Serious Injury in Metropolitan and Regional Victoria: Exploring Travel to Treatment and Utilisation of Post-Discharge Health Services by Injury Type
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Variables
2.4. Data Measurement
2.5. Statistical Methods
3. Results
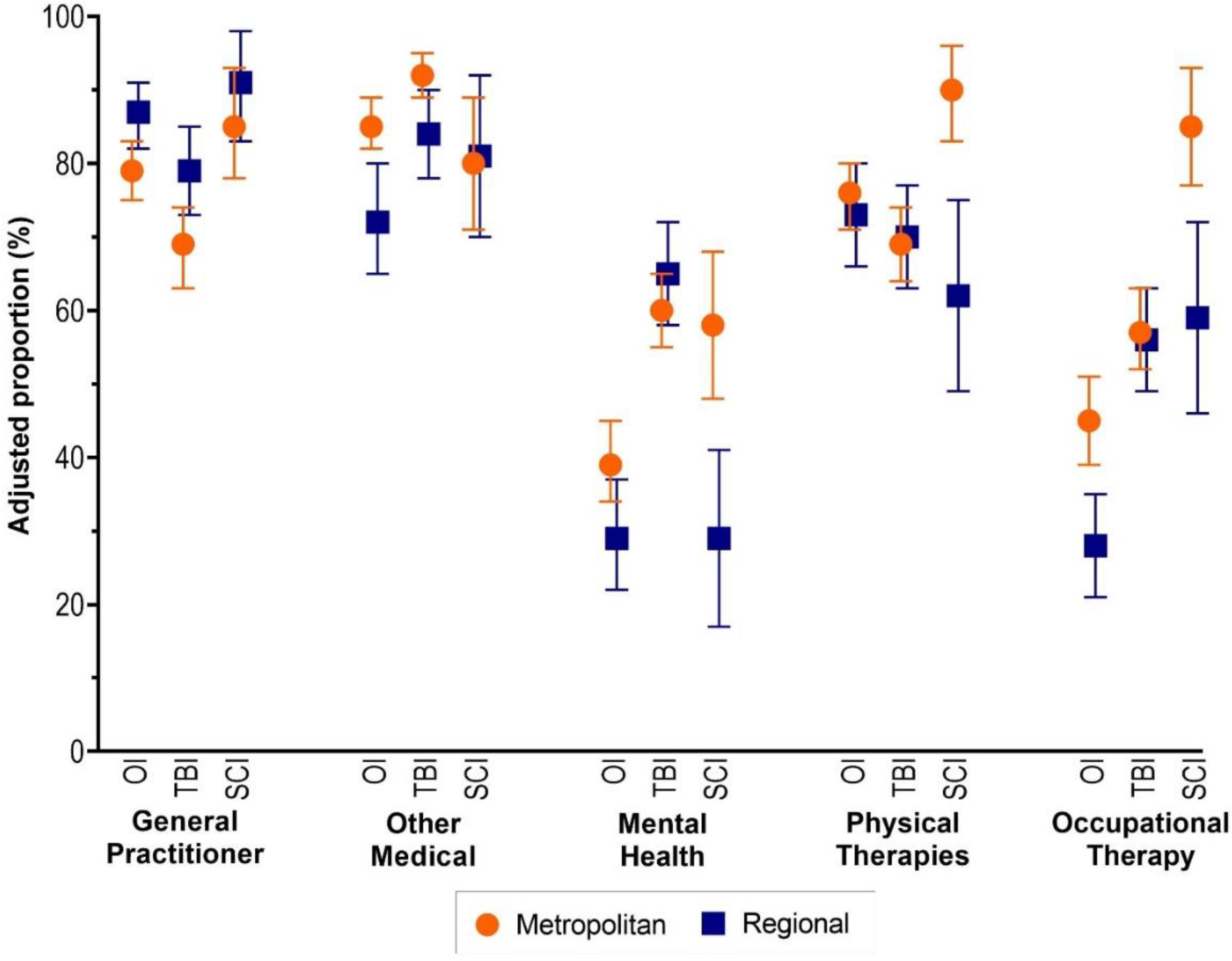
3.1. Service Use
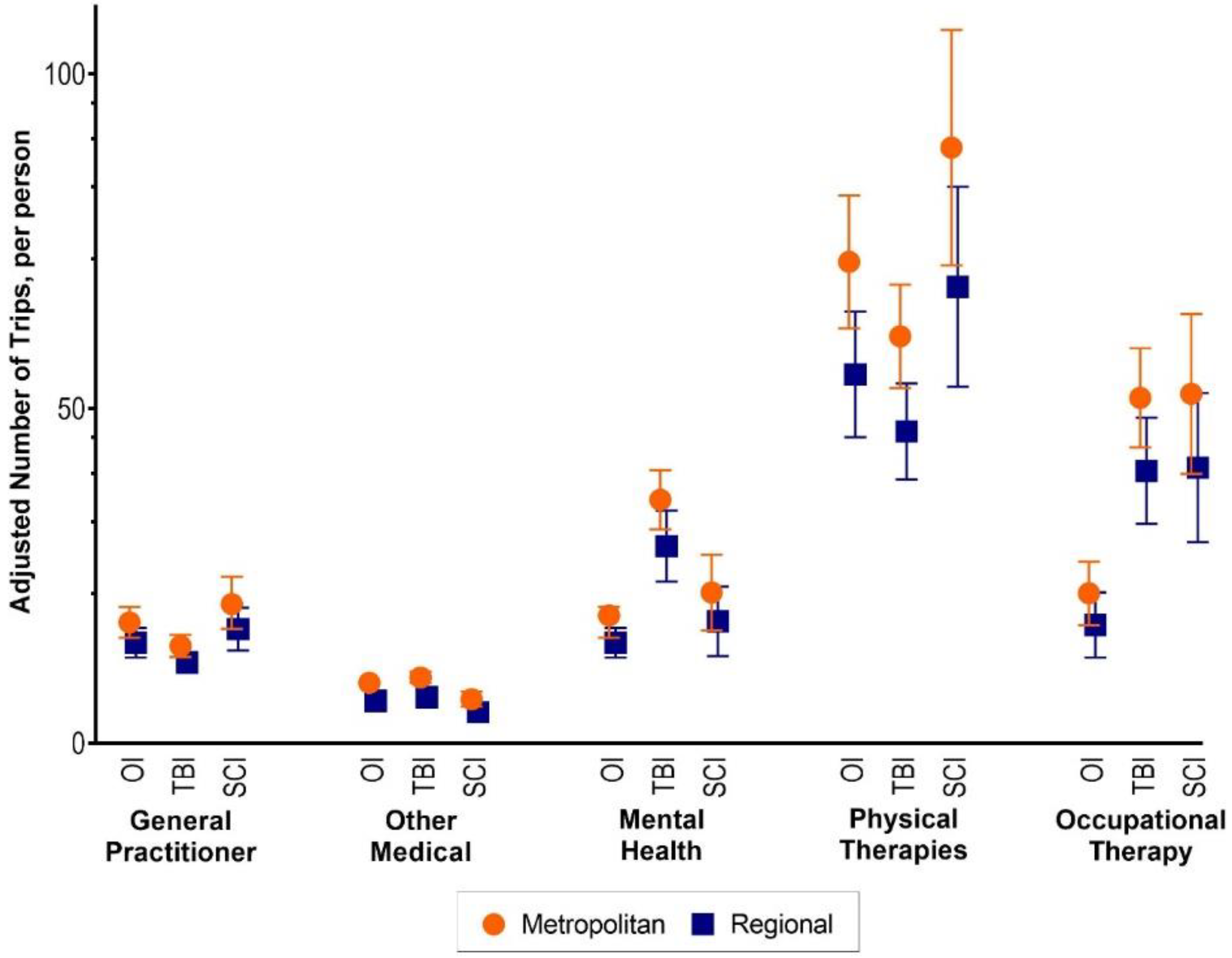
3.2. Number of Trips
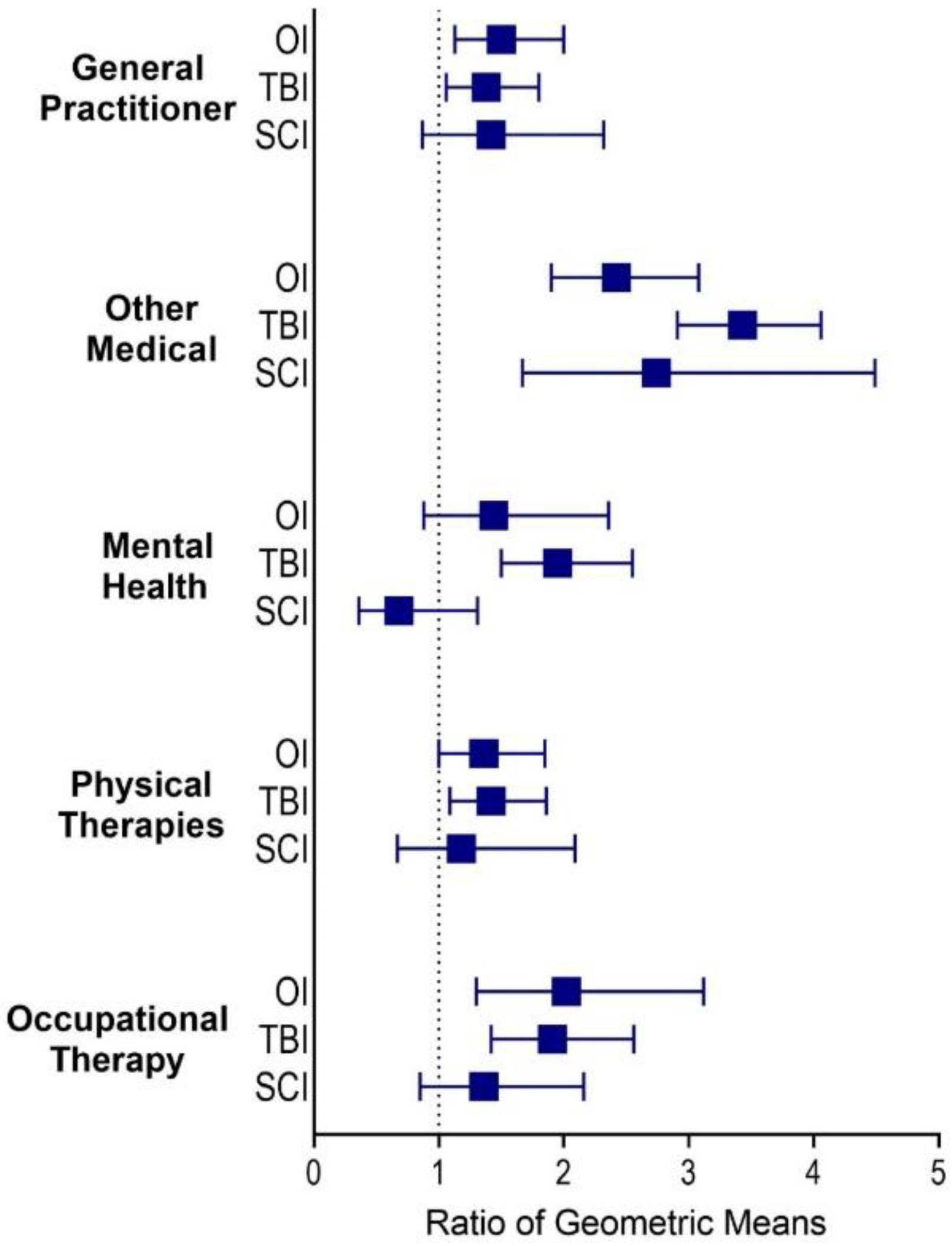
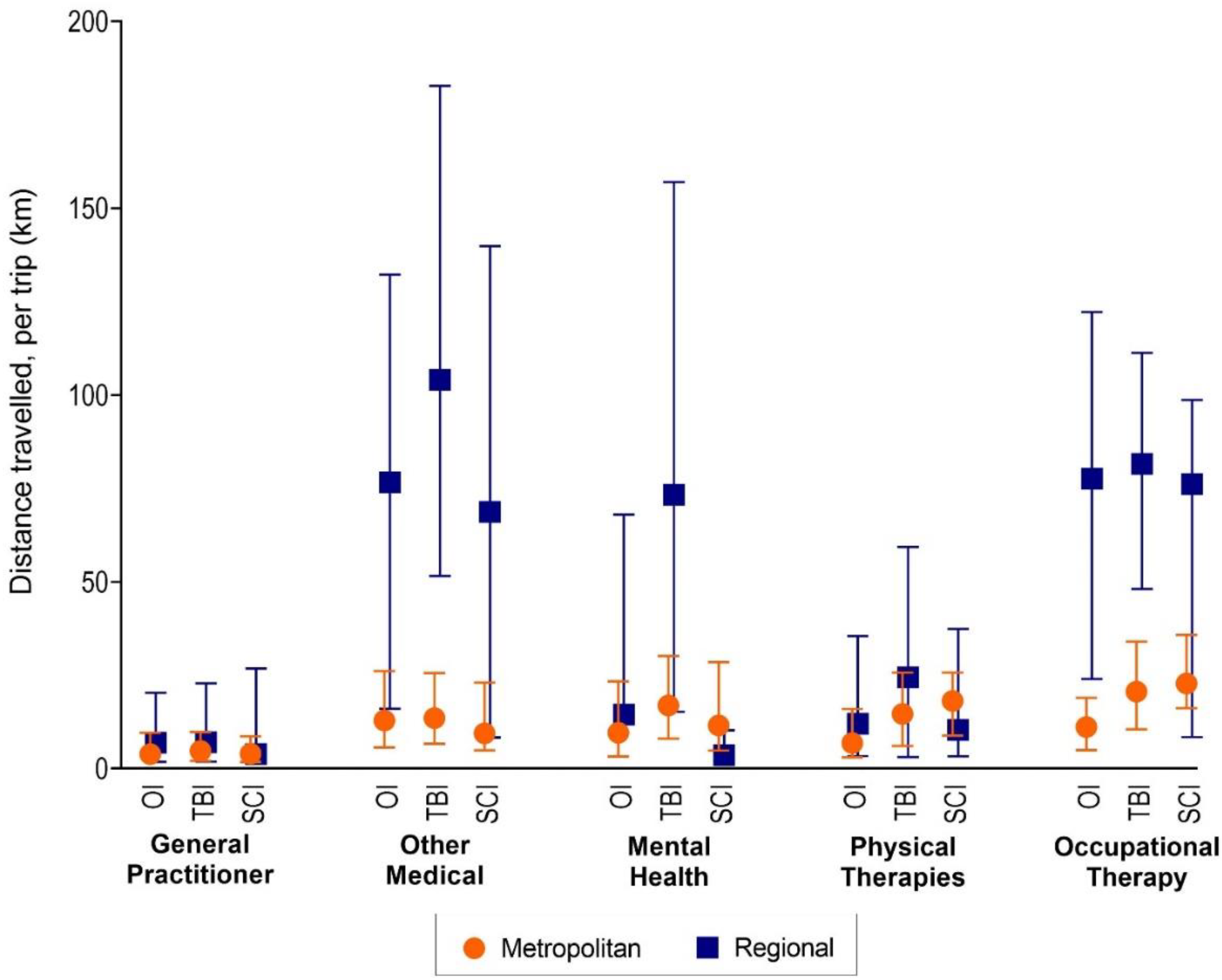
3.3. Distance Travelled
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Recommendation | Page | ||
|---|---|---|---|
| Title and abstract | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract | 1 |
| (b) Provide in the abstract an informative and balanced summary of what was performed and what was found | 1 | ||
| Introduction | |||
| Background/rationale | 2 | Explain the scientific background and rationale for the investigation being reported | 1 |
| Objectives | 3 | State specific objectives, including any prespecified hypotheses | 2 |
| Methods | |||
| Study design | 4 | Present key elements of study design early in the paper | 2 |
| Setting | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | 2–3 |
| Participants | 6 | (a) Give the eligibility criteria and the sources and methods of selection of participants. Describe methods of follow-up | 3–4 |
