Factors Related to HPV Vaccination Intention among MSM in China: A Bayesian Network Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects of Study
2.2. Inclusion and Exclusion Criteria
2.3. Questionnaire Content
2.4. Statistical Analysis
3. Results
3.1. General Demographic Characteristics and HPV Vaccination Intention
3.2. Behavioral Characteristics and HPV Vaccination Intention
3.3. Knowledge Attitudes, Risk Threat Perception, and HPV Vaccination Intention
3.4. Bayesian Network Model
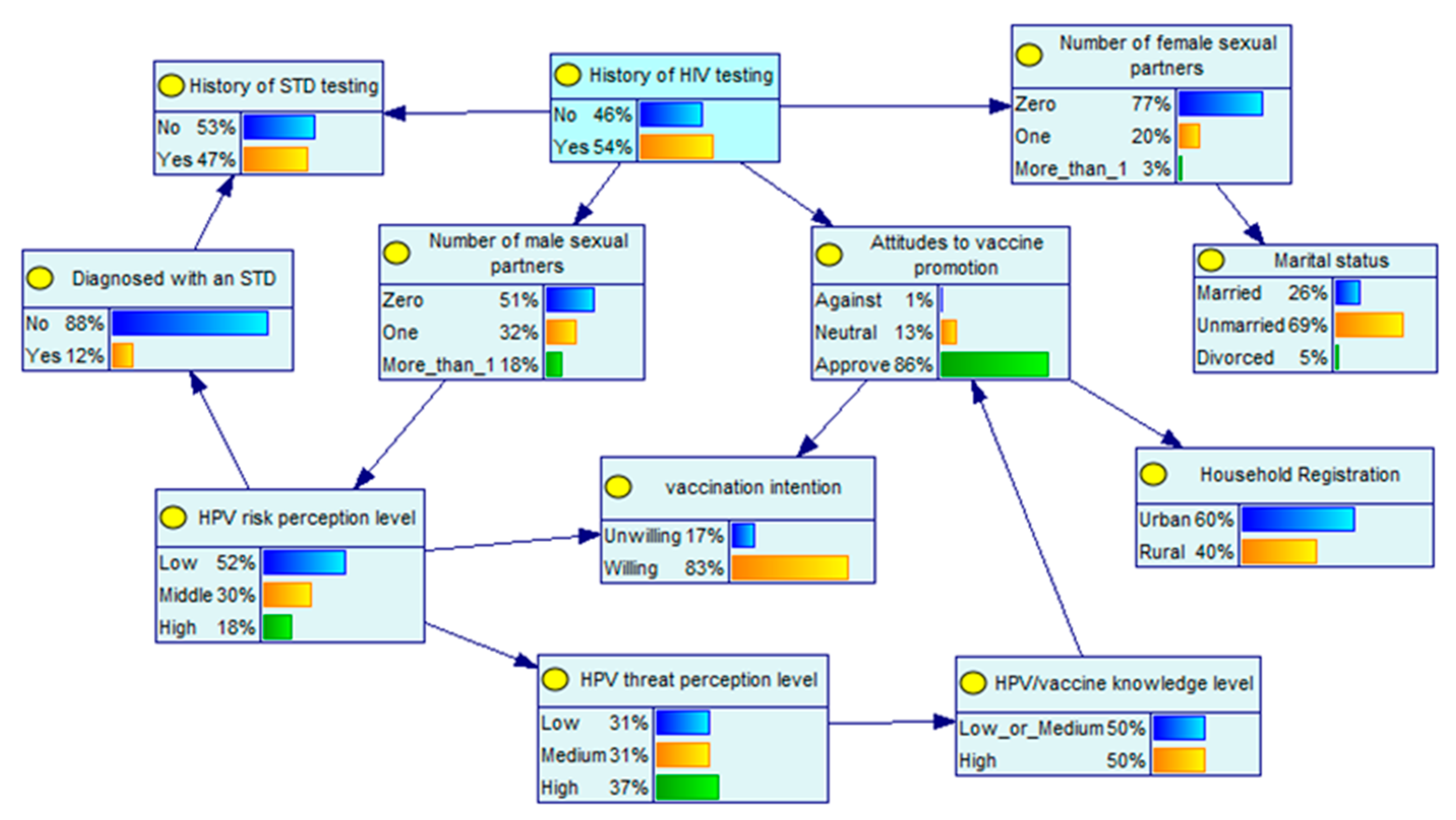
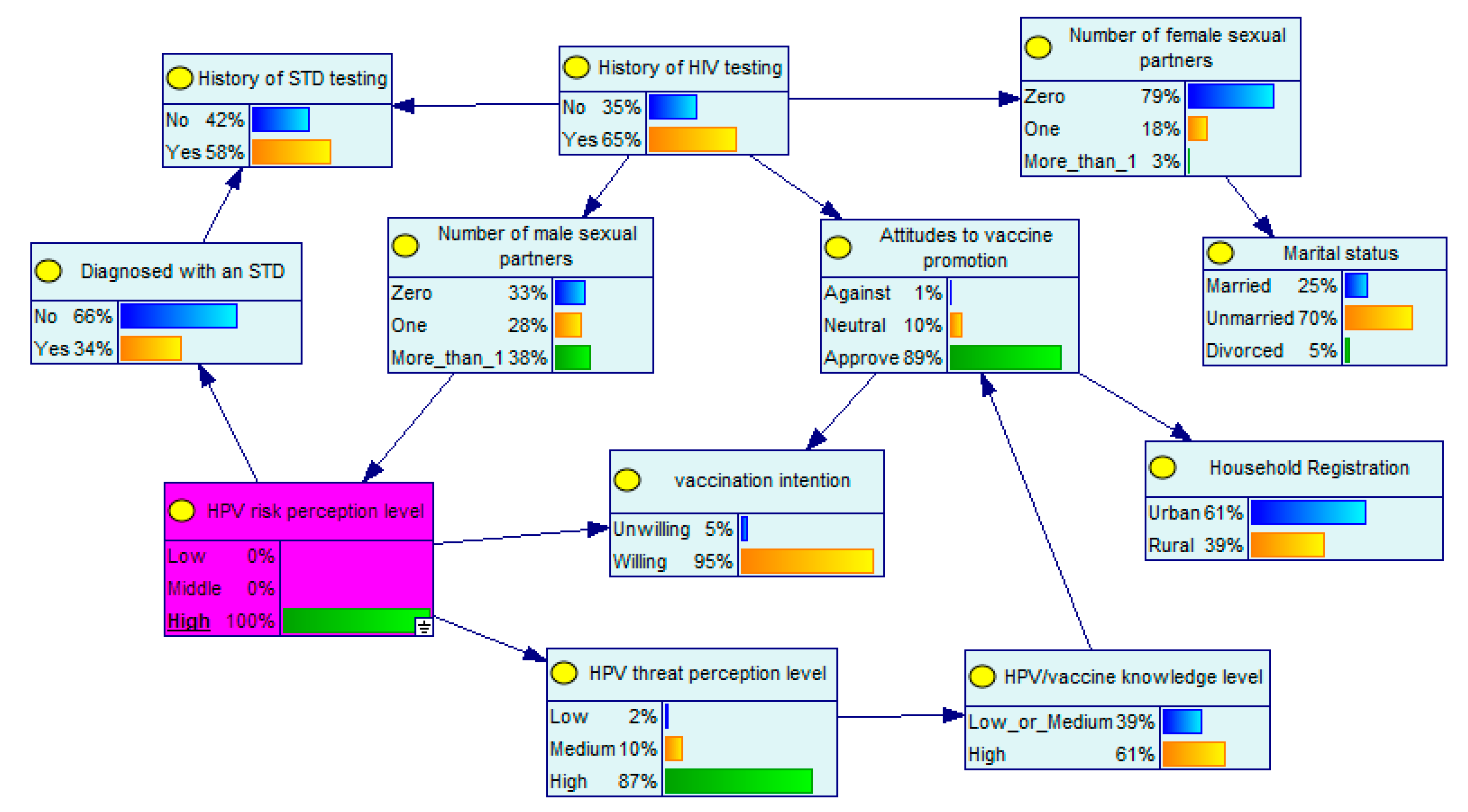
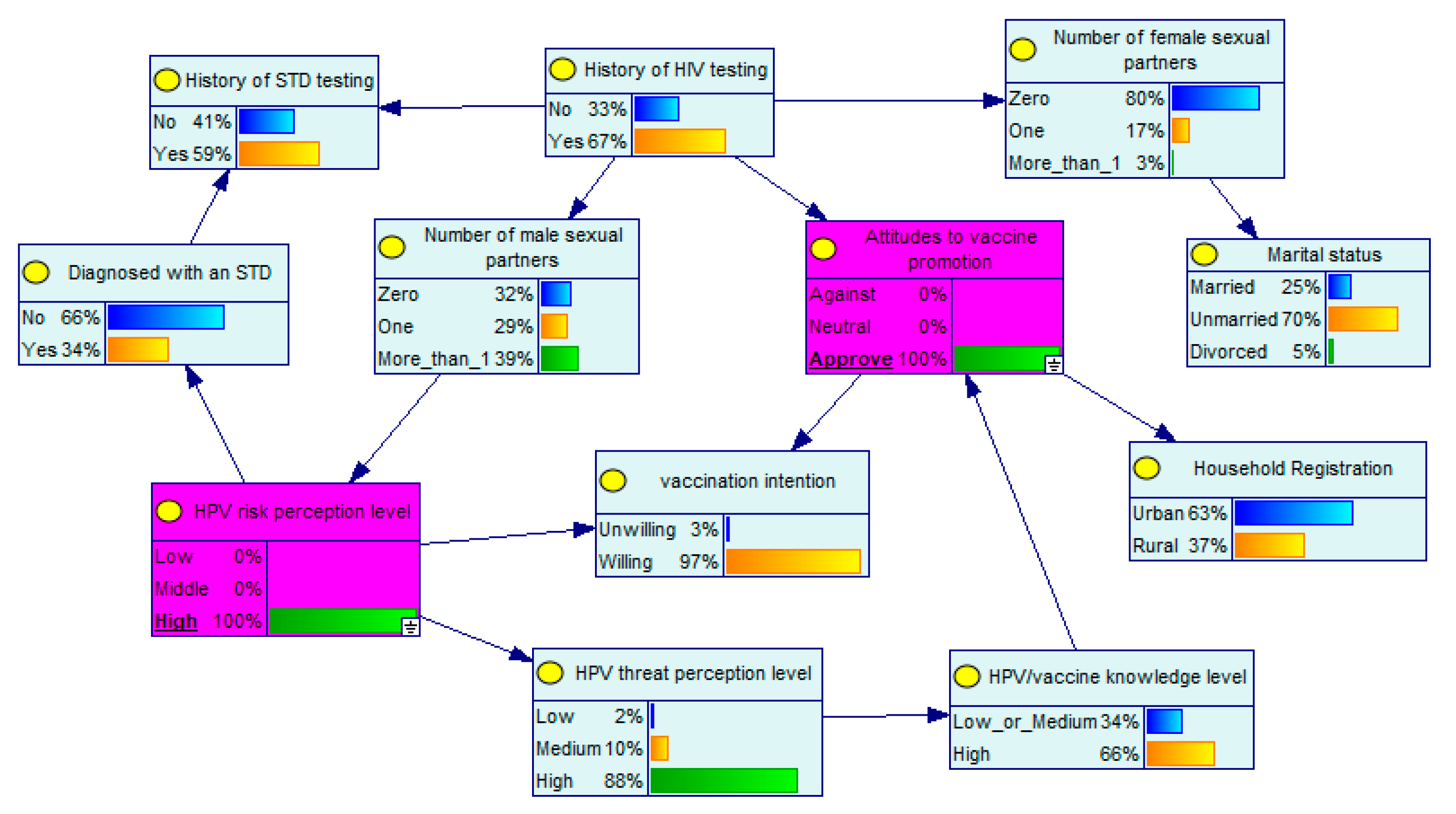
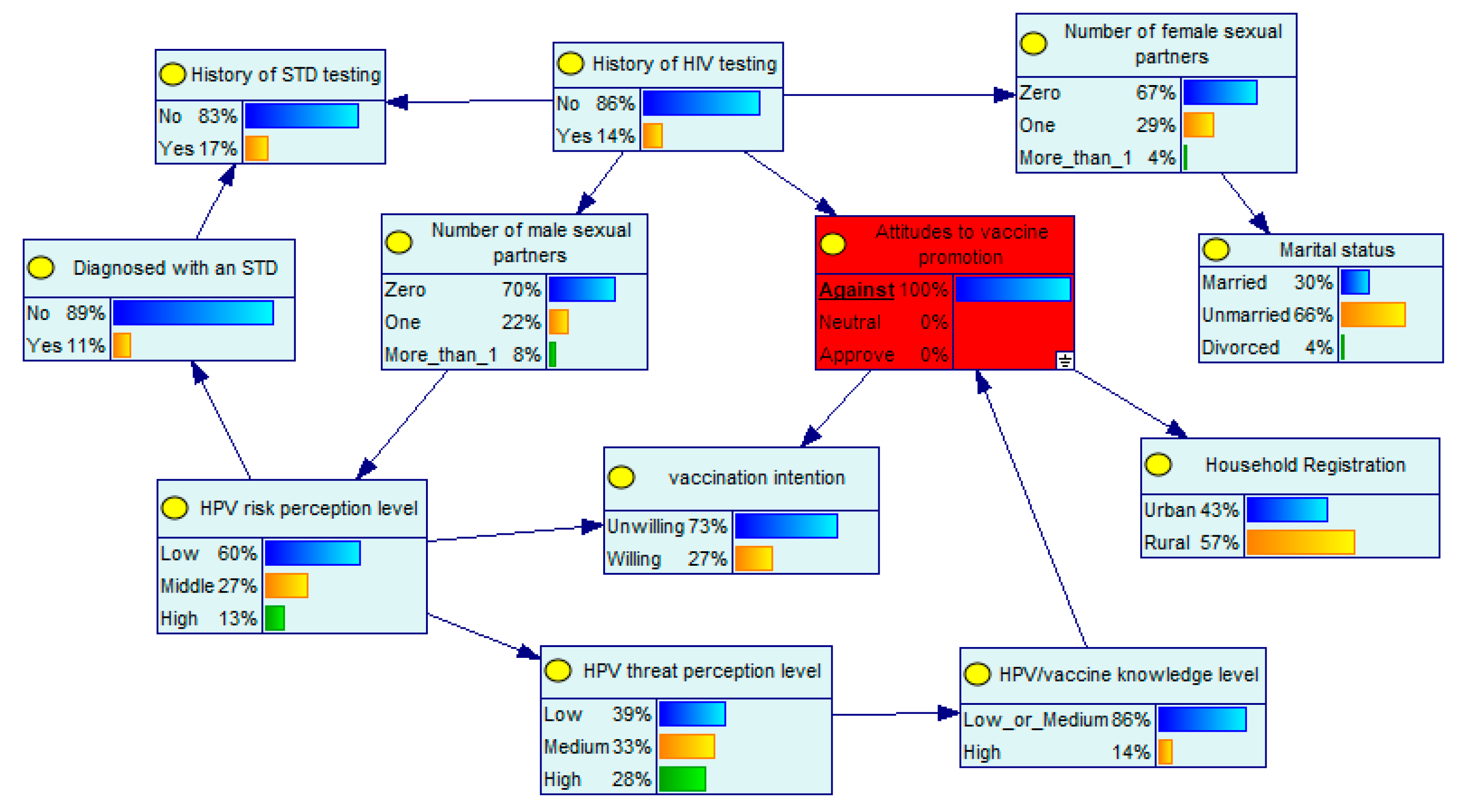
3.5. Conditional Probabilistic Reasoning
4. Discussion
4.1. Willingness to Vaccinate
4.2. Relevant Factors
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McBride, A.A. Human Papillomaviruses: Diversity, Infection and Host Interactions. Nat. Rev. Microbiol. 2022, 20, 95–108. [Google Scholar] [CrossRef]
- Lei, J.; Ploner, A.; Elfström, K.M.; Wang, J.; Roth, A.; Fang, F.; Sundström, K.; Dillner, J.; Sparén, P. HPV Vaccination and the Risk of Invasive Cervical Cancer. N. Engl. J. Med. 2020, 383, 1340–1348. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Dong, Y. Human Papillomavirus and Oral Squamous Cell Carcinoma: A Review of HPV-Positive Oral Squamous Cell Carcinoma and Possible Strategies for Future. Curr. Probl. Cancer 2017, 41, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Franceschi, S.; Clifford, G.M. Human Papillomavirus Types from Infection to Cancer in the Anus, According to Sex and Hiv Status: A Systematic Review and Meta-Analysis. Lancet Infect. Dis. 2018, 18, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Wittekindt, C.; Wagner, S.; Bushnak, A.; Prigge, E.S.; Doeberitz, M.V.; Würdemann, N.; Bernhardt, K.; Pons-Kühnemann, J.; Maulbecker-Armstrong, C.; Klussmann, J.P. Increasing Incidence Rates of Oropharyngeal Squamous Cell Carcinoma in Germany and Significance of Disease Burden Attributed to Human Papillomavirus. Cancer Prev. Res. (Phila.) 2019, 12, 375–382. [Google Scholar] [CrossRef]
