Development of the Korean Medicine Core Outcome Set for Primary Dysmenorrhea (COS-PD-KM) for Herbal Medicine Treatment of Primary Dysmenorrhea in Primary Clinics
Abstract
1. Introduction
2. Methods
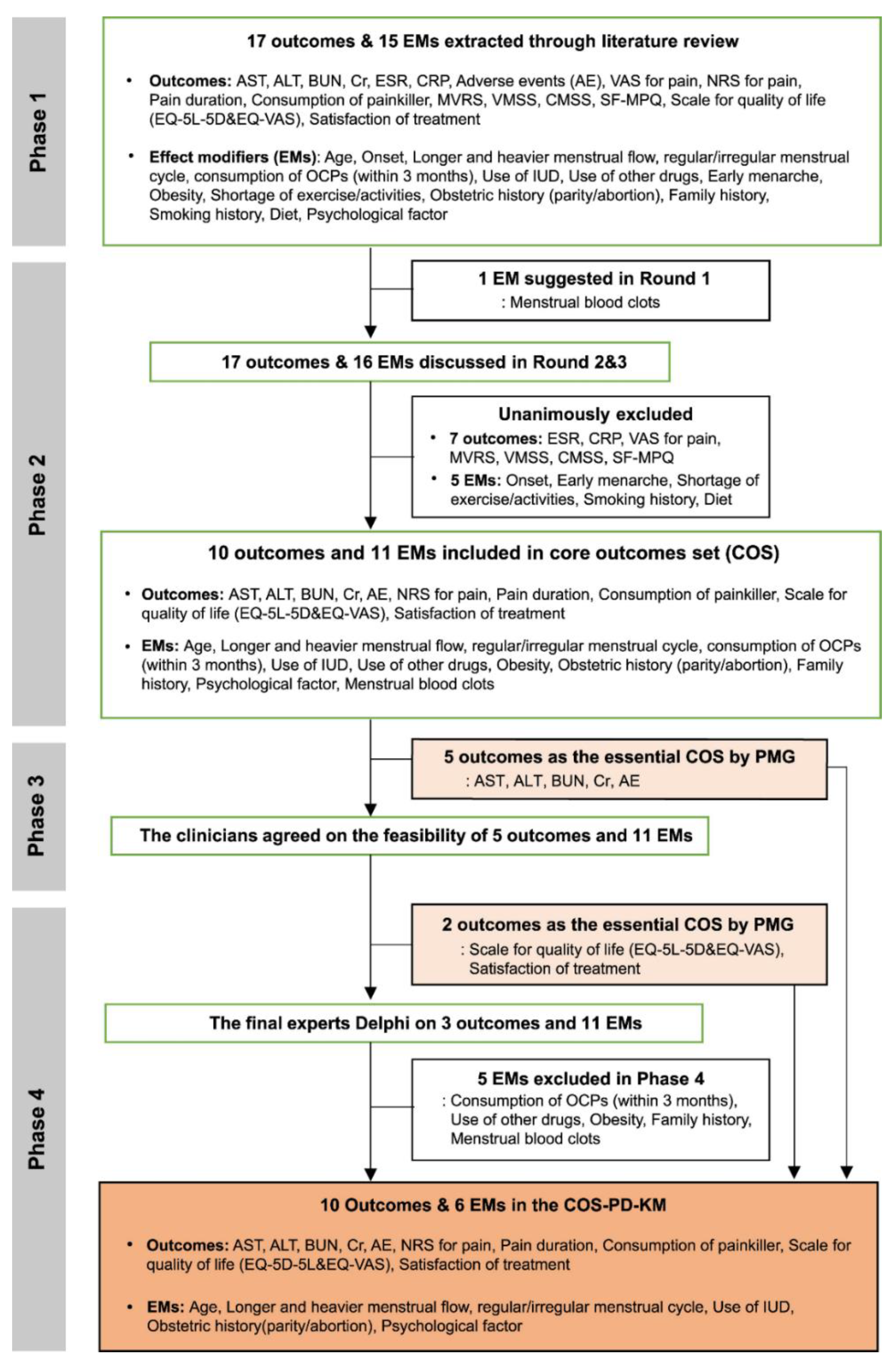
2.1. Phase 1: Establishing a Study Advisory Group and Generating a Comprehensive List of Outcomes and EMs
2.2. Phase 2: Consensus in Experts
2.3. Phase 3: Consensus in Primary Clinicians
2.4. Phase 4: Final Consensus in Experts
2.5. Data Analysis
2.5.1. Phase 2: Consensus among Experts
2.5.2. Phase 3: Consensus among Primary Clinicians
2.5.3. Phase 4: Final Consensus among Experts
2.6. Ethics and Consent
3. Results
3.1. Phase 1: Generating and Refining a Comprehensive List of Outcomes and EMs
3.2. Phase 2: Consensus among Experts
3.3. Phase 3: Consensus among Primary Clinicians
3.4. Phase 4: Final Consensus in Experts
4. Discussion
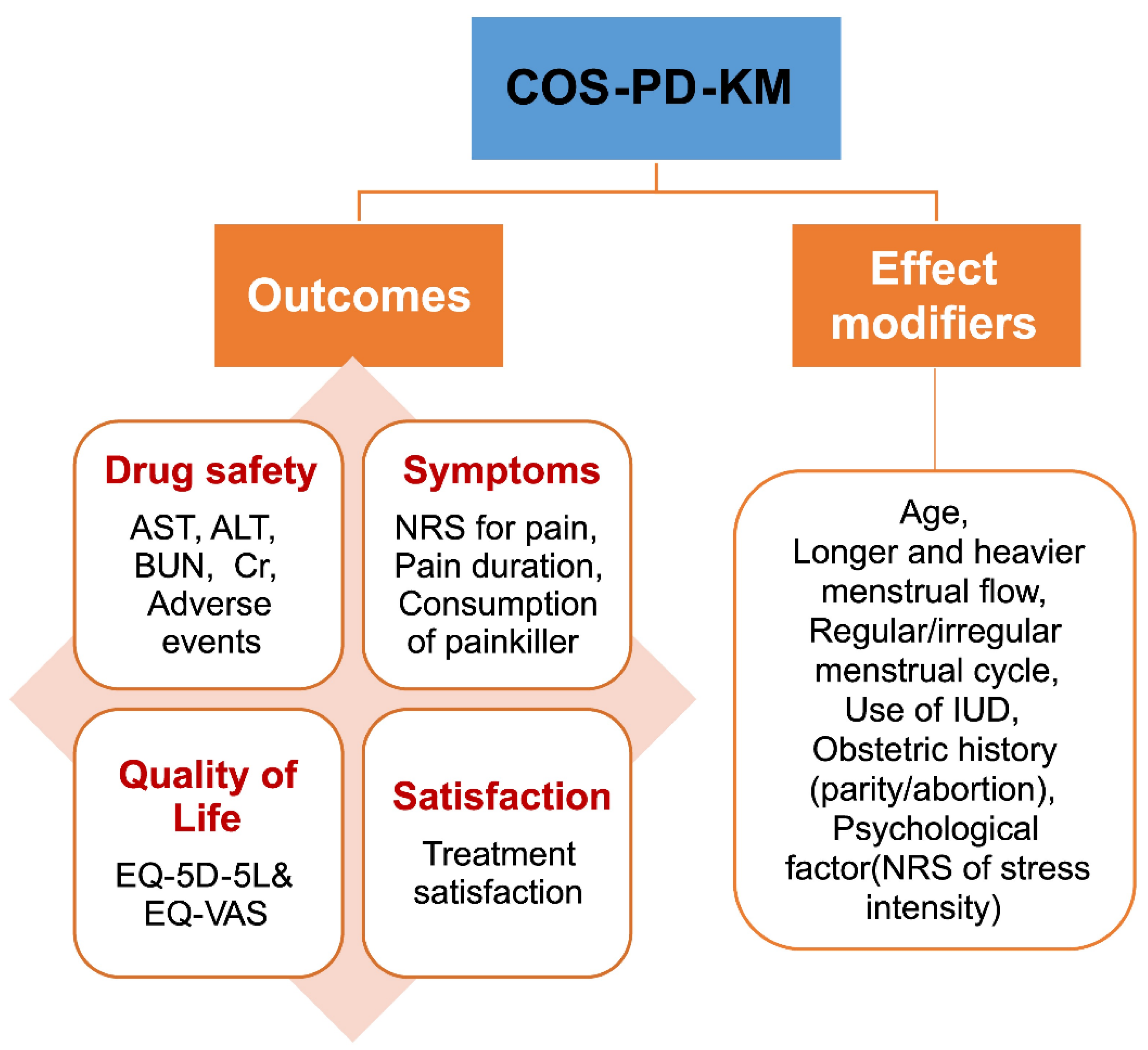
4.1. Summary of the Main Results
4.2. Considerations for COS Development
4.3. Outcomes Included in the COS and Their Implications
4.4. Implications for the Development Process
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Dawood, M.Y. Primary dysmenorrhea: Advances in pathogenesis and management. Obstet. Gynecol. 2006, 108, 428–441. [Google Scholar] [CrossRef] [PubMed]
- Ju, H.; Jones, M.; Mishra, G. The Prevalence and Risk Factors of Dysmenorrhea. Epidemiol. Rev. 2013, 36, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Morrow, C.; Naumburg, E.H. Dysmenorrhea. Prim. Care Clin. Off. Pract. 2009, 36, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Marjoribanks, J.; Ayeleke, R.O.; Farquhar, C.; Proctor, M. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst. Rev. 2015, 2015, CD001751. [Google Scholar] [CrossRef] [PubMed]
- Sharghi, M.; Mansurkhani, S.M.; Ashtary-Larky, D.; Kooti, W.; Niksefat, M.; Firoozbakht, M.; Behzadifar, M.; Azami, M.; Servatyari, K.; Jouybari, L. An update and systematic review on the treatment of primary dysmenorrhea. JBRA Assist. Reprod. 2019, 23, 51–57. [Google Scholar] [CrossRef]