| (b) For matched studies, give matching criteria and number of exposed and unexposed | n/a | ||
| Variables | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | 4 |
| Data sources/measurement | 8 | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | 2–3 |
| Bias | 9 | Describe any efforts to address potential sources of bias | - |
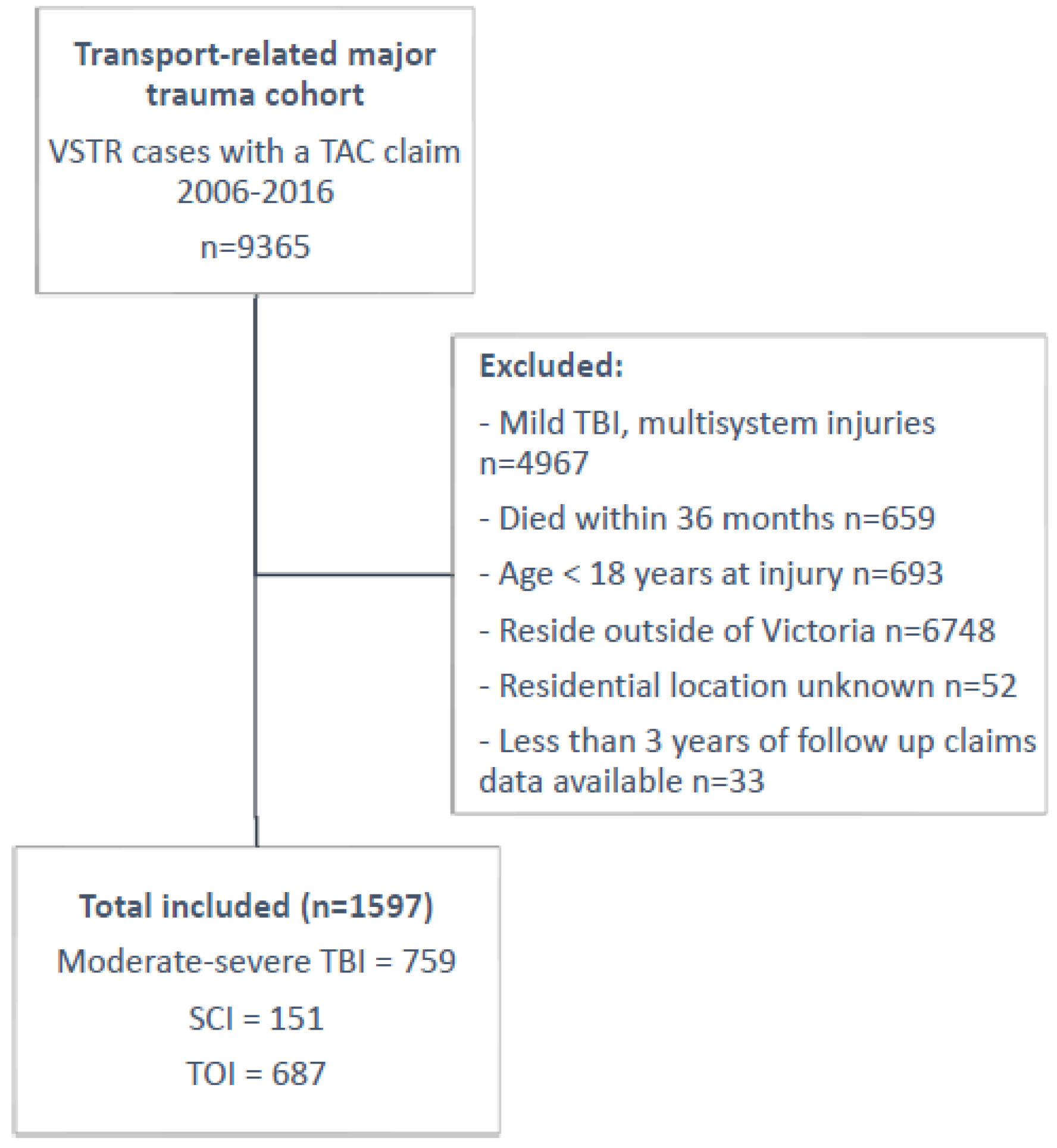
| Study size | 10 | Explain how the study size was arrived at | Figure 1 |
| Quantitative variables | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | 4 |
| Statistical methods | 12 | (a) Describe all statistical methods, including those used to control for confounding | 4 |
| (b) Describe any methods used to examine subgroups and interactions | 4–5 | ||
| (c) Explain how missing data were addressed | n/a | ||
| (d) If applicable, explain how loss to follow-up was addressed | n/a | ||
| (e) Describe any sensitivity analyses | - | ||
| Results | |||
| Participants | 13 | (a) Report numbers of individuals at each stage of study, e.g., numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analysed | 5 |
| (b) Give reasons for non-participation at each stage | n/a | ||
| © Consider use of a flow diagram | Figure 1 | ||
