Social Connectedness, Physical Distancing, and Anxiety in Complying with Shelter-In-Place Orders and Advisories during the Once-In-A-Century COVID-19 Pandemic in the US: A Study of Social Media and Internet Users
Abstract
1. Introduction
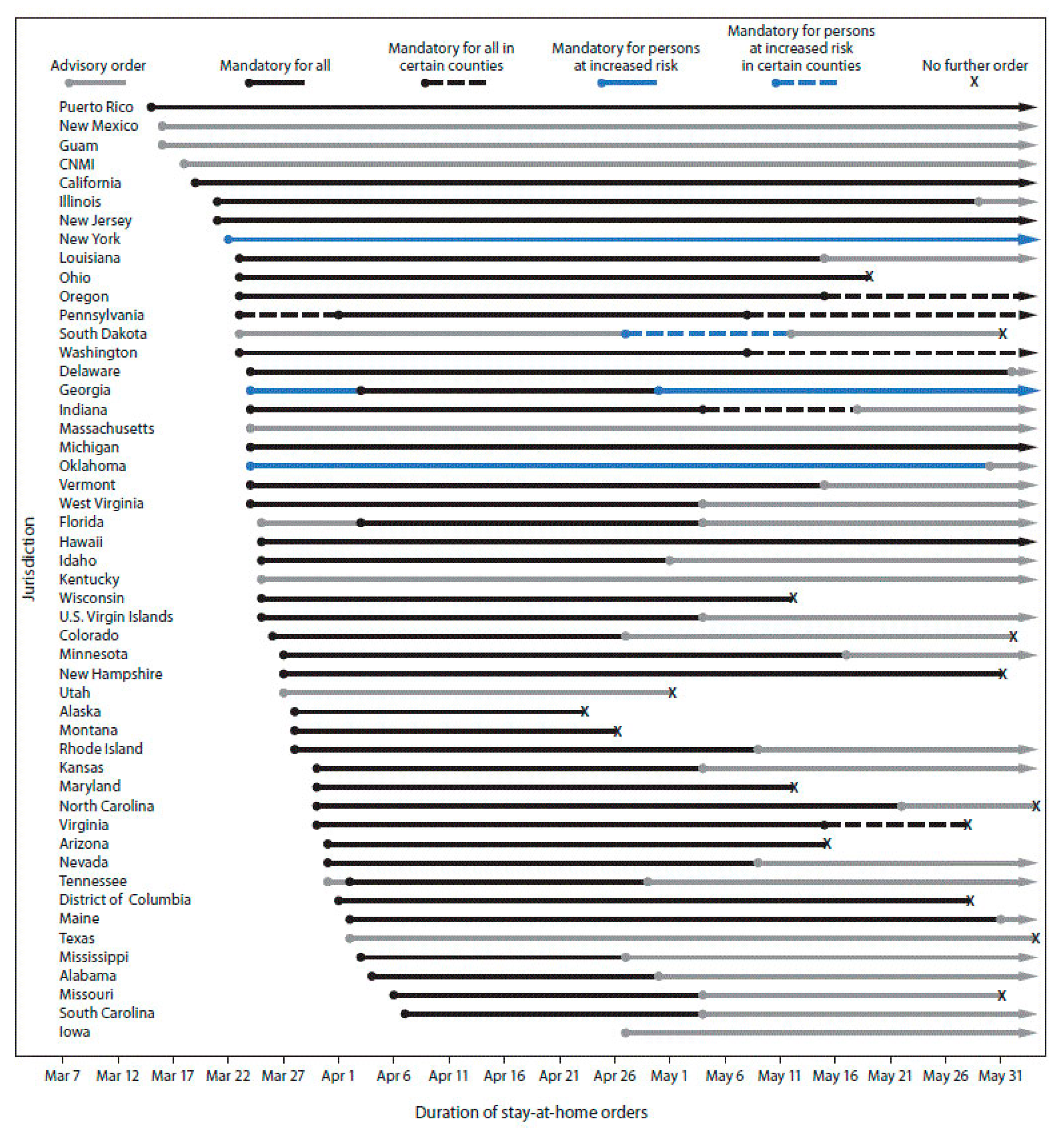
1.1. Physical Distancing
1.2. Anxiety
1.3. Social Connectedness
2. Materials and Methods
2.1. Sample
2.2. Measures
2.2.1. Physical Distancing
2.2.2. Social Connectedness
2.2.3. Anxiety
2.2.4. Socio-Demographic Variables
2.3. Structural Equation Modeling
3. Results
3.1. Descriptive Statistics
3.2. SEM Results
4. Discussion
Caveats and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B. Survey Instrument
- Physical distancing
- First day you stayed home. If you can’t remember the exact date, enter an approximate date
- Last day you stayed home. If you can’t remember the exact date, enter an approximate date
- Shelter in place compliance
- I can safely stay in my home for at least 15 days.
- Race
- Choose one or more of the following categories that best describe your race.
- Ethnicity
- 2.
- Do you consider yourself to be of Hispanic, Latino/a, or Spanish origin?
