Hoyme 2016 fetal alcohol spectrum disorder diagnostic guidelines. Adv. Pediatr. Res. 2019, 6, 31. [Google Scholar] [CrossRef]
- Astley, S.J.; Bledsoe, J.M.; Davies, J.K.; Thorne, J.C. Comparison of the FASD 4-Digit Code and Hoyme et al. 2016 FASD diagnostic guidelines. Adv. Pediatr. Res. 2017, 4, 13. [Google Scholar]
- Clarren, S.; I Halliwell, C.; Werk, C.M.; Sebaldt, R.J.; Petrie, A.; Lilley, C.; Cook, J. Using a Common Form for Consistent Collection and Reporting of FASD Data from Across Canada: A Feasibility Study. J. Popul. Ther. Clin. Pharmacol. 2015, 22, e211–e218. [Google Scholar]
- Sims, R.; Michaleff, Z.A.; Glasziou, P.; Thomas, R. Consequences of a Diagnostic Label: A Systematic Scoping Review and Thematic Framework. Front. Public Health 2021, 9, 725877. [Google Scholar] [CrossRef]
- Temple, V.K.; Prasad, S.; Popova, S.; Lindsay, A. Long-term outcomes following Fetal Alcohol Spectrum Disorder (FASD) diagnosis in adulthood. J. Intellect. Dev. Disabil. 2021, 46, 272–280. [Google Scholar] [CrossRef]
- Chamberlain, K.; Reid, N.; Warner, J.; Shelton, D.; Dawe, S. A qualitative evaluation of caregivers’ experiences, understanding and outcomes following diagnosis of FASD. Res. Dev. Disabil. 2017, 63, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Mattson, S.N.; Bernes, G.A.; Doyle, L.R. Fetal Alcohol Spectrum Disorders: A Review of the Neurobehavioral Deficits Associated with Prenatal Alcohol Exposure. Alcohol. Clin. Exp. Res. 2019, 43, 1046–1062. [Google Scholar] [CrossRef] [PubMed]
- Okulicz-Kozaryn, K.; Maryniak, A.; Borkowska, M.; Śmigiel, R.; Dylag, K.A. Diagnosis of Fetal Alcohol Spectrum Disorders (FASDs): Guidelines of Interdisciplinary Group of Polish Professionals. Int. J. Environ. Res. Public Health 2021, 18, 7526. [Google Scholar] [CrossRef] [PubMed]
- Correa, V.C.; Lugo-Agudelo, L.H.; Aguirre-Acevedo, D.C.; Contreras, J.A.P.; Borrero, A.M.P.; Patiño-Lugo, D.F.; Valencia, D.A.C. Individual, health system, and contextual barriers and facilitators for the implementation of clinical practice guidelines: A systematic metareview. Health Res. Policy Syst. 2020, 18, 74. [Google Scholar] [CrossRef]
- Fischer, F.; Lange, K.; Klose, K.; Greiner, W.; Kraemer, A. Barriers and Strategies in Guideline Implementation—A Scoping Review. Healthcare 2016, 4, 36. [Google Scholar]
- Cabana, M.D.; Rand, C.S.; Powe, N.R.; Wu, A.W.; Wilson, M.H.; Abboud, P.-A.C.; Rubin, H.R. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999, 282, 1458–1465. [Google Scholar] [CrossRef]
- Francke, A.L.; Smit, M.C.; de Veer, A.J.; Mistiaen, P. Factors influencing the implementation of clinical guidelines for health care professionals: A systematic meta-review. BMC Med. Inform. Decis. Mak. 2008, 8, 38. [Google Scholar] [CrossRef]
- Lau, R.; Stevenson, F.; Ong, B.N.; Dziedzic, K.; Treweek, S.; Eldridge, S.; Everitt, H.; Kennedy, A.; Qureshi, N.; Rogers, A.; et al. Achieving change in primary care—Causes of the evidence to practice gap: Systematic reviews of reviews. Implement. Sci. 2016, 11, 40. [Google Scholar] [CrossRef]
- Wozniak, J.R.; Riley, E.P.; Charness, M.E. Clinical presentation, diagnosis, and management of fetal alcohol spectrum disorder. Lancet Neurol. 2019, 18, 760–770. [Google Scholar]
- Jones, K.L.; Robinson, L.K.; Bakhireva, L.N.; Marintcheva, G.; Storojev, V.; Strahova, A.; Sergeevskaya, S.; Budantseva, S.; Mattson, S.N.; Riley, E.P.; et al. Accuracy of the Diagnosis of Physical Features of Fetal Alcohol Syndrome by Pediatricians After Specialized Training. Pediatrics 2006, 118, e1734–e1738. [Google Scholar] [CrossRef]
- Beauchamp, M.H.; Brooks, B.L.; Barrowman, N.; Aglipay, M.; Keightley, M.; Anderson, P.; Yeates, K.O.; Osmond, M.H.; Zemek, R. Empirical Derivation and Validation of a Clinical Case Definition for Neuropsychological Impairment in Children and Adolescents. J. Int. Neuropsychol. Soc. 2015, 21, 596–609. [Google Scholar] [CrossRef] [PubMed]
- Guilmette, T.J.; Sweet, J.J.; Hebben, N.; Koltai, D.; Mahone, E.M.; Spiegler, B.J.; Stucky, K.; Westerveld, M.; Participants, C. American Academy of Clinical Neuropsychology consensus conference statement on uniform labeling of performance test scores. Clin. Neuropsychol. 2020, 34, 437–453. [Google Scholar] [CrossRef] [PubMed]
- Perumal, N.; Bassani, D.; Roth, D.E. Use and Misuse of Stunting as a Measure of Child Health. J. Nutr. 2018, 148, 311–315. [Google Scholar] [CrossRef]