- Prigge, E.S.; Doeberitz, M.V.; Reuschenbach, M. Clinical Relevance and Implications of HPV-Induced Neoplasia in Different Anatomical Locations. Mutat. Res. Rev. Mutat. Res. 2017, 772, 51–66. [Google Scholar] [CrossRef]
- Chesson, H.W.; Dunne, E.F.; Hariri, S.; Markowitz, L.E. The Estimated Lifetime Probability of Acquiring Human Papillomavirus in the United States. Sex. Transm. Dis. 2014, 41, 660–664. [Google Scholar] [CrossRef]
- Serrano, B.; Brotons, M.; Bosch, F.X.; Bruni, L. Epidemiology and Burden of HPV-Related Disease. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 47, 14–26. [Google Scholar] [CrossRef]
- Gargano, J.W.; Unger, E.R.; Liu, G.; Steinau, M.; Meites, E.; Dunne, E.; Markowitz, L.E. Prevalence of Genital Human Papillomavirus in Males, United States, 2013-2014. J. Infect. Dis. 2017, 215, 1070–1079. [Google Scholar] [CrossRef]
- Wei, F.; Yin, K.; Wu, X.; Lan, J.; Huang, S.; Sheng, W.; Zhao, J.; Su, Y.; Wang, Y.; Li, Y.; et al. Human Papillomavirus Prevalence and Associated Factors in Women and Men in South China: A Population-Based Study. Emerg. Microbes Infect. 2016, 5, e119. [Google Scholar] [CrossRef]
- Meites, E.; Szilagyi, P.G.; Chesson, H.W.; Unger, E.R.; Romero, J.R.; Markowitz, L.E. Human Papillomavirus Vaccination for Adults: Updated Recommendations of the Advisory Committee on Immunization Practices. Morb. Mortal. Wkly. Rep. 2019, 68, 698–702. [Google Scholar] [CrossRef]
- Spinner, C.; Ding, L.; Bernstein, D.I.; Brown, D.R.; Franco, E.L.; Covert, C.; Kahn, J.A. Human Papillomavirus Vaccine Effectiveness and Herd Protection in Young Women. Pediatrics 2019, 143, e20181902. [Google Scholar] [CrossRef]
