Level of Trust of the Population in the Unified Health System in the Midst of the COVID-19 Crisis in Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Research Scenario and Epidemiological Context
2.3. Population
2.4. Data Analysis
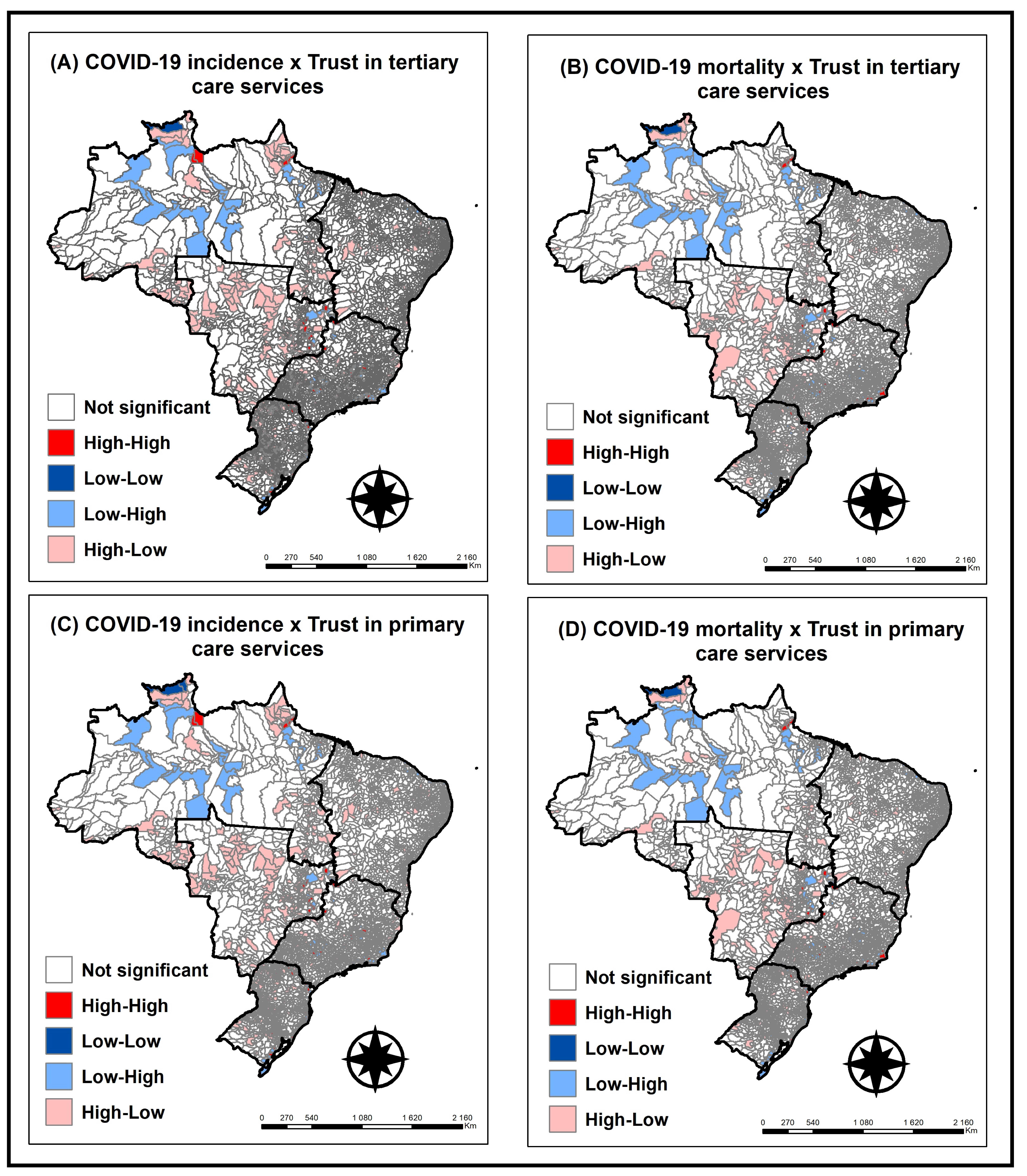
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- OPAS. OMS Declara que COVID-19 é Caracterizada Como Pandemia—OPAS/OMS|Organização Pan-Americana da Saúde. Organização Pan-Americana de Saúde 5. 2020. Available online: https://www.paho.org/pt/news/30-1-2020-who-declares-public-health-emergency-novel-coronavirus (accessed on 20 March 2021).
