Caregiving Responsibilities and Mental Health Outcomes in Young Adult Carers during the COVID-19 Pandemic: A Longitudinal Study
Abstract
1. Introduction
The Present Study
- To investigate differences in caregiving responsibilities in the context of the COVID-19 pandemic across three groups of young adults: carers in a parental illness context, those caring for an ill non-parent family member, and non-carers. Informed by prior research, we predicted that young adult carers would report higher caregiving responsibilities than non-carer peers and that young adult carers of an ill parent would report higher caregiving responsibilities than those caring for an ill non-parent family member.
- To identify socio-demographic and COVID-19 context and lockdown contextual elements that are associated with higher caregiving responsibilities in young adult carers relative to non-carers.
- To examine the longitudinal association between caregiving responsibilities and mental health outcomes (operationalized as fear of COVID-19, anxiety, depression, and wellbeing) after controlling for the effects of family health status (parental vs. other ill family member) and relevant socio-demographic and COVID-19 context variables. Based on the findings from previous research, we predicted that higher caregiving responsibilities would predict subsequent poorer mental health outcomes.
2. Materials and Methods
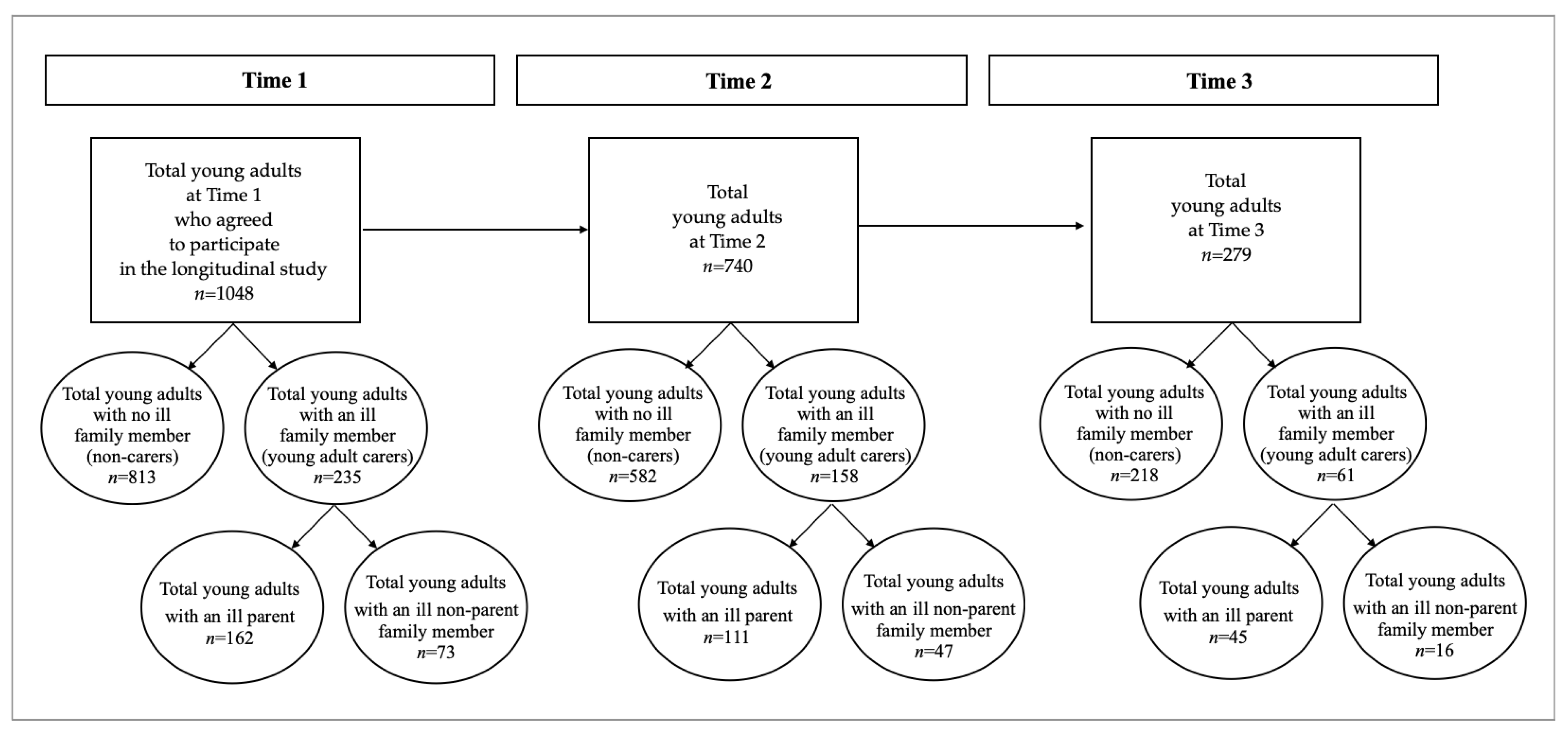
2.1. Participants and Recruitment Procedure
2.2. Measures
2.2.1. Family Health Status
2.2.2. Socio-Demographics
2.2.3. COVID-19 and Lockdown Context Variables
2.2.4. Caregiving Responsibilities
2.2.5. Mental Health Outcomes
Fear of COVID-19
Anxiety
Depression
Wellbeing
2.3. Data Analysis Approach
3. Results
3.1. Preliminary Data Analyses
3.1.1. Sample Characteristics
3.1.2. Attrition
3.2. Differences in Caregiving Responsibilities among PI, OIFM and Non-Carer Groups
3.3. Correlations between Time 1 Socio-Demographics and Times 1 and 2 COVID-19 Context Variables and Time 2 Caregiving Responsibilities
3.4. Longitudinal Associations between Caregiving Responsibilities and Mental Health Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leu, A.; Becker, S. A Cross-National and Comparative Classification of in-Country Awareness and Policy Responses to ‘Young Carers’. J. Youth Stud. 2017, 20, 750–762. [Google Scholar] [CrossRef]
- Pakenham, K.I.; Bursnall, S.; Chiu, J.; Cannon, T.; Okochi, M. The Psychosocial Impact of Caregiving on Young People Who Have a Parent with an Illness or Disability: Comparisons between Young Caregivers and Noncaregivers. Rehabil. Psychol. 2006, 51, 113–126. [Google Scholar] [CrossRef]
- Dharampal, R.; Ani, C. The Emotional and Mental Health Needs of Young Carers: What Psychiatry Can Do. BJPsych Bull 2020, 44, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Fleitas Alfonzo, L.; Singh, A.; Disney, G.; Ervin, J.; King, T. Mental Health of Young Informal Carers: A Systematic Review. Soc. Psychiatry Psychiatr. Epidemiol. 2022. [Google Scholar] [CrossRef]