- Age
- 3.
- What is your age? years
- Number of people at home
- 4.
- What is the total number of people that live in your home? include yourself, all other adults and children
- 65 years and older
- 5.
- Of the total number of people in your household, how many are 65 years of age or older?
- Employment status
- 6.
- Which best describes your employment status?
- Income
- 7.
- What is your annual household income from all sources?
- Zip code
- 8.
- What is the zip code of your current address?
- Generalized Anxiety Disorder
- Feeling nervous, anxious, or on edge
- Not being able to stop or control worrying
- Worrying too much about different things
- Trouble relaxing
- Being so restless that its hard to sit still
- Becoming easily annoyed or irritable
- Feeling afraid as if something awful might happen
- Social Provisions Scale
- 8.
- There are people I can depend on to help me if I really need it.
- 9.
- There are people who enjoy the same social activities I do.
- 10.
- I have close relationships that provide me with a sense of emotional security and well-being.
- 11.
- There is someone I could talk to about important decisions in my life.
- 12.
- I have relationships where my competence and skills are recognized.
- 13.
- There is a trustworthy person I could turn to for advice if I were having problems.
- 14.
- I feel part of a group of people who share my attitudes and beliefs.
- 15.
- I feel a strong emotional bond with at least one other person.
- 16.
- There are people who admire my talents and abilities.
- 17.
- There are people I can count on in an emergency.
- Family Support
- 18.
- Planning family activities is difficult because we misunderstand each other.
- 19.
- In time of crisis we can turn to each other for support.
- 20.
- We cannot talk to each other about sadness we feel.
- 21.
- Individuals are accepted for what they are.
- 22.
- We avoid discussing our fears and concerns.
- 23.
- We can express feelings to each other.
- 24.
- There are lots of bad feelings in the family.
- 25.
- We feel accepted for what we are.
- 26.
- Making decisions is a problem for our family.
- 27.
- We are able to make decisions about how to solve problems.
- 28.
- We don’t get along well together.
- 29.
- We confide in each other.
Appendix C
| No. | State Name | SFIPS | No. of Participants | % Total |
|---|---|---|---|---|
| 1 | Alabama | 1 | 1 | 0.20% |
| 2 | Arizona | 4 | 1 | 0.20% |
| 3 | California | 6 | 4 | 0.81% |
| 4 | Colorado | 8 | 1 | 0.20% |
| 5 | Florida | 12 | 2 | 0.40% |
| 6 | Georgia | 13 | 2 | 0.40% |
| 7 | Illinois | 17 | 6 | 1.21% |
| 8 | Kentucky | 21 | 5 | 1.01% |
| 9 | Maryland | 24 | 2 | 0.40% |
| 10 | Massachusetts | 25 | 1 | 0.20% |
| 11 | Michigan | 26 | 3 | 0.61% |
| 12 | Missouri | 29 | 3 | 0.61% |
| 13 | New Jersey | 34 | 2 | 0.40% |
| 14 | New Mexico | 35 | 2 | 0.40% |
| 15 | New York | 36 | 8 | 1.62% |
| 16 | North Carolina | 37 | 6 | 1.21% |
| 17 | Ohio | 39 | 3 | 0.61% |
| 18 | Oklahoma | 40 | 3 | 0.61% |
| 19 | Oregon | 41 | 4 | 0.81% |
| 20 | Pennsylvania | 42 | 6 | 1.21% |
| 21 | South Carolina | 45 | 1 | 0.20% |
| 22 | Tennessee | 47 | 3 | 0.61% |
| 23 | Texas | 48 | 396 | 80.16% |
| 24 | Virginia | 51 | 7 | 1.42% |
| 25 | Washington | 53 | 9 | 1.82% |
| 26 | West Virginia | 54 | 2 | 0.40% |
| 27 | Wisconsin | 55 | 2 | 0.40% |
| 28 | Unknown zip code | 9 | 1.82% | |
| Total | 494 | 100.00% |
| Physical Distancing (days) | 0–15 | 16–30 | 31–45 | 46–60 | 61–75 | 76 or More | Total |
|---|---|---|---|---|---|---|---|
| 1. Race | |||||||
| Color | 3 | 11 | 13 | 12 | 13 | 11 | 63 |
| 4.76 | 17.46 | 20.63 | 19.05 | 20.63 | 17.46 | 100 | |
| White | 20 | 120 | 134 | 67 | 45 | 45 | 431 |