- Petrosky, E.; Bocchini, J.A., Jr.; Hariri, S.; Chesson, H.; Curtis, C.R.; Saraiya, M.; Unger, E.R.; Markowitz, L.E. Use of 9-Valent Human Papillomavirus (HPV) Vaccine: Updated HPV Vaccination Recommendations of the Advisory Committee on Immunization Practices. Morb. Mortal. Wkly. Rep. 2015, 64, 300–304. [Google Scholar]
- Meites, E.; Winer, R.L.; Newcomb, M.E.; Gorbach, P.M.; Querec, T.D.; Rudd, J.; Collins, T.; Lin, J.; Moore, J.; Remble, T.; et al. Vaccine Effectiveness against Prevalent Anal and Oral Human Papillomavirus Infection among Men Who Have Sex with Men—United States, 2016–2018. J. Infect. Dis. 2020, 222, 2052–2060. [Google Scholar] [CrossRef]
- Winer, R.L.; Lin, J.; Querec, T.D.; Unger, E.R.; Stern, J.E.; Rudd, J.M.; Golden, M.R.; Swanson, F.; Markowitz, L.E.; Meites, E. Effectiveness of Human Papillomavirus (HPV) Vaccination against Penile HPV Infection in Men Who Have Sex with Men and Transgender Women. J. Infect. Dis. 2022, 225, 422–430. [Google Scholar] [CrossRef]
- Cranston, R.D. Young Gay Men and the Quadrivalent Human Papillomavirus Vaccine--Much to Gain (and Lose). J. Infect. Dis. 2014, 209, 635–638. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zou, Z.; Fairley, C.K.; Ong, J.J.; Hocking, J.; Canfell, K.; Ma, X.; Chow, E.P.F.; Xu, X.; Zhang, L.; Zhuang, G. Domestic HPV Vaccine Price and Economic Returns for Cervical Cancer Prevention in China: A Cost-Effectiveness Analysis. Lancet Glob Health 2020, 8, e1335–e1344. [Google Scholar] [CrossRef] [PubMed]
- Díez-Domingo, J.; Sánchez-Alonso, V.; Villanueva, R.J.; Acedo, L.; Tuells, J. Impact of a Gender-Neutral HPV Vaccination Program in Men Who Have Sex with Men (Msm). Int. J. Environ. Res. Public Health 2021, 18, 963. [Google Scholar] [CrossRef] [PubMed]