- Lacey, R.E.; Xue, B.; McMunn, A. The Mental and Physical Health of Young Carers: A Systematic Review. Lancet Public Health 2022, 7, e787–e796. [Google Scholar] [CrossRef]
- Sieh, D.S.; Meijer, A.M.; Oort, F.J.; Visser-Meily, J.M.A.; Van der Leij, D.A.V. Problem Behavior in Children of Chronically Ill Parents: A Meta-Analysis. Clin. Child Fam. Psychol. Rev. 2010, 13, 384–397. [Google Scholar] [CrossRef]
- Landi, G.; Pakenham, K.I.; Grandi, S.; Tossani, E. Young Adult Carers during the Pandemic: The Effects of Parental Illness and Other Ill Family Members on COVID-19-Related and General Mental Health Outcomes. Int. J. Environ. Res. Public Health 2022, 19, 3391. [Google Scholar] [CrossRef]
- van der Werf, H.M.; Luttik, M.L.A.; de Boer, A.; Roodbol, P.F.; Paans, W. Growing up with a Chronically Ill Family Member—The Impact on and Support Needs of Young Adult Carers: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 855. [Google Scholar] [CrossRef]
- Chevrier, B.; Lamore, K.; Untas, A.; Dorard, G. Young Adult Carers’ Identification, Characteristics, and Support: A Systematic Review. Front. Psychol. 2022, 13, 990257. [Google Scholar] [CrossRef]
- Landi, G.; Pakenham, K.I.; Crocetti, E.; Grandi, S.; Tossani, E. Examination of the Tripartite Model of Youth Caregiving in the Context of Parental Illness. Psychol. Health 2022, 37, 397–418. [Google Scholar] [CrossRef]
- Arnett, J.J.; Žukauskienė, R.; Sugimura, K. The New Life Stage of Emerging Adulthood at Ages 18–29 Years: Implications for Mental Health. Lancet Psychiatry 2014, 1, 569–576. [Google Scholar] [CrossRef]
- Arnett, J.J. Emerging Adulthood: The Winding Road from the Late Teens through the Twenties; Oxford University Press: Oxford, UK, 2014; ISBN 978-0-19-992938-2. [Google Scholar]
- Syed, M. Emerging Adulthood: Developmental Stage, Theory, or Nonsense? The Oxford Handbook of Emerging Adulthood; Arnett, J.J., Ed.; Oxford University Press: Cambridge, UK, 2016; pp. 11–25. ISBN 978-0-19-979557-4. [Google Scholar]
- Aleni Sestito, L.; Sica, L.S. Identity Formation of Italian Emerging Adults Living with Parents: A Narrative Study. J. Adolesc. 2014, 37, 1435–1447. [Google Scholar] [CrossRef] [PubMed]
- Cox, S.D.; Pakenham, K.I. Confirmatory Factor Analysis and Invariance Testing of the Young Carer of Parents Inventory (YCOPI). Rehabil. Psychol. 2014, 59, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Pakenham, K.I.; Cox, S. The Effects of Parental Illness and Other Ill Family Members on Youth Caregiving Experiences. Psychol. Health 2015, 30, 857–878. [Google Scholar] [CrossRef] [PubMed]
- Landi, G.; Pakenham, K.I.; Benassi, M.; Giovagnoli, S.; Tossani, E.; Grandi, S. A Model of the Effects of Parental Illness on Youth Adjustment and Family Functioning: The Moderating Effects of Psychological Flexibility on Youth Caregiving and Stress. Int. J. Environ. Res. Public Health 2021, 18, 4902. [Google Scholar] [CrossRef]