- Moucheraud, C.; Guo, H.; Macinko, J. Trust in Governments And Health Workers Low Globally, Influencing Attitudes Toward Health Information, Vaccines. Health Aff. Proj. Hope 2021, 40, 1215–1224. [Google Scholar] [CrossRef] [PubMed]
- Trust in Healthcare by Country 2021. Statista. Available online: https://www.statista.com/statistics/1071027/trust-levels-towards-healthcare-in-select-countries/ (accessed on 11 September 2021).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Naderifar, M.; Goli, H.; Ghaljaie, F. Snowball Sampling: A Purposeful Method of Sampling in Qualitative Research. Strides Dev. Med. Educ. 2017, 14, e67670. [Google Scholar] [CrossRef]
- Agresti, A. Categorical Data Analysis; Wiley Series in Probability and Statistics; Wiley: Hoboken, NJ, USA, 2002. [Google Scholar]
- McCullagh, P. Regression Models for Ordinal Data. J. R. Stat. Soc. Ser. B Methodol. 1980, 42, 109–127. [Google Scholar] [CrossRef]
- Agresti, A. Analysis of Ordinal Categorical Data, 2nd ed.; John Wiley and Sons Inc.: Hoboken, NJ, USA, 2012. [Google Scholar] [CrossRef]
- Gunst, R.F.; Myers, R.H.; Montgomery, D.C. Response Surface Methodology: Process and Product Optimization Using Designed Experiments. Technometrics 1996, 38, 285. [Google Scholar] [CrossRef]
- Grove, D.; Sakamoto, Y.; Ishiguro, M.; Kitagawa, G. Akaike Information Criterion Statistics. The Statistician; Springer: Beijing, China, 1988; Volume 37. [Google Scholar]
- Zeileis, A.; Hothorn, T. Diagnostic Checking in Regression Relationships. R News 2002, 2, 7–10. [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística (IBGE). Brasil em Síntese [Internet]. 2022. Available online: https://brasilemsintese.ibge.gov.br/ (accessed on 26 July 2022).
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef] [PubMed]
- OECD. Government at a Glance 2021 [Internet]. OECD. 2021. Available online: https://www.oecdilibrary.org/governance/government-at-a-glance-2021_1c258f55-en (accessed on 20 March 2022).
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health; WHO: Geneva, Switzerland, 2010; 79p. Available online: http://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf (accessed on 1 March 2022).
- Read, L.; Korenda, L.; Nelson, H. Trust in the Health Care System | Deloitte Insights. Deloitte Insights [Internet]. 2021. Available online: https://www2.deloitte.com/us/en/insights/industry/health-care/trust-in-healthcare-system.htm (accessed on 1 March 2022).
- IBGE. Síntese de Indicadores Sociais—SIS. IBGE. 2019. Available online: https://www.ibge.gov.br/estatisticas/sociais/educacao/9221-sintese-de-indicadores-sociais.html?=&t=resultados (accessed on 1 March 2022).
- Reigada, C.L.d.L.; Romano, V.F. O uso do SUS como estigma: A visão de uma classe média. Physis Rev. de Saúde Coletiva 2018, 28, 280316. Available online: http://www.scielo.br/j/physis/a/6mk4Hsqvwf9kKcdfKFKMv6y/?lang=pt (accessed on 20 March 2022).
- De Freitas, C.M.; Silva, I.V.D.M.E.; Cidade, N.d.C.; da Silva, M.A.; Peres, M.C.M.; Nunes, F.S.B. A Gestão de Riscos e Governança na Pandemia por COVID-19 no Brasil: Análise dos Decretos Estaduais no Primeiro Mês; Relatório Técnico e Sumário Executivo [Internet]. Vol. 1, Centro de Estudos e Pesquisas em Emergências e Desastres em Saúde—Cepedes. CEPEDES/ENSP/Fiocruz. 2020. Available online: https://www.arca.fiocruz.br/bitstream/icict/41452/2/relatorio_cepedes_gestao_riscos_covid19_final.pdf (accessed on 2 February 2022).
