Abstract
Background: Over the years, forensic pathology has registered the spread of new methods of suicide, such as the ingestion of sodium nitrite. Sodium nitrite causes increased methemoglobin, resulting in systemic hypoxia, metabolic acidosis, and cyanosis. Since sodium nitrite is a preservative, the ingestion of foods containing an excessive amount of this substance can also cause acute intoxication up to death. The present review is aimed at guiding health professionals in the identification and management of sodium-nitrite-related intoxications and deaths. Methods: A systematic literature search was carried out on PubMed by following the PRISMA statement’s criteria. A total of 35 studies with 132 cases were enrolled, and the data were cataloged in Microsoft Excel. To establish the causal correlation between sodium nitrite ingestion and death, the Naranjo Adverse Drug Reaction Probability Scale was used. Results: In addition to the small number of cases that have currently been published, the study demonstrated that there was a general methodological discrepancy in the diagnostic process. However, some interesting results have emerged, especially in post-mortem diagnostics. Conclusion: Sodium-nitrite-related deaths represent a challenge for forensic pathologists; therefore, it is important to promptly recognize the essential features and perform the necessary and unrepeatable examinations for the correct diagnosis of the cause of death.
1. Introduction
Nowadays, suicide continues to represent a burden that affects the entire world population. According to the World Health Organization (WHO), suicide-related deaths are estimated to be around 703,000 annually, and 58% involve people under 50; moreover, the data show that 77% of suicide cases are recorded in low- and middle-income countries [1]. Data published by the Centers for Disease Control and Prevention (CDC) in 2022, which were in relation to the US population for the twenty years from 2000 to 2020, showed that the suicide rate increased by 30%, with a peak that was reached in 2018 and with a 3–4 times higher rate in males [2]. In fact, individuals of the male and female genders have different approaches to this practice; specifically, men are more frequently involved in effective suicidal events, contrary to women, who more frequently only attempt suicide. Furthermore, one difference consists in the propensity of males to choose methodologies that are characterized by greater lethality and violence [3]; hanging represents the most frequent method used by men, while drug abuse is the method used most frequently by women [4,5]. There are conflicting data when considering different countries. For example, in countries where the possession of weapons is widespread, such as the USA, the main method of suicide in men is by firearms [6]. Acute intoxication with exogenous substances can occur through the adoption of different modalities, such as, primarily, ingestion, inhalation, and poisoning by chemical substances, including pesticides [7]. The advent of the internet, as well as the evolution of society and life habits, has determined a heterogenization of suicide methods over the years. The particular cases previously reported in the literature are progressively increasing, thus allowing one to highlight how new methods of suicide suddenly spread.
Among these, the acute ingestion of sodium nitrite is becoming increasingly important. Sodium nitrite is an inorganic compound that, at environmental temperature, has a crystalline, odorless, yellowish-white, water-soluble, and hygroscopic appearance. This compound is characterized by its easy availability and has found applications in several fields. It is widely prescribed in medicine, where it is mainly administered as an antidote to cyanide poisoning [8], while, in the food industry, it is used as a preservative (labeled with the code “E250”) in meat products to inhibit bacterial growth and prevent deterioration, as well as to improve organoleptic characteristics (appearance, color, and taste) through a reaction with myoglobin [9]. Given its dose-dependent toxicity, over the years, international governmental bodies have regulated the use of this preservative to protect public health and food safety [10,11,12]. Despite this, the same restrictions have not been applied in the context of trade. Still today, this substance is easily available, even online. Its easy availability and affordable cost have allowed its progressive and sudden spread as a means of suicide, even among young people of both genders.