- Pakenham, K.I.; Cox, S. Test of a Model of the Effects of Parental Illness on Youth and Family Functioning. Health Psychol. 2012, 31, 580–590. [Google Scholar] [CrossRef]
- Blake-Holmes, K.; McGowan, A. ‘It’s Making His Bad Days into My Bad Days’: The Impact of Coronavirus Social Distancing Measures on Young Carers and Young Adult Carers in the United Kingdom. Child Fam. Soc. Work. 2022, 27, 22–29. [Google Scholar] [CrossRef]
- Pakenham, K.I.; Cox, S. The Effects of Parental Illness and Other Ill Family Members on the Adjustment of Children. Ann. Behav. Med. 2014, 48, 424–437. [Google Scholar] [CrossRef]
- Boumans, N.P.G.; Dorant, E. A Cross-Sectional Study on Experiences of Young Adult Carers Compared to Young Adult Noncarers: Parentification, Coping and Resilience. Scand. J. Caring Sci. 2018, 32, 1409–1417. [Google Scholar] [CrossRef]
- Ali, L.; Ahlström, B.H.; Krevers, B.; Sjöström, N.; Skärsäter, I. Support for Young Informal Carers of Persons with Mental Illness: A Mixed-Method Study. Issues Ment. Health Nurs. 2013, 34, 611–618. [Google Scholar] [CrossRef]
- Chevrier, B.; Untas, A.; Dorard, G. Are We All the Same When Faced with an Ill Relative? A Person-Oriented Approach to Caring Activities and Mental Health in Emerging Adult Students. Int. J. Environ. Res. Public Health 2022, 19, 8104. [Google Scholar] [CrossRef]
- Day, C. An Empirical Case Study of Young Adult Carers’ Engagement and Success in Higher Education. Int. J. Incl. Educ. 2021, 25, 1597–1615. [Google Scholar] [CrossRef]
- Greene, J.; Cohen, D.; Siskowski, C.; Toyinbo, P. The Relationship Between Family Caregiving and the Mental Health of Emerging Young Adult Caregivers. J. Behav. Health Serv. Res. 2017, 44, 551–563. [Google Scholar] [CrossRef]
- Grenard, D.L.; Valencia, E.J.; Brown, J.A.; Winer, R.L.; Littman, A.J. Impact of Caregiving During Emerging Adulthood on Frequent Mental Distress, Smoking, and Drinking Behaviors: United States, 2015–2017. Am. J. Public Health 2020, 110, 1853–1860. [Google Scholar] [CrossRef]
- Haugland, B.S.M.; Hysing, M.; Sivertsen, B. The Burden of Care: A National Survey on the Prevalence, Demographic Characteristics and Health Problems Among Young Adult Carers Attending Higher Education in Norway. Front. Psychol. 2020, 10, 2859. [Google Scholar] [CrossRef]
- Levine, C.; Hunt, G.G.; Halper, D.; Hart, A.Y.; Lautz, J.; Gould, D.A. Young Adult Caregivers: A First Look at an Unstudied Population. Am. J. Public Health 2005, 95, 2071–2075. [Google Scholar] [CrossRef]
- Van der Werf, H.M.; Luttik, M.L.A.; Francke, A.L.; Roodbol, P.F.; Paans, W. Students Growing up with a Chronically Ill Family Member; a Survey on Experienced Consequences, Background Characteristics, and Risk Factors. BMC Public Health 2019, 19, 1486. [Google Scholar] [CrossRef]
- Haugland, B.S.M.; Hysing, M.; Sivertsen, B. Study Progress, Recreational Activities, and Loneliness in Young Adult Carers: A National Student Survey. BMC Psychol. 2022, 10, 43. [Google Scholar] [CrossRef] [PubMed]
