Knowledge, Attitudes and Practices Related to Medication, Antibiotics, and Vaccination among Public Service Population: National Survey Conducted in France
Abstract
1. Introduction
2. Materials and Methods
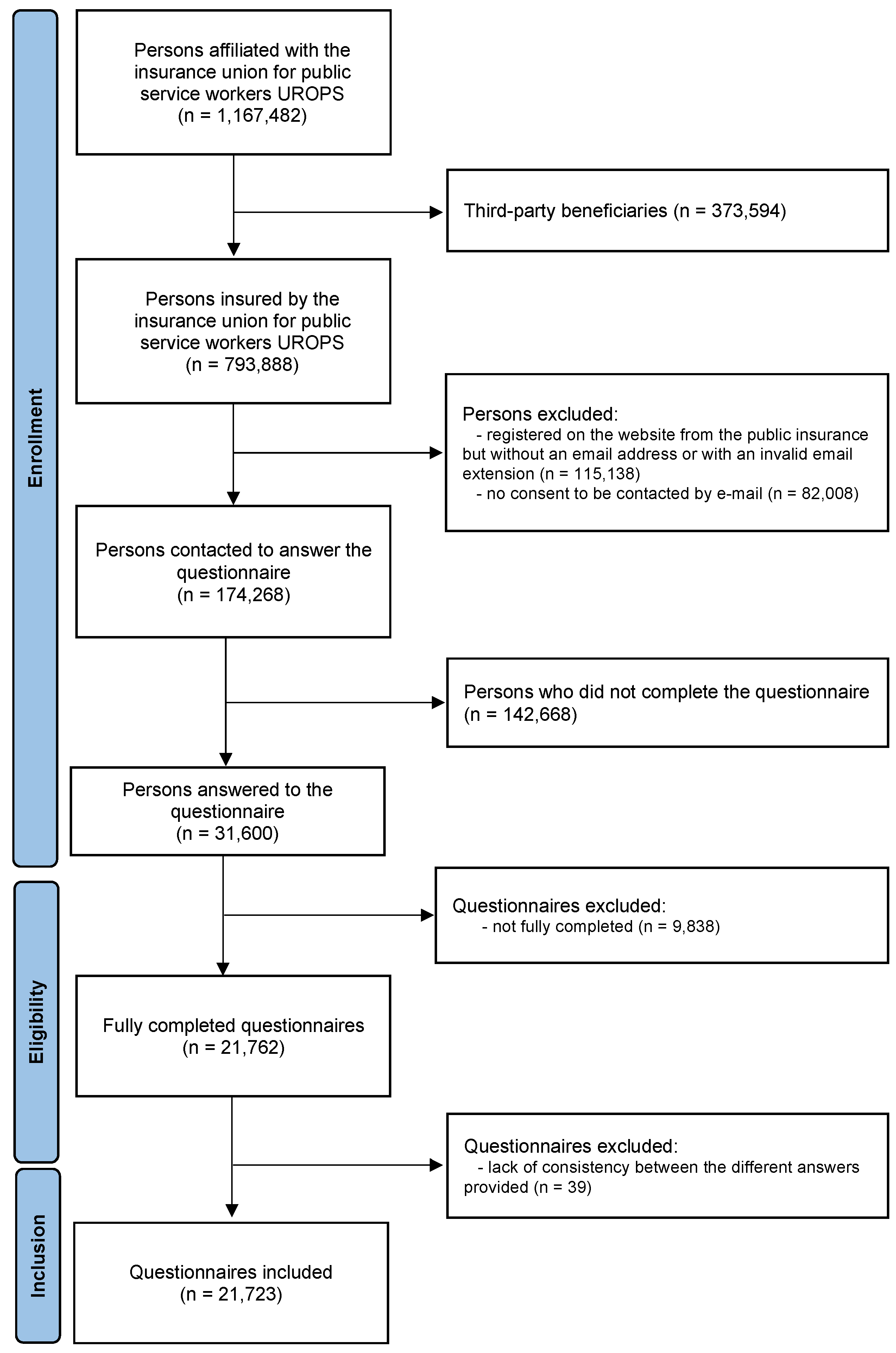
2.1. Study Design
2.2. Selection of Respondents
2.3. Ethics
2.4. Measurement Tool
2.5. Statistical Analysis
- -
- The levels of knowledge related to antibiotics or vaccination were evaluated post-collection using the responses of the 4 statements; “low” when zero or 1 right answer was provided, “moderate” for 2 or 3 right answers and “high” for 4 right answers;
- -
- Polymedication has been defined as taking at least 3 medications per day;
- -
- Antibiotic misuse was defined as (i) self-interruption of the prescription duration, or (ii) taking non-prescribed antibiotics for himself, his children or relatives. The polymedicated respondents were identified as respondents with at least 3 medications per day;
- -
- A proactive behavior was identified among respondents when: (i) self-evaluation by the respondent of the need for antibiotics and asking the doctor for a prescription, or (ii) they had already discussed their medication with their physician/pharmacist on their own initiative, or (iii) if they were taking medication for better sleep, they had already tried non-medicinal methods, or (iv) if they were taking medication for stress or anxiety, they had already tried non-medicinal methods;
- -
- Vaccinophobia was defined by the combination of four kinds of behavior: The vaccinophobic respondents were identified as respondents (i) who are not up to date with their vaccines, and (ii) not interested in receiving additional information on vaccines or vaccination, (iii) would not be vaccinated regardless of the conditions of access to vaccines, and (iv) would not be vaccinated regardless of the cost of vaccines.
