Emergency Department Visits for Heat-Related Emergency Conditions in the United States from 2008–2020
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Variables
2.2. Statistical Analysis
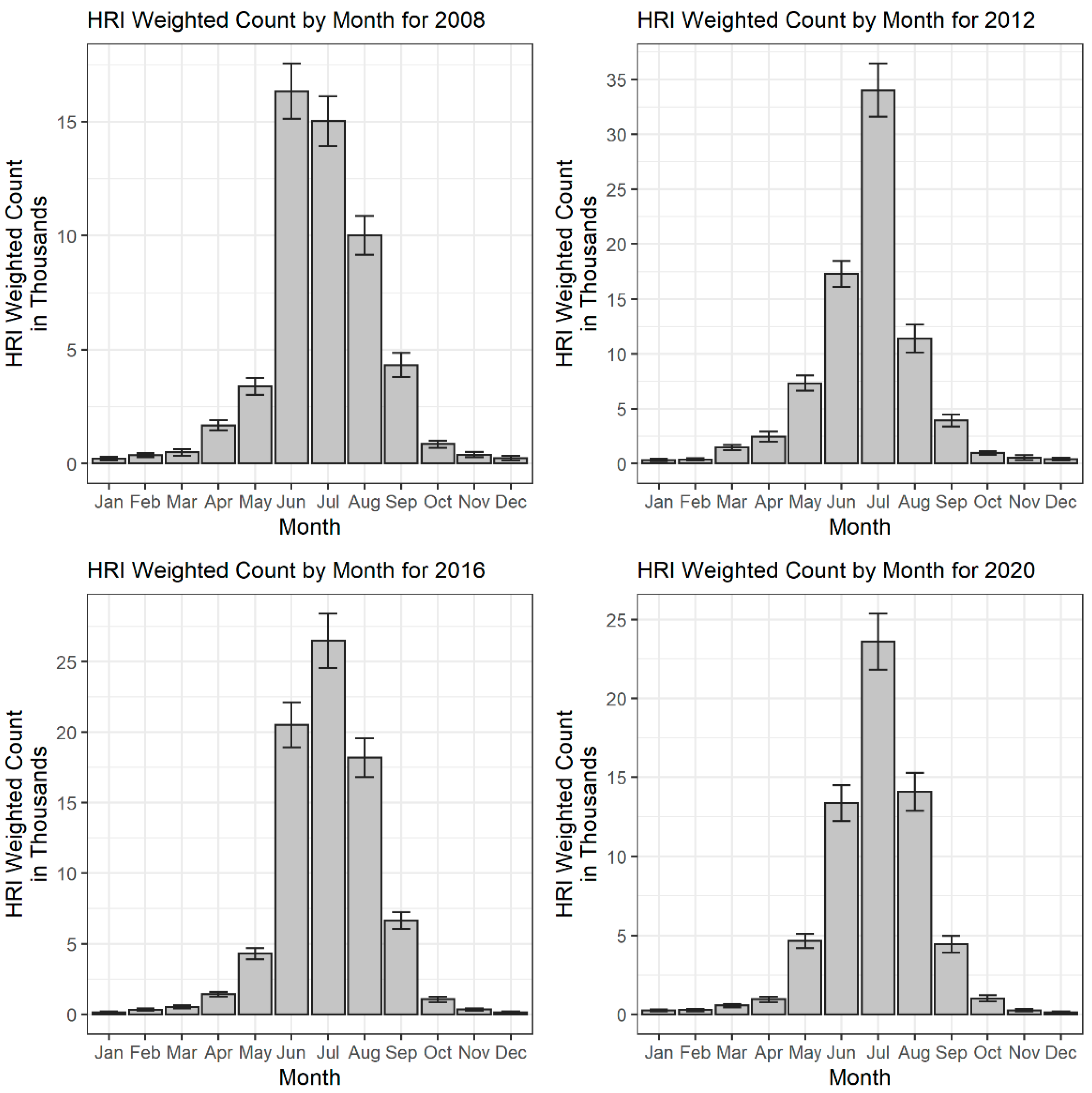
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| ICD-9-CM Code | Diagnosis |
|---|---|
| 992.0 | Heat stroke and sunstroke |
| 992.1 | Heat syncope |
| 992.2 | Heat cramps |
| 992.3 | Heat exhaustion, anhidrotic |
| 992.4 | Heat exhaustion, due to salt depletion |
| 992.5 | Heat exhaustion, unspecified |
| 992.6 | Heat fatigue, transient |
| 992.7 | Heat edema |
| 992.8 | Other specified heat effects |
| 992.9 | Unspecified effects of heat and light |
| E900.0 | Accident caused by excessive heat due to weather conditions |
| E900.9 | Accidents due to excessive heat of unspecified origin |
| ICD-10-CM Code | Diagnosis |
| T67.0 | Heat stroke and sunstroke |
| T67.1 | Heat syncope |
| T67.2 | Heat cramps |
| T67.3 | Heat exhaustion, anhidrotic |
| T67.4 | Heat exhaustion, due to salt depletion |
| T67.5 | Heat exhaustion, unspecified |
| T67.6 | Heat fatigue, transient |
| T67.7 | Heat edema |
| T67.8 | Other specified heat effects |
| T67.9 | Unspecified effects of heat and light |
| V93.2 | Heat exposure on board watercraft |
| X30 | Exposure to excessive natural heat |
| X32 | Exposure to sunlight |
References
- Raftery, A.E.; Zimmer, A.; Frierson, D.M.W.; Startz, R.; Liu, P. Less than 2 °C warming by 2100 unlikely. Nat. Clim. Chang. 2017, 7, 637–641. [Google Scholar] [CrossRef] [PubMed]
- Kalkstein, L.S.; Greene, J.S. An evaluation of climate/mortality relationships in large U.S. cities and the possible impacts of a climate change. Environ. Health Perspect. 1997, 105, 84–93. [Google Scholar] [CrossRef] [PubMed]
- More Intense, More Frequent, and Longer Lasting Heat Waves in the 21st Century. Available online: https://www.science.org/doi/10.1126/science.1098704?cookieSet=1 (accessed on 23 June 2022).
- Habeeb, D.; Vargo, J.; Stone, B. Rising heat wave trends in large US cities. Nat. Hazards 2015, 76, 1651–1665. [Google Scholar] [CrossRef]