- Lin, A.; Ong, K.J.; Hobbelen, P.; King, E.; Mesher, D.; Edmunds, W.J.; Sonnenberg, P.; Gilson, R.; Bains, I.; Choi, Y.H.; et al. Impact and Cost-Effectiveness of Selective Human Papillomavirus Vaccination of Men Who Have Sex with Men. Clin. Infect. Dis. 2017, 64, 580–588. [Google Scholar] [CrossRef]
- Zhang, L.; Regan, D.G.; Ong, J.J.; Gambhir, M.; Chow, E.P.F.; Zou, H.; Law, M.; Hocking, J.; Fairley, C.K. Targeted Human Papillomavirus Vaccination for Young Men Who Have Sex with Men in Australia Yields Significant Population Benefits and Is Cost-Effective. Vaccine 2017, 35, 4923–4929. [Google Scholar] [CrossRef]
- Mann-Barnes, T.; Bhimla, A.; Coronado, M.; Lin, T.; Duro-Aina, A.; Park, H.; Ma, G.X. Factors That Predict HPV Vaccination Behavior among Young Men-Who-Have-Sex-with-Men in the Greater Philadelphia Region. J. Racial Ethn. Health Disparities 2022. [Google Scholar] [CrossRef]
- Stearns, S.; Quaife, S.L.; Forster, A. Examining Facilitators of HPV Vaccination Uptake in Men Who Have Sex with Men: A Cross-Sectional Survey Design. Int. J. Environ. Res. Public Health 2020, 17, 7713. [Google Scholar] [CrossRef]
- Meng, X.; Jia, T.; Zhang, X.; Zhu, C.; Chen, X.; Zou, H. Analysis on Willingness to Receive Human Papillomavirus Vaccination among Risk Males and Related Factors. Chin. J. Epidemiol. 2015, 36, 1119–1124. [Google Scholar]
- Ji, J.; Yang, C.; Liu, J.; Liu, J.; Yin, B. A Comparative Study on Swarm Intelligence for Structure Learning of Bayesian Networks. Soft Comput. 2017, 21, 6713–6738. [Google Scholar] [CrossRef]
- Hughes, R.E. Using a Bayesian Network to Predict L5/S1 Spinal Compression Force from Posture, Hand Load, Anthropometry, and Disc Injury Status. Appl. Bionics Biomech. 2017, 2017, 2014961. [Google Scholar] [CrossRef]