| 4.64 | 27.84 | 31.09 | 15.55 | 10.44 | 10.44 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 2. Ethnicity | |||||||
| Non-Hispanic | 10 | 67 | 70 | 31 | 15 | 14 | 207 |
| 4.83 | 32.37 | 33.82 | 14.98 | 7.25 | 6.76 | 100 | |
| Hispanic | 13 | 64 | 77 | 48 | 43 | 42 | 287 |
| 4.53 | 22.3 | 26.83 | 16.72 | 14.98 | 14.63 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 3. Gender | |||||||
| Male | 7 | 19 | 29 | 21 | 15 | 12 | 103 |
| 6.8 | 18.45 | 28.16 | 20.39 | 14.56 | 11.65 | 100 | |
| Female | 16 | 112 | 114 | 58 | 43 | 44 | 387 |
| 4.13 | 28.94 | 29.46 | 14.99 | 11.11 | 11.37 | 100 | |
| Total | 23 | 131 | 143 | 79 | 58 | 56 | 490 |
| 4.69 | 26.73 | 29.18 | 16.12 | 11.84 | 11.43 | 100 | |
| 4. Age | |||||||
| 18 to 19 | 0 | 0 | 5 | 2 | 4 | 4 | 15 |
| 0 | 0 | 33.33 | 13.33 | 26.67 | 26.67 | 100 | |
| 20 to 29 | 6 | 17 | 34 | 24 | 20 | 17 | 118 |
| 5.08 | 14.41 | 28.81 | 20.34 | 16.95 | 14.41 | 100 | |
| 30 to 39 | 6 | 34 | 36 | 15 | 10 | 11 | 112 |
| 5.36 | 30.36 | 32.14 | 13.39 | 8.93 | 9.82 | 100 | |
| 40 to 49 | 3 | 32 | 25 | 11 | 11 | 15 | 97 |
| 3.09 | 32.99 | 25.77 | 11.34 | 11.34 | 15.46 | 100 | |
| 50 to 59 | 3 | 28 | 22 | 13 | 10 | 3 | 79 |
| 3.8 | 35.44 | 27.85 | 16.46 | 12.66 | 3.8 | 100 | |
| 60 and older | 5 | 20 | 25 | 14 | 3 | 6 | 73 |
| 6.85 | 27.4 | 34.25 | 19.18 | 4.11 | 8.22 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 5. Number of people at home | |||||||
| 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 2 | 9 | 55 | 59 | 28 | 19 | 12 | 182 |
| 4.95 | 30.22 | 32.42 | 15.38 | 10.44 | 6.59 | 100 | |
| 3 | 5 | 33 | 28 | 16 | 11 | 16 | 109 |
| 4.59 | 30.28 | 25.69 | 14.68 | 10.09 | 14.68 | 100 | |
| 4 | 3 | 28 | 33 | 13 | 16 | 16 | 109 |
| 2.75 | 25.69 | 30.28 | 11.93 | 14.68 | 14.68 | 100 | |
| 5 | 2 | 10 | 14 | 15 | 6 | 7 | 54 |
| 3.7 | 18.52 | 25.93 | 27.78 | 11.11 | 12.96 | 100 | |
| 6 | 4 | 5 | 13 | 7 | 6 | 5 | 40 |
| 10 | 12.5 | 32.5 | 17.5 | 15 | 12.5 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 6. Number of people 65 or older at home | |||||||
| 0 | 17 | 99 | 116 | 54 | 46 | 42 | 374 |
| 4.55 | 26.47 | 31.02 | 14.44 | 12.3 | 11.23 | 100 | |
| 1 | 4 | 20 | 13 | 15 | 9 | 11 | 72 |
| 5.56 | 27.78 | 18.06 | 20.83 | 12.5 | 15.28 | 100 | |
| 2 | 2 | 10 | 18 | 10 | 3 | 3 | 46 |
| 4.35 | 21.74 | 39.13 | 21.74 | 6.52 | 6.52 | 100 | |
| 3 | 0 | 2 | 0 | 0 | 0 | 0 | 2 |
| 0 | 100 | 0 | 0 | 0 | 0 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 7. Family Support | |||||||
| Low | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Moderate | 0 | 0 | 1 | 0 | 1 | 0 | 2 |
| 0 | 0 | 50 | 0 | 50 | 0 | 100 | |
| High | 20 | 114 | 114 | 65 | 44 | 49 | 406 |
| 4.93 | 28.08 | 28.08 | 16.01 | 10.84 | 12.07 | 100 | |
| Very high | 3 | 17 | 32 | 14 | 13 | 7 | 86 |
| 3.49 | 19.77 | 37.21 | 16.28 | 15.12 | 8.14 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 8. Social Provision | |||||||
| Low | 0 | 3 | 2 | 0 | 0 | 0 | 5 |
| 0 | 60 | 40 | 0 | 0 | 0 | 100 | |
| Moderate | 0 | 2 | 2 | 2 | 3 | 4 | 13 |
| 0 | 15.38 | 15.38 | 15.38 | 23.08 | 30.77 | 100 | |
| High | 5 | 17 | 31 | 15 | 13 | 9 | 90 |
| 5.56 | 18.89 | 34.44 | 16.67 | 14.44 | 10 | 100 | |
| Very high | 18 | 109 | 112 | 62 | 42 | 43 | 386 |
| 4.66 | 28.24 | 29.02 | 16.06 | 10.88 | 11.14 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 9. Anxiety | |||||||
| Mild | 11 | 60 | 80 | 43 | 24 | 22 | 240 |
| 4.58 | 25 | 33.33 | 17.92 | 10 | 9.17 | 100 | |
| Moderate | 7 | 53 | 38 | 22 | 18 | 15 | 153 |
| 4.58 | 34.64 | 24.84 | 14.38 | 11.76 | 9.8 | 100 | |
| Moderately severe | 1 | 13 | 21 | 6 | 7 | 9 | 57 |
| 1.75 | 22.81 | 36.84 | 10.53 | 12.28 | 15.79 | 100 | |
| Severe | 4 | 5 | 8 | 8 | 9 | 10 | 44 |