- Wilk, P.; Gunz, A.; Maltby, A.; Ravichakaravarthy, T.; Clemens, K.K.; Lavigne, É.; Lim, R.; Vicedo-Cabrera, A.M. Extreme heat and paediatric emergency department visits in Southwestern Ontario. Paediatr. Child Health 2020, 26, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Oray, N.C.; Oray, D.; Aksay, E.; Atilla, R.; Bayram, B. The impact of a heat wave on mortality in the emergency department. Medicine 2018, 97, e13815. [Google Scholar] [CrossRef] [PubMed]
- Yip, F.Y.; Flanders, W.D.; Wolkin, A.; Engelthaler, D.; Humble, W.; Neri, A.; Lewis, L.; Backer, L.; Rubin, C. The impact of excess heat events in Maricopa County, Arizona: 2000–2005. Int. J. Biometeorol. 2008, 52, 765–772. [Google Scholar] [CrossRef] [PubMed]
- Chaseling, G.K.; Iglesies-Grau, J.; Juneau, M.; Nigam, A.; Kaiser, D.; Gagnon, D. Extreme Heat and Cardiovascular Health: What a Cardiovascular Health Professional Should Know. Can. J. Cardiol. 2021, 37, 1828–1836. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Sain, S.; Mearns, L.O.; Anderson, H.A.; Kovats, S.; Ebi, K.L.; Bekkedal, M.Y.; Kanarek, M.S.; Patz, J.A. The impact of extreme heat on morbidity in Milwaukee, Wisconsin. Clim. Chang. 2012, 110, 959–976. [Google Scholar] [CrossRef]
- Hajat, S.; O’Connor, M.; Kosatsky, T. Health effects of hot weather: From awareness of risk factors to effective health protection. Lancet 2010, 375, 856–863. [Google Scholar] [CrossRef]
- Baccini, M.; Kosatsky, T.; Analitis, A.; Anderson, H.R.; D’Ovidio, M.; Menne, B.; Michelozzi, P.; Biggeri, A.; PHEWE Collaborative Group. Impact of heat on mortality in 15 European cities: Attributable deaths under different weather scenarios. J. Epidemiol. Community Health 2011, 65, 64–70. [Google Scholar] [CrossRef]
- Ye, X.; Wolff, R.; Yu, W.; Vaneckova, P.; Pan, X.; Tong, S. Ambient Temperature and Morbidity: A Review of Epidemiological Evidence. Environ. Health Perspect. 2012, 120, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Deschênes, O.; Moretti, E. Extreme Weather Events, Mortality, and Migration. Rev. Econ. Stat. 2009, 91, 659–681. [Google Scholar] [CrossRef]