- Requejo-Castro, D.; Giné-Garriga, R.; Pérez-Foguet, A. Bayesian Network Modelling of Hierarchical Composite Indicators. Sci. Total Environ. 2019, 668, 936–946. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.H.; Liu, Z.Z.; Cui, S.T.; Chu, Z.X.; Jiang, Y.J.; Xu, J.J.; Hu, Q.H.; Shang, H. High Human Papillomavirus Vaccine Acceptability and Cost-Effectiveness of the Chinese 2-Valent Vaccine among Men Who Have Sex with Men: A Cross-Sectional Study in Shenyang, China. Front. Med. (Lausanne) 2021, 8, 763564. [Google Scholar] [CrossRef]
- Hoefer, L.; Tsikis, S.; Bethimoutis, G.; Nicolaidou, E.; Paparizos, V.; Antoniou, C.; Kanelleas, A.; Chardalias, L.; Stavropoulos, G.E.; Schneider, J.; et al. HPV Vaccine Acceptability in High-Risk Greek Men. Hum. Vaccin. Immunother. 2018, 14, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wang, Y.; Liu, L.; Fan, Y.; Liu, Z.; Wang, Y.; Nie, S. Awareness and Knowledge About Human Papillomavirus Vaccination and Its Acceptance in China: A Meta-Analysis of 58 Observational Studies. BMC Public Health 2016, 16, 216. [Google Scholar] [CrossRef] [PubMed]
- Tian, T.; Sang, G.; Cai, A.; Huang, B.; Dai, J. Willingness to Receive Human Papiilomavirus Vaccination and Its Related Factors among Hiv-Negative Men Who Have Sex with Men. Chin. J. Public Health 2018, 34, 229–233. [Google Scholar]
- He, W.; Pan, H.; Lin, B.; Zhong, X. Analysis of HPV Vaccination Willingness Amongst Hiv-Negative Men Who Have Sex with Men in China. Vaccines 2021, 9, 1069. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.; Geoffroy, E.; Tian, K.; Wang, L.; Feng, L.; Feng, J.; Qin, Y.; Wu, P.; Zhang, S.; Geng, M.; et al. Knowledge, Attitudes, and Behaviors (Kab) of Influenza Vaccination in China: A Cross-Sectional Study in 2017/2018. Vaccines 2019, 8, 7. [Google Scholar] [CrossRef] [PubMed]