- Smriti, D.; Ambulkar, S.; Meng, Q.; Kaimal, G.; Ramotar, K.; Park, S.Y.; Huh-Yoo, J. Creative Arts Therapies for the Mental Health of Emerging Adults: A Systematic Review. Arts Psychother. 2022, 77, 101861. [Google Scholar] [CrossRef]
- Landi, G.; Boccolini, G.; Giovagnoli, S.; Pakenham, K.I.; Grandi, S.; Tossani, E. Validation of the Italian Young Carer of Parents Inventory-Revised (YCOPI-R). Disabil. Rehabil. 2022, 44, 795–806. [Google Scholar] [CrossRef]
- Soraci, P.; Ferrari, A.; Abbiati, F.A.; Del Fante, E.; De Pace, R.; Urso, A.; Griffiths, M.D. Validation and Psychometric Evaluation of the Italian Version of the Fear of COVID-19 Scale. Int. J. Ment. Health Addict. 2020, 44, 795–806. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Kroenke & Spitzer Instruction Manual: Instructions for Patient Health Questionnaire (PHQ) and GAD-7 Measures. Available online: www.Phqscreeners.Com (accessed on 9 March 2020).
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Plummer, F.; Manea, L.; Trepel, D.; McMillan, D. Screening for Anxiety Disorders with the GAD-7 and GAD-2: A Systematic Review and Diagnostic Metaanalysis. Gen. Hosp. Psychiatry 2016, 39, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Mazzotti, E.; Fassone, G.; Picardi, A.; Sagoni, E.; Ramieri, L.; Lega, I.; Camaioni, D.; Abeni, D.; Pasquini, P. II Patient Health Questionnaire (PHQ) per lo screening dei disturbi psichiatrici: Uno studio di validazione nei confronti della Intervista Clinica Strutturata per il DSM-IV asse I (SCID-I). Ital. J. Psychopathol. 2003, 9, 235–242. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Manea, L.; Gilbody, S.; McMillan, D. Optimal Cut-off Score for Diagnosing Depression with the Patient Health Questionnaire (PHQ-9): A Meta-Analysis. CMAJ 2012, 184, E191–E196. [Google Scholar] [CrossRef]
- Petrillo, G.; Capone, V.; Caso, D.; Keyes, C.L.M. The Mental Health Continuum–Short Form (MHC–SF) as a Measure of Well-Being in the Italian Context. Soc. Indic. Res. 2015, 121, 291–312. [Google Scholar] [CrossRef]
- Keyes, C.L.M.; Wissing, M.; Potgieter, J.P.; Temane, M.; Kruger, A.; van Rooy, S. Evaluation of the Mental Health Continuum–Short Form (MHC–SF) in Setswana-Speaking South Africans. Clin. Psychol. Psychother. 2008, 15, 181–192. [Google Scholar] [CrossRef]
- Lamers, S.M.A.; Westerhof, G.J.; Bohlmeijer, E.T.; ten Klooster, P.M.; Keyes, C.L.M. Evaluating the Psychometric Properties of the Mental Health Continuum-Short Form (MHC-SF). J. Clin. Psychol. 2011, 67, 99–110. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017; pp. 1998–2018. [Google Scholar]
- Little, R.J.A. A Test of Missing Completely at Random for Multivariate Data with Missing Values. J. Am. Stat. Assoc. 1988, 83, 1198–1202. [Google Scholar] [CrossRef]
- Bollen, K.A. Structural Equations with Latent Variables; John Wiley & Sons: Oxford, UK, 1989; p. xiv, 514. ISBN 978-0-471-01171-2. [Google Scholar]