- Kegel, F.; Luo, O.D.; Richer, S. The Impact of Extreme Heat Events on Emergency Departments in Canadian Hospitals. Wilderness Environ. Med. 2021, 32, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Weinberger, K.R.; Nori-Sarma, A.; Spangler, K.R.; Sun, Y.; Dominici, F.; Wellenius, G.A. Ambient heat and risks of emergency department visits among adults in the United States: Time stratified case crossover study. BMJ 2021, 375, e065653. [Google Scholar] [CrossRef] [PubMed]
- Gauer, R.; Meyers, B.K. Heat-Related Illnesses. Am. Fam. Phys. 2019, 99, 482–489. [Google Scholar] [PubMed]
- Fuhrmann, C.M.; Sugg, M.M.; Konrad, C.E.; Waller, A. Impact of Extreme Heat Events on Emergency Department Visits in North Carolina (2007–2011). J. Community Health 2016, 41, 146–156. [Google Scholar] [CrossRef]
- Basu, R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ. Health 2009, 8, 40. [Google Scholar] [CrossRef]
- Basu, R.; Pearson, D.; Malig, B.; Broadwin, R.; Green, R. The effect of high ambient temperature on emergency room visits. Epidemiology 2012, 23, 813–820. [Google Scholar] [CrossRef]
- Mathes, R.W.; Ito, K.; Lane, K.; Matte, T.D. Real-time surveillance of heat-related morbidity: Relation to excess mortality associated with extreme heat. PLoS ONE 2017, 12, e0184364. [Google Scholar] [CrossRef]
- Knowlton, K.; Rotkin-Ellman, M.; King, G.; Margolis, H.G.; Smith, D.; Solomon, G.; Trent, R.; English, P. The 2006 California Heat Wave: Impacts on Hospitalizations and Emergency Department Visits. Environ. Health Perspect. 2009, 117, 61–67. [Google Scholar] [CrossRef]
- Harduar Morano, L.; Bunn, T.L.; Lackovic, M.; Lavender, A.; Dang, G.T.T.; Chalmers, J.J.; Li, Y.; Zhang, L.; Flammia, D.D. Occupational heat-related illness emergency department visits and inpatient hospitalizations in the southeast region, 2007–2011. Am. J. Ind. Med. 2015, 58, 1114–1125. [Google Scholar] [CrossRef] [PubMed]
- Fechter-Leggett, E.D.; Vaidyanathan, A.; Choudhary, E. Heat Stress Illness Emergency Department Visits in National Environmental Public Health Tracking States, 2005–2010. J. Community Health 2016, 41, 57–69. [Google Scholar] [CrossRef] [PubMed]
- US EPA. Climate Change Indicators: Seasonal Temperature. 2021. Available online: https://www.epa.gov/climate-indicators/climate-change-indicators-seasonal-temperature (accessed on 21 June 2022).