3. Results
3.1. Characteristics of Respondents and Sample Size
3.2. Distribution of Respondents According to the Occupational Status
3.3. Socio-Demographic Characteristics According to the Occupational Status
3.4. Knowledge, Attitudes and Practices Related to Antibiotics, Medication and Vaccination According to the Occupational Status
3.5. Determinants of Risky Behaviors and Practices with Public Service Population in France
3.5.1. Determinants of the Polymedication
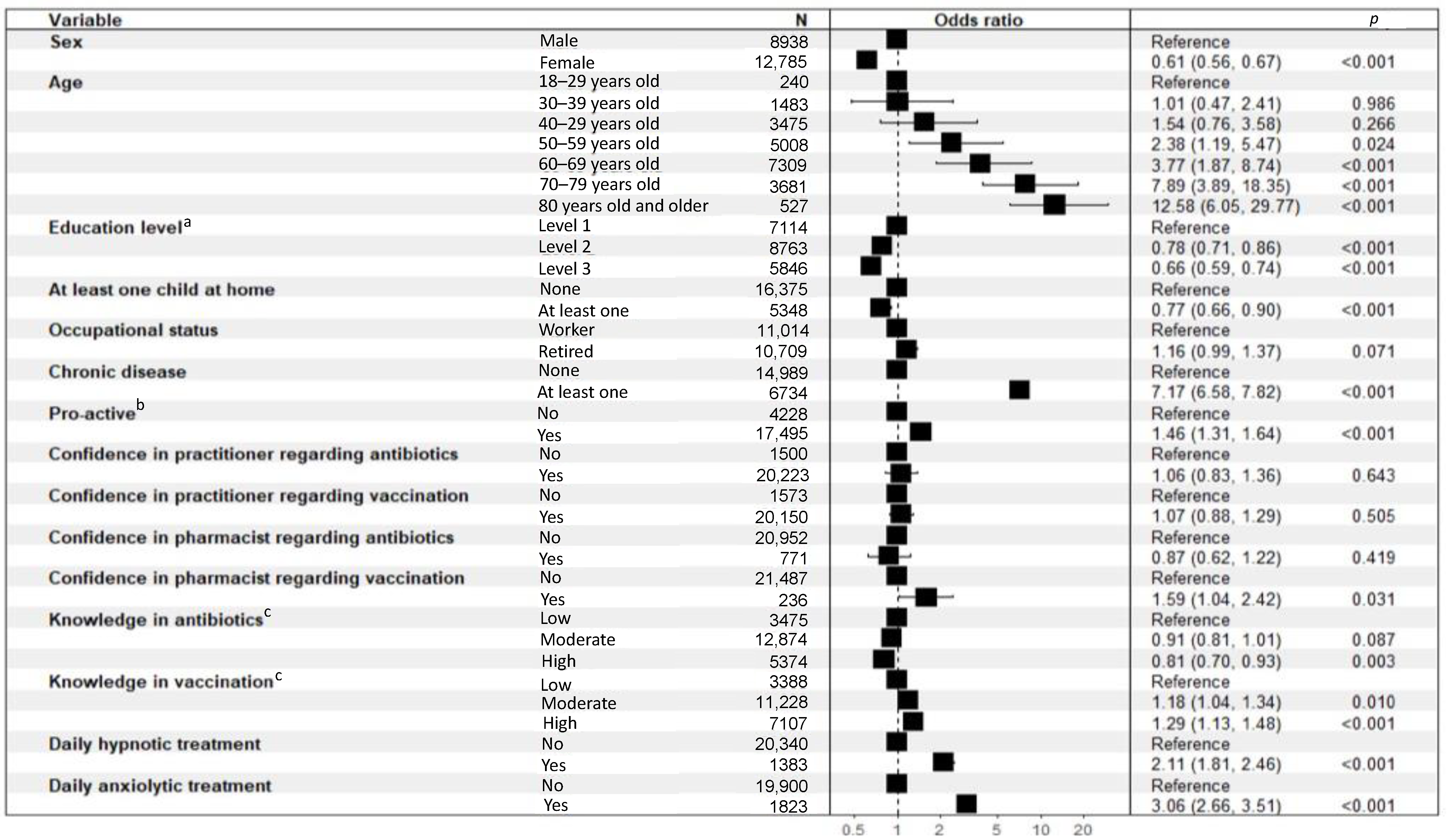
3.5.2. Determinants of the Daily Use of Anxiolytic or Hypnotic Treatments
3.5.3. Determinants of the Misuse of Antibiotics
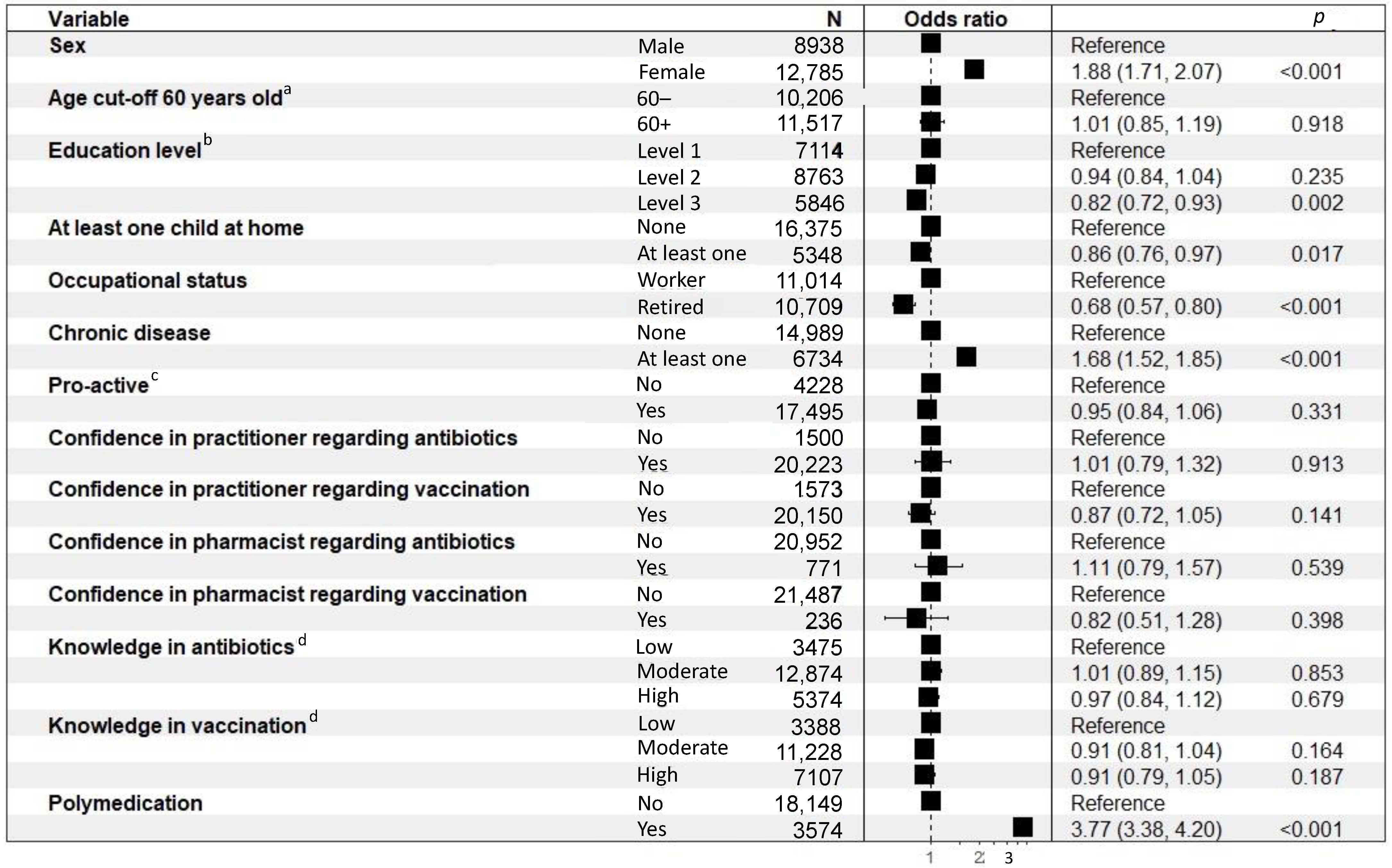
3.5.4. Determinants of Vaccinophobia
4. Discussion
4.1. Key Points Concerning the Population
4.2. Key Points Concerning the Anxiolytics and Hypnotics
4.3. Key Points Concerning the Polymedication
4.4. Key Points Concerning the Antibiotics
4.5. Key Points Concerning the Vaccinophobia
4.6. Key Points Concerning Confidence in Trusting Information Source
4.7. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sengupta, S.; Chattopadhyay, M.K.; Grossart, H.-P. The Multifaceted Roles of Antibiotics and Antibiotic Resistance in Nature. Front. Microbiol. 2013, 4, 47. [Google Scholar] [CrossRef] [PubMed]
- Machowska, A.; Stålsby Lundborg, C. Drivers of Irrational Use of Antibiotics in Europe. Int. J. Environ. Res. Public Health 2018, 16, 27. [Google Scholar] [CrossRef] [PubMed]
- Etzioni-Friedman, T.; Etzioni, A. Adherence to Immunization: Rebuttal of Vaccine Hesitancy. Acta Haematol. 2021, 144, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Crimmins, E.M. Lifespan and Healthspan: Past, Present, and Promise. Gerontologist 2015, 55, 901–911. [Google Scholar] [CrossRef]
- Sharma, M.; Loh, K.P.; Nightingale, G.; Mohile, S.G.; Holmes, H.M. Polypharmacy and Potentially Inappropriate Medication Use in Geriatric Oncology. J. Geriatr. Oncol. 2016, 7, 346–353. [Google Scholar] [CrossRef]
- Aljeaidi, M.S.; Haaksma, M.L.; Tan, E.C.K. Polypharmacy and Trajectories of Health-Related Quality of Life in Older Adults: An Australian Cohort Study. Qual. Life Res. 2022, 31, 2663–2671. [Google Scholar] [CrossRef]
- Van Wilder, L.; Devleesschauwer, B.; Clays, E.; Pype, P.; Vandepitte, S.; De Smedt, D. Polypharmacy and Health-Related Quality of Life/Psychological Distress Among Patients With Chronic Disease. Prev. Chronic Dis. 2022, 19, E50. [Google Scholar] [CrossRef]