- Jun, J.H.; Lee, H.W.; Choi, J.; Choi, T.Y.; Lee, J.A.; Go, H.Y.; Lee, M.S. Perceptions of using herbal medicines for managing menopausal symptoms: A web-based survey of Korean medicine doctors. Integr. Med. Res. 2019, 8, 229–233. [Google Scholar] [CrossRef]
- Lee, H.W.; Choi, T.Y.; Lee, M.S.; Lee, J.A.; Jun, J.H.; Choi, J.; Ang, L.; Lee, C.H.; Lee, J.M.; Park, K.S.; et al. Prescription patterns of herbal medicine for menopausal disorders in major Korean medicine hospitals: A multicenter retrospective study. Integr. Med. Res. 2020, 10, 100706. [Google Scholar] [CrossRef]
- Lee, J.W.; Hyun, M.K.; Kim, H.J.; Kim, D.I. Acupuncture and herbal medicine for female infertility: An overview of systematic reviews. Integr. Med. Res. 2020, 10, 100694. [Google Scholar] [CrossRef]
- Jun, J.H.; Choi, T.Y.; Lee, J.A.; Yun, K.J.; Lee, M.S. Herbal medicine (Gan Mai Da Zao decoction) for depression: A systematic review and meta-analysis of randomized controlled trials. Maturitas 2014, 79, 370–380. [Google Scholar] [CrossRef]
- Lee, H.; Choi, T.Y.; Myung, C.S.; Lee, J.A.; Lee, M.S. Herbal medicine (Shaofu Zhuyu decoction) for treating primary dysmenorrhea: A systematic review of randomized clinical trials. Maturitas 2016, 86, 64–73. [Google Scholar] [CrossRef]
- Lee, H.W.; Jun, J.H.; Kil, K.J.; Ko, B.S.; Lee, C.H.; Lee, M.S. Herbal medicine (Danggui Shaoyao San) for treating primary dysmenorrhea: A systematic review and meta-analysis of randomized controlled trials. Maturitas 2015, 85, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Woo, H.; Ji, H.; Park, K.; Hwang, D.; Lee, C.; Jang, J. A Survey on Korean Medicine Doctors’ Recognition and Clinical Fields of Treating Primary Dysmenorrhea for Developing Korean Medicine Clinical Practice Guideline for Dysmenorrhea. J. Korean Obstet. Gynecol. 2017, 30, 93–106. [Google Scholar]
- Park, K.S.; Park, K.I.; Hwang, D.S.; Lee, J.M.; Jang, J.B.; Lee, C.H. A review of in vitro and in vivo studies on the efficacy of herbal medicines for primary dysmenorrhea. Evid.-Based Complement. Altern. Med. 2014, 2014, 296860. [Google Scholar] [CrossRef] [PubMed]
- Zheng, W.; Li, M.; Wang, Y.; Lv, B.; Zhang, X.; Chen, L.; Zhu, K.; Wang, Z.; Li, B.; Xiao, W. Guizhi fuling capsule exhibits antidysmenorrhea activity by inhibition of cyclooxygenase activity. Evid.-Based Complement. Altern. Med. 2020, 2020, 8607931. [Google Scholar] [CrossRef]