- US EPA. Seasonality and Climate Change. 2021. Available online: https://www.epa.gov/climate-indicators/seasonality-and-climate-change (accessed on 21 June 2022).
- Shifting Seasons. Conservation in a Changing Climate. Available online: https://climatechange.lta.org/climate-impacts/shifting-seasons/ (accessed on 21 June 2022).
- Harduar Morano, L.; Watkins, S.; Kintziger, K. A Comprehensive Evaluation of the Burden of Heat-Related Illness and Death within the Florida Population. Int. J. Environ. Res. Public Health 2016, 13, 551. [Google Scholar] [CrossRef] [PubMed]
- Gacutan, K. Healthcare Cost and Utilization Project—HCUP. 2019. Available online: https://www.hcup-us.ahrq.gov/db/nation/neds/NEDS_Introduction_2020.jsp (accessed on 15 June 2022).
- NEDS Overview. Available online: https://www.hcup-us.ahrq.gov/nedsoverview.jsp (accessed on 13 July 2022).
- Harduar Morano, L.; Watkins, S. Evaluation of Diagnostic Codes in Morbidity and Mortality Data Sources for Heat-Related Illness Surveillance. Public Health Rep. 2017, 132, 326–335. [Google Scholar] [CrossRef] [PubMed]
- National Centers for Environmental Information (NCEI); NOAA National Centers for Environmental Information. Climate at a Glance. Available online: https://www.ncdc.noaa.gov/cag/national/time-series (accessed on 15 June 2022).
- Regulations.gov. Available online: https://www.regulations.gov/document/EPA-HQ-OAR-2013-0566-0218 (accessed on 18 June 2022).
- Leonardi, G.; Hajat, S.; Kovats, R.; Smith, G.; Cooper, D.; Gerard, E. Syndromic surveillance use to detect the early effects of heat-waves: An analysis of NHS Direct data in England. Soz.-Präventivmedizin 2006, 51, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Nitschke, M.; Tucker, G.R.; Hansen, A.L.; Williams, S.; Zhang, Y.; Bi, P. Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: A case-series analysis. Environ. Health 2011, 10, 42. [Google Scholar] [CrossRef]
- Medina-Ramón, M.; Zanobetti, A.; Cavanagh, D.P.; Schwartz, J. Extreme Temperatures and Mortality: Assessing Effect Modification by Personal Characteristics and Specific Cause of Death in a Multi-City Case-Only Analysis. Environ. Health Perspect. 2006, 114, 1331–1336. [Google Scholar] [CrossRef]
- Stafoggia, M.; Forastiere, F.; Agostini, D.; Biggeri, A.; Bisanti, L.; Cadum, E.; Caranci, N.; de’Donato, F.; De Lisio, S.; De Maria, M.; et al. Vulnerability to heat-related mortality: A multicity, population-based, case-crossover analysis. Epidemiology 2006, 17, 315–323. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. Bridged-Race Population Estimates 1990–2019 Request. Available online: https://wonder.cdc.gov/bridged-race-v2019.html (accessed on 14 June 2022).
- Zanobetti, A.; O’Neill, M.S.; Gronlund, C.J.; Schwartz, J.D. Susceptibility to Mortality in Weather Extremes: Effect Modification by Personal and Small Area Characteristics in a Multi-City Case-Only Analysis. Epidemiology 2013, 24, 809–819. [Google Scholar] [CrossRef]
- Licker, R.; Dahl, K.; Abatzoglou, J.T. Quantifying the impact of future extreme heat on the outdoor work sector in the United States. Elem. Sci. Anthr. 2022, 10, 48. [Google Scholar] [CrossRef]
- US EPA. Climate Change Indicators: U.S. and Global Temperature. 2016. Available online: https://www.epa.gov/climate-indicators/climate-change-indicators-us-and-global-temperature (accessed on 20 June 2022).