- Selya, A.S.; Rose, J.S.; Dierker, L.C.; Hedeker, D.; Mermelstein, R.J. A Practical Guide to Calculating Cohen’s F2, a Measure of Local Effect Size, from PROC MIXED. Front. Psychol. 2012, 3, 111. [Google Scholar] [CrossRef] [PubMed]
- Ellis, P.D. The Essential Guide to Effect Sizes: Statistical Power, Meta-Analysis, and the Interpretation of Research Results; Cambridge University Press: Cambridge, UK, 2010; ISBN 978-1-139-48815-0. [Google Scholar]
- Bacci, M.L. Avanti Giovani, Alla Riscossa: Come Uscire Dalla Crisi Giovanile in Italia; Il Mulino: Bologna, Italy, 2008; ISBN 978-88-15-12653-5. [Google Scholar]
- Crocetti, E.; Meeus, W. “Family Comes First!” Relationships with Family and Friends in Italian Emerging Adults. J. Adolesc. 2014, 37, 1463–1473. [Google Scholar] [CrossRef]
- García-Mendoza, M.C.; Parra, A.; Sánchez-Queija, I.; Oliveira, J.E.; Coimbra, S. Gender Differences in Perceived Family Involvement and Perceived Family Control during Emerging Adulthood: A Cross-Country Comparison in Southern Europe. J. Child. Fam. Stud. 2022, 31, 1007–1018. [Google Scholar] [CrossRef]
- Aldridge, J. Where Are We Now? Twenty-Five Years of Research, Policy and Practice on Young Carers. Crit. Soc. Policy 2018, 38, 155–165. [Google Scholar] [CrossRef]
- Leu, A.; Guggiari, E.; Phelps, D.; Magnusson, L.; Nap, H.H.; Hoefman, R.; Lewis, F.; Santini, S.; Socci, M.; Boccaletti, L.; et al. Cross-National Analysis of Legislation, Policy and Service Frameworks for Adolescent Young Carers in Europe. J. Youth Stud. 2022, 25, 1215–1235. [Google Scholar] [CrossRef]
- Stamatopoulos, V. Supporting Young Carers: A Qualitative Review of Young Carer Services in Canada. Int. J. Adolesc. Youth 2016, 21, 178–194. [Google Scholar] [CrossRef]
- Hendricks, B.A.; Kavanaugh, M.S.; Bakitas, M.A. How Far Have We Come? An Updated Scoping Review of Young Carers in the U.S. Child Adolesc Soc. Work. J. 2021, 38, 491–504. [Google Scholar] [CrossRef]
- Stolper, H.; van Doesum, K.; Henselmans, P.; Bijl, A.L.; Steketee, M. The Patient’s Voice as a Parent in Mental Health Care: A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 13164. [Google Scholar] [CrossRef]
| PI (n = 162) | OIFM (n = 73) | Non-Carers (n = 813) | Total Sample (N = 1048) | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | % | M (SD) | % | M (SD) | % | M (SD) | % | M (SD) |
| Socio-demographics | ||||||||
| Gender: female | 75.31 | 76.71 | 73.92 | 74.33 | ||||
| Age years | 24.10 (2.65) | 24.29 (2.66) | 24.57 (2.84) | 24.48 (2.80) | ||||
| Education | ||||||||
| Primary school | 2.47 | 1.37 | 3.08 | 2.86 | ||||
| Secondary school | 42.59 | 42.47 | 39.11 | 39.89 | ||||
| Bachelor’s degree | 50.62 | 49.32 | 53.38 | 52.67 | ||||
| Postgraduate course | 4.32 | 6.85 | 4.43 | 4.58 | ||||
| Single | 96.27 | 92.78 | 86.97 | 88.70 | ||||
| Married or living with a partner | 3.09 | 6.85 | 13.28 | 11.26 | ||||
| Currently working | 23.46 | 28.77 | 36.41 | 33.87 | ||||
| Currently studying | 67.90 | 61.64 | 57.81 | 59.64 | ||||