- Nadarzynski, T.; Smith, H.; Richardson, D.; Pollard, A.; Llewellyn, C. Perceptions of HPV and Attitudes Towards HPV Vaccination Amongst Men Who Have Sex with Men: A Qualitative Analysis. Br. J. Health Psychol. 2017, 22, 345–361. [Google Scholar] [CrossRef] [PubMed]
- Yao, P.Y.; Lin, C.Y.; Ko, N.Y.; Zou, H.; Lee, C.W.; Strong, C. Predicting Human Papillomavirus Vaccine Uptake in Men Who Have Sex with Men the Influence of Vaccine Price and Receiving an HPV Diagnosis. BMC Public Health 2022, 22, 28. [Google Scholar] [CrossRef]
| Variable | Cases | Willing to Be Vaccinated | OR (95% CI) | p Value | |
|---|---|---|---|---|---|
| N | % | ||||
| Total | 969 | 802 | 82.77 | ||
| Age | |||||
| 14–18 | 33 | 27 | 81.82 | Reference | |
| 18–35 | 719 | 598 | 83.17 | 1.098 (0.403, 2.547) | 0.839 |
| 35–55 | 217 | 177 | 81.57 | 0.983 (0.349, 2.399) | 0.972 |
| Household Registration | |||||
| Rural | 388 | 309 | 79.64 | Reference | |
| Urban | 581 | 493 | 84.85 | 1.432 (1.023, 2.003) | 0.036 |
| Region | |||||
| Developed | 254 | 206 | 81.10 | Reference | |
| Moderately developed | 193 | 153 | 79.27 | 0.891 (0.558, 1.429) | 0.630 |
| Less developed | 522 | 443 | 84.87 | 1.307 (0.876, 1.933) | 0.184 |
| Ethnicity | |||||
| Han nationality | 933 | 733 | 82.85 | Reference | |
| Other nationalities | 36 | 29 | 80.56 | 0.858 (0.390, 2.159) | 0.721 |
| Education level | |||||
| Illiterate/semi-literate | 9 | 7 | 77.78 | Reference | |
| Primary | 10 | 7 | 70.00 | 0.667 (0.070, 5.291) | 0.702 |
| Junior high | 71 | 53 | 74.65 | 0.841 (0.118, 3.871) | 0.838 |
| High/secondary school | 168 | 138 | 82.14 | 1.314 (0.190, 5.765) | 0.741 |
| Junior college | 234 | 185 | 79.06 | 1.079 (0.157, 4.632) | 0.926 |
| College and above | 477 | 412 | 86.37 | 1.811 (0.266, 7.687) | 0.465 |
| Employment status | |||||
| Employed | 707 | 591 | 83.59 | Reference | |