| 9.09 | 11.36 | 18.18 | 18.18 | 20.45 | 22.73 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 10. Compliance with stay-home order | |||||||
| Strongly | 0 | 4 | 3 | 1 | 2 | 1 | 11 |
| 0 | 36.36 | 27.27 | 9.09 | 18.18 | 9.09 | 100 | |
| Disagree | 1 | 6 | 5 | 2 | 5 | 2 | 21 |
| 4.76 | 28.57 | 23.81 | 9.52 | 23.81 | 9.52 | 100 | |
| Agree | 7 | 41 | 38 | 28 | 16 | 16 | 146 |
| 4.79 | 28.08 | 26.03 | 19.18 | 10.96 | 10.96 | 100 | |
| Strongly | 15 | 80 | 101 | 48 | 35 | 37 | 316 |
| 4.75 | 25.32 | 31.96 | 15.19 | 11.08 | 11.71 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 11. Work status | |||||||
| Not working | 4 | 21 | 39 | 19 | 16 | 17 | 116 |
| 3.45 | 18.1 | 33.62 | 16.38 | 13.79 | 14.66 | 100 | |
| Working | 19 | 110 | 108 | 60 | 42 | 39 | 378 |
| 5.03 | 29.1 | 28.57 | 15.87 | 11.11 | 10.32 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| 12. Income | |||||||
| $10000 or less | 0 | 2 | 4 | 4 | 6 | 4 | 20 |
| 0 | 10 | 20 | 20 | 30 | 20 | 100 | |
| $10,000–$19,999 | 0 | 3 | 12 | 5 | 5 | 4 | 29 |
| 0 | 10.34 | 41.38 | 17.24 | 17.24 | 13.79 | 100 | |
| $20,000–$29,999 | 2 | 5 | 5 | 5 | 6 | 3 | 26 |
| 7.69 | 19.23 | 19.23 | 19.23 | 23.08 | 11.54 | 100 | |
| $30,000–$39,999 | 1 | 8 | 17 | 3 | 4 | 7 | 40 |
| 2.5 | 20 | 42.5 | 7.5 | 10 | 17.5 | 100 | |
| $40,000–$49,999 | 1 | 7 | 8 | 5 | 3 | 4 | 28 |
| 3.57 | 25 | 28.57 | 17.86 | 10.71 | 14.29 | 100 | |
| $50,000–$59,999 | 3 | 12 | 8 | 7 | 10 | 4 | 44 |
| 6.82 | 27.27 | 18.18 | 15.91 | 22.73 | 9.09 | 100 | |
| $60,000–$69,999 | 2 | 7 | 12 | 4 | 7 | 2 | 34 |
| 5.88 | 20.59 | 35.29 | 11.76 | 20.59 | 5.88 | 100 | |
| $70,000–$79,999 | 2 | 15 | 12 | 4 | 2 | 2 | 37 |
| 5.41 | 40.54 | 32.43 | 10.81 | 5.41 | 5.41 | 100 | |
| $80,000–$89,999 | 2 | 5 | 5 | 3 | 2 | 5 | 22 |
| 9.09 | 22.73 | 22.73 | 13.64 | 9.09 | 22.73 | 100 | |
| $90,000–$99,999 | 1 | 8 | 8 | 3 | 1 | 3 | 24 |
| 4.17 | 33.33 | 33.33 | 12.5 | 4.17 | 12.5 | 100 | |
| $100,000 | 9 | 59 | 56 | 36 | 12 | 18 | 190 |
| 4.74 | 31.05 | 29.47 | 18.95 | 6.32 | 9.47 | 100 | |
| Total | 23 | 131 | 147 | 79 | 58 | 56 | 494 |
| 4.66 | 26.52 | 29.76 | 15.99 | 11.74 | 11.34 | 100 | |
| Residuals of Observed Variables | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean residuals | |||||||||||||
| Stay | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| raw | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Covariance residuals | |||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
| 1 | Physical distancing | 0 | |||||||||||
| 2 | Anxiety | 0 | 0 | ||||||||||
| 3 | Social provisions | 0 | 0 | 0 | |||||||||
| 4 | Family support | 0 | 0 | 0 | 0 | ||||||||
| 5 | Race | 0 | 0 | 0 | 0 | 0 | |||||||
| 6 | Hispanic | 0.1 | 0 | 0 | 0 | 0 | 0 | ||||||
| 7 | Age | 0 | 0 | 0 | -0.1 | 0 | 0 | 0 | |||||
| 8 | Family size | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||||
| 9 | 65 years and older | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |||
| 10 | Compliance | 0.1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ||
| 11 | Employment status | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 12 | Income | 0 | 0 | 0.2 | -0.2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fit Statistic | Value | Description |
|---|---|---|
| Likelihood ratio | ||
| chi2_ms(25) | 49.612 | model vs. saturated |
| p > chi2 | 0.0020 | |
| chi2_bs(38) | 177.157 | baseline vs. saturated |
| p > chi2 | 0.0000 | |
| Population error | ||
| RMSEA | 0.045 | Root mean squared error of approximation |
| 90% CI, lower bound | 0.026 | |
| upper bound | 0.063 | |
| pclose | 0.663 | Probability RMSEA <= 0.05 |
| Information criteria | ||
| AIC | 13,448.34 | Akaike’s |
| BIC | 13,536.593 | Bayesian |