- Ma, H.; Su, S.; Duan, J.; Tang, Y.; Zhou, J.; Guo, J.; Zhan, Z. Evaluation of the analgesic activities of the crude aqueous extract and fractions of Shao Fu Zhu Yu decoction. Pharm. Biol. 2011, 49, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Liang, N.; Gao, L.; Jia, C. Danggui Sini Decoction (herbal medicine) for the treatment of primary dysmenorrhoea: A systematic review and meta-analysis. J. Obstet. Gynecol. 2020, 41, 1001–1009. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Proctor, M.; Bensoussan, A.; Smith, C.A.; Wu, E. Chinese herbal medicine for primary dysmenorrhoea. Cochrane Database Syst. Rev. 2007, 17, CD005288. [Google Scholar] [CrossRef]
- Kirkham, J.; Gorst, S.; Altman, D.G.; Blazeby, J.; Clarke, M.; Devane, D.; Gargon, E.; Moher, D.; Schmitt, J.; Tugwell, P.; et al. Core Outcome Set–STAndards for Reporting: The COS-STAR Statement. PLoS Med. 2016, 13, e1002148. [Google Scholar] [CrossRef]
- Ayre, C.; Scally, A.J. Critical Values for Lawshe’s Content Validity Ratio. Meas. Eval. Couns. Dev. 2014, 47, 79–86. [Google Scholar] [CrossRef]
- Jang, S.K.; Kwon, C.S. Setting on Aims of Elementary Science Gifted Classes and Teaching Professionalism of Elementary Science Gifted Teachers through Delphi Method. J. Korean Soc. Earth Sci. Educ. 2014, 7, 99–109. [Google Scholar] [CrossRef]
- Cha, J.; Kim, S.; Kim, P.W.; Lee, H.; Ko, M.M.; Jang, S.; Lee, M.S. Development of the Korean Medicine Core Outcome Set for Stroke Sequelae: Herbal Medicine Treatment of Elderly Patients With Stroke Sequelae in Primary Clinics. Front. Pharmacol. 2022, 13, 868662. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Choi, S. A case report of the registry of herbal decoction for weight loss using a Practice-Based Research Network. Korean Herb. Med. Inf. 2021, 9, 109–118. [Google Scholar]