- De Almeida, R. Bolsonaro President: Conservatism, Evangelism and the Brazilian Crisis. Novos Estud. CEBRAP 2019, 38, 185–213. [Google Scholar]
- Bazán, P.R.; de Azevedo Neto, R.M.; Dias, J.A.; Salvatierra , V.G.; Sanches, L.G.; Lacerda, S.S.; Amaro, E., Jr.; Kozasa, E.H.; Balardin, J.B. COVID-19 information exposure in digital media and implications for employees in the health care sector: Findings from an online survey. Einstein Sao Paulo Braz. 2020, 18, eAO6127. [Google Scholar] [CrossRef]
- Harring, N.; Jagers, S.C.; Löfgren, Å. COVID-19: Large-scale collective action, government intervention, and the importance of trust. World Dev. 2021, 138, 105236. [Google Scholar] [CrossRef] [PubMed]
- Szwarcwald, C.L.; Júnior, P.R.B.d.; Damacena, G.N.; Malta, D.C.; Barros, M.B.d.; Romero, D.E.; de Almeida, W.d.; Azevedo, L.O.; Machado, Í.E.; Lima, M.G.; et al. ConVid—Behavior Survey by the Internet during the COVID-19 pandemic in Brazil: Conception and application methodology. Cad. Saude Publica 2021, 37, e00268320. [Google Scholar] [CrossRef] [PubMed]
- Faleiros, F.; Käppler, C.; Pontes, F.A.R.; Silva, S.S.d.; de Goes, F.d.S.N.; Cucick, C.D. Use of virtual questionnaire and dissemination as a data collection strategy in scientific studies. Texto Contexto. Enferm. 2016, 25, 3880014. [Google Scholar] [CrossRef]
| Variables | Categories |
|---|---|
| Independent Variables | |
| Sex | Male, Female |
| Age | Continuous |
| Region | North, Northeast, Midwest, Southeast, South |
| Education level | <=Elementary school, complete primary education, high school, graduate, and postgraduate degree |
| Income | Less than 1 minimum wage, from 1 to 2 minimum wages, from 2 to 5 minimum wages, from 5 to 10 minimum wages, above 10 minimum wages, don’t know/prefer not to inform |
| Skin color | White, black/brown, yellow/indigenous |
| Marital status | Single, married/stable union, separated, widowed |
| Religion | Catholic, spiritism, evangelical, other religions, no religion |
| Occupation | Retired, unemployed, public employee, private employee, self-employed/informal/offers, student, other |
| Years of residence | 0 to 10 years, >10 to 20 years, >20 to 30 years, > 30 years |
| Number of people living at home | Continuous |
| Number of people contributing to the family income | Continuous |
| Area of residence | Urban, rural |
| Type of housing | Own, rented/leased, other |
| Health insurance | Yes, No |
| Use of SUS | Yes, No |
| Receives a visit from the community agent | Yes, No |
| Health clinic where he lives | Yes, no, I do not know |
| Aid from the government | Yes, No |
| Sources of information | |
| International organizations | Yes, No |
| Friends and/or family | Yes, No |
| Social support networks | Yes, No |
| News, newspapers | Yes, No |
| Numerical Variables | Mean | Standard Deviation |
|---|---|---|
| Age | 46.1 | 14.8 |
| Residents at home | 2.8 | 1.7 |
| People who contribute to the family income | 1.8 | 0.8 |
| Categorical variables | Frequency | % |
| Sex | ||
| Male | 252 | 24.8 |
| Female | 766 | 75.2 |
| Region | ||
| Midwest | 43 | 4.2 |
| Northeast | 94 | 9.2 |
| North | 65 | 6.4 |
| Southeast | 672 | 66 |