| Descriptive data | 14 | (a) Give characteristics of study participants (e.g., demographic, clinical, social) and information on exposures and potential confounders | Table 1 |
| (b) Indicate number of participants with missing data for each variable of interest | n/a | ||
| (c) Summarise follow-up time (e.g., average and total amount) | 5 | ||
| Outcome data | 15 | Report numbers of outcome events or summary measures over time | 5–8 |
References
- World Health Organization. World Health Organization Global Burden of Disease; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Post, M.W.M.; van Leeuwen, C.M.C. Psychosocial issues in spinal cord injury: A review. Spinal Cord 2012, 50, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Dahm, J.; Ponsford, J. Comparison of long-term outcomes following traumatic injury: What is the unique experience for those with brain injury compared with orthopaedic injury? Injury 2015, 46, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Gabbe, B.J.; Simpson, P.M.; Cameron, P.A.; Ponsford, J.; Lyons, R.A.; Collie, A.; Harrison, J.E.; Ameratunga, S.; Nunn, A.; Braaf, S.; et al. Long-term health status and trajectories of seriously injured patients: A population-based longitudinal study. PLoS Med. 2017, 14, e1002322. [Google Scholar] [CrossRef] [PubMed]
- Keeves, J.; Gabbe, B.J.; Ekegren, C.L.; Fry, R.; Beck, B. Regional variation in travel to health services following transport-related major trauma. Injury 2021, 53, 1707–1715. [Google Scholar] [CrossRef]
- Gabbe, B.J.; Sleney, J.S.; Gosling, C.M.; Wilson, K.; Hart, M.J.; Sutherland, A.M.; Christie, N. Patient perspectives of care in a regionalised trauma system: Lessons from the Victorian State Trauma System. Med. J. Aust. 2013, 198, 149–152. [Google Scholar] [CrossRef]
- Keeves, J.; Braaf, S.C.; Ekegren, C.L.; Beck, B.; Gabbe, B.J. Caring for people with serious injuries in urban and regional communities: A qualitative investigation of healthcare providers’ perceptions. Disabil. Rehabil. 2020, 43, 3052–3060. [Google Scholar] [CrossRef]
- Keeves, J.; Braaf, S.C.; Ekegren, C.L.; Beck, B.; Gabbe, B.J. Access to Healthcare Following Serious Injury: Perspectives of Allied Health Professionals in Urban and Regional Settings. Int. J. Environ. Res. Public Health 2021, 18, 1230. [Google Scholar] [CrossRef]
- Ruseckaite, R.; Gabbe, B.; Vogel, A.P.; Collie, A. Health care utilisation following hospitalisation for transport-related injury. Injury 2012, 43, 1600–1605. [Google Scholar] [CrossRef]
- Victorian State Trauma Registry Annual Report 2019–2020; Victorian State Trauma Outcomes Registry and Monitoring Group: Melbourne, Australia, 2021.