- Fröhlich, S.E.; Zaccolo, A.V.; da Silva, S.L.C.; Mengue, S.S. Association between Drug Prescribing and Quality of Life in Primary Care. Pharm. World Sci. 2010, 32, 744–751. [Google Scholar] [CrossRef]
- Poole, K.; George, R.; Decraene, V.; Shankar, K.; Cawthorne, J.; Savage, N.; Welfare, W.; Dodgson, A. Active Case Finding for Carbapenemase-Producing Enterobacteriaceae in a Teaching Hospital: Prevalence and Risk Factors for Colonization. J. Hosp. Infect. 2016, 94, 125–129. [Google Scholar] [CrossRef]
- Lee, J.-H. Perspectives towards Antibiotic Resistance: From Molecules to Population. J. Microbiol. 2019, 57, 181–184. [Google Scholar] [CrossRef]
- O’Neill, J. AMR Review Paper-Tackling a Crisis for the Health and Wealth of Nations. AMR Rev. Pap. 2014, 1, 2–14. [Google Scholar]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Intensive Care Med. 2021, 47, 1181–1247. [Google Scholar] [CrossRef] [PubMed]
- Shaghaghi, A.; Asadi, M.; Allahverdipour, H. Predictors of Self-Medication Behavior: A Systematic Review. Iran. J. Public Health 2014, 43, 136–146. [Google Scholar] [PubMed]
- Katsuki, M.; Yamagishi, C.; Matsumori, Y.; Koh, A.; Kawamura, S.; Kashiwagi, K.; Kito, T.; Entani, A.; Yamamoto, T.; Ikeda, T.; et al. Questionnaire-Based Survey on the Prevalence of Medication-Overuse Headache in Japanese One City-Itoigawa Study. Neurol. Sci. 2022, 43, 3811–3822. [Google Scholar] [CrossRef]
- Sabuncu, E.; David, J.; Bernède-Bauduin, C.; Pépin, S.; Leroy, M.; Boëlle, P.-Y.; Watier, L.; Guillemot, D. Significant Reduction of Antibiotic Use in the Community after a Nationwide Campaign in France, 2002–2007. PLoS Med. 2009, 6, e1000084. [Google Scholar] [CrossRef] [PubMed]
- Giry, M.; Pulcini, C.; Rabaud, C.; Boivin, J.M.; Mauffrey, V.; Birgé, J. Acceptability of Antibiotic Stewardship Measures in Primary Care. Med. Mal. Infect. 2016, 46, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Rosman, S.; Le Vaillant, M.; Pelletier-Fleury, N. Gaining Insight into Benzodiazepine Prescribing in General Practice in France: A Data-Based Study. BMC Fam. Pract. 2011, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Cengotitabengoa, M.; Diaz-Gutierrez, M.J.; Besga, A.; Bermúdez-Ampudia, C.; López, P.; Rondon, M.B.; Stewart, D.E.; Perez, P.; Gutierrez, M.; Gonzalez-Pinto, A. Benzodiazepine Prescriptions and Falls in Older Men and Women. Rev. Psiquiatr. Salud Ment. (Engl. Ed.) 2018, 11, 12–18. [Google Scholar] [CrossRef]