Sodium nitrite results in an increase in the concentration of methemoglobin (MHb), which normally constitutes only 1–2% of the total circulating hemoglobin. Hemoglobin is a tetrameric metalloprotein with four subunits, each of which is bound to a heme group capable of binding an Fe2+/Fe3+ ion. Normally, heme binds ferrous iron (Fe2+), which is capable of transporting the oxygen molecule so that it can be released into the tissue. Sometimes, such as through the action of sodium nitrite, ferrous iron is oxidized to ferric iron (Fe3+), thus losing its ability to bind oxygen and resulting in a greater affinity for oxygen in the remaining Fe2+ heme groups that are present in the same hemoglobin structure. Thus, hemoglobin is transformed into MHb, which has a lower capacity to transport oxygen and release it into the tissue [13]. In fact, the allosteric modifications of MHb, in addition to allowing bonds with a smaller number of oxygen molecules, result in the establishment of a stronger bond, which is the reason for the difficulty of the release of the oxygen into the tissue; therefore, clinically, the percentage of residual oxyhemoglobin constitutes only the theoretical oxygen transport capacity, as the effective peripheral release capacity must be considered. The reduction in aerobic cellular metabolism resulting from systemic hypoxia due to MHb results in heterogeneous conditions that range from metabolic acidosis to cyanosis and death [14].
The present systematic review, which was conducted according to the PRISMA 2020 guidelines, aspires to frame the main features of deaths due to sodium nitrite intake; specifically, this research aims to summarize the current evidence derived from the small number of cases reported in the literature. As a secondary objective, this study focuses on post-mortem assessments to provide support to healthcare professionals who are involved in the investigation of sodium-nitrite-related deaths.
2. Materials and Methods
2.1. Search Strategy and Study Selection
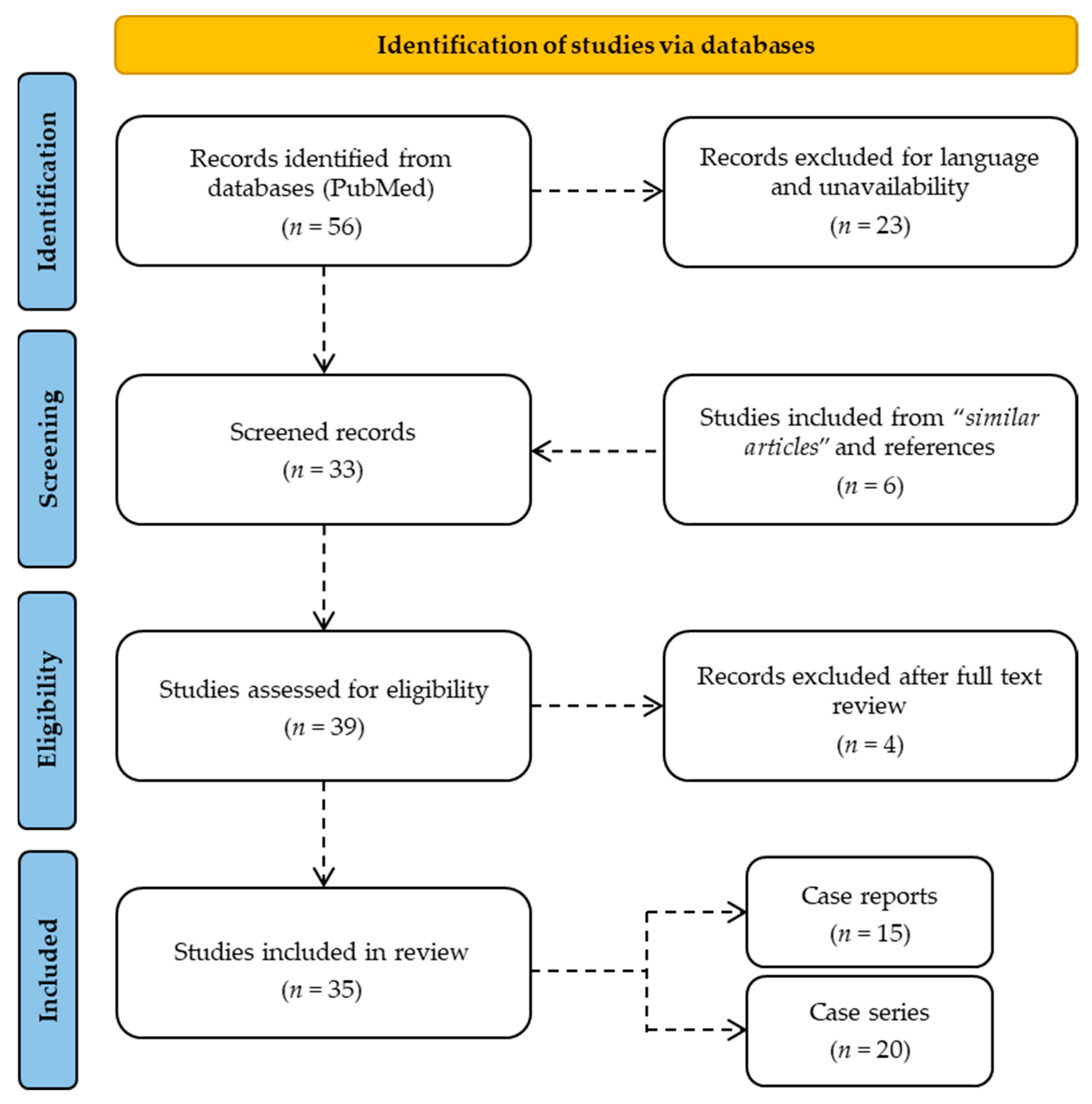
The present review involved a systematic literature search carried out up to 21 June, 2022 on PubMed while following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement’s criteria [15,16], without time limits (Figure 1). In order to broaden the number of studies included in the search, MeSH terms, Boolean operators, and free-text terms were used to carry out the review. Articles focusing on the effects of sodium nitrite ingestion were initially searched using the terms “sodium nitrite AND ((intoxication) OR (death) OR (suicide) OR (ingestion))” in the title, abstract, and keywords. The study design included case reports and case series. No unpublished or gray literature was consulted. A total of 56 studies relevant to the present review were identified on PubMed; of these, 12 were excluded due to unavailability and 11 were excluded because they were not in English. The analysis of the references during the full-text reading allowed the inclusion of a further 6 studies. After evaluating the abstracts and the full texts, 4 articles were excluded because they were not relevant to the research topic. Therefore, the present review involved the inclusion of a total of 35 studies, which were divided into 15 case reports and 20 case series. The data in each included study were extracted by using Microsoft Excel spreadsheets; these data included information on the authors, journal, year of publication, country, sample size, gender, age, comorbidities, method of assumption, intentionality, any other substances taken, symptoms and times of manifestation, hospitalization, mortality, scene investigations, post-mortem assessments, and diagnosis of death.
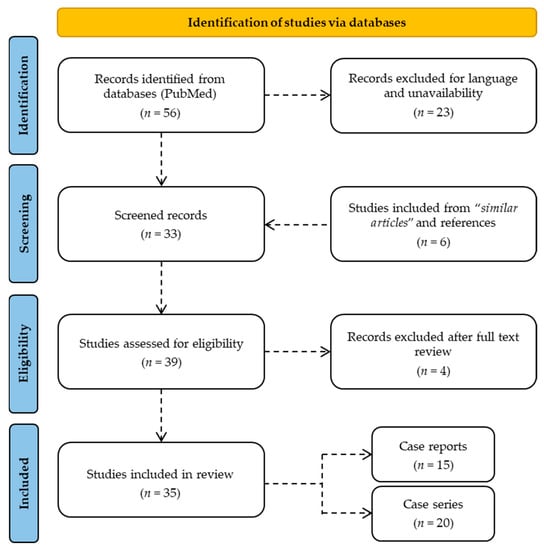
Figure 1.
Flow diagram of the design of the study in accordance with the PRISMA 2020 guidelines.
2.2. Causality Assessment
This study considered a causality assessment by applying the Naranjo Adverse Drug Reaction Probability Scale [17] to validate the evidence provided by the review. This scoring algorithm, which is used in the context of pharmacovigilance, was applied to attribute to sodium nitrite a scientifically objective causal correlation with intoxication and death. The scale consists of 10 questions with 3 possible answers, each of which is assigned a score that allows the attribution of the probability of such a causal correlation in each case. The scores are between −4 and +12, and they permit the following division of adverse drug reactions based on the probability of their existence:
- −
- definite (score ≥ 9);
- −
- probable (score between 5 and 8);
- −
- possible (score between 2 and 4);
- −
- doubtful (score < 2).
3. Results
3.1. General Features
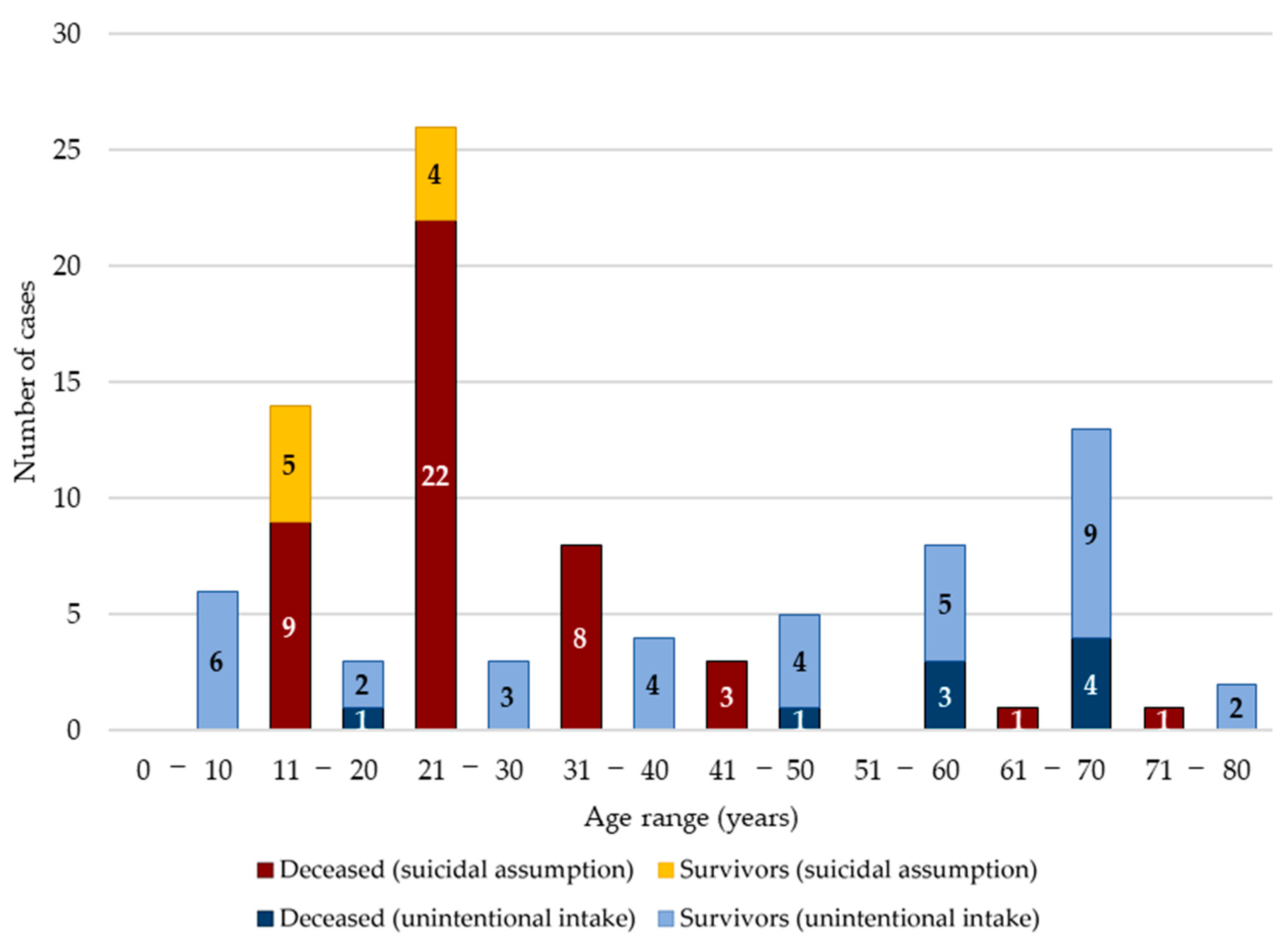
The present systematic review included a total of 35 papers, divided into 15 case reports and 20 case series (Table 1); 11 studies were carried out in America, as well as 11 in Asia, nine in Europe, three in Australia, and one in Africa. Overall, a total of 132 subjects were included (75 males, 34 females, and 23 of undefined gender); ages were available for 97 cases and ranged from 2 to 76 years, with an average of 35.6 years (Figure 2). In 53 of the 132 cases, the ingestion of sodium nitrite occurred for suicidal purposes, while in the remaining 79 cases, it occurred accidentally. A total of 21 of the 53 suicides were hospitalized, but 12 of these died anyway. However, 73 of the 79 individuals with accidental ingestions accessed the emergency room, and of these, only six died during hospitalization.