| Baseline comparison | ||
| CFI | 0.823 | Comparative |
| TLI | 0.731 | Tucker–Lewis |
| Size of residuals | ||
| SRMR | 0.036 | Standardized |
| CD | −8.786 | Coefficient |
| No. | Study Variable | Obs | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|---|---|
| 1 | Physical distancing | 494 | 3.38 | 1.40 | 1 | 6 |
| 2 | Anxiety | 494 | 1.81 | 0.96 | 1 | 4 |
| 3 | Social provisions | 494 | 3.73 | 0.56 | 1 | 4 |
| 4 | Family support | 494 | 3.17 | 0.39 | 2 | 4 |
| 5 | Race | 494 | 0.11 | 0.31 | 0 | 1 |
| 6 | Hispanic | 494 | 0.58 | 0.49 | 0 | 1 |
| 7 | Age | 494 | 3.66 | 1.45 | 1 | 6 |
| 8 | Family size | 494 | 3.31 | 1.29 | 2 | 6 |
| 9 | 65 years and older | 494 | 0.34 | 0.66 | 0 | 3 |
| 10 | Compliance | 494 | 3.55 | 0.68 | 1 | 4 |
| 11 | Employment status | 494 | 0.77 | 0.42 | 0 | 1 |
| 12 | Income | 494 | 7.66 | 3.35 | 1 | 11 |
References
- Bar-On, Y.M.; Flamholz, A.; Phillips, R.; Milo, R. SARS-CoV-2 (COVID-19) by the numbers. Elife 2020, 9, e57309. [Google Scholar] [CrossRef] [PubMed]
- WHO. Naming the Coronavirus Disease (COVID-19) and the Virus That Causes It. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (accessed on 25 October 2020).
- US CDC. United States COVID-19 Cases and Deaths by State. Available online: https://covid.cdc.gov/covid-data-tracker/#cases_casesper100klast7days (accessed on 25 October 2020).
- USAFacts. US Coronavirus Cases and Deaths; Track COVID-19 Data Daily by State and County. Available online: https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/ (accessed on 25 October 2020).
- US CDC. How COVID-19 Spreads. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html (accessed on 25 October 2020).
- US CDC. Interim Pre-Pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States—Early, Targeted, Layered Use of Nonpharmaceutical Interventions; US Centers for Disease Control and Prevention (US CDC): Atlanta, GA, USA, 2007.
- US CDC. Nonpharmaceutical Interventions (NPIs). Available online: https://www.cdc.gov/nonpharmaceutical-interventions/index.html (accessed on 25 October 2020).
- NIH. Fourth Large-Scale COVID-19 Vaccine Trial Begins in the United States: Trial Evaluating Investigational Janssen COVID-19 Vaccine. Available online: https://www.nih.gov/news-events/news-releases/fourth-large-scale-covid-19-vaccine-trial-begins-united-states (accessed on 25 October 2020).
- Childs, M.L.; Kain, M.P.; Kirk, D.; Harris, M.; Couper, L.; Nova, N.; Delwel, I.; Ritchie, J.; Mordecai, E.A. The impact of long-term non-pharmaceutical interventions on COVID-19 epidemic dynamics and control. medRxiv 2020. [Google Scholar] [CrossRef]
- Brulliard, K. Social Distancing Is So Hard Because It’s Contrary to Human Nature. Wash. Post. 2020. Available online: https://www.washingtonpost.com/science/2020/03/17/coronavirus-social-distancing/ (accessed on 19 March 2020).
- US CDC. Coping with Stress. Available online: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html (accessed on 25 October 2020).
- Melo, M.C.A.; Soares, D.D. Impact of social distancing on mental health during the COVID-19 pandemic: An urgent discussion. Int. J. Soc. Psychiatr. 2020, 66, 625–626. [Google Scholar] [CrossRef] [PubMed]
- The White House, What Is Social Distancing? Available online: https://www.youtube.com/watch?v=Nlyxz2X97Do (accessed on 19 March 2020).
- Moreland, A.; Herlihy, C.; Tynan, M.A.; Sunshine, G.; McCord, R.F.; Hilton, C.; Poovey, J.; Werner, A.K.; Jones, C.D.; Fulmer, E.B.; et al. Timing of State and Territorial COVID-19 Stay-at-Home Orders and Changes in Population Movement—United States, March 1–May 31, 2020; US Centers for Disease Control and Prevention (CDC): Atlanta, GA, USA, 2020; pp. 1198–1203.