- Sellers, R.V.; Salazar, R.; Martinez, C.; Gelfond, S.D.; Deuter, M.; Hayes, H.G.; Ketchum, N.; Pollock, B.H. Difficult Encounters with Psychiatric Patients: A South Texas Psychiatry Practice-based Research Network (PBRN) Study. J. Am. Board Fam. Med. 2012, 25, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Bajalan, Z.; Moafi, F.; MoradiBaglooei, M.; Alimoradi, Z. Mental health and primary dysmenorrhea: A systematic review. J. Psychosom. Obstet. Gynecol. 2018, 40, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Iacovides, S.; Avidon, I.; Baker, F.C. What we know about primary dysmenorrhea today: A critical review. Hum. Reprod. Update 2015, 21, 762–778. [Google Scholar] [CrossRef] [PubMed]
- Kho, K.A.; Shields, J.K. Diagnosis and Management of Primary Dysmenorrhea. JAMA 2020, 323, 268. [Google Scholar] [CrossRef]
- Leem, J.; Kim, K.I.; Seo, J.H.; Cheong, M.J.; Youn, I. Korean medicine doctors’ views on Western medicine and Korean medicine collaborative treatment in Korea: Study protocol for a qualitative study. Eur. J. Integr. Med. 2020, 37, 101141. [Google Scholar] [CrossRef]
- Ryu, J.S.; Lim, B.M.; Cho, B.M.; Lee, W.C.; Yoon, T.H. Consciousness on cooperative practices between doctors who working in cooperative practicing hospitals and general hospital. J. Soc. Prev. Korean Med. 2009, 13, 29–41. [Google Scholar]
- Chung, V.C.; Hillier, S.; Lau, C.H.; Wong, S.Y.S.; Yeoh, E.K.; Griffiths, S.M. Referral to and attitude toward traditional Chinese medicine among western medical doctors in postcolonial Hong Kong. Soc. Sci. Med. 2011, 72, 247–255. [Google Scholar] [CrossRef]
- Lim, J.; Yun, Y.; Lee, S.Y.; Cho, Y.; Chae, H. Perspectives on Medical Services Integration among Conventional Western, Traditional Korean, and Dual-Licensed Medical Doctors in Korea. Evid.-Based Complement. Altern. Med. 2013, 2013, 105413. [Google Scholar] [CrossRef]
- Gao, L.; Jia, C.; Zhang, H.; Ma, C. Wenjing decoction (herbal medicine) for the treatment of primary dysmenorrhea: A systematic review and meta-analysis. Arch. Gynecol. Obstet. 2017, 296, 679–689. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.R.; Park, K.S.; Woo, H.L.; Lee, M.J.; Yoon, J.G.; Lee, H.J.; Hwang, D.S.; Lee, C.H.; Jang, J.B.; Lee, J.M. Herbal medicine (Taohong Siwu Tang) for the treatment of primary dysmenorrhea: A systematic review and meta-analysis. Explore. 2020, 16, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Ang, L.; Lee, M.S.; Alimoradi, Z.; Kim, E. Fennel for Reducing Pain in Primary Dysmenorrhea: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients. 2020, 12, 3438. [Google Scholar] [CrossRef]
