Sense of Control and Depression during Public Health Restrictions and the COVID-19 Pandemic
Abstract
1. Introduction
1.1. Background
1.2. Current Studies
2. Materials and Methods
2.1. Ethical Statement
2.2. Context
2.3. Participants
2.3.1. Time 1 Participants
2.3.2. Time 1 and 2 Participants
2.4. Measures
2.4.1. Beck Depression Inventory BDI: [21]
2.4.2. Sense of Control Scale SOC: [24]
2.4.3. Experience of Public Health Restrictions PHR: [7]
Restriction Impact (0–50)
Restriction Number
Time 1 versus Time 2 Adaptation
2.5. Procedure
2.6. Analytic Strategy
3. Results
3.1. Time 1 Results
3.1.1. Descriptive Measures
3.1.2. BDI Category, the Sense of Control and Perception of Restrictions
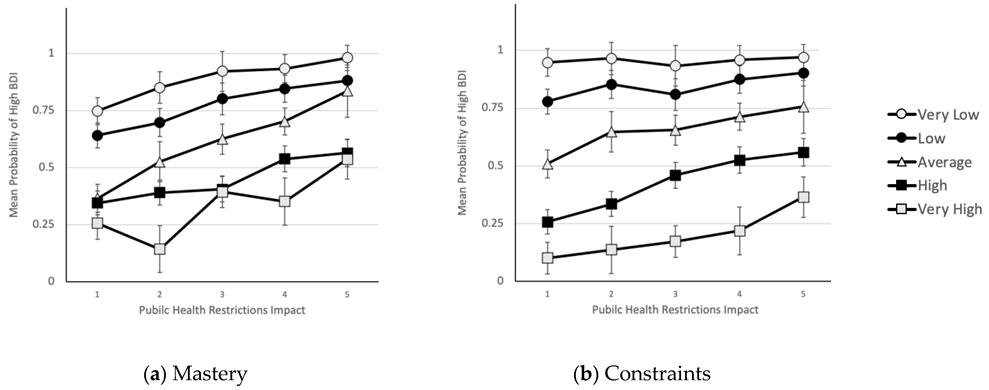
3.1.3. H1. Joint Effects of Predictors on Probability of Being in High BDI Group
3.2. Time 2 Results
3.2.1. Descriptive Measures
3.2.2. H2. Time 1 versus Time 2
3.2.3. H3. Effect of Time 1 Measures on Probability of High BDI at Time 2
4. Discussion
4.1. Limitations and Strengths
4.2. Implications for Mental Health
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

References
- Bueno-Notivol, J.; Gracia-García, P.; Olaya, B.; Lasheras, I.; López-Antón, R.; Santabárbara, J. Prevalence of depression during the COVID-19 outbreak: A meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021, 21, 100196. [Google Scholar] [CrossRef] [PubMed]
- Chu, I.Y.-H.; Alam, P.; Larson, H.J.; Lin, L. Social consequences of mass quarantine during epidemics: A systematic review with implications for the COVID-19 response. J. Travel Med. 2020, 27, taaa192. [Google Scholar] [CrossRef] [PubMed]
- Koffman, J.; Gross, J.; Etkind, S.N.; Selman, L. Uncertainty and COVID-19: How are we to respond? J. R. Soc. Med. 2020, 113, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Gan, Y.; Ma, J.; Wu, J.; Chen, Y.; Zhu, H.; Hall, B.J. Immediate and delayed psychological effects of province-wide lockdown and personal quarantine during the COVID-19 outbreak in China. Psychol. Med. 2022, 52, 1321–1332. [Google Scholar] [CrossRef] [PubMed]
- Brailovskaia, J.; Margraf, J. Predicting adaptive and maladaptive responses to the Coronavirus (COVID-19) outbreak: A prospective longitudinal study. Int. J. Clin. Health Psychol. 2020, 20, 183–191. [Google Scholar] [CrossRef]
- Xiong, P.; Ming, W.-K.; Zhang, C.; Bai, J.; Luo, C.; Cao, W.; Zhang, F.; Tao, Q. Factors influencing mental health among Chinese medical and non-medical students in the early stage of the COVID-19 pandemic. Front. Public Health 2021, 9, 603331. [Google Scholar] [CrossRef]
- Senan, S.; Halbrook, Y.; Kornbrot, D.E.; Msetfi, R.M. Depression symptoms and the perception of public health restrictions during the COVID-19 pandemic in Saudi Arabia: The protective effect of sense of control. Prev. Med. Rep. 2022, 28, 101836. [Google Scholar] [CrossRef]
- Hajek, A.; Sabat, I.; Neumann-Böhme, S.; Schreyögg, J.; Barros, P.P.; Stargardt, T.; König, H.-H. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: Longitudinal evidence from the European COvid Survey (ECOS). J. Affect. Disord. 2022, 299, 517–524. [Google Scholar] [CrossRef]