Table 1.
Main features of the included studies.
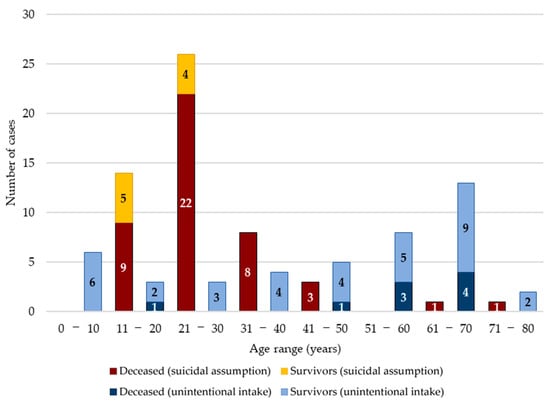
Figure 2.
Stratifications by age range; there is a subdivision between suicidal and unintentional intake of sodium nitrite, as well as the respective mortality and survival.
3.2. Medical History
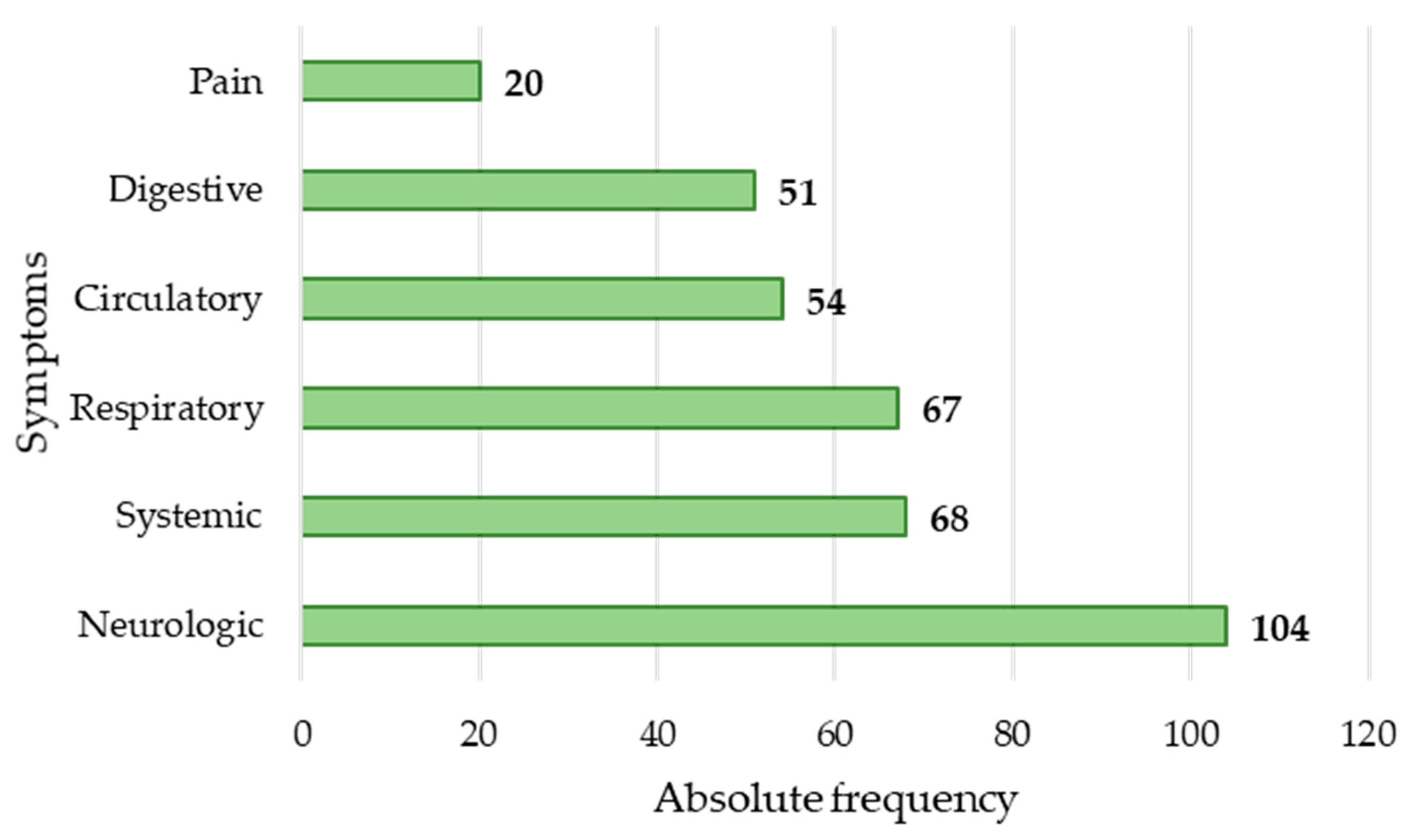
In 95 cases, it was possible to collect information relating to the symptoms (Figure 3). The symptoms that were most commonly presented were cyanosis of the face and/or extremities (64; 48.49%), breathing abnormalities (64; 48.49%), altered level of consciousness (57; 43.18%), dizziness (30; 22.73%), vomiting (28; 21.21%), nausea (22; 16.67%), pain (headache: 18, 13.64%; abdominal pain: 1, 0.76%, and chest pain: 1, 0.76%), and tachycardia (19; 14.39%).
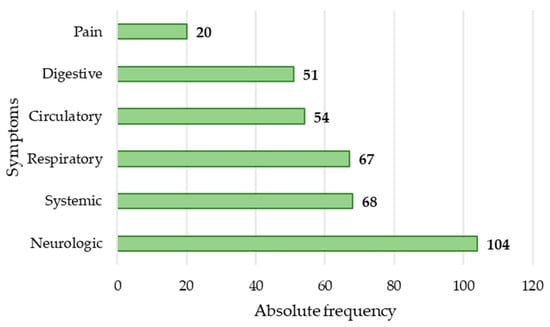
Figure 3.
Absolute frequency of symptoms.