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull. World Health Organ. 2007, 85, 867–872. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Regional Population Growth, Australia, 2017–2018. Available online: www.abs.gov.au/ausstats/abs@.nsf/0/B7616AB91C66CDCFCA25827800183B7B?Opendocument (accessed on 9 July 2019).
- Cameron, P.A.; Gabbe, B.J.; Cooper, D.J.; Walker, T.; Judson, R.; McNeil, J. A statewide system of trauma care in Victoria: Effect on patient survival. Med. J. Aust. 2008, 189, 546–550. [Google Scholar] [CrossRef]
- Transport Accident Act 1986. Melbourne, Australia. 2020. Available online: https://www.legislation.vic.gov.au/in-force/acts/transport-accident-act-1986/151 (accessed on 1 September 2022).
- Victorian State Trauma Registry Annual Report 2019–2020. Melbourne, Australia. Available online: https://www.monash.edu/__data/assets/pdf_file/0008/2706047/VSTR-Annual-Report-2019-20-WEB_FINAL.pdf (accessed on 1 September 2022).
- Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS): Volume 5-Remoteness Structure, July 2011. Available online: http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/A277D01B6AF25F64CA257B03000D7EED/$File/1270055005_july%202011.pdf (accessed on 13 October 2020).
- Pink, B. Information Paper: An Introduction to Socio-Economic Indexes for Areas (SEIFA), 2006; Australian Bureau of Statistics: Canberra, Australia, 2008.