- Reid, C.E.; O’neill, M.S.; Gronlund, C.J.; Brines, S.J.; Brown, D.G.; Diez-Roux, A.V.; Schwartz, J. Mapping Community Determinants of Heat Vulnerability. Environ. Health Perspect. 2009, 117, 1730–1736. [Google Scholar] [CrossRef] [PubMed]
- Kalkstein, L.S. Saving lives during extreme weather in summer. BMJ 2000, 321, 650–651. [Google Scholar] [CrossRef] [PubMed]
- Kilbourne, E.M.; Choi, K.; Jones, T.S.; Thacker, S.B. Risk Factors for Heatstroke: A Case-Control Study. JAMA 1982, 247, 3332–3336. [Google Scholar] [CrossRef] [PubMed]
- Vaidyanathan, A.; Saha, S.; Vicedo-Cabrera, A.M.; Gasparrini, A.; Abdurehman, N.; Jordan, R.; Hawkins, M.; Hess, J.; Elixhauser, A. Assessment of extreme heat and hospitalizations to inform early warning systems. Proc. Natl. Acad. Sci. USA 2019, 116, 5420–5427. [Google Scholar] [CrossRef] [PubMed]
- Grumm, R.; Arnott, J.; Halblaub, J. The epic eastern North American warm episode of March 2012. J. Oper. Meteorol. 2014, 2, 36–50. [Google Scholar] [CrossRef]
- National Centers for Environmental Information (NCEI). March 2015 National Climate Report. Available online: https://www.ncei.noaa.gov/access/monitoring/monthly-report/national/201503 (accessed on 20 July 2022).
- National Centers for Environmental Information (NCEI). March 2017 National Climate Report. Available online: https://www.ncei.noaa.gov/access/monitoring/monthly-report/national/201703 (accessed on 20 July 2022).
- Hajat, S.; Kovats, R.S.; Atkinson, R.W.; Haines, A. Impact of hot temperatures on death in London: A time series approach. J. Epidemiol. Community Health 2002, 56, 367–372. [Google Scholar] [CrossRef]
- Kalkstein, A.J.; Kalkstein, L.S.; Vanos, J.K.; Eisenman, D.P.; Grady Dixon, P. Heat/mortality sensitivities in Los Angeles during winter: A unique phenomenon in the United States. Environ. Health 2018, 17, 45. [Google Scholar] [CrossRef]

| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 62,519 | 55,868 | 95,580 | 96,215 | 90,789 | 74,276 | 67,542 | 79,273 | 90,364 | 89,216 | 105,660 | 99,832 | 71,298 |
| Hospital Region | |||||||||||||
| Northeast | 8010 | 5135 | 11,625 | 10,116 | 9969 | 11,846 | 5795 | 6879 | 8107 | 6850 | 10,700 | 8621 | 6057 |
| Midwest | 11,488 | 9758 | 21,560 | 28,646 | 27,704 | 16,122 | 11,213 | 14,054 | 17,838 | 15,452 | 21,049 | 17,634 | 14,126 |
| South | 30,059 | 28,405 | 50,697 | 44,491 | 38,902 | 31,288 | 36,149 | 44,470 | 50,889 | 46,118 | 56,728 | 59,604 | 38,151 |
| West | 12,961 | 12,571 | 11,698 | 12,961 | 14,214 | 15,021 | 14,384 | 13,870 | 13,531 | 20,796 | 17,183 | 13,974 | 12,964 |
| Patient Age | |||||||||||||
| 0–4 | 1161 | 1060 | 1390 | 1426 | 1615 | 1188 | 1487 | 1448 | 960 | 1067 | 1324 | 976 | 586 |
| 5–17 | 8432 | 7557 | 11,203 | 11,368 | 10,339 | 8589 | 7452 | 9244 | 9227 | 9512 | 10,721 | 9044 | 4242 |
| 18–49 | 33,515 | 29,284 | 52,416 | 52,571 | 48,905 | 39,973 | 36,299 | 44,063 | 49,370 | 45,759 | 54,015 | 52,609 | 38,657 |