- Leem, J.; Jo, J.; Kwon, C.Y.; Lee, H.; Park, K.S.; Lee, J.M. Herbal medicine (Hyeolbuchukeo-tang or Xuefu Zhuyu decoction) for treating primary dysmenorrhea: A systematic review and meta-analysis of randomized controlled trials. Medicine. 2020, 98, e14170. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Liu, A.; Lin, M.; Liao, S.; Wen, Z. Chinese herbal formula siwutang for treating primary dysmenorrhea: A systematic review and meta-analysis of randomized controlled trials. Maturitas. 2020, 138, 26–35. [Google Scholar] [CrossRef]
- Seo, J.; Lee, H.; Lee, D.; Jo, H.G. Dangguijagyag-san for primary dysmenorrhea: A PRISMA-compliant systematic review and meta-analysis of randomized-controlled trials. Medicine. 2020, 99, e22761. [Google Scholar] [CrossRef]
- Xu, Y.; Yang, Q.; Wang, X. Efficacy of herbal medicine (cinnamon/fennel/ginger) for primary dysmenorrhea: A systematic review and meta-analysis of randomized controlled trials. J. Int. Med. Res. 2020, 8, 300060520936179. [Google Scholar] [CrossRef]
| List of Outcomes and Effect Modifiers | Step 1: Literature Review (10 SRs) | Step 2: Further Reviews on Related Literature | Step 3: PMG Discussions (Outcomes Discussed in Phase 2) |
|---|---|---|---|
| Outcomes | |||
| Aspartate transaminase | ○ | ○ | ○ |
| Alanine transaminase | ○ | ○ | ○ |
| Blood urea nitrogen | ○ | ○ | ○ |
| Creatinine | ○ | ○ | ○ |
| Erythrocyte sedimentation rate | ○ | ○ | ○ |
| C-reactive protein | ○ | ○ | ○ |
| Adverse events | ○ | ○ | |
| Visual analog scale for pain | ○ | ○ | ○ |
| Numeric rating scale for pain | ○ | ○ | ○ |
| Pain duration for one menstrual cycle | ○ | ○ | |
| Consumption of painkiller for one menstrual cycle | ○ | ○ | |
| Multidimensional Verbal Rating Scale | ○ | ○ | |
| Verbal Multidimensional Scoring System | ○ | ○ | |
| COX Menstrual Symptom Scale | ○ | ○ | |
| McGill Pain Questionnaire | ○ | ○ | ○ |
| Brief Pain Questionnaire | ○ | Not specific to PD and similar to NRS | |
| Depression as an associated symptom | ○ | Discussed that it is more suitable as effect modifier | |