| Student | 168 | 139 | 82.74 | 0.941 (0.609, 1.493) | 0.789 |
| Unemployed | 94 | 72 | 76.60 | 0.642 (0.389, 1.098) | 0.094 |
| Marital status | |||||
| Married | 250 | 194 | 77.60 | Reference | |
| Unmarried | 672 | 570 | 84.82 | 1.613 (1.116, 2.315) | 0.010 |
| Divorced | 47 | 38 | 80.85 | 1.219 (0.577, 2.822) | 0.621 |
| Monthly disposable income | |||||
| 1000 RMB or less | 76 | 58 | 76.32 | Reference | |
| 1001–3000 RMB | 222 | 182 | 81.98 | 1.412 (0.740, 2.623) | 0.283 |
| 3001–5000 RMB | 250 | 212 | 84.80 | 1.731 (0.906, 3.223) | 0.089 |
| 5001–10000 RMB | 296 | 242 | 81.76 | 1.391 (0.744, 2.513) | 0.286 |
| 10000 RMB or more | 125 | 108 | 86.40 | 1.972 (0.943, 4.144) | 0.071 |
| Variable | Cases | Willing to Be Vaccinated | OR (95%CI) | p Value | |
|---|---|---|---|---|---|
| N | % | ||||
| Number of male sexual partners (last 6 months) | |||||
| 0 | 490 | 374 | 76.33 | Reference | |
| 1 | 306 | 272 | 88.89 | 2.481 (1.659, 3.797) | <0.001 |
| >1 | 173 | 156 | 90.17 | 2.846 (1.697, 5.051) | <0.001 |
| Number of female sexual partners (last 6 months) | |||||
| 0 | 703 | 628 | 84.52 | Reference | |
| 1 | 197 | 155 | 78.68 | 0.676 (0.458, 1.011) | 0.052 |
| >1 | 29 | 19 | 65.52 | 0.348 (0.161, 0.797) | 0.009 |
| History of STD testing | |||||
| No | 514 | 400 | 77.82 | Reference | |
| Yes | 455 | 402 | 88.35 | 2.162 (1.525, 3.099) | <0.001 |
| History of HIV testing | |||||
| No | 448 | 341 | 76.12 | Reference | |
| Yes | 521 | 461 | 88.48 | 2.411 (1.712, 3.422) | <0.001 |
| Diagnosed with an STD (last 6 months) | |||||
| No | 852 | 694 | 81.46 | Reference | |
| Yes | 117 | 108 | 92.31 | 2.732 (1.429, 5.910) | 0.005 |
| Variable | Cases | Willing to Be Vaccinated | OR (95% CI) | p Value | |
|---|---|---|---|---|---|
| N | % | ||||
| HPV/vaccine knowledge level | |||||