- Fountoulakis, K.N.; Apostolidou, M.K.; Atsiova, M.B.; Florou, A.K.; Gousiou, D.S.; Katsara, A.R.; Mantzari, S.N.; Padouva-Markoulaki, M.; Padouva-Markoulaki, M.; Papatriantafyllou, E.I.; et al. Self-reported changes in anxiety, depression and suicidality during the COVID-19 lockdown in Greece. J. Affect. Disord. 2021, 279, 624–629. [Google Scholar] [CrossRef]
- Hyland, P.; Shevlin, M.; McBride, O.; Murphy, J.; Karatzias, T.; Bentall, R.P.; Martinez, A.; Vallières, F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020, 142, 249–256. [Google Scholar] [CrossRef]
- Li, J.; Yang, Z.; Qiu, H.; Wang, Y.; Jian, L.; Ji, J.; Li, K. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry 2020, 19, 249. [Google Scholar] [CrossRef] [PubMed]
- Rehman, U.; Shahnawaz, M.G.; Khan, N.H.; Kharshiing, K.D.; Khursheed, M.; Gupta, K.; Kashyap, D.; Uniyal, R. Depression, anxiety and stress among Indians in times of Covid-19 lockdown. Community Ment. Health J. 2021, 57, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Planchuelo-Gómez, Á.; Odriozola-González, P.; Irurtia, M.J.; de Luis-García, R. Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. J. Affect. Disord. 2020, 277, 842–849. [Google Scholar] [CrossRef] [PubMed]
- Ustun, G. Determining depression and related factors in a society affected by COVID-19 pandemic. Int. J. Soc. Psychiatry 2021, 67, 54–63. [Google Scholar] [CrossRef]
- Fancourt, D.; Steptoe, A.; Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. Lancet Psychiatry 2021, 8, 141–149. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Sahni, P.S.; Singh, K.; Sharma, N.; Garg, R. Yoga an effective strategy for self-management of stress-related problems and wellbeing during COVID19 lockdown: A cross-sectional study. PLoS ONE 2021, 16, e0245214. [Google Scholar] [CrossRef]
- Van Mulukom, V.; Muzzulini, B.; Rutjens, B.T.; Van Lissa, C.J.; Farias, M. The psychological impact of threat and lockdowns during the COVID-19 pandemic: Exacerbating factors and mitigating actions. Transl. Behav. Med. 2021, 11, 1318–1329. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 2007, 147, 573–577. [Google Scholar] [CrossRef]
- Breslau, J.; Finucane, M.L.; Locker, A.R.; Baird, M.D.; Roth, E.A.; Collins, R.L. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev. Med. 2021, 143, 106362. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Storch, E.A.; Roberti, J.W.; Roth, D.A. Factor structure, concurrent validity, and internal consistency of the beck depression inventory—Second edition in a sample of college students. Depress. Anxiety 2004, 19, 187–189. [Google Scholar] [CrossRef] [PubMed]
- Loosman, W.; Siegert, C.; Korzec, A.; Honig, A. Validity of the Hospital Anxiety and Depression Scale and the Beck Depression Inventory for use in end-stage renal disease patients. Br. J. Clin. Psychol. 2010, 49, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Gale, T.; Hawley, C. A model for handling missing items on two depression rating scales. Int. Clin. Psychopharmacol. 2001, 16, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Lachman, M.E.; Weaver, S.L. The sense of control as a moderator of social class differences in health and well-being. J. Personal. Soc. Psychol. 1998, 74, 763–773. [Google Scholar] [CrossRef]