| Not in education, employment, or training | 9.88 | 12.32 | 9.59 | 9.82 | ||||
| Socio-economic status | ||||||||
| <EUR 15,000 | 25.31 | 15.07 | 15.74 | 17.18 | ||||
| EUR 15,001–36,000 | 43.83 | 38.36 | 43.30 | 43.03 | ||||
| EUR 36,000–70,000 | 21.60 | 38.36 | 30.75 | 29.87 | ||||
| >EUR 70,000 | 9.26 | 8.22 | 10.21 | 9.92 | ||||
| Italian nationality | 98.15 | 98.63 | 97.42 | 97.61 | ||||
| Presence of a physical health condition | 11.11 | 16.44 | 8.86 | 9.73 | ||||
| Ill family member illness type—physical | 66.05 | 56.16 | - | 14.03 | ||||
| Ill family member illness type—mental | 46.29 | 45.21 | - | 11.07 | ||||
| COVID-19 and lockdown context variables | ||||||||
| Insufficient home dimension a | 1.39 (1.01) | 1.51 (1.16) | 1.34 (1.01) | 1.36 (1.02) | ||||
| Number of people in the household | 3.44 (1.08) | 3.92 (1.19) | 3.11 (1.18) | 3.22 (1.18) | ||||
| Reduced family income | 11.11 | 9.60 | 8.00 | 8.59 | ||||
| Working or studying from home a | 2.68 (1.79) | 2.37 (1.82) | 2.32 (1.84) | 2.38 (1.84) | ||||
| Work in a health-care setting | 11.11 | 10.96 | 11.56 | 11.92 | ||||
| Structural change to social network b | 1.97 (1.27) | 2.01 (1.38) | 2.01 (1.27) | 2.01 (1.27) | ||||
| Percentage of time spent in red zone | 34.23 (22.39) | 32.74 (24.25) | 33.02 (23.69) | 33.97 (24.02) | ||||
| COVID-19 infected (T1 + T2) | 19.75 | 9.59 | 15.50 | 16.27 | ||||
| COVID-19 hospitalized (T1 + T2) | 0.00 | 0.00 | 0.00 | 0.00 | ||||
| Family member infected (T1 + T2) | 38.22 | 23.29 | 33.03 | 33.13 | ||||
| Family member hospitalized (T1 + T2) | 10.49 | 4.11 | 8.61 | 8.59 | ||||
| Family member death (T1 + T2) | 7.41 | 5.48 | 10.95 | 8.49 | ||||
| COVID-19 vaccine (T1 + T2) | 17.35 | 12.82 | 19.60 | 18.84 | ||||
| T2 caregiving responsibilities | 2.16 (0.71) | 2.11 (0.77) | 1.89 (0.72) | 1.95 (0.73) | ||||
| Time 2 Caregiving Responsibilities | ||||
|---|---|---|---|---|
| PI (n = 111) | OIFM (n = 47) | YACs (n = 158) | Non-Carers (n = 582) | |
| Socio-demographics | ||||
| Gender (1 = female) | −0.037 | 0.047 | −0.011 | −0.072 |
| Age | 0.019 | 0.411 * | 0.098 | −0.064 |
| Low education (1 = secondary school or below) | −0.001 | 0.122 | 0.085 | 0.020 |
| Currently single ¥ | −0.074 | −0.143 | −0.065 | 0.005 |
| Currently working ¥ | 0.081 | 0.117 | −0.117 | 0.009 |
| Currently studying ¥ | −0.390 | 0.112 | −0.283 | 0.007 |
| Not in education, employment, or training ¥ | −0.151 | 0.113 | 0.121 | 0.060 |
| Low socio-economic status (1 = < EUR 15,000) | 0.017 | −0.123 | 0.021 | 0.099 * |
| Nationality (1 = Italian) | −0.098 | 0.102 | 0.091 | −0.017 |
| Presence of a physical health condition ¥ | −0.038 | −0.092 | −0.080 | 0.035 |
| Family illness type—physical ¥ | 0.051 | 0.064 | 0.042 | - |
| Family illness type—mental ¥ | −0.042 | −0.037 | −0.042 | - |
| COVID−19 Context Variables | ||||
| Insufficient home dimension | 0.126 | 0.112 | 0.183 * | −0.039 |
| Number of people in the household | −0.006 | −0.011 | 0.022 | 0.061 |