- Schuster, M.; Duclos, P. WHO Recommendations Regarding Vaccine Hesitancy. Vaccine 2015, 33, 4155–4218. [Google Scholar]
- Hudson, A.; Montelpare, W.J. Predictors of Vaccine Hesitancy: Implications for COVID-19 Public Health Messaging. Int. J. Environ. Res. Public Health 2021, 18, 8054. [Google Scholar] [CrossRef]
- Geneau, R. Editorial-Pulling Health Promotion and Chronic Disease Prevention from the Margins of the Global Public Health Agenda—Again. Health Promot. Chronic Dis. Prev. Can. 2021, 41, 71–72. [Google Scholar] [CrossRef] [PubMed]
- Antimicrobial Consumption Database (ESAC-Net). Available online: https://www.ecdc.europa.eu/en/antimicrobial-consumption/surveillance-and-disease-data/database (accessed on 30 September 2022).
- Herr, M.; Grondin, H.; Sanchez, S.; Armaingaud, D.; Blochet, C.; Vial, A.; Denormandie, P.; Ankri, J. Polypharmacy and Potentially Inappropriate Medications: A Cross-Sectional Analysis among 451 Nursing Homes in France. Eur. J. Clin. Pharmacol. 2017, 73, 601–608. [Google Scholar] [CrossRef] [PubMed]
- L’état de Santé de la Population en France-Rapport 2017|Direction de la Recherche, des Études, de l’évaluation et des Statistiques. Available online: https://drees.solidarites-sante.gouv.fr/publications-documents-de-reference/rapports/letat-de-sante-de-la-population-en-france-rapport-2017 (accessed on 30 September 2022).
- Gordon, R.S. An Operational Classification of Disease Prevention. Public Health Rep. 1983, 98, 107–109. [Google Scholar]
- Mittelmark, M.; Sagy, S.; Eriksson, M.; Bauer, G.; Pelikan, J.; Lindström, B.; Espnes, G. The Handbook of Salutogenesis; Springer: Cham, Switzerland, 2022. [Google Scholar]
- Bezes, P.; Jeannot, G. The Development and Current Features of the French Civil Service System. In Civil Service Systems in Western Europe, 2nd ed.; Edward Elgar Publishing: Cheltenham, UK, 2011; pp. 185–215. [Google Scholar]
- De Montchalin, A. Plan Santé au Travail Dans la Fonction Publique. Available online: https://www.fonction-publique.gouv.fr/files/files/publications/hors_collections/Plan_Sante_Travail_FP_2022_2025.pdf (accessed on 6 October 2022).