| South | 144 | 14.1 |
| Color/race | ||
| Yellow/indigenous | 21 | 2.1 |
| White | 708 | 69.5 |
| Black/brown | 289 | 28.4 |
| Marital status | ||
| Married/stable union | 507 | 49.8 |
| Separated | 143 | 14 |
| Single | 351 | 34.5 |
| Windowed | 17 | 1.7 |
| Religion | ||
| Catholic | 389 | 38.2 |
| Spiritism | 122 | 12 |
| Evangelical | 114 | 11.2 |
| Other | 93 | 9.1 |
| No religion | 300 | 29.5 |
| Occupation | ||
| Retired | 141 | 13.9 |
| Autonomous/informal/offers | 97 | 9.5 |
| Unemployed | 46 | 4.5 |
| Private employee | 146 | 14.3 |
| Public employee | 385 | 37.8 |
| Student | 124 | 12.2 |
| Other | 79 | 7.8 |
| Education | ||
| Incomplete elementary school | 9 | 0.9 |
| Complete primary education | 16 | 1.6 |
| High school | 177 | 17.4 |
| Graduated | 260 | 25.5 |
| Postgraduate studies | 556 | 54.6 |
| Income (in minimum wages) | ||
| Less than 1 | 22 | 2.2 |
| 1 to 2 | 72 | 7.1 |
| 2 to 5 | 273 | 26.8 |
| 5 to 10 | 298 | 29.3 |
| More than 10 | 286 | 28.1 |
| Prefer not to inform/do not know | 61 | 6 |
| No income | 6 | 0.6 |
| Type of housing | ||
| Own | 726 | 71.3 |
| Rent/Lease | 242 | 23.8 |
| Granted | 37 | 3.6 |
| Other | 13 | 1.3 |
| Area of residence | ||
| Rural | 30 | 2.9 |
| Urban | 988 | 97.1 |
| Categorical Variables | Frequency | % |
|---|---|---|
| Trust level in public health services to face COVID-19 | ||
| Hospital | ||
| No trust | 74 | 7.3 |
| Little trust | 326 | 32 |
| Trust | 515 | 50.6 |
| High trust | 103 | 10.1 |
| Basic health unit/health center | ||
| No trust | 143 | 14 |
| Little trust | 421 | 41.4 |
| Trust | 396 | 38.9 |
| High trust | 58 | 5.7 |
| Odds Ratio (OR) | 95%CI | p-Value | |
|---|---|---|---|
| Sex | |||
| Female | Ref | Ref | Ref |
| Male | 1.36 | 1.02–1.81 | 0.0340 |
| Region | |||
| Southeast | Ref | Ref | Ref |
| Midwest: less confident | 0.92 | 0.27–3.17 | 0.9032 |
| Midwest: confident | 0.49 | 0.26–0.95 | 0.0357 |
| Midwest: very confident | 0.15 | 0.02–1.15 | 0.0689 |
| North East: less confident | 2.18 | 0.75–6.33 | 0.1483 |
| North East: confident | 0.95 | 0.60–1.52 | 0.8589 |
| North East: very confident | 1,21 | 0.62–2.38 | 0.5665 |
| North: less confident | 0.52 | 0.22–1.20 | 0.1296 |
| North: confident | 0.43 | 0.24–0.74 | 0.0027 |
| South: less confident | 3.18 | 1.11–9.11 | 0.0309 |
| South: confident | 2.06 | 1.13–3.17 | 0.0010 |
| South: very confident | 0.90 | 0.49–1.65 | 0.7460 |
| Age | 0.97 | 0.96–0.98 | 0.0000 |
| Religion | |||
| Catholic | Ref | Ref | Ref |
| Spiritist | 1.38 | 0.92–2.07 | 0.1162 |
| Evangelical | 0.65 | 0.43–0.98 | 0.0429 |
| Other | 0.68 | 0.44–1.07 | 0.1022 |
| No religion | 0.91 | 0.67–1.23 | 0.5562 |
| Occupation | |||
| Other | Ref | Ref | Ref |
| Retired | 1.10 | 0.62–1.94 | 0.7363 |
| Autonomous | 1.24 | 0.70–2.20 | 0.4580 |
| Private employee | 0.93 | 0.46–1.91 | 0.8616 |
| Public employee | 0.84 | 0.49–1.45 | 0.5519 |
| Student | 1.48 | 0.91–2.39 | 0.1085 |
| Residential area | |||
| Urban | Ref | Ref | Ref |
| Rural | 0.45 | 0.22–0.91 | 0.0267 |
| Sources of information to stay informed about COVID-19 | |||
| International organization: No | Ref | Ref | Ref |
| International organization: Yes | 1.41 | 1.09–1.82 | 0.0074 |