| Scale for quality of life (QoL) (12-Item Short Form Survey or 36-Item Short Form Survey) | ○ | Difficult to assess in KM primary clinic | |
| Scale for QoL (EuroQol-5 Dimensions-5 Level) | ○ | ○ | |
| Satisfaction with treatment | ○ | ○ | |
| Effect modifiers | |||
| Age | ○ | ○ | |
| Onset of primary dysmenorrhea | ○ | ○ | |
| Longer and heavier menstrual flow | ○ | ○ | |
| Regular/irregular menstrual cycle | ○ | ○ | |
| Consumption of drug interaction oral contraceptive pill (within 3 months) | ○ | ○ | |
| Use of intrauterine devices | ○ | ○ | |
| Use of other drugs | ○ | ○ | |
| Age of menarche (early menarche) | ○ | ○ | |
| Obesity (including body mass index) | ○ | ○ | |
| Shortage of exercise/activities | ○ | ○ | |
| Obstetric history (parity/abortion) | ○ | ○ | |
| Family history | ○ | ○ | |
| Smoking history | ○ | ○ | |
| Diet (repeated intake of caffeine, dairy products, omega-3, etc.) | ○ | ○ | |
| Psychological factors (anxiety, depression, stress) | ○ | ○ |
| Category | Question | Mean | Median | Degree of Consensus | Degree of Convergence |
|---|---|---|---|---|---|
| Outcomes | NRS for pain | 8.27 | 9.00 | 0.89 | 0.50 |
| Pain duration | 6.73 | 7.00 | 0.50 | 1.75 | |
| Consumption of painkiller | 7.09 | 7.00 | 0.64 | 1.25 | |
| Satisfaction of treatment | 7.73 | 8.00 | 0.88 | 0.50 | |
| Quality of life (EQ-5D-5 L and EQ-VAS) | 5.36 | 6.00 | 0.58 | 1.25 | |
| Effect modifiers about menstrual/related gynecological history | Age; Longer and heavier menstrual flow; Regular/irregular menstrual cycle; Consumption of drug interaction oral contraceptive pill (within 3 months); Use of intrauterine devices; Use of other drugs; Obesity (including body mass index); Obstetric history (parity/abortion); Family history; Psychological factor (anxiety, depression, stress); Menstrual blood clots | 7.27 | 8.00 | 0.75 | 1.00 |
| Category/Question | Mean | Median | Degree of Consensus | Degree of Convergence |
|---|---|---|---|---|
| Outcomes | ||||
| NRS for pain | 4 | 4 | 1 | 0 |
| Pain duration for one menstrual cycle | 3.25 | 4 | 1 | 0 |
| Consumption of pain killers for one menstrual cycle | 3.5 | 4 | 0.75 | 0.5 |