- Gostin, L.O.; Wiley, L.F. Governmental Public Health Powers During the COVID-19 Pandemic: Stay-at-home Orders, Business Closures, and Travel Restrictions. JAMA 2020, 323, 2137–2138. [Google Scholar] [CrossRef]
- LeBlanc, P. Fauci: ‘I Don’t Understand Why’ Every State Hasn’t Issued Stay-at-Home Orders. Available online: https://www.cnn.com/2020/04/02/politics/fauci-stay-home-coronavirus-states-cnntv/index.html (accessed on 28 October 2020).
- Malone, C.; Bourassa, K. Americans Didn’t Wait for Their Governors to Tell Them to Stay Home Because of COVID-19. Available online: https://fivethirtyeight.com/features/americans-didnt-wait-for-their-governors-to-tell-them-to-stay-home-because-of-covid-19/ (accessed on 28 October 2020).
- WV HHSD. Governor Issues Stay-at-Home Order. Available online: https://dhhr.wv.gov/COVID-19/Pages/Governor-Issues-Stay-at-Home-Order.aspx (accessed on 28 October 2020).
- Castillo, R.C.; Staguhn, E.D.; Weston-Farber, E. The effect of state-level stay-at-home orders on COVID-19 infection rates. Am. J. Infect. Control 2020, 48, 958–960. [Google Scholar] [CrossRef]
- The New York Times. See How All 50 States Are Reopening (and Closing Again); The New York Times: New York, NY, USA, 2020. [Google Scholar]
- Warren, A.M.; Zolfaghari, K.; Fresnedo, M.; Bennett, M.; Pogue, J.; Waddimba, A.; Zvolensky, M.; Carlbring, P.; Powers, M.B. Anxiety sensitivity, COVID-19 fear, and mental health: Results from a United States population sample. Cogn. Behav. Ther. 2021, 50, 204–216. [Google Scholar] [CrossRef]
- Guo, Y.Y.; Shen, M.X.; Zhang, X.; Xiao, Y.; Zhao, S.; Yin, M.Z.; Bu, W.B.; Wang, Y.; Chen, X.; Su, J. Association of Socioeconomic Changes due to the COVID-19 Pandemic With Health Outcomes in Patients With Skin Diseases: Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e22288. [Google Scholar] [CrossRef]
- Tull, M.T.; Edmonds, K.A.; Scamaldo, K.M.; Richmond, J.R.; Rose, J.P.; Gratz, K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020, 289, 113098. [Google Scholar] [CrossRef]
- Williams, S.N.; Armitage, C.J.; Tampe, T.; Dienes, K. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: A UK-based focus group study. BMJ Open 2020, 10, e039334. [Google Scholar] [CrossRef]
- Cornwell, E.Y.; Waite, L.J. Social disconnectedness, perceived isolation, and health among older adults. J. Health Soc. Behav. 2009, 50, 31–48. [Google Scholar] [CrossRef]
- Cornwell, E.Y.; Waite, L.J. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J. Gerontol. B Psychol. Sci. Soc. Sci. 2009, 64 (Suppl. S1), i38–i46. [Google Scholar] [CrossRef] [PubMed]
- Firestone, L. Coping with Loneliness During a Pandemic. Available online: https://www.psychologytoday.com/us/blog/compassion-matters/202004/coping-loneliness-during-pandemic (accessed on 10 April 2020).
- Wood, J. Pandemic Fuels Feelings of Loneliness, Anxiety in People Over 70. Available online: https://psychcentral.com/news/2020/07/25/pandemic-fuels-feelings-of-loneliness-anxiety-in-people-over-70#1 (accessed on 10 May 2022).
- Hwang, T.-J.; Rabheru, K.; Peisah, C.; Reichman, W.; Ikeda, M. Loneliness and social isolation during the COVID-19 pandemic. Int. Psychogeriatr. 2020, 32, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Petersen, A. Loneliness, Anxiety and Loss: The Covid Pandemic’s Terrible Toll on Kids. Available online: https://www.wsj.com/articles/pandemic-toll-children-mental-health-covid-school-11617969003 (accessed on 9 April 2020).
- GGSC. Social Connection Defined. Greater Good Sci. Mag. 2020. Available online: https://greatergood.berkeley.edu/topic/social_connection/definition (accessed on 19 April 2020).
- Smith, J.R. Before Coronavirus We Were Dying of Loneliness. Can a Pandemic Help America Heal? Available online: https://www.cnn.com/2020/04/17/health/loneliness-epidemic-coronavirus-healing-wellness/index.html (accessed on 17 April 2020).