A psychiatric anamnesis was collected in only 10 cases of ingestion for suicidal purposes. The psychiatric histories included depression (7; 70%), previous suicide attempts (6; 60%), bipolar disorder (2; 20%), schizophrenia (1; 10%), paranoia (1; 10%), previous self-harm attempts (1; 10%), and post-traumatic stress disorder (1; 10%).
3.3. Post-Mortem Investigations
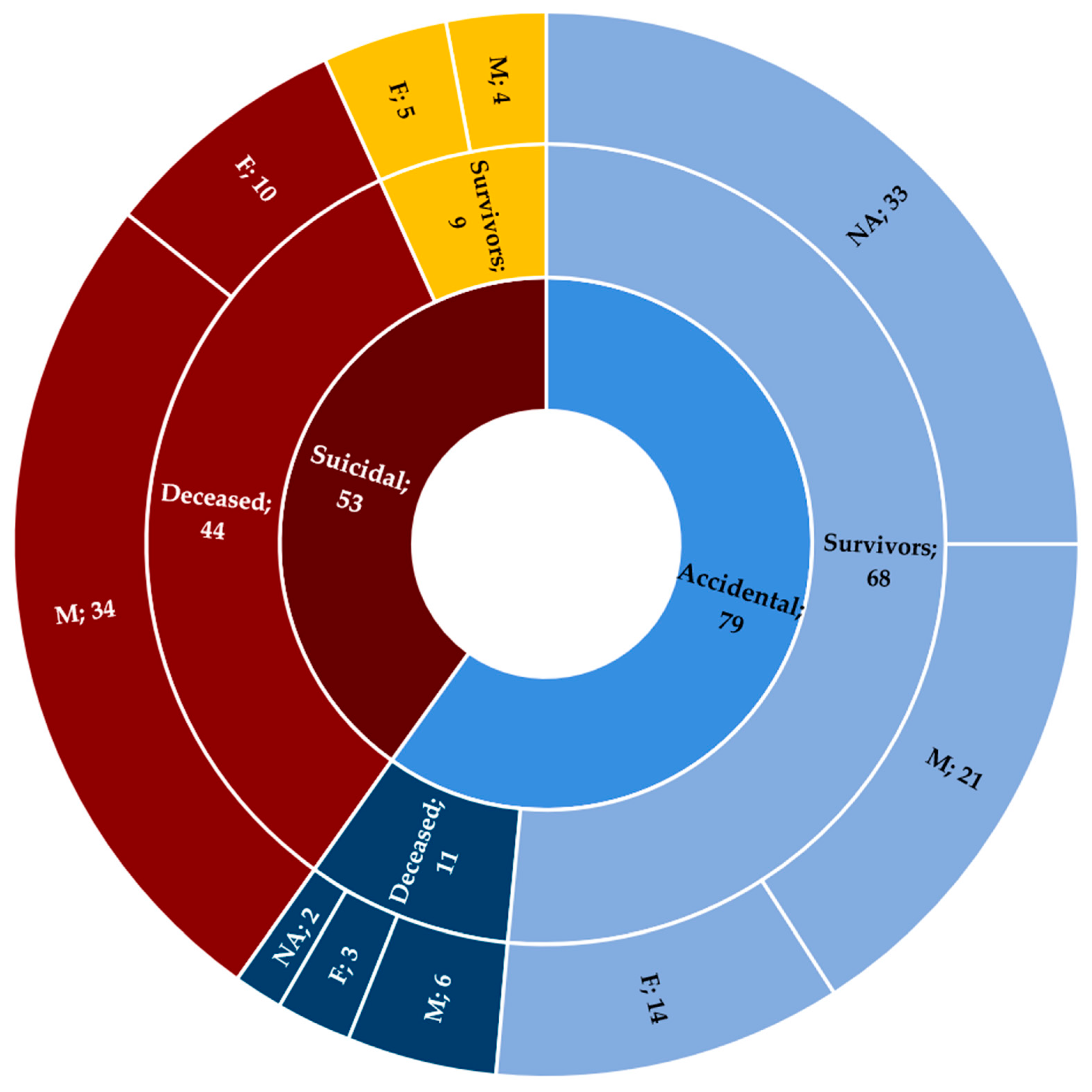
Out of the total number of cases, death occurred in 55 of the subjects (41.67%) (Table 2); specifically, it occurred in the cases of 40 males (72.73%), 13 females (23.64%), and two subjects without information about their gender (3.63%) (Figure 4). Concerning the reason for the consumption, in 44 cases (80%), suicidal intent was found, while in 11 cases (20%), the event was accidental. Of the 55 cases, the majority (37; 67.27%) were found dead and, therefore, not hospitalized.

Table 2.
Main characteristics of the deaths stratified by the age of the subjects.
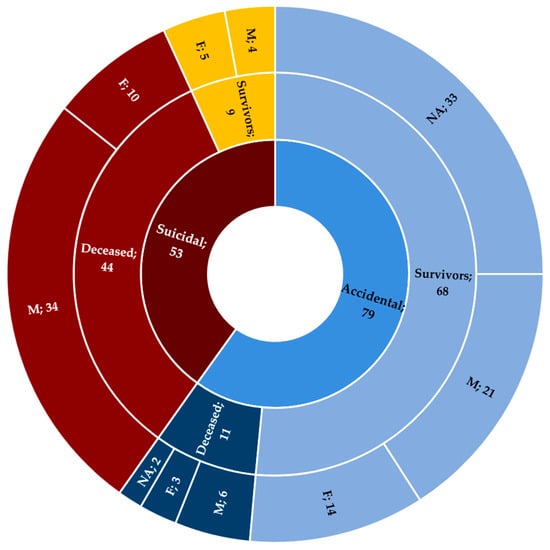
Figure 4.
Stratification of cases in relation to intentionality and accidentality. NA: not available; M: male; F: female.
In 24 cases, an investigation of the scene made it possible to identify particular objects near the body or in adjacent rooms. Specifically, the presence of at least one open container containing crystalline, odorless, and yellowish-white-colored powder, possibly bearing the label “Sodium nitrite”, was identified; usually, spoons, bottles, and glasses soiled with a whitish substance were also present. Sometimes, suicide notes and other medications were found.
In 39 cases, a post-mortem examination was performed. On external inspection, lividity varied in color from bluish red to mottled purple–gray; intense cyanosis of the face and extremities (up to gunmetal gray) was also highlighted. The autopsy revealed the presence of extremely thin and chocolate-colored blood and brown-colored organs—mainly the heart, kidneys, and liver—as well as whitish and paste-like residues in the gastric lumen; sometimes, these findings were associated with pulmonary and cerebral edema.
Microscopic examinations were carried out in only five cases. Histopathology revealed alterations related to comorbidities (myocardial fibrosis, coronary artery disease), signs of hypoxia (early myocardial ischemia), and non-specific findings (pulmonary edema).
Regarding post-mortem toxicology, methemoglobin (MHb) was studied in the blood, gastric content, and cerebrospinal and pericardial fluid (Table 3). The investigation of blood samples allowed the detection of concentrations between 9.87% and 83.4% in 26 cases; it must be specified that in 3 of the 26 cases, the investigations gave a positive result, in another three cases, the value exceeded the laboratory’s upper limit of detection, and in two cases, the results were not available. In 1 of the 26 cases, the dosage was studied in both a blood sample taken during the cadaveric inspection (MHb: 33%) and in two samples carried out during the autopsy (one of heart blood and one of peripheral blood; MHb: 26%); the results of tests in gastric content and cerebrospinal and pericardial fluid were not available.

Table 3.
Summary of the post-mortem toxicology results.