- Sharma, A.; Minh Duc, N.T.; Luu Lam Thang, T.; Nam, N.H.; Ng, S.J.; Abbas, K.S.; Huy, N.T.; Marušić, A.; Paul, C.L.; Kwok, J.; et al. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J. Gen. Intern. Med. 2021, 36, 3179–3187. [Google Scholar] [CrossRef] [PubMed]
- Loi N°47-649 du 9 Avril 1947 Dite Morice Portant Ratification du Decret 462971 du 31-12-1946 Relatif a L’institution du Regime de Securite Sociale des Fonctionnaires Sous Reserve de L’art. 2 Dudit Decret Qui se Trouve Modifie-Légifrance. Available online: https://www.legifrance.gouv.fr/jorf/id/JORFTEXT000000865022 (accessed on 6 October 2022).
- Ameli, le Site de L’assurance Maladie en Ligne|Ameli.fr|Assuré. Available online: https://www.ameli.fr/ (accessed on 6 October 2022).
- Voidăzan, S.; Moldovan, G.; Voidăzan, L.; Zazgyva, A.; Moldovan, H. Knowledge, Attitudes and Practices Regardingthe Use of Antibiotics. Study on the General Population of Mureş County, Romania. Infect. Drug Resist. 2019, 12, 3385–3396. [Google Scholar] [CrossRef]
- Mazińska, B.; Strużycka, I.; Hryniewicz, W. Surveys of Public Knowledge and Attitudes with Regard to Antibiotics in Poland: Did the European Antibiotic Awareness Day Campaigns Change Attitudes? PLoS ONE 2017, 12, e0172146. [Google Scholar] [CrossRef]
- De Godoi Rezende Costa Molino, C.; Chocano-Bedoya, P.O.; Sadlon, A.; Theiler, R.; Orav, J.E.; Vellas, B.; Rizzoli, R.; Kressig, R.W.; Kanis, J.A.; Guyonnet, S.; et al. Prevalence of Polypharmacy in Community-Dwelling Older Adults from Seven Centres in Five European Countries: A Cross-Sectional Study of DO-HEALTH. BMJ Open 2022, 12, e051881. [Google Scholar] [CrossRef]
- Schönenberg, A.; Prell, T. Factors Influencing Self-Reported Medication Use in the Survey of Health Aging and Retirement in Europe (SHARE) Dataset. Healthcare 2021, 9, 1752. [Google Scholar] [CrossRef]
- Huang, C.-Y.; Yang, S.-Y.; Mojtabai, R.; Lin, S.-K.; He, Y.-L.; Chong, M.-Y.; Ungvari, G.; Tan, C.-H.; Xiang, Y.-T.; Sartorius, N.; et al. Trends of Polypharmacy and Prescription Patterns of Antidepressants in Asia. J. Clin. Psychopharmacol. 2018, 38, 598–603. [Google Scholar] [CrossRef]
- Sites, B.D.; Davis, M.; Herrick, M. Anxiolytic and Sedative Polypharmacy among US Opioid Users: A Cross-Sectional Study. Reg. Anesth. Pain Med. 2022, 47, 370–371. [Google Scholar] [CrossRef]
- Wang, L.-J.; Chen, Y.-C.; Chen, C.-K.; Chou, W.-J.; Chou, M.-C. Trends in Anxiolytic-Hypnotic Use and Polypharmacy in Taiwan, 2002–2009: A Nationwide, Population-Based Survey. Psychiatr. Serv. 2014, 65, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.T.; D’Angelo, S.; Harris, E.C.; Linaker, C.; Coggon, D. The Role of Mental Health Problems and Common Psychotropic Drug Treatments in Accidental Injury at Work: A Case-Control Study. Occup. Environ. Med. 2014, 71, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Geulayov, G.; Ferrey, A.; Casey, D.; Wells, C.; Fuller, A.; Bankhead, C.; Gunnell, D.; Clements, C.; Kapur, N.; Ness, J.; et al. Relative Toxicity of Benzodiazepines and Hypnotics Commonly Used for Self-Poisoning: An Epidemiological Study of Fatal Toxicity and Case Fatality. J. Psychopharmacol. 2018, 32, 654–662. [Google Scholar] [CrossRef]
- Waters, S. Suicide Voices: Testimonies of Trauma in the French Workplace. Med. Humanit. 2017, 43, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Bonde, J.P.E.; Munch-Hansen, T.; Wieclaw, J.; Westergaard-Nielsen, N.; Agerbo, E. Psychosocial Work Environment and Antidepressant Medication: A Prospective Cohort Study. BMC Public Health 2009, 9, 262. [Google Scholar] [CrossRef]
- Lavigne, E.; Bourbonnais, R. Psychosocial Work Environment, Interpersonal Violence at Work and Psychotropic Drug Use among Correctional Officers. Int. J. Law Psychiatry 2010, 33, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Thielen, K.; Nygaard, E.; Rugulies, R.; Diderichsen, F. Job Stress and the Use of Antidepressant Medicine: A 3.5-Year Follow-up Study among Danish Employees. Occup. Environ. Med. 2011, 68, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Madsen, I.E.H.; Diderichsen, F.; Burr, H.; Rugulies, R. Person-Related Work and Incident Use of Antidepressants: Relations and Mediating Factors from the Danish Work Environment Cohort Study. Scand. J. Work Environ. Health 2010, 36, 435–444. [Google Scholar] [CrossRef]