- Hruschka, D.J. One size does not fit all. How universal standards for normal height can hide deprivation and create false paradoxes. Am. J. Hum. Biol. 2021, 33, e23552. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.V.; Pearson, T.A.; Bennett, G.C.; Cushman, W.C.; Gaziano, T.A.; Gorman, P.N.; Handler, J.; Krumholz, H.M.; Kushner, R.F.; MacKenzie, T.D.; et al. ACC/AHA Special Report: Clinical Practice Guideline Implementation Strategies: A Summary of Systematic Reviews by the NHLBI Implementation Science Work Group: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2017, 69, 1076–1092. [Google Scholar]
- First, M.B.; Gaebel, W.; Maj, M.; Stein, D.J.; Kogan, C.S.; Saunders, J.B.; Poznyak, V.B.; Gureje, O.; Lewis-Fernández, R.; Maercker, A.; et al. An organization- and category-level comparison of diagnostic requirements for mental disorders in ICD-11 and DSM-5. World Psychiatry 2021, 20, 34–51. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, J.C. Diagnostic Issues and Controversies in DSM-5: Return of the False Positives Problem. Annu. Rev. Clin. Psychol. 2016, 12, 105–132. [Google Scholar] [CrossRef]
- Singh, D.; Sinnott-Armstrong, W. The DSM-5 definition of mental disorder: Critique and alternatives. Public Aff. Q. 2015, 29, 5–31. [Google Scholar]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Doyle, L.R.; Mattson, S.N. Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE): Review of Evidence and Guidelines for Assessment. Curr. Dev. Disord. Rep. 2015, 2, 175–186. [Google Scholar] [CrossRef]
| Clinic Frequency | Canadian Guidelines (2016) (n = 15) | Australian Guidelines (Bower & Elliot, 2016) (n = 7) | 4 Digit Code (Astley, 2004) (n = 12) | Other Guidelines (n = 4) | Multiple Guidelines (n = 17) | |
|---|---|---|---|---|---|---|
| Country | ||||||
| United States | 22 | 10 | 4 | 8 | ||
| Australia | 8 | 7 | 1 | |||
| New Zealand | 8 | 6 | 2 | |||
| Canada | 10 | 9 | 1 | |||
| UK | 3 | 3 | ||||
| Other | 4 | 1 | 1 | 2 | ||
| Clinic Type | ||||||
| Hospital | 20 | 7 | 3 | 3 | 3 | 4 |
| Community agency | 14 | 6 | 3 | 4 | 0 | 1 |
| University | 6 | 0 | 0 | 2 | 2 | 2 |
| Private practice | 15 | 1 | 1 | 3 | 0 | 10 |
| Other * | 6 | 2 | 1 | 1 | 0 | 2 |
| Diagnostic Criteria | Frequency |
|---|---|
| Australian Guide to FASD Diagnosis (Bower & Elliott, 2016) | 9 |
| Canadian Diagnostic Guideline (Chudley et al., 2005) | 3 |
| Revised Canadian Diagnostic Guideline (Cook et al., 2016) | 22 |
| Revised United States Institute of Medicine Criteria (Hoyme et al., 2005) | 6 |
| 4-Digit Diagnostic Code (Astley, 2004) | 21 |
| Centers for Disease Control and Prevention (Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis, 2004) | 7 |
| Emory Clinic Diagnostic Guidelines | 2 |
| DSM 5 | 4 |
| Revised United States Institute of Medicine Criteria (Hoyme et al., 2016) | 2 |
| Other | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reid, N.; Shanley, D.C.; Logan, J.; White, C.; Liu, W.; Hawkins, E. International Survey of Specialist Fetal Alcohol Spectrum Disorder Diagnostic Clinics: Comparison of Diagnostic Approach and Considerations Regarding the Potential for Unification. Int. J. Environ. Res. Public Health 2022, 19, 15663. https://doi.org/10.3390/ijerph192315663
Reid N, Shanley DC, Logan J, White C, Liu W, Hawkins E. International Survey of Specialist Fetal Alcohol Spectrum Disorder Diagnostic Clinics: Comparison of Diagnostic Approach and Considerations Regarding the Potential for Unification. International Journal of Environmental Research and Public Health. 2022; 19(23):15663. https://doi.org/10.3390/ijerph192315663
Chicago/Turabian StyleReid, Natasha, Dianne C. Shanley, Jayden Logan, Codi White, Wei Liu, and Erinn Hawkins. 2022. "International Survey of Specialist Fetal Alcohol Spectrum Disorder Diagnostic Clinics: Comparison of Diagnostic Approach and Considerations Regarding the Potential for Unification" International Journal of Environmental Research and Public Health 19, no. 23: 15663. https://doi.org/10.3390/ijerph192315663
APA StyleReid, N., Shanley, D. C., Logan, J., White, C., Liu, W., & Hawkins, E. (2022). International Survey of Specialist Fetal Alcohol Spectrum Disorder Diagnostic Clinics: Comparison of Diagnostic Approach and Considerations Regarding the Potential for Unification. International Journal of Environmental Research and Public Health, 19(23), 15663. https://doi.org/10.3390/ijerph192315663