A search for nitrite was conducted in the blood, vitreous humor, gastric and bowel content, urine, cerebrospinal and pericardial fluid, liver, kidney, and costal cartilage. Blood samples taken during the autopsy were tested in 16 cases; in detail, the concentrations in heart blood ranged from 1.3 to 170 mg/L, while in peripheral blood, they varied from 1.1 to 298 mg/L; in two cases, the combined investigations in heart and peripheral blood samples gave negative results, but the correlation between death and sodium nitrite was, however, confirmed by other evidence. Vitreous humor was tested in one case (57.7 mg/L), gastric content in 15 cases (range: 6.8–16,000 mg/L), and urine in one case (24.6 mg/L); in one case, the investigation of nitrite was performed in cerebrospinal fluid (negative) and pericardial fluid (181 mg/L). An investigation of nitrite was also carried out in one case on a liver and kidney mixture (0.003 mg/kg); in one case, the liver (0.3 mg/kg), kidney (3.6 mg/kg), and costal cartilage (3.4 mg/kg) were tested; in one case, the dosage of nitrite in bowel content was assessed (4.2 mg/L).
In one case, sodium nitrite was assessed in blood with a positive result. Gastric content was also tested for sodium nitrite in seven cases; in two cases, the concentrations were equal to 13,000 and 24,000 mg/L, in four cases, the test was positive, and in one case, it was negative.
The search for nitrate was performed on blood and on gastric and bowel content, as well as cerebrospinal and pericardial fluid. In 13 cases, autopsy samples of heart blood (range: 71.69–524.8 mg/L) and peripheral blood (range: 83.48–476.4 mg/L) were tested; in one case, a peripheral blood sample taken during the cadaveric inspection was examined, and it had a value of 220.6 mg/L. Nitrate was also detected in gastric content in two cases (5.0 mg/L, 137.8 mg/L), in bowel content in one case (0.8 mg/L), and in cerebrospinal fluid (50.5 mg/L) and pericardial fluid (91.7 mg/L) in one case.
Sodium (148 mmol/L) and chloride (124 mmol/L) were examined in vitreous humor in one case.
Substances of abuse and/or drugs were investigated in blood and urine in 25 cases; the tests were positive in 13 cases and negative in nine cases; the results were not available in three cases.
3.4. Causality Assessment
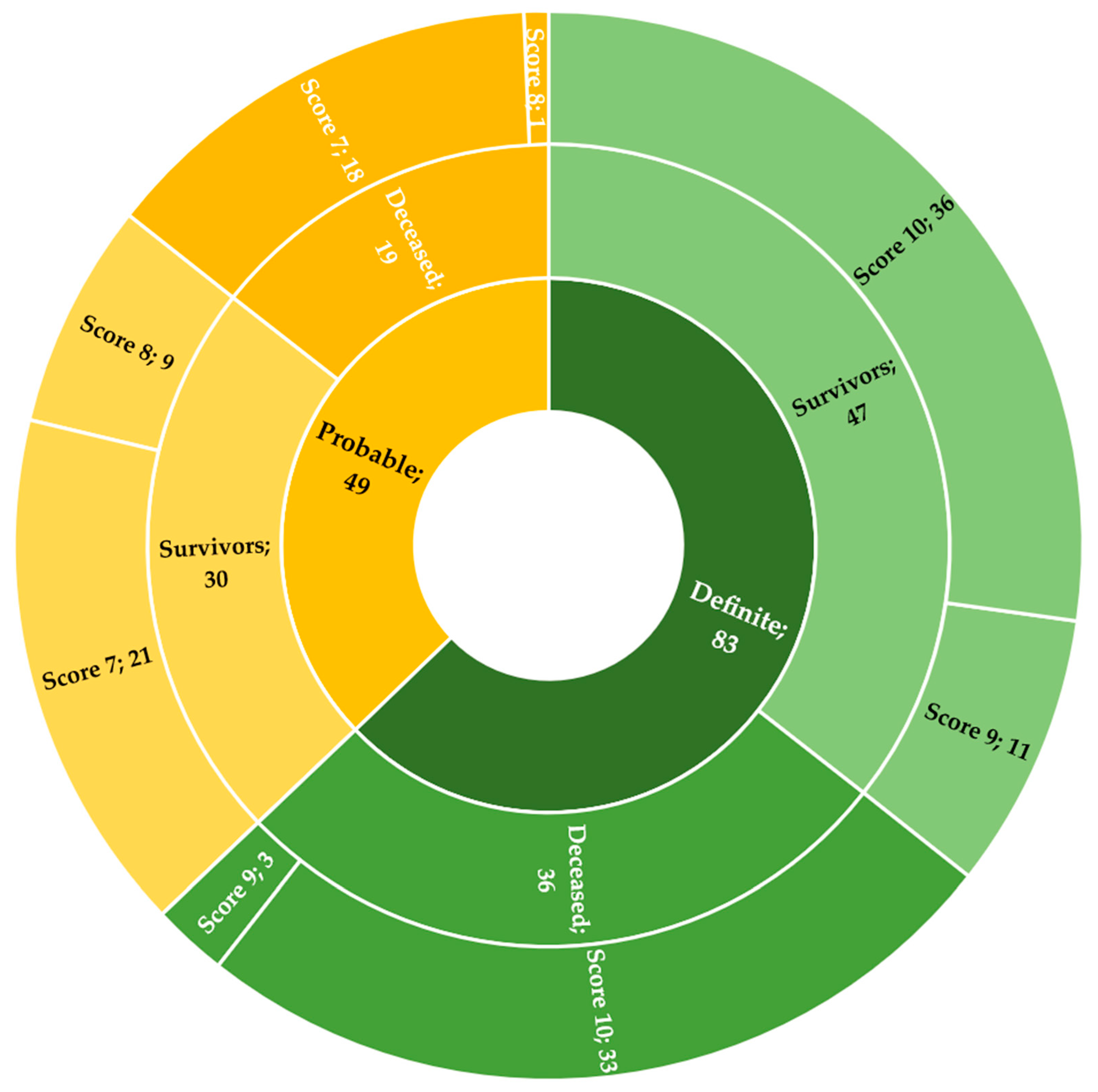
The attribution of a numerical value according to the Naranjo Adverse Drug Reaction Probability Scale made it possible to detect a score of 10 in 69 cases (36 survivors, 33 deceased), a score of 9 in 14 cases (11 survivors, 3 deceased), a score of 8 in 10 cases (9 survivors, 1 deceased), and a score of 7 in 39 cases (21 survivors, 18 deceased).
In consideration of the stratification of the categories and the scores obtained, the causal correlation between sodium nitrite ingestion and intoxication/death was definite in 83 cases (62.88%; 47 survivors, 36 deceased) and probable in 49 cases (37.12%; 30 survivors, 19 deceased) (Figure 5).
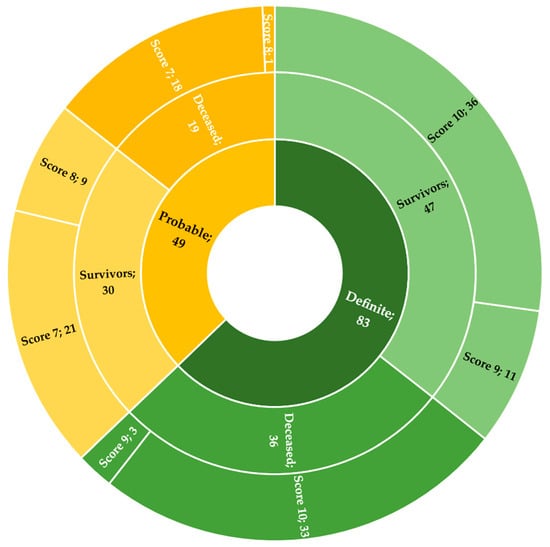
Figure 5.