- Madsen, I.E.H.; Hanson, L.L.M.; Rugulies, R.; Theorell, T.; Burr, H.; Diderichsen, F.; Westerlund, H. Does Good Leadership Buffer Effects of High Emotional Demands at Work on Risk of Antidepressant Treatment? A Prospective Study from Two Nordic Countries. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 1209–1218. [Google Scholar] [CrossRef]
- Lassalle, M.; Chastang, J.-F.; Niedhammer, I. Working Conditions and Psychotropic Drug Use: Cross-Sectional and Prospective Results from the French National SIP Study. J. Psychiatr. Res. 2015, 63, 50–57. [Google Scholar] [CrossRef]
- Alonso, J.; Angermeyer, M.C.; Bernert, S.; Bruffaerts, R.; Brugha, T.S.; Bryson, H.; de Girolamo, G.; Graaf, R.; Demyttenaere, K.; Gasquet, I.; et al. Psychotropic Drug Utilization in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) Project. Acta Psychiatr. Scand. 2004, 109, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Midão, L.; Giardini, A.; Menditto, E.; Kardas, P.; Costa, E. Polypharmacy Prevalence among Older Adults Based on the Survey of Health, Ageing and Retirement in Europe. Arch. Gerontol. Geriatr. 2018, 78, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.S.; Kochar, B.D.; Kennelty, K.; Ernst, M.E.; Chan, A.T. Emerging Approaches to Polypharmacy among Older Adults. Nat. Aging 2021, 1, 347–356. [Google Scholar] [CrossRef]
- Mangin, D.; Bahat, G.; Golomb, B.A.; Mallery, L.H.; Moorhouse, P.; Onder, G.; Petrovic, M.; Garfinkel, D. International Group for Reducing Inappropriate Medication Use & Polypharmacy (IGRIMUP): Position Statement and 10 Recommendations for Action. Drugs Aging 2018, 35, 575–587. [Google Scholar] [CrossRef] [PubMed]
- Rozsnyai, Z.; Jungo, K.T.; Reeve, E.; Poortvliet, R.K.E.; Rodondi, N.; Gussekloo, J.; Streit, S. What Do Older Adults with Multimorbidity and Polypharmacy Think about Deprescribing? The LESS Study-a Primary Care-Based Survey. BMC Geriatr. 2020, 20, 435. [Google Scholar] [CrossRef]
- Vanhaesebrouck, A.; Vuillermoz, C.; Robert, S.; Parizot, I.; Chauvin, P. Who Self-Medicates? Results from Structural Equation Modeling in the Greater Paris Area, France. PLoS ONE 2018, 13, e0208632. [Google Scholar] [CrossRef] [PubMed]
- European Commission, Directorate General for Health and Food Safety. TNS Political & Social. In Antimicrobial Resistance: Summary; Directorate General for Health and Food Safety: Brussels, Belgium, 2016. [Google Scholar]
- Guo, H.; Hildon, Z.J.-L.; Lye, D.C.B.; Straughan, P.T.; Chow, A. The Associations between Poor Antibiotic and Antimicrobial Resistance Knowledge and Inappropriate Antibiotic Use in the General Population Are Modified by Age. Antibiotics 2021, 11, 47. [Google Scholar] [CrossRef] [PubMed]
- McNulty, C.A.M.; Boyle, P.; Nichols, T.; Clappison, D.P.; Davey, P. Antimicrobial Drugs in the Home, United Kingdom. Emerg. Infect. Dis. 2006, 12, 1523–1526. [Google Scholar] [CrossRef] [PubMed]
- Mathew, P.; Sivaraman, S.; Chandy, S. Communication Strategies for Improving Public Awareness on Appropriate Antibiotic Use: Bridging a Vital Gap for Action on Antibiotic Resistance. J. Fam. Med. Prim. Care 2019, 8, 1867–1871. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2015; ISBN 978-92-4-150976-3. [Google Scholar]
- Uchil, R.R.; Kohli, G.S.; Katekhaye, V.M.; Swami, O.C. Strategies to Combat Antimicrobial Resistance. J. Clin. Diagn. Res. 2014, 8, ME01. [Google Scholar] [CrossRef]
- Ventola, C.L. The Antibiotic Resistance Crisis: Part 2: Management Strategies and New Agents. Pharm. Ther. 2015, 40, 344–352. [Google Scholar]
- Micoli, F.; Bagnoli, F.; Rappuoli, R.; Serruto, D. The Role of Vaccines in Combatting Antimicrobial Resistance. Nat. Rev. Microbiol. 2021, 19, 287–302. [Google Scholar] [CrossRef] [PubMed]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to Participate in a COVID-19 Vaccine Clinical Trial and to Get Vaccinated against COVID-19 in France during the Pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef]