| 50–64 | 10,585 | 9922 | 17,432 | 17,572 | 16,938 | 13,686 | 12,711 | 14,707 | 17,441 | 18,008 | 21,453 | 20,577 | 14,708 |
| 65–79 | 5648 | 5171 | 8730 | 8882 | 8992 | 7576 | 6853 | 6971 | 9411 | 10,280 | 12,964 | 12,393 | 9635 |
| ≥80 | 3178 | 2875 | 4403 | 4390 | 3995 | 3265 | 2735 | 2829 | 3955 | 4589 | 5184 | 4231 | 3466 |
| Patient Sex | |||||||||||||
| Female | 20,925 | 17,500 | 29,103 | 29,759 | 30,159 | 23,192 | 20,808 | 24,169 | 25,992 | 27,161 | 32,603 | 29,774 | 19,141 |
| Male | 41,573 | 38,288 | 66,444 | 66,413 | 60,627 | 51,078 | 46,724 | 55,104 | 64,360 | 62,056 | 73,041 | 70,047 | 52,147 |
| ZIP Code Income Quartile | |||||||||||||
| 1st (Lowest) | 18,496 | 16,930 | 32,454 | 32,790 | 30,549 | 24,868 | 25,062 | 29,127 | 32,968 | 31,932 | 40,052 | 39,420 | 27,151 |
| 2nd | 18,473 | 15,587 | 26,620 | 25,672 | 23,809 | 20,627 | 19,768 | 20,070 | 25,760 | 25,164 | 29,412 | 25,766 | 20,500 |
| 3rd | 12,674 | 12,226 | 19,338 | 20,799 | 19,916 | 15,666 | 12,161 | 16,966 | 17,453 | 16,791 | 19,312 | 18,912 | 12,442 |
| 4th | 10,603 | 9237 | 14,607 | 14,539 | 14,243 | 11,096 | 8523 | 11,141 | 11,985 | 12,671 | 13,993 | 13,174 | 8901 |
| Payer | |||||||||||||
| Public | 17,448 | 16,641 | 29,367 | 31,654 | 31,159 | 26,053 | 26,471 | 28,506 | 34,215 | 36,802 | 43,724 | 39,536 | 28,928 |
| Private | 24,787 | 21,392 | 34,472 | 33,654 | 30,949 | 24,123 | 21,248 | 27,067 | 29,206 | 27,818 | 32,600 | 30,248 | 20,644 |
| Self-Pay | 12,292 | 11,044 | 21,133 | 19,816 | 18,782 | 16,262 | 13,155 | 16,099 | 18,446 | 16,922 | 20,214 | 21,724 | 15,342 |
| Other | 7723 | 6674 | 10,281 | 10,623 | 9734 | 7714 | 6525 | 7405 | 8312 | 7348 | 8968 | 8221 | 6242 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dring, P.; Armstrong, M.; Alexander, R.; Xiang, H. Emergency Department Visits for Heat-Related Emergency Conditions in the United States from 2008–2020. Int. J. Environ. Res. Public Health 2022, 19, 14781. https://doi.org/10.3390/ijerph192214781
Dring P, Armstrong M, Alexander R, Xiang H. Emergency Department Visits for Heat-Related Emergency Conditions in the United States from 2008–2020. International Journal of Environmental Research and Public Health. 2022; 19(22):14781. https://doi.org/10.3390/ijerph192214781
Chicago/Turabian StyleDring, Penelope, Megan Armstrong, Robin Alexander, and Henry Xiang. 2022. "Emergency Department Visits for Heat-Related Emergency Conditions in the United States from 2008–2020" International Journal of Environmental Research and Public Health 19, no. 22: 14781. https://doi.org/10.3390/ijerph192214781
APA StyleDring, P., Armstrong, M., Alexander, R., & Xiang, H. (2022). Emergency Department Visits for Heat-Related Emergency Conditions in the United States from 2008–2020. International Journal of Environmental Research and Public Health, 19(22), 14781. https://doi.org/10.3390/ijerph192214781