- Senan, S.; Msetfi, R.M.; El Keshky, M.; Halbrook, Y.J. The relationship between perception of control and mood: The intervening effect of cultural values in a Saudi Arabian sample. PLoS ONE 2019, 14, e0220509. [Google Scholar] [CrossRef]
- Sugawara, D.; Chishima, Y.; Kubo, T.; Reza, R.I.A.B.R.; Phoo, E.Y.; Ng, S.L.; Masuyama, A.; Gu, Y.; Tee, E.Y. Mental health and psychological resilience during the COVID-19 pandemic: A cross-cultural comparison of Japan, Malaysia, China, and the US. J. Affect. Disord. 2022, 311, 500–507. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef]
- Santomauro, D.F.; Herrera, A.M.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef] [PubMed]
- Qi, T.; Hu, T.; Ge, Q.-Q.; Zhou, X.-N.; Li, J.-M.; Jiang, C.-L.; Wang, W. COVID-19 pandemic related long-term chronic stress on the prevalence of depression and anxiety in the general population. BMC Psychiatry 2021, 21, 380. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.J.; Fusco, R.A. Does sense of control predict depression among individuals after psychiatric hospital discharge? J. Nerv. Ment. Dis. 2015, 203, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Chou, K.-L.; Chi, I. Stressful life events and depressive symptoms: Social support and sense of control as mediators or moderators? Int. J. Aging Hum. Dev. 2001, 52, 155–171. [Google Scholar] [CrossRef]
- Alcover, C.-M.; Rodríguez, F.; Pastor, Y.; Thomas, H.; Rey, M.; Del Barrio, J.L. Group membership and social and personal identities as psychosocial coping resources to psychological consequences of the COVID-19 confinement. Int. J. Environ. Res. Public Health 2020, 17, 7413. [Google Scholar] [CrossRef]
- Curl, A.L.; Wolf, K.E. The impact of COVID-19 on depressive symptoms and loneliness for middle-aged and older adults. Sustainability 2022, 14, 6316. [Google Scholar] [CrossRef]
- Frazier, P.; Liu, Y.; Asplund, A.; Meredith, L.; Nguyen-Feng, V.N. US college student mental health and COVID-19: Comparing pre-pandemic and pandemic timepoints. J. Am. Coll. Health 2021, 1–11. [Google Scholar] [CrossRef]
- Precht, L.-M.; Margraf, J.; Stirnberg, J.; Brailovskaia, J. It’s all about control: Sense of control mediates the relationship between physical activity and mental health during the COVID-19 pandemic in Germany. Curr. Psychol. 2021, 1–9. [Google Scholar] [CrossRef]
- Mohd Fauzi, M.F.; Mohd Yusoff, H.; Muhamad Robat, R.; Mat Saruan, N.A.; Ismail, K.I.; Mohd Haris, A.F. Doctors’ mental health in the midst of COVID-19 pandemic: The roles of work demands and recovery experiences. Int. J. Environ. Res. Public Health 2020, 17, 7340. [Google Scholar] [CrossRef]
- Shinan-Altman, S.; Levkovich, I. Are personal resources and perceived stress associated with psychological outcomes among Israeli teachers during the third COVID-19 lockdown? Int. J. Environ. Res. Public Health 2022, 19, 5634. [Google Scholar] [CrossRef]
- Skapinakis, P.; Bellos, S.; Oikonomou, A.; Dimitriadis, G.; Gkikas, P.; Perdikari, E.; Mavreas, V. Depression and its relationship with coping strategies and illness perceptions during the COVID-19 lockdown in Greece: A cross-sectional survey of the population. Depress. Res. Treat. 2020, 2020, 3158954. [Google Scholar] [CrossRef] [PubMed]
- Stimpson, J.P. Prospective evidence for a reciprocal relationship between sense of control and depressive symptoms following a flood. Stress Health J. Int. Soc. Investig. Stress 2006, 22, 161–166. [Google Scholar] [CrossRef]