- Bendau, A.; Plag, J.; Petzold, M.B.; Ströhle, A. COVID-19 Vaccine Hesitancy and Related Fears and Anxiety. Int. Immunopharmacol. 2021, 97, 107724. [Google Scholar] [CrossRef] [PubMed]
- Paakkari, L.; Okan, O. COVID-19: Health Literacy Is an Underestimated Problem. Lancet Public Health 2020, 5, e249–e250. [Google Scholar] [CrossRef]
- Montagni, I.; Ouazzani-Touhami, K.; Mebarki, A.; Texier, N.; Schück, S.; Tzourio, C.; CONFINS group. Acceptance of a COVID-19 Vaccine Is Associated with Ability to Detect Fake News and Health Literacy. J. Public Health 2021, 43, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Fincham, J.E. Response Rates and Responsiveness for Surveys, Standards, and the Journal. Am. J. Pharm. Educ. 2008, 72, 43. [Google Scholar] [CrossRef] [PubMed]



| Variable | All (N = 21,723) | Workers (N = 11,014) | Retired (N = 10,709) | p-Value |
|---|---|---|---|---|
| Gender | <0.0001 | |||
| male | 8938 (41.1) | 3887 (35.3) | 5051 (47.2) | |
| female | 12,785 (58.9) | 7127 (64.7) | 5658 (52.8) | |
| Age range | <0.0001 | |||
| 18–29 years | 240 (1.1) | 240 (2.2) | 0 (0.0) | |
| 30–39 years | 1483 (6.8) | 1481 (13.4) | 2 (0.0) | |
| 40–49 years | 3475 (16.0) | 3470 (31.5) | 5 (0.0) | |
| 50–59 years | 5008 (23.1) | 4620 (41.9) | 388 (3.6) | |
| 60–69 years | 7309 (33.6) | 1185 (10.8) | 6124 (57.2) | |
| 70–79 years | 3681 (16.9) | 11 (0.1) | 3670 (34.3) | |
| ≥80 years | 527 (2.4) | 7 (0.1) | 520 (4.9) | |
| Marital status | <0.0001 | |||
| Single | 2592 (11.9) | 1935 (17.6) | 657 (6.1) | |
| Divorced | 2457 (11.3) | 1249 (11.3) | 1208 (11.3) | |
| Married | 12,794 (58.9) | 5399 (49.0) | 7395 (69.1) | |
| Civil union | 1240 (5.7) | 1096 (10.0) | 144 (1.3) | |
| Common-law | 1524 (7.0) | 1162 (10.6) | 362 (3.4) | |
| Widowed | 1116 (5.1) | 173 (1.6) | 943 (8.8) | |
| Children living in the household | <0.0001 | |||
| 0 | 16,375 (75.4) | 6050 (54.9) | 10,325 (96.4) | |
| >1 | 5348 (24.6) | 4964 (45.1) | 384 (3.6) | |
| Level of study | <0.0001 | |||
| Below “Baccalaureate” degree | 7114 (32.7) | 2224 (20.2) | 4890 (45.7) | |
| Greater than or equal to “Baccalaureate” degree and less than or equal to “Baccalaureate” degree plus 2 years | 8763 (40.3) | 5049 (45.8) | 3714 (34.7) | |
| Higher than “Baccalaureate” degree plus 2 years | 5846 (26.9) | 3741 (34.0) | 2105 (19.7) | |
| Chronic disease or disability or health problem | <0.0001 | |||
| Yes | 6734 (31.0) | 2942 (26.7) | 3792 (35.4) | |
| No | 14,989 (69.0) | 8072 (73.3) | 6917 (64.8) | |
| Type of chronic disease or disability or health problem 1 | ||||
| Respiratory problems | 1301 (6.0) | 591 (8.8) | 710 (10.5) | |
| Heart, artery, vein or stroke disease | 1825 (8.4) | 475 (7.1) | 1350 (20.0) | |
| Metabolic disease | 2178 (10.0) | 830 (12.3) | 1348 (20.0) | |
| Tumors | 869 (4.0) | 294 (4.4) | 575 (8.5) | |
| Mental illness | 350 (1.6) | 238 (3.5) | 112 (1.7) | |
| Locomotor problems | 1552 (7.1) | 667 (9.9) | 885 (13.1) | |
| Other | 2194 (10.1) | 1113 (16.5) | 1081 (16.1) |
| Variable | All (N = 21,723) | Workers (N = 11,014) | Retired (N = 10,709) | p-Value |
|---|---|---|---|---|
| ANTIBIOTICS | ||||
| Knowledge a | <0.0001 | |||
| Low | 3475 (16.0) | 1451 (13.2) | 2024 (18.9) | |
| Moderate | 12,874 (59.3) | 6107 (55.4) | 6767 (63.2) | |
| High | 5374 (24.7) | 3456 (31.4) | 1918 (17.9) | |
| Antibiotics ineffective against viruses | 15,521 (71.5) | 8143 (73.9) | 7378 (68.9) | |
| Antibiotics effective against bacteria | 16,116 (74.2) | 8531 (77.5) | 7585 (70.8) | |
| Taking antibiotics often can make them less effective | 19,849 (91.4) | 10,231 (92.90) | 9618 (89.8) | |
| Antibiotics, in general, don’t make it possible to heal more quickly | 7842 (36.1) | 4766 (43.3) | 3076 (28.70) | |
| Antibiotics misuse | <0.0001 | |||
| Yes | 6083 (28.0) | 3659 (33.2) | 2424 (22.6) | |
| No | 15640 (72.0) | 7355 (66.8) | 8285 (77.4) | |
| Self-interruption of the antibiotics prescription duration | 2628 (12.1) | 1601 (14.5) | 1027 (9.6) | |
| Take non-prescribed antibiotics for himself or for his children or for his relatives | 4555 (21.0) | 2809 (25.5) | 1746 (16.3) | |
| MEDICATION | ||||
| Anxiolytic intake in the last few months | <0.0001 | |||
| Yes | 4429 (20.4) | 2241 (20.3) | 2188 (20.4) | |