Data on the application of the Naranjo Adverse Drug Reaction Probability Scale.
4. Discussion
The present systematic review aimed to analyze suicidal or unintentional ingestion of sodium nitrite; specifically, the features of the involved subjects (sex, age, and comorbidities), circumstantial data (manner of intake, intentionality, and other substances taken), symptoms, hospitalization, and post-mortem investigations (if any) were considered.
Particular attention was paid to the ingestion of sodium nitrite for suicidal purposes, a pervasive phenomenon that is afflicting public health worldwide. The prevention of the risk of suicide constitutes a challenge for suicidology, which tries daily to face ever-new anticonservative methodologies [53]. To prevent both suicidal behaviors and suicides, it is advisable to implement a multidisciplinary approach based on the involvement of different complementary professional figures in both the hospital and the territorial setting on the training of non-healthcare professionals. An aspect that is not to be underestimated is the involvement of the media, which should play an important role in suicide prevention campaigns in order to portray suicide as an act that should be avoided and not emulated, which is often, unfortunately, the case [54].
Nowadays, in parallel with societal change, the culture of suicide is also evolving in both its methods and its age groups. In fact, the increasing diffusion and the simplicity with which it is possible to access devices connected to the internet have allowed the spread of content to an ever-wider audience [55]. Currently, through dozens of social networks, it is possible to share one’s thoughts and contributions with the rest of the world, as well as, vice versa, to learn new knowledge from the latter. Sometimes, shared content is not characterized by social utility and legality. This is the case on many websites that list multiple methods of suicide and even try to induce mentally fragile subjects to partake in them [56]. Such free and often uncontrolled communication, which borders on illegality, causes extreme situations such as suicide to be ever closer and more realistically feasible. It is not rare to find cases in which ways to commit suicide are researched online [57,58]. From this perspective, information relating to the action and availability of substances such as sodium nitrite has been made known to the group of the population that uses the web the most—young people [59,60].
The evidence that arose from the 35 studies considered here permits the confirmation of this phenomenon; in fact, it emerged that 90.6% of the subjects who ingested sodium nitrite for suicidal purposes were aged between 15 and 39 years and, thus, belonged to the population that used the internet as a main source of information the most.
Given the spread of the phenomenon, it would be advisable, on the one hand, to implement tight checks of online content and, on the other hand, to tackle the health problem. More precisely, from the perspective of prevention and public health, it appears to be important to protect the categories that are at risk by limiting the diffusion of content alluding to the use of sodium nitrite for suicidal purposes.
Therefore, in hospitals, one important aspect is the training of health professionals—not necessarily psychiatrists—to quickly identify an acute intoxication and to implement the necessary treatments (intravenous methylene blue and life-support therapies) [61,62]. This concept is also supported by the data that emerged from the studies considered here. In fact, the results highlight how mortality is higher in non-hospitalized subjects due to the absence of adequate drug and life-support therapy.
Mortality was significantly higher in cases of voluntary intake than in cases of involuntary intake, which was certainly due to the greater quantities of sodium nitrite that were taken in the event of a suicide attempt. The intake of an excessive but non-lethal quantity of sodium nitrite guarantees a longer survival interval, with the possibility of accessing an emergency department and receiving the appropriate therapy [63]. Another aspect is linked to the condition of solitude in which suicidal acts are carried out. In fact, it is more frequent that the consumption of food containing an excessive quantity of sodium nitrite occurs in the presence of witnesses who are able to provide help and quickly transport the subject to the hospital.
The rapidity in causing death and the simple availability of sodium nitrite have allowed the increased diffusion of this substance as a means of suicide [64]. Therefore, to establish its role in provoking death, it is essential, firstly, to identify all cases, even if only suspicious, and, secondly, to carry out all of the necessary post-mortem investigations to make the correct diagnosis of death. According to the evidence obtained here, an important role in framing the cases is played by the investigation of the scene. An adequate observation of the environment in which the body was found allowed the identification of peculiar objects—specifically, the discovery of open plastic packages containing crystalline, odorless, and yellowish-white-colored powder, which possibly bore the label “Sodium Nitrite”, and spoons soiled with whitish material, as well as bottles and glasses with a deposit of the same substance on the bottom. Such items may be associated with a suicide note and other drugs. These characteristic findings should constitute the main elements to be sought in cases of suspected ingestion of sodium nitrite, or, in the absence of suspicion, should represent the main objects noticed during the investigation of a scene to direct further examinations. The centrality of the investigation of the scene needs to be affirmed considering the results. The currently available literature analyzed in the present study attested that an inspection was ordered in only 48.98% of cases. Such a frequency, although significant, precludes the possibility of immediately obtaining data that are capable of directing the diagnosis in many cases.
An autopsy must be accurate to highlight peculiarities [65] such as a change in hypostasis in the extremities and face, which can range from dark-bluish red to mottled purple–gray, which is associated with intense cyanosis, up to gunmetal gray, as well as fluid and chocolate-brown blood. In some cases, the organs—mainly the heart, kidneys, and liver—were also brown in color; drug residues were also detectable in the gastric content. Sometimes, these findings may be associated with non-specific signs that are frequent in deaths related to the intake of exogenous substances, such as pulmonary and cerebral edema. Although they were frequent in the cases observed, the external signs were not pathognomonic and were rarely able to condition the subsequent diagnostic approach. Nevertheless, caution and methodological rigor are recommended in the execution of an external examination in order to interpret the findings correctly and to plan the subsequent investigations fruitfully. Furthermore, autopsy is fundamental for the sampling of biological fluids and tissues in order to search for nitrite, nitrate (obtained from the reaction of nitrite with oxyhemoglobin in the blood) [66], and the methemoglobin (MHb) dosage.
The analysis of data regarding toxicology was very difficult due to the methodological discrepancies in the available studies. Despite the differences, the most commonly used matrices included blood (for the investigation of MHb, nitrite, and nitrate) and gastric content (for nitrite investigations). In a minority of cases, urine, cerebrospinal fluid, vitreous humor, pericardial fluid, and others (such as the liver, kidney, bowel content, and costal cartilage) were taken. Specifically, it emerged that the direct search for nitrites is not a routine examination and was carried out only in a limited percentage of cases. This evaluation can be performed on several biological matrices, but the most commonly used are blood (for the entry of the substance into circulation) and gastric contents (for the methods of intake). Furthermore, although they were always higher than the normal percentage (1–2%), the MHb values showed wide variability, with a range from 9.87% to 83.4%. Although values around 70% are usually fatal [67], concentrations that are not too far from the normal range do not allow the exclusion of sodium nitrite as the cause of death, especially in cases in which comorbidities coexist. This statement is supported by studies in the literature that show that, in the clinical setting, the percentage of residual oxyhemoglobin represents only a theoretical capacity for oxygen transport, as it is necessary to take the effective tissue release capacity into account. The latter is strongly influenced by allosteric modifications of MHb, which are at the basis of a lower ability to transport oxygen, as well as a lower ability to release it. However, it is not possible to unambiguously determine the MHb concentration, especially in post-mortem analyses. In fact, these values may artificially be shown to be, on the one hand, increased after repeated freezing and thawing cycles and the lack of use of preservatives and, on the other hand, reduced due to the lack of prevention of the intracellular enzymatic reduction of MHb to hemoglobin and putrefactive hemolysis [68,69,70,71]. Therefore, the general orientation of forensic pathologists is to consider a causal correlation between the ingestion of sodium nitrite and death even for lower MHb values, as long as this association is substantiated by further objectivity [72].