| Reduced family income ¥ | 0.039 | 0.152 | 0.128 | 0.081 |
| Working or studying from home | 0.018 | −0.289 * | 0.083 | 0.028 |
| Work in a health-care setting ¥ | 0.013 | 0.162 | 0.094 | 0.010 |
| Structural change to social network | 0.184 | −0.081 | 0.067 | 0.025 |
| Percentage of time spent in red zone (T1 + T2) | −0.044 | −0.055 | −0.088 | −0.050 |
| COVID−19 infected (T1 + T2) ¥ | −0.096 | 0.012 | −0.096 | 0.050 |
| Family member infected (T1 + T2) ¥ | 0.111 | 0.018 | 0.073 | −0.084 |
| Family member hospitalized (T1 + T2) ¥ | −0.001 | 0.114 | 0.051 | −0.019 |
| Family member death (T1 + T2) ¥ | −0.063 | 0.045 | −0.031 | −0.029 |
| COVID-19 Vaccine (T1 + T2) ¥ | 0.126 | −0.149 | −0.028 | −0.012 |
| Time 3 Fear of COVID-19 | Time 3 Anxiety | Time 3 Depression | Time 3 Wellbeing | |
|---|---|---|---|---|
| β (ƒ2) | β (ƒ2) | β (ƒ2) | β (ƒ2) | |
| Time 2 Caregiving responsibilities | 0.153 * (0.024) | 0.194 ** (0.039) | 0.158 ** (0.026) | −0.214 ** (0.048) |
| Family health status | ||||
| PI † | −0.020 (0.000) | 0.026 (0.001) | 0.088 (0.008) | −0.129 (0.017) |
| OIFM † | −0.002 (0.000) | −0.053 (0.003) | −0.038 (0.001) | −0.014 (0.000) |
| Other confounders | ||||
| Age | 0.009 (0.000) | −0.050 (0.003) | −0.124 (0.016) | 0.065 (0.004) |
| Marital status | 0.078 (0.006) | 0.024 (0.001) | 0.095 (0.009) | −0.133 (0.018) |
| Currently working | −0.134 (0.018) | −0.078 (0.006) | −0.072 (0.005) | 0.247 ** (0.065) |
| Insufficient home dimension | −0.028 (0.001) | 0.071 (0.005) | 0.111 (0.012) | 0.029 (0.001) |
| Working or studying from home | −0.073 (0.005) | 0.103 (0.011) | 0.086 (0.007) | −0.001 (0.000) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landi, G.; Pakenham, K.I.; Cattivelli, R.; Grandi, S.; Tossani, E. Caregiving Responsibilities and Mental Health Outcomes in Young Adult Carers during the COVID-19 Pandemic: A Longitudinal Study. Int. J. Environ. Res. Public Health 2022, 19, 15149. https://doi.org/10.3390/ijerph192215149
Landi G, Pakenham KI, Cattivelli R, Grandi S, Tossani E. Caregiving Responsibilities and Mental Health Outcomes in Young Adult Carers during the COVID-19 Pandemic: A Longitudinal Study. International Journal of Environmental Research and Public Health. 2022; 19(22):15149. https://doi.org/10.3390/ijerph192215149
Chicago/Turabian StyleLandi, Giulia, Kenneth I. Pakenham, Roberto Cattivelli, Silvana Grandi, and Eliana Tossani. 2022. "Caregiving Responsibilities and Mental Health Outcomes in Young Adult Carers during the COVID-19 Pandemic: A Longitudinal Study" International Journal of Environmental Research and Public Health 19, no. 22: 15149. https://doi.org/10.3390/ijerph192215149
APA StyleLandi, G., Pakenham, K. I., Cattivelli, R., Grandi, S., & Tossani, E. (2022). Caregiving Responsibilities and Mental Health Outcomes in Young Adult Carers during the COVID-19 Pandemic: A Longitudinal Study. International Journal of Environmental Research and Public Health, 19(22), 15149. https://doi.org/10.3390/ijerph192215149