| No | 17,294 (79.6) | 8773 (79.7) | 8521 (79.6) | |
| Hypnotic intake in the last few months | <0.0001 | |||
| Yes | 4645 (21.4) | 2671 (24.3) | 1974 (18.4) | |
| No | 17,078 (78.6) | 8343 (75.7) | 8735 (81.6) | |
| Daily medication intake | <0.0001 | |||
| Yes (1 or more) | 13,572 (62.5) | 5400 (49.0) | 8172 (76.3) | |
| No | 8151 (37.5) | 5614 (51.0) | 2537 (23.7) | |
| Polymedication b | <0.0001 | |||
| Yes | 3574 (16.5) | 956 (8.7) | 2618 (24.4) | |
| No | 18,149 (83.5) | 10,058 (91.3) | 8091 (75.6) | |
| Proactive behavior c | <0.0001 | |||
| Yes | 18,191 (83.7) | 9450 (85.8) | 8741 (81.6) | |
| No | 3532 (16.3) | 1564 (14.2) | 1968 (18.4) | |
| Self-evaluation of its antibiotic needs and active request for it | 16,242 (74.8) | 8703 (79.0) | 7539 (70.4) | |
| If medication intake, has already discussed it with physician/pharmacist on own initiative | 4934 (22.7) | 1712 (15.5) | 3222 (30.1) | |
| If medication intake for sleep disorder, has already tried non-medication methods | 2803 (12.9) | 1511 (13.7) | 1292 (12.1) | |
| If medication intake for anxiety, has already tried non-medication methods | 3077 (14.2) | 1859 (16.9) | 1218 (11.4) | |
| VACCINATION | ||||
| Knowledge | <0.0001 | |||
| Low | 3388 (15.6) | 1537 (14.0) | 1851 (17.3) | |
| Moderate | 11,228 (51.7) | 5759 (52.3) | 5469 (51.1) | |
| High | 7107 (32.7) | 3718 (33.8) | 3389 (31.6) | |
| Useful to be vaccinated even against a disease that has disappeared | 15,976 (73.5) | 8696 (79.0) | 7280 (68.0) | |
| Vaccination is better to develop its own immune defenses than to have the disease | 15,342 (70.6) | 7883 (71.6) | 7459 (69.7) | |
| Vaccines are effective and useful | 19,175 (88.3) | 9680 (87.9) | 9495 (88.7) | |
| Vaccines don’t cause serious side effects | 9770 (45.0) | 4872 (44.2) | 4898 (45.7) | |
| Vaccinophobia | <0.0001 | |||
| Yes | 279 (1.3) | 93 (0.8) | 186 (1.7) | |
| No | 21,444 (98.7) | 10,921 (99.2) | 10,523 (98.3) | |
| Not up to date with vaccinations | 2798 (12.9) | 1155 (10.5) | 1643 (15.3) | |
| Not search for information about vaccine schedule, and/or composition of vaccines and/or current state of scientific knowledge about vaccines and/or recommended vaccines for foreign travel | 15,928 (73.3) | 7891 (71.6) | 8307 (75.0) | |
| No intention to get vaccinated even if it is possible at the workplace and/or in a pharmacy | 7024 (32.3) | 3239 (29.4) | 3785 (35.3) | |
| No intention to be vaccinated even if the cost is reduced and/or if the vaccine is free | 8865 (40.8) | 4305 (39.1) | 4560 (42.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lvovschi, V.-E.; Carrouel, F.; du Sartz de Vigneulles, B.; Lamure, M.; Motyka, G.; Fraticelli, L.; Dussart, C. Knowledge, Attitudes and Practices Related to Medication, Antibiotics, and Vaccination among Public Service Population: National Survey Conducted in France. Int. J. Environ. Res. Public Health 2022, 19, 14044. https://doi.org/10.3390/ijerph192114044
Lvovschi V-E, Carrouel F, du Sartz de Vigneulles B, Lamure M, Motyka G, Fraticelli L, Dussart C. Knowledge, Attitudes and Practices Related to Medication, Antibiotics, and Vaccination among Public Service Population: National Survey Conducted in France. International Journal of Environmental Research and Public Health. 2022; 19(21):14044. https://doi.org/10.3390/ijerph192114044
Chicago/Turabian StyleLvovschi, Virginie-Eve, Florence Carrouel, Benjamin du Sartz de Vigneulles, Michel Lamure, Geneviève Motyka, Laurie Fraticelli, and Claude Dussart. 2022. "Knowledge, Attitudes and Practices Related to Medication, Antibiotics, and Vaccination among Public Service Population: National Survey Conducted in France" International Journal of Environmental Research and Public Health 19, no. 21: 14044. https://doi.org/10.3390/ijerph192114044
APA StyleLvovschi, V.-E., Carrouel, F., du Sartz de Vigneulles, B., Lamure, M., Motyka, G., Fraticelli, L., & Dussart, C. (2022). Knowledge, Attitudes and Practices Related to Medication, Antibiotics, and Vaccination among Public Service Population: National Survey Conducted in France. International Journal of Environmental Research and Public Health, 19(21), 14044. https://doi.org/10.3390/ijerph192114044