| Effect modifiers | ||||
| Age | 3.2 | 4 | 0.75 | 0.5 |
| Longer and heavier menstrual flow | 3.25 | 4 | 0.75 | 0.5 |
| Regular/irregular menstrual cycle | 4 | 4 | 1 | 0 |
| Consumption of OCPs (within 3 months) | 2.6 | 3 | 0 | 1.5 |
| Use of IUD | 3.6 | 4 | 0.75 | 0.5 |
| Use of other drugs | 2.4 | 3 | 0.33 | 1 |
| Obesity (including BMI) | 2 | 2 | 0 | 1 |
| Obstetric history (parity/abortion) | 2.2 | 4 | 0.75 | 0.5 |
| Family history | 2.2 | 3 | 0.33 | 1 |
| Psychological factor (NRS of stress intensity) | 3.6 | 4 | 0.75 | 0.5 |
| Menstrual blood clots | 2.6 | 3 | 0 | 1.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, P.-W.; Kim, S.; Kim, D.-I.; Cha, J.; Lee, H.-S.; Ko, M.M.; Jang, S.; Yang, C.; Lee, M.S. Development of the Korean Medicine Core Outcome Set for Primary Dysmenorrhea (COS-PD-KM) for Herbal Medicine Treatment of Primary Dysmenorrhea in Primary Clinics. Int. J. Environ. Res. Public Health 2022, 19, 15321. https://doi.org/10.3390/ijerph192215321
Kim P-W, Kim S, Kim D-I, Cha J, Lee H-S, Ko MM, Jang S, Yang C, Lee MS. Development of the Korean Medicine Core Outcome Set for Primary Dysmenorrhea (COS-PD-KM) for Herbal Medicine Treatment of Primary Dysmenorrhea in Primary Clinics. International Journal of Environmental Research and Public Health. 2022; 19(22):15321. https://doi.org/10.3390/ijerph192215321
Chicago/Turabian StyleKim, Pyung-Wha, Sungha Kim, Dong-Il Kim, Jiyun Cha, He-Sol Lee, Mi Mi Ko, Soobin Jang, Changsop Yang, and Myeong Soo Lee. 2022. "Development of the Korean Medicine Core Outcome Set for Primary Dysmenorrhea (COS-PD-KM) for Herbal Medicine Treatment of Primary Dysmenorrhea in Primary Clinics" International Journal of Environmental Research and Public Health 19, no. 22: 15321. https://doi.org/10.3390/ijerph192215321
APA StyleKim, P.-W., Kim, S., Kim, D.-I., Cha, J., Lee, H.-S., Ko, M. M., Jang, S., Yang, C., & Lee, M. S. (2022). Development of the Korean Medicine Core Outcome Set for Primary Dysmenorrhea (COS-PD-KM) for Herbal Medicine Treatment of Primary Dysmenorrhea in Primary Clinics. International Journal of Environmental Research and Public Health, 19(22), 15321. https://doi.org/10.3390/ijerph192215321