- Jacobson, N.C.; Lekkas, D.; Price, G.; Heinz, M.V.; Song, M.; O’Malley, A.J.; Barr, P.J. Flattening the Mental Health Curve: COVID-19 Stay-at-Home Orders Are Associated With Alterations in Mental Health Search Behavior in the United States. JMIR Ment. Health 2020, 7, 11. [Google Scholar] [CrossRef]
- Chiu, C.-Y.; Motl, R.W.; Ditchman, N. Validation of the Social Provisions Scale in people with multiple sclerosis. Rehabil. Psychol. 2016, 61, 297–307. [Google Scholar] [CrossRef]
- Iapichino, E.; Rucci, P.; Corbani, I.E.; Apter, G.; Bollani, M.Q.; Cauli, G.; Gala, C.; Bassi, M. Development and validation of an abridged version of the Social Provisions Scale (SPS-10) in Italian. J. Psychopathol. G. Di Psicopatol. 2016, 22, 157–163. [Google Scholar]
- Durlofsky, P. How to Cope with the Emotional Effects of Social Distancing. Available online: https://mainlinetoday.com/home-slider/thinking-forward-how-to-cope-with-anxiety-social-distancing/ (accessed on 19 April 2020).
- Okabe-Miyamoto, K.; Folk, D.; Lyubomirsky, S.; Dunn, E.W. Changes in social connection during COVID-19 social distancing: It’s not (household) size that matters, it’s who you’re with. PLoS ONE 2021, 16, e0245009. [Google Scholar] [CrossRef]
- Valtorta, N.K.; Kanaan, M.; Gilbody, S.; Hanratty, B. Loneliness, social isolation and social relationships: What are we measuring? A novel framework for classifying and comparing tools. BMJ Open 2016, 6, e010799. [Google Scholar] [CrossRef]
- Hare-Duke, L.; Dening, T.; de Oliveira, D.; Milner, K.; Slade, M. Conceptual framework for social connectedness in mental disorders: Systematic review and narrative synthesis. J. Affect. Disord. 2019, 245, 188–199. [Google Scholar] [CrossRef]
- Weiss, R. The Provisions of Social Relationships. In Doing Unto Others: Joining, Molding, Conforming, Helping, Loving; Rubin, Z., Ed.; Prentice-Hall: Englewood Cliffs, NJ, USA, 1974. [Google Scholar]
- Orpana, H.M.; Lang, J.J.; Yurkowski, K. Validation of a brief version of the Social Provisions Scale using Canadian national survey data. Health Promot. Chronic Dis. Prev. Can. 2019, 39, 323–332. [Google Scholar] [CrossRef]
- Steigen, A.M.; Bergh, D. The Social Provisions Scale: Psychometric properties of the SPS-10 among participants in nature-based services. Disabil. Rehabil. 2019, 41, 1690–1698. [Google Scholar] [CrossRef]
- Miller, I.W.; Bishop, D.S.; Epstein, N.B.; Keitner, G.I. The Mcmaster Family Assessment Device—Reliability and Validity. J. Marital. Fam. Ther. 1985, 11, 345–356. [Google Scholar] [CrossRef]
- Hamilton, E.; Carr, A. Systematic Review of Self-Report Family Assessment Measures. Family Process 2016, 55, 16–30. [Google Scholar] [CrossRef] [PubMed]
- de Haan, K.L.B.; Hafekost, J.; Lawrence, D.; Sawyer, M.G.; Zubrick, S.R. Reliability and Validity of a Short Version of the General Functioning Subscale of the McMaster Family Assessment Device. Family Process 2015, 54, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.R.; Creech, J.C. Ordinal Measures in Multiple Indicator Models: A Simulation Study of Categorization Error. Am. Sociol. Rev. 1983, 48, 398–407. [Google Scholar] [CrossRef]
- Norman, G. Likert scales, levels of measurement and the “laws” of statistics. Adv. Health Sci. Educ. 2010, 15, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.M.; Artino, A.R., Jr. Analyzing and interpreting data from likert-type scales. J. Grad. Med. Educ. 2013, 5, 541–542. [Google Scholar] [CrossRef]
- Zumbo, B.D.; Zimmerman, D.W. Is the selection of statistical methods governed by level of measurement? Can. Psychol. Psychol. Can. 1993, 34, 390–400. [Google Scholar] [CrossRef]
- Malaquias, S.; Crespo, C.; Francisco, R. How do Adolescents Benefit from Family Rituals? Links to Social Connectedness, Depression and Anxiety. J. Child Fam. Stud. 2015, 24, 3009–3017. [Google Scholar] [CrossRef]
- Wang, Y.-N.; Yaun, Z.-J.; Leng, W.-C.; Xia, L.-Y.; Wang, R.-X.; Li, Z.-Z.; Zhou, Y.-J.; Zhang, X.-Y. Role of perceived family support in psychological distress for pregnant women during. World J. Psychiatry 2021, 11, 365–374. [Google Scholar] [CrossRef]
- Thomas, P.A.; Liu, H.; Umberson, D. Family Relationships and Well-Being. Innov. Aging 2017, 1, igx025. [Google Scholar] [CrossRef] [PubMed]