Regarding accidental ingestion, despite the reduced frequency, it is important to focus on some epidemiological and preventive aspects. In the context of accidentality, most cases of intoxication can be traced back to the uncontrolled production of homemade foods. In such circumstances, the involvement of groups of people with heterogeneous clinical manifestations is not uncommon. From the clinical point of view, the manifestations are frequently mild, as no significant quantities of the additive are taken. In cases of survival, access to hospital care is extremely frequent. However, the index of clinical suspicion can sometimes be very low under consideration of the non-specificity of symptoms (nausea, vomiting, dyspnea, altered state of consciousness, and tachycardia). In fatal cases, the symptoms are mainly characterized by cyanosis, respiratory and hemodynamic instability, and alteration of consciousness. Even so, about half of the subjects die before reaching the hospital, which is probably due to the ingestion of high doses of sodium nitrite and a coincidence of chronic diseases. The scenario outlined here emphasizes the role of anamnestic collection in identifying patients to be sent for targeted diagnostic tests, including toxicological ones.
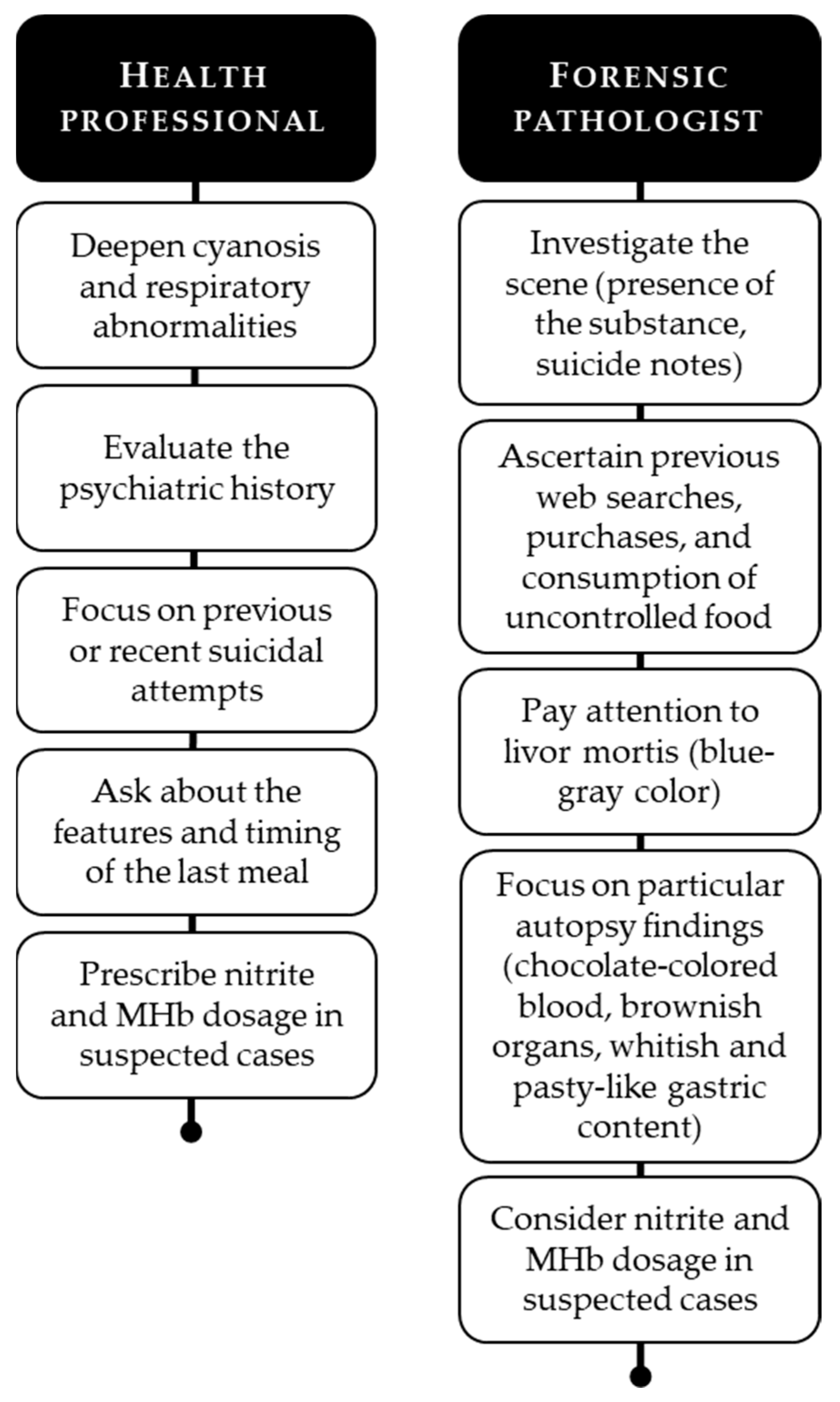
Given the above, the evidence that is currently available permits the presentation of an outline of practical advice for health professionals and forensic pathologists who are involved in cases of intoxication or death from sodium nitrite (Figure 6).

Figure 6.
Practical advice for healthcare professionals and forensic pathologists.
Finally, a problem of considerable importance is represented by the attribution of the causal relationship between the intake of the substance and intoxication or death. This task is particularly demanding, especially in cases in which the evidence highlighted cannot be univocally interpreted [73]. This gap can largely be filled by answering some questions about the phenomenology of the reaction to sodium nitrite ingestion.
5. Conclusions
Intoxication and death due to the ingestion of sodium nitrite represent a challenge for forensic pathologists. In fact, whether it is suicidal or unintentional ingestion, physicians must develop the necessary knowledge to suspect this methemoglobinemia to carry out necessary and unrepeatable tests for the correct diagnosis [74]. Future research and the sharing of evidence will guarantee the implementation of knowledge, as well as an ever more immediate identification of suspected cases.
Author Contributions
Conceptualization, M.P. and M.A.; Methodology, M.P. and M.S.; Validation, S.D., F.M. and M.C.D.; Formal analysis, M.C., F.M. and M.C.D.; Investigation, M.P. and M.C.D.; Data curation, M.P., M.A. and M.C.; Writing—original draft preparation, M.P., M.A. and F.M.; Writing—review and editing, M.P., S.D. and M.S.; Visualization, S.D. and M.S.; Supervision, P.F. and V.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organisation. Suicide: Key Facts. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 16 February 2021).
- Garnett, M.F.; Curtin, S.C.; Stone, D.M. Suicide Mortality in the United States, 2000–2020. NCHS Data. Brief. 2022, 433, 1–8. [Google Scholar]
- Mergl, R.; Koburger, N.; Heinrichs, K.; Székely, A.; Toth, M.D.; Coyne, J.; Quintão, S.; Arensman, E.; Coffey, C.; Maxwell, M.; et al. What Are Reasons for the Large Gender Differences in the Lethality of Suicidal Acts? An Epidemiological Analysis in Four European Countries. PLoS ONE 2015, 10, e0129062. [Google Scholar] [CrossRef] [PubMed]
- Tsirigotis, K.; Gruszczynski, W.; Tsirigotis-Woloszczak, M. Gender differentiation in methods of suicide attempts. Med. Sci. Monit. 2011, 17, PH65–PH70. [Google Scholar] [CrossRef] [PubMed]
- Cibis, A.; Mergl, R.; Bramesfeld, A.; Althaus, D.; Niklewski, G.; Schmidtke, A.; Hegerl, U. Preference of lethal methods is not the only cause for higher suicide rates in males. J. Affect. Disord. 2012, 136, 9–16. [Google Scholar] [CrossRef]
- O’Rourke, M.C.; Jamil, R.T.; Siddiqui, W. Suicide Screening and Prevention. In StatPearls (Internet); StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Barranco, R.; Frigiolini, F.M.E.; Orcioni, G.F.; Malandrino, M.; Salomone, A.; Ventura, F. A Rare Case of Fatal Self-Poisoning with Sodium Nitrite: Autopsy and Toxicological Findings. Am. J. Forensic Med. Pathol. 2021, 42, 379–382. [Google Scholar] [CrossRef] [PubMed]
- Leavesley, H.B.; Li, L.; Mukhopadhyay, S.; Borowitz, J.L.; Isom, G.E. Nitrite-Mediated Antagonism of Cyanide Inhibition of Cytochrome c Oxidase in Dopamine Neurons. Toxicol. Sci. 2010, 115, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, J.S.; Andrew, L.M. Human safety controversies surrounding nitrate and nitrite in the diet. Nitric Oxide 2012, 26, 259–266. [Google Scholar] [CrossRef]
- Commission Decision (EU) 2018/702 of 8 May 2018 Concerning National Provisions Notified by Denmark on the Addition of Nitrite to Certain Meat Products (Notified under Document C(2018) 2721). Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32018D0702 (accessed on 17 September 2022).