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Ronca, E.; Scheel-Sailer, A.; Eriks-Hoogland, I.; Brach, M.; Debecker, I.; Gemperli, A. Factors influencing specialized health care utilization by individuals with spinal cord injury: A cross-sectional survey. Spinal Cord 2021, 59, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Gabbe, B.J.; Sutherland, A.M.; Williamson, O.D.; Cameron, P.A. Use of health care services 6 months following major trauma. Aust. Health Rev. 2007, 31, 628–632. [Google Scholar] [CrossRef] [PubMed]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2009; Volume 892. [Google Scholar]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Touhami, D.; Brach, M.; Essig, S.; Ronca, E.; Debecker, I.; Eriks-Hoogland, I.; Scheel-Sailer, A.; Münzel, N.; Gemperli, A. First contact of care for persons with spinal cord injury: A general practitioner or a spinal cord injury specialist? BMC Fam. Pract. 2021, 22, 1–195. [Google Scholar] [CrossRef] [PubMed]
- LaVela, S.L.; Smith, B.; Weaver, F.M.; Miskevics, S.A. Geographical proximity and health care utilization in veterans with SCI&D in the USA. Soc. Sci. Med. 2004, 59, 2387–2399. [Google Scholar] [CrossRef]
- Kettlewell, J.; Timmons, S.; Bridger, K.; Kendrick, D.; Kellezi, B.; Holmes, J.; Patel, P.; Radford, K. A study of mapping usual care and unmet need for vocational rehabilitation and psychological support following major trauma in five health districts in the UK. Clin. Rehabil. 2021, 35, 750–764. [Google Scholar] [CrossRef]
- Khan, F.; Baguley, I.J.; Cameron, I.D. 4: Rehabilitation after traumatic brain injury. Med. J. Aust. 2003, 178, 290–295. [Google Scholar] [CrossRef]
- Jonnagaddala, J.; Godinho, M.A.; Liaw, S.-T. From telehealth to virtual primary care in Australia? a rapid scoping review. Int. J. Med. Inform. 2021, 151, 104470. [Google Scholar] [CrossRef]
- Bell, N.; Kidanie, T.; Cai, B.; Krause, J.S. Geographic variation in outpatient health care service utilization after spinal cord injury. Arch. Phys. Med. Rehabil. 2017, 98, 341–346. [Google Scholar] [CrossRef]
- Ronca, E.; Scheel-Sailer, A.; Koch, H.G.; Essig, S.; Brach, M.; Münzel, N.; Gemperli, A.; Group, S.S. Satisfaction with access and quality of healthcare services for people with spinal cord injury living in the community. J. Spinal Cord Med. 2020, 43, 111–121. [Google Scholar] [CrossRef]
- Simpson, G.K.; Daher, M.; Hodgkinson, A.; Strettles, B. Comparing the Injury Profile, Service Use, Outcomes, and Comorbidities of People With Severe TBI Across Urban, Regional, and Remote Populations in New South Wales: A Multicentre Study. J. Head Trauma Rehabil. 2016, 31, E26–E38. [Google Scholar] [CrossRef] [PubMed]
- Xia, T.; Iles, R.; Newnam, S.; Lubman, D.I.; Collie, A. Patterns of health service use following work-related injury and illness in Australian truck drivers: A latent class analysis. Am. J. Ind. Med. 2020, 63, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Legg, M.; Foster, M.; Jones, R.; Kendall, M.; Fleming, J.; Nielsen, M.; Kendall, E.; Borg, D.; Geraghty, T. The impact of obstacles to health and rehabilitation services on functioning and disability: A prospective survey on the 12-months after discharge from specialist rehabilitation for acquired brain injury. Disabil. Rehabil. 2022, 44, 5919–5929. [Google Scholar] [CrossRef] [PubMed]
- Beatty, P.W.; Hagglund, K.J.; Neri, M.T.; Dhont, K.R.; Clark, M.J.; Hilton, S.A. Access to health care services among people with chronic or disabling conditions: Patterns and predictors. Arch. Phys. Med. Rehabil. 2003, 84, 1417–1425. [Google Scholar] [CrossRef]
- Ronca, E.; Brunkert, T.; Koch, H.G.; Jordan, X.; Gemperli, A. Residential location of people with chronic spinal cord injury: The importance of local health care infrastructure. BMC Health Serv. Res. 2018, 18, 657. [Google Scholar] [CrossRef] [PubMed]
- Mitsch, V.; Curtin, M.; Badge, H. The provision of brain injury rehabilitation services for people living in rural and remote New South Wales, Australia. Brain Inj. 2014, 28, 1504–1513. [Google Scholar] [CrossRef]