| Education | |||
| Graduated | Ref | Ref | Ref |
| Elementary school | 3.05 | 1.29–7.22 | 0.0109 |
| High school | 1.15 | 0.77–1.71 | 0.4853 |
| Postgraduate studies | 1.32 | 0.98–1.78 | 0.0673 |
| Income (in minimum wages) | |||
| More than 10 | Ref | Ref | Ref |
| 1 to 2 | 0.35 | 0.20–0.61 | 0.0003 |
| 2 to 5 | 0.69 | 0.49–0.98 | 0.0436 |
| 5 to 10 | 0.64 | 0.47–0.89 | 0.0089 |
| Less than 1 | 0.36 | 0.15–0.83 | 0.0178 |
| Prefer not to inform/do not know | 0.65 | 0.37–1.12 | 0.1247 |
| Odds Ratio (OR) | 95%CI | p-Value | |
|---|---|---|---|
| Marital status | |||
| Married | Ref | Ref | Ref |
| Separated | 0.67 | 0.47–0.95 | 0.0274 |
| Single | 1.17 | 0.89–1.52 | 0.2417 |
| Windowed | 1.55 | 0.61–3.90 | 0.3503 |
| Education | |||
| Graduated | Ref | Ref | Ref |
| Elementary school | 2.40 | 1.09–5.25 | 0.0283 |
| High school | 1.06 | 0.73–1.52 | 0.7484 |
| Postgraduate studies | 1.83 | 1.38–2.42 | 0.0000 |
| Type of housing | |||
| Own | Ref | Ref | Ref |
| Rent/lease | 1.45 | 1.10–1.92 | 0.0073 |
| Other | 1.51 | 0.88–2.60 | 0.1339 |
| Sources of information used to stay informed about COVID-19 | |||
| International organizations: No | Ref | Ref | Ref |
| International organizations: Yes: 1 | 1.35 | 1.06–1.72 | 0.0151 |
| Friends and/or family: No | Ref | Ref | Ref |
| Friends and/or family: Yes: 3 | 1.32 | 1.02–1.70 | 0.0312 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araújo, J.S.T.d.; Delpino, F.M.; Berra, T.Z.; Moura, H.S.D.; Ramos, A.C.V.; Nascimento, M.C.d.; Alonso, J.B.; Silva, R.V.d.S.; de Freitas, G.L.; Teibo, T.K.A.; et al. Level of Trust of the Population in the Unified Health System in the Midst of the COVID-19 Crisis in Brazil. Int. J. Environ. Res. Public Health 2022, 19, 14999. https://doi.org/10.3390/ijerph192214999
Araújo JSTd, Delpino FM, Berra TZ, Moura HSD, Ramos ACV, Nascimento MCd, Alonso JB, Silva RVdS, de Freitas GL, Teibo TKA, et al. Level of Trust of the Population in the Unified Health System in the Midst of the COVID-19 Crisis in Brazil. International Journal of Environmental Research and Public Health. 2022; 19(22):14999. https://doi.org/10.3390/ijerph192214999
Chicago/Turabian StyleAraújo, Juliana Soares Tenório de, Felipe Mendes Delpino, Thaís Zamboni Berra, Heriederson Sávio Dias Moura, Antônio Carlos Vieira Ramos, Murilo César do Nascimento, Jonas Bodini Alonso, Ruan Víctor dos Santos Silva, Giselle Lima de Freitas, Titilade Kehinde Ayandeyi Teibo, and et al. 2022. "Level of Trust of the Population in the Unified Health System in the Midst of the COVID-19 Crisis in Brazil" International Journal of Environmental Research and Public Health 19, no. 22: 14999. https://doi.org/10.3390/ijerph192214999
APA StyleAraújo, J. S. T. d., Delpino, F. M., Berra, T. Z., Moura, H. S. D., Ramos, A. C. V., Nascimento, M. C. d., Alonso, J. B., Silva, R. V. d. S., de Freitas, G. L., Teibo, T. K. A., Gonzales, R. I. C., & Arcêncio, R. A. (2022). Level of Trust of the Population in the Unified Health System in the Midst of the COVID-19 Crisis in Brazil. International Journal of Environmental Research and Public Health, 19(22), 14999. https://doi.org/10.3390/ijerph192214999