| BDI Category | Low BDI | High BDI | Independent t-Test | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor Variables | M | SE | 95% | 95% | M | SE | 95% | 95% | |
| LCL | UCL | LCL | UCL | ||||||
| Mastery | 5.53 | 0.08 | 5.38 | 5.68 | 4.64 | 0.08 | 4.48 | 4.79 | 7.61 * |
| Constraints | 5.15 | 0.08 | 4.99 | 5.31 | 3.76 | 0.07 | 3.61 | 3.9 | 12.48 * |
| Restriction Impact | 29.03 | 0.89 | 27.26 | 30.8 | 34.08 | 0.71 | 32.69 | 35.48 | 4.42 * |
| Restrictions Number | 7.27 | 0.38 | 6.52 | 8.02 | 9.8 | 0.25 | 9.3 | 10.3 | 5.77 * |
| Variables | B | SE | Wald | df | p | Exp(B) | ESw |
|---|---|---|---|---|---|---|---|
| 1. Restrictions number | 0.104 | 0.043 | 5.79 | 1 | 0.016 | 1.11 | 0.136 |
| 2. Constraints | −2.117 | 0.281 | 56.79 | 1 | <0.001 | 0.12 | 0.425 |
| 3. Mastery × Restrictions Impact | −0.017 | 0.006 | 8.1 | 1 | 0.004 | −0.017 | 0.161 |
| 4. Constraints × Restrictions Impact | 0.028 | 0.008 | 11.83 | 1 | <0.001 | 0.028 | 0.194 |
| Constant | 7.965 | 1.153 | 47.73 | 1 | <0.001 | 2877.17 |
| BDI | Low BDI | High BDI | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | M | SE | LCL | UCL | M | SE | LCL | UCL | F | p |
| Mastery | 5.70 | 0.17 | 5.35 | 6.05 | 4.69 | 0.26 | 4.14 | 5.24 | 11.39 | 0.002 |
| Constraint | 5.56 | 0.16 | 5.22 | 5.89 | 3.85 | 0.26 | 3.3 | 4.39 | 34.72 | <0.001 |
| Impact | 31.93 | 1.26 | 29.37 | 34.50 | 31.53 | 2.86 | 25.47 | 37.59 | 0.02 | 0.882 |
| Number | 7.23 | 0.77 | 5.67 | 8.80 | 7.94 | 0.78 | 6.29 | 9.59 | 0.36 | 0.551 |
| Predictor | Time | M | SE | LCL | UCL | F | p | Cohen’s d |
|---|---|---|---|---|---|---|---|---|
| BDI | 1 | 12.51 | 1.34 | 9.81 | 15.21 | 9.12 | 0.004 | 0.45 |
| 2 | 9.88 | 1.25 | 7.36 | 12.39 | ||||
| Mastery | 1 | 5.20 | 0.16 | 4.88 | 5.52 | 1.70 | 0.199 | −0.19 |
| 2 | 5.34 | 0.16 | 5.02 | 5.66 | ||||
| Constraints | 1 | 4.64 | 0.18 | 4.29 | 5.00 | 7.79 | 0.008 | −0.41 |
| 2 | 4.94 | 0.18 | 4.57 | 5.31 | ||||
| Impact | 1 | 32.68 | 1.38 | 29.9 | 35.47 | 0.49 | 0.486 | 0.10 |
| 2 | 31.79 | 1.29 | 29.19 | 34.38 | ||||
| Number | 1 | 8.49 | 0.63 | 7.22 | 9.75 | 5.78 | 0.020 | 0.33 |
| 2 | 7.50 | 0.56 | 6.36 | 8.62 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Msetfi, R.; Kornbrot, D.; Halbrook, Y.J.; Senan, S. Sense of Control and Depression during Public Health Restrictions and the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 14429. https://doi.org/10.3390/ijerph192114429
Msetfi R, Kornbrot D, Halbrook YJ, Senan S. Sense of Control and Depression during Public Health Restrictions and the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(21):14429. https://doi.org/10.3390/ijerph192114429
Chicago/Turabian StyleMsetfi, Rachel, Diana Kornbrot, Yemaya J. Halbrook, and Salha Senan. 2022. "Sense of Control and Depression during Public Health Restrictions and the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 21: 14429. https://doi.org/10.3390/ijerph192114429
APA StyleMsetfi, R., Kornbrot, D., Halbrook, Y. J., & Senan, S. (2022). Sense of Control and Depression during Public Health Restrictions and the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(21), 14429. https://doi.org/10.3390/ijerph192114429