- Batista, P.; Duque, V.; Luzio-Vaz, A.; Pereira, A. Anxiety impact during COVID-19: A systematic review. J. Infect. Dev. Ctries. 2021, 15, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Bridgland, V.M.E.; Moeck, E.K.; Green, D.M.; Swain, T.L.; Nayda, D.M.; Matson, L.A.; Hutchison, N.P.; Takarangi, M.K.T. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE 2021, 16, e0240146. [Google Scholar] [CrossRef] [PubMed]
- Sheek-Hussein, M.; Abu-Zidan, F.M.; Stip, E. Disaster management of the psychological impact of the COVID-19 pandemic. Int. J. Emerg. Med. 2021, 14, 19. [Google Scholar] [CrossRef] [PubMed]
- Bergman, D.; Bethell, C.; Gombojav, N.; Hassink, S.; Stange, K.C. Physical Distancing With Social Connectedness. Ann. Fam. Med. 2020, 18, 272–277. [Google Scholar] [CrossRef]
- Jay, J.; Bor, J.; Nsoesie, E.O.; Lipson, S.K.; Jones, D.K.; Galea, S.; Raifman, J. Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat. Hum. Behav. 2020, 4, 1294–1302. [Google Scholar] [CrossRef]



| Standardized | Standard | ||||
|---|---|---|---|---|---|
| Coefficient | Error | z | p > z | ||
| Structural | |||||
| Physical distancing | |||||
| Anxiety | −1.640 | * | 0.477 | −3.440 | 0.001 |
| Race | 0.156 | 0.085 | 1.850 | 0.065 | |
| Hispanic | 0.079 | 0.091 | 0.870 | 0.385 | |
| Age | −0.414 | * | 0.141 | −2.950 | 0.003 |
| Family size | 0.207 | * | 0.098 | 2.120 | 0.034 |
| 65 years and older | −0.072 | 0.095 | −0.760 | 0.448 | |
| Compliance | −0.195 | 0.100 | −1.950 | 0.052 | |
| Employment status | −0.111 | 0.093 | −1.200 | 0.231 | |
| Income | −0.309 | * | 0.121 | −2.540 | 0.011 |
| Constant | 7.824 | *** | 1.631 | 4.800 | 0.000 |
| Anxiety | |||||
| Social connectedness | 1.054 | *** | 0.019 | 55.590 | 0.000 |
| Constant | −1.670 | 0.848 | −1.970 | 0.049 | |
| Social connectedness | |||||
| Physical distancing | 1.398 | *** | 0.318 | 4.400 | 0.000 |
| Measurement | |||||
| Social provisions | |||||
| Social connectedness | −0.255 | *** | 0.053 | −4.760 | 0.000 |
| Constant | 7.585 | *** | 0.320 | 23.720 | 0.000 |
| Family support | |||||
| Social connectedness | 0.148 | *** | 0.052 | 2.830 | 0.005 |
| Constant | 7.707 | *** | 0.348 | 22.180 | 0.000 |
| var(e.Physical distancing) | 3.418 | 1.428 | 1.507 | 7.752 | |
| var(e.Anxiety) | 0.266 | 0.279 | 0.034 | 2.084 | |
| var(e.Social provisions) | 0.935 | 0.029 | 0.880 | 0.994 | |
| var(e.Family support) | 0.978 | 0.016 | 0.947 | 1.010 | |
| var(e.Social connectedness) | 2.303 | 0.820 | 1.146 | 4.627 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kyne, D.; Robledo, C.; Clark, L.C.; Charak, R.; Salahuddin, M.; Morrow, J. Social Connectedness, Physical Distancing, and Anxiety in Complying with Shelter-In-Place Orders and Advisories during the Once-In-A-Century COVID-19 Pandemic in the US: A Study of Social Media and Internet Users. Int. J. Environ. Res. Public Health 2022, 19, 15282. https://doi.org/10.3390/ijerph192215282
Kyne D, Robledo C, Clark LC, Charak R, Salahuddin M, Morrow J. Social Connectedness, Physical Distancing, and Anxiety in Complying with Shelter-In-Place Orders and Advisories during the Once-In-A-Century COVID-19 Pandemic in the US: A Study of Social Media and Internet Users. International Journal of Environmental Research and Public Health. 2022; 19(22):15282. https://doi.org/10.3390/ijerph192215282
Chicago/Turabian StyleKyne, Dean, Candace Robledo, Loren Cliff Clark, Ruby Charak, Meliha Salahuddin, and Jay Morrow. 2022. "Social Connectedness, Physical Distancing, and Anxiety in Complying with Shelter-In-Place Orders and Advisories during the Once-In-A-Century COVID-19 Pandemic in the US: A Study of Social Media and Internet Users" International Journal of Environmental Research and Public Health 19, no. 22: 15282. https://doi.org/10.3390/ijerph192215282
APA StyleKyne, D., Robledo, C., Clark, L. C., Charak, R., Salahuddin, M., & Morrow, J. (2022). Social Connectedness, Physical Distancing, and Anxiety in Complying with Shelter-In-Place Orders and Advisories during the Once-In-A-Century COVID-19 Pandemic in the US: A Study of Social Media and Internet Users. International Journal of Environmental Research and Public Health, 19(22), 15282. https://doi.org/10.3390/ijerph192215282