- Archer, K.R.; Castillo, R.C.; MacKenzie, E.J.; Bosse, M.J.; Group, L.S. Perceived need and unmet need for vocational, mental health, and other support services after severe lower-extremity trauma. Arch. Phys. Med. Rehabil. 2010, 91, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Cox, R.J.; Amsters, D.I.; Pershouse, K.J. The need for a multidisciplinary outreach service for people with spinal cord injury living in the community. Clin. Rehabil. 2001, 15, 600–606. [Google Scholar] [CrossRef]


| All Cases (1597) | TOI (687) | TBI (759) | SCI (151) | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Gender | ||||
| Male | 1122 (70.3) | 461 (67.1) | 537 (70.8) | 124 (82.1) |
| Female | 475 (29.7) | 226 (32.9) | 222 (29.2) | 27 (17.9) |
| Age group, years | ||||
| 18–24 | 480 (30.1) | 153 (22.1) | 297 (39.1) | 31 (20.5) |
| 25–34 | 367 (23.0) | 151 (22.0) | 175 (23.1) | 41 (27.2) |
| 35–44 | 275 (17.2) | 123 (17.9) | 123 (16.2) | 29 (19.2) |
| 45–54 | 206 (12.9) | 104 (15.1) | 82 (10.8) | 20 (13.2) |
| 55–64 | 120 (7.5) | 67 (9.8) | 42 (5.5) | 11 (7.3) |
| 65–74 | 76 (4.8) | 39 (5.7) | 24 (3.1) | 13 (8.6) |
| 75+ | 73 (4.6) | 51 (7.4) | 16 (2.1) | 6 (4.0) |
| Injury Severity Score, median (IQR) | 20 (13–29) | 13 (9–14) | 29 (22–38) | 29 (24–33) |
| CCI [22] weight (CCI) [1] | ||||
| 0 | 857 (53.5) | 521 (75.6) | 235 (30.8) | 101 (66.4) |
| 1 | 582 (36.4) | 126 (18.3) | 424 (55.6) | 33 (21.7) |
| >1 | 142 (8.9) | 32 (4.6) | 98 (12.9) | 13 (8.6) |
| Acute hospital LOS (days), median (IQR) | 13 (7–24) | 8 (5–13) | 18 (11–29) | 24 (13–39) |
| Region (ARIA+ 2016) | ||||
| Major cities | 1040 (65.1) | 441 (65.2) | 507 (66.8) | 92 (60.9) |
| Inner regional | 438 (27.4) | 184 (26.8) | 205 (27.0) | 49 (32.5) |
| Outer regional | 119 (7.5) | 62 (9.0) | 47 (6.2) | 10 (6.6) |
| Socioeconomic status (IRSAD) | ||||
| 1 (most disadvantaged) | 268 (16.8) | 128 (18.6) | 118 (15.5) | 22 (14.5) |
| 2 | 168 (10.5) | 72 (10.5) | 81 (10.6) | 15 (9.9) |
| 3 | 309 (19.3) | 128 (18.6) | 150 (19.8) | 31 (20.5) |
| 4 | 432 (27.1) | 189 (27.5) | 202 (26.6) | 41 (27.2) |
| 5 (least disadvantaged) | 420 (26.3) | 170 (24.7) | 208 (27.4) | 42 (27.8) |
| Discharge destination | ||||
| Home | 287 (18.0) | 237 (34.5) | 41 (5.4) | 9 (6.0) |
| Other (e.g., inpatient rehabilitation) | 1310 (82.0) | 450 (65.4) | 718 (94.6) | 142 (94.0) |
| Road user [2] | ||||
| Motor vehicle driver or passenger | 881 (55.2) | 348 (50.6) | 451 (59.5) | 82 (53.9) |
| Motorcyclist | 347 (21.7) | 198 (28.8) | 99 (13.0) | 50 (32.9) |
| Pedestrian | 244 (15.4) | 85 (12.4) | 154 (20.3) | 6 (4.0) |
| Bicyclist | 91 (5.7) | 42 (6.1) | 41 (5.4) | 8 (5.3) |
| All Cases | TBI | SCI | TOI | |||||
|---|---|---|---|---|---|---|---|---|
| (n = 1597) | (n = 759) | (n = 151) | (n = 687) | |||||
| n | % | n | % | n | % | n | % | |
| Physiotherapy | 59,532 | 30.7 | 27,556 | 27.0 | 9667 | 31.7 | 22,309 | 36.5 |
| Occupational Therapy | 34,268 | 17.7 | 23,026 | 22.5 | 6557 | 21.5 | 4685 | 7.7 |
| GP Consult | 20,078 | 10.4 | 8791 | 8.6 | 2937 | 9.6 | 8350 | 13.7 |
| Psychology | 18,907 | 9.7 | 14,480 | 14.1 | 1285 | 4.2 | 3142 | 5.1 |
| Nursing | 13,289 | 6.9 | 2436 | 2.4 | 6032 | 19.8 | 4821 | 7.9 |
| Medical (other) | 10,972 | 5.7 | 6315 | 6.2 | 803 | 2.6 | 3854 | 6.3 |
| Speech Therapy | 8373 | 4.3 | 8143 | 7.9 | 165 | 0.5 | 65 | 0.1 |
| Hydrotherapy | 6917 | 3.6 | 1727 | 1.7 | 233 | 0.8 | 4957 | 8.1 |
| Exercise Physiology | 6832 | 3.5 | 1816 | 1.8 | 839 | 2.8 | 4177 | 6.8 |
| Vocational counselling | 4175 | 2.2 | 1720 | 1.7 | 359 | 1.2 | 2096 | 3.4 |
| Social Work | 1792 | 0.9 | 1203 | 1.2 | 313 | 1.0 | 276 | 0.5 |
| Psychiatry | 1584 | 0.8 | 1049 | 1.0 | 80 | 0.3 | 455 | 0.7 |
| Podiatry | 1193 | 0.6 | 348 | 0.3 | 551 | 1.8 | 294 | 0.5 |
| Osteopathy | 1017 | 0.5 | 306 | 0.3 | 112 | 0.4 | 599 | 1.0 |
| Dental | 990 | 0.5 | 864 | 0.8 | 55 | 0.2 | 71 | 0.1 |
| Dietitian | 800 | 0.4 | 511 | 0.5 | 186 | 0.6 | 103 | 0.2 |
| Case Conferences | 741 | 0.4 | 444 | 0.4 | 30 | 0.1 | 267 | 0.4 |
| Chiropractor | 680 | 0.4 | 380 | 0.4 | 66 | 0.2 | 234 | 0.4 |
| Attendant carer | 623 | 0.3 | 444 | 0.4 | 119 | 0.4 | 60 | 0.1 |
| Paramedical (other) | 557 | 0.3 | 443 | 0.4 | 36 | 0.1 | 78 | 0.1 |
| Acupuncture | 468 | 0.2 | 275 | 0.3 | 29 | 0.1 | 164 | 0.3 |
| Optical | 291 | 0.2 | 257 | 0.3 | 6 | <0.1 | 28 | <0.1 |
| Total | 194,079 | 102,534 | 30,460 | 61,085 | ||||