| Medium/low level | 481 | 361 | 75.05 | Reference | |
| High level | 488 | 441 | 90.37 | 3.119 (2.180, 4.528) | <0.001 |
| HPV risk perception level | |||||
| Low level | 504 | 390 | 77.38 | Reference | |
| Medium level | 293 | 248 | 84.64 | 1.611 (1.109, 2.374) | 0.020 |
| High level | 172 | 164 | 95.35 | 5.992 (3.040, 13.608) | <0.001 |
| HPV threat perception level | |||||
| Low level | 305 | 224 | 73.44 | Reference | |
| Medium level | 305 | 250 | 81.97 | 1.644 (1.119, 2.429) | 0.012 |
| High level | 359 | 328 | 91.36 | 3.826 (2.470, 6.060) | <0.001 |
| Attitudes to vaccine promotion | |||||
| Against | 14 | 6 | 42.86 | Reference | |
| Neutral | 127 | 62 | 48.82 | 1.272 (0.419, 4.061) | 0.6723 |
| Approve | 828 | 734 | 88.65 | 10.411 (3.546, 32.242) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Q.; Zhou, T.; Zhong, X. Factors Related to HPV Vaccination Intention among MSM in China: A Bayesian Network Model. Int. J. Environ. Res. Public Health 2022, 19, 15532. https://doi.org/10.3390/ijerph192315532
Chen Q, Zhou T, Zhong X. Factors Related to HPV Vaccination Intention among MSM in China: A Bayesian Network Model. International Journal of Environmental Research and Public Health. 2022; 19(23):15532. https://doi.org/10.3390/ijerph192315532
Chicago/Turabian StyleChen, Qiao, Tianyi Zhou, and Xiaoni Zhong. 2022. "Factors Related to HPV Vaccination Intention among MSM in China: A Bayesian Network Model" International Journal of Environmental Research and Public Health 19, no. 23: 15532. https://doi.org/10.3390/ijerph192315532
APA StyleChen, Q., Zhou, T., & Zhong, X. (2022). Factors Related to HPV Vaccination Intention among MSM in China: A Bayesian Network Model. International Journal of Environmental Research and Public Health, 19(23), 15532. https://doi.org/10.3390/ijerph192315532