| Participants Using Service (n, %) | Service Use, Adjusted OR (95%CI) | p * | Trips per Person, Median (IQR) | Adjusted IRR (95%CI) | p† | |
|---|---|---|---|---|---|---|
| General Practitioner | ||||||
| TOI | ||||||
| Major cities | 329 (74.6) | Reference | 9 (4–22) | Reference | ||
| Regional | 206 (83.7) | 1.76 (1.1–2.9) | 0.02 | 9 (3–21) | 0.81 (0.66–0.99) | 0.04 |
| TBI | ||||||
| Major cities | 370 (73.0) | Reference | 9 (3–18) | Reference | ||
| Regional | 211 (83.7) | 1.76 (1.1–2.8) | 0.02 | 10 (4–22) | 0.90 (0.75–1.1) | 0.31 |
| SCI | ||||||
| Major cities | 80 (87.0) | Reference | 18.5 (10.5–30) | Reference | ||
| Regional | 54 (91.5) | 1.73 (0.5–5.4) | 0.35 | 15 (6–23) | 0.65 (0.5–0.9) | 0.02 |
| Medical Specialists | ||||||
| TOI | ||||||
| Major cities | 360 (81.6) | Reference | 5 (2–11) | Reference | ||
| Regional | 160 (65.0) | 0.44 (0.28–0.70) | 0.001 | 3 (2–8) | 0.71 (0.6–0.9) | <0.001 |
| TBI | ||||||
| Major cities | 477 (94.1) | Reference | 8 (4–14) | Reference | ||
| Regional | 220 (87.3) | 0.43 (0.24–0.78) | 0.01 | 5 (3–9.5) | 0.65 (0.6–0.8) | <0.001 |
| SCI | ||||||
| Major cities | 76 (82.6) | Reference | 4 (2–9.5) | Reference | ||
| Regional | 49 (83.1) | 1.07 (0.42–2.70) | 0.89 | 4 (2–8) | 0.90 (0.6–1.2) | 0.51 |
| Mental Health | ||||||
| TOI | ||||||
| Major cities | 158 (35.8) | Reference | 11 (4–26) | Reference | ||
| Regional | 56 (22.8) | 0.63 (0.41–0.96) | 0.03 | 7 (4–23) | 0.88 (0.6–1.3) | 0.47 |
| TBI | ||||||
| Major cities | 330 (65.1) | Reference | 23.5 (8–54) | Reference | ||
| Regional | 169 (67.1) | 1.23 (0.84–1.81) | 0.29 | 16 (6–36) | 0.78 (0.6–1.0) | 0.05 |
| SCI | ||||||
| Major cities | 57 (62.0) | Reference | 14 (7–35) | Reference | ||
| Regional | 17 (28.8) | 0.28 (0.1–0.6) | 0.001 | 10 (4–17) | 0.84 (0.5–1.5) | 0.58 |
| Physical Therapies | ||||||
| TOI | ||||||
| Major cities | 322 (73.0) | Reference | 42 (15–102) | Reference | ||
| Regional | 176 (71.5) | 0.87 (0.57–1.33) | 0.54 | 34 (14–74.5) | 0.76 (0.6–0.9) | 0.01 |
| TBI | ||||||
| Major cities | 355 (70.0) | Reference | 40 (14–85) | Reference | ||
| Regional | 181 (71.8) | 1.08 (0.72–1.62) | 0.71 | 34 (10–72) | 0.81 (0.6–1.0) | 0.07 |
| SCI | ||||||
| Major cities | 84 (91.3) | Reference | 87 (41–131.5) | Reference | ||
| Regional | 39 (66.1) | 0.18 (0.07–0.45) | <0.001 | 46 (9–92) | 0.63 (0.41–0.95) | 0.03 |
| Occupational Therapy | ||||||
| TOI | ||||||
| Major cities | 165 (37.4) | Reference | 9 (2–25) | Reference | ||
| Regional | 55 (22.4) | 0.45 (0.29–0.69) | <0.001 | 4 (2–22) | 0.76 (0.5–1.1) | 0.17 |
| TBI | ||||||
| Major cities | 317 (62.5) | Reference | 30 (8–73) | Reference | ||
| Regional | 154 (61.1) | 0.95 (0.65–1.39) | 0.81 | 24.5 (5–57) | 0.89 (0.7–1.2) | 0.40 |
| SCI | ||||||
| Major cities | 81 (88.0) | Reference | 49 (14–93) | Reference | ||
| Regional | 39 (66.1) | 0.24 (0.10–0.58) | 0.001 | 11 (3–62) | 0.55 (0.3–0.9) | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Keeves, J.; Gabbe, B.; Arnup, S.; Ekegren, C.; Beck, B. Serious Injury in Metropolitan and Regional Victoria: Exploring Travel to Treatment and Utilisation of Post-Discharge Health Services by Injury Type. Int. J. Environ. Res. Public Health 2022, 19, 14063. https://doi.org/10.3390/ijerph192114063
Keeves J, Gabbe B, Arnup S, Ekegren C, Beck B. Serious Injury in Metropolitan and Regional Victoria: Exploring Travel to Treatment and Utilisation of Post-Discharge Health Services by Injury Type. International Journal of Environmental Research and Public Health. 2022; 19(21):14063. https://doi.org/10.3390/ijerph192114063
Chicago/Turabian StyleKeeves, Jemma, Belinda Gabbe, Sarah Arnup, Christina Ekegren, and Ben Beck. 2022. "Serious Injury in Metropolitan and Regional Victoria: Exploring Travel to Treatment and Utilisation of Post-Discharge Health Services by Injury Type" International Journal of Environmental Research and Public Health 19, no. 21: 14063. https://doi.org/10.3390/ijerph192114063
APA StyleKeeves, J., Gabbe, B., Arnup, S., Ekegren, C., & Beck, B. (2022). Serious Injury in Metropolitan and Regional Victoria: Exploring Travel to Treatment and Utilisation of Post-Discharge Health Services by Injury Type. International Journal of Environmental Research and Public Health, 19(21), 14063. https://doi.org/10.3390/ijerph192114063