- Consolidated Text: Regulation (EC) No 1333/2008 of the European Parliament and of the Council of 16 December 2008 on Food Additives (Text with EEA Relevance). Available online: https://eur-lex.europa.eu/eli/reg/2008/1333/2016-05-25 (accessed on 17 September 2022).
- Scopetti, M.; Padovano, M.; Peruch, M.; Concato, M.; Livieri, T.; Radaelli, D.; D’Errico, S. Recreational cannabis use: Regulatory aspects, public opinion and concerns for public health. In Current Pharmaceutical Biotechnology; Bentham Science Publishers: Sharjah, United Arab Emirates, 2022; Online ahead of print. [Google Scholar] [CrossRef]
- Wright, R.O.; Lewander, W.J.; Woolf, A.D. Methemoglobinemia: Etiology, Pharmacology, and Clinical Management. Ann. Emerg. Med. 1999, 34, 646–656. [Google Scholar] [CrossRef]
- Anderson, C.M.; Woodside, K.J.; Spencer, T.A.; Hunter, G.C. Methemoglobinemia: An unusual cause of postoperative cyanosis. J. Vasc. Surg. 2004, 39, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Naranjo, C.A.; Busto, U.; Sellers, E.M.; Sandor, P.; Ruiz, I.; Roberts, E.A.; Janecek, E.; Domecq, C.; Greenblatt, D.J. A method for estimating the probability of adverse drug reactions. Clin. Pharmacol. Ther. 1981, 30, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Çağlar, A.; Karaarslan, U.; Ulusoy, E.; Akgül, F.; Köroğlu, T.F.; Duman, M.; Yılmaz, D.; Er, A.; Inci, G. Severe Methemoglobinemia Due to Nitrite Intoxication in a Child Who was Misdiagnosed with Sepsis. Turk. J. Pediatr. Emerg. Intensiv. Care. Med. 2016, 3, 155–158. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Methemoglobinemia following unintentional ingestion of sodium nitrite-New York, 2002. MMWR Morb. Mortal. Wkly. Rep. 2002, 51, 639–642. [Google Scholar]
- Cruz, M.D.; Glick, J.; Merker, S.H.; Vearrier, D. Survival after severe methemoglobinemia secondary to sodium nitrate ingestion. Toxicol. Commun. 2018, 2, 21–23. [Google Scholar] [CrossRef]
- Cvetković, D.; Živković, V.; Lukić, V.; Nikolić, S. Sodium nitrite food poisoning in one family. Forensic. Sci. Med. Pathol. 2018, 15, 102–105. [Google Scholar] [CrossRef]
- Dean, D.E.; Looman, K.B.; Topmiller, R.G. Fatal methemoglobinemia in three suicidal sodium nitrite poisonings. J. Forensic. Sci. 2021, 66, 1570–1576. [Google Scholar] [CrossRef]
- Durão, C.; Pedrosa, F.; Dinis-Oliveira, R.J. A fatal case by a suicide kit containing sodium nitrite ordered on the internet. J. Forensic Leg. Med. 2020, 73, 101989. [Google Scholar] [CrossRef]
- Durão, C.; Pedrosa, F.; Dinis-Oliveira, R.J. Another suicide by sodium nitrite and multiple drugs: An alarming trend for “exit”? Forensic. Sci. Med. Pathol. 2020, 17, 362–366. [Google Scholar] [CrossRef]
- Finan, A.; Keenan, P.; Donovan, F.O.; Mayne, P.; Murphy, J. Lesson of the week: Methaemoglobinaemia associated with sodium nitrite in three siblings. BMJ 1998, 317, 1138–1139. [Google Scholar] [CrossRef]
- Gowans, W.J. Fatal methaemoglobinaemia in a dental nurse. A case of sodium nitrite poisoning. Br. J. Gen. Pract. 1990, 40, 470–471. [Google Scholar] [PubMed]
- Harvey, M.; Cave, G.; Chanwai, G. Fatal methaemoglobinaemia induced by self-poisoning with sodium nitrite. Emerg. Med. Australas. 2010, 22, 463–465. [Google Scholar] [CrossRef] [PubMed]
- Hickey, T.B.; MacNeil, J.A.; Hansmeyer, C.; Pickup, M.J. Fatal methemoglobinemia: A case series highlighting a new trend in intentional sodium nitrite or sodium nitrate ingestion as a method of suicide. Forensic Sci. Int. 2021, 326, 110907. [Google Scholar] [CrossRef]
- Hwang, C.; Yeon, S.-H.; Jung, J.; Na, J.-Y. An autopsy case of sodium nitrite-induced methemoglobinemia with various post-mortem analyses. Forensic Sci. Med. Pathol. 2021, 17, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, A.; Smith, C.; Promnitz, D.A.; Joffe, B.I.; Seftel, H.C. Methaemoglobinaemia due to accidental sodium nitrite poisoning. Report of 10 cases. S. Afr. Med. J. 1990, 77, 300–301. [Google Scholar]
- Katabami, K.; Hayakawa, M.; Gando, S. Severe Methemoglobinemia due to Sodium Nitrite Poisoning. Case Rep. Emerg. Med. 2016, 2016, 9013816. [Google Scholar] [CrossRef]
- Kennedy, N.; Smith, C.P.; McWhinney, P. Faulty sausage production causing methaemoglobinaemia. Arch. Dis. Child. 1997, 76, 367–368. [Google Scholar] [CrossRef]
- Kim, M.; Kim, S.; Yang, W.; Sim, J. Determination of nitrite and nitrate in postmortem whole blood samples of 10 sodium nitrite poisoning cases: The importance of nitrate in determining nitrite poisoning. Forensic Sci. Int. 2022, 335, 111279. [Google Scholar] [CrossRef]
- Lee, C.; Jang, E.J.; Yum, H.; Choi, Y.S.; Hong, J. Unintentional mass sodium nitrite poisoning with a fatality. Clin. Toxicol. 2017, 55, 678–679. [Google Scholar] [CrossRef]
- Lien, Y.-H.; Lin, Y.-C.; Chen, R.J. A case report of acquired methemoglobinemia rescued by veno-venous extracorporeal membrane oxygenation. Medicine 2021, 100, e25522. [Google Scholar] [CrossRef]
- Maric, P.; Ali, S.S.; Heron, L.G.; Rosenfeld, D.; Greenwood, M.; Bs(Hons), P.M.M.; Frcpa, F.L.G.H.; Fracp, F.D.R. Methaemoglobinaemia following ingestion of a commonly available food additive. Med. J. Aust. 2008, 188, 156–158. [Google Scholar] [CrossRef] [PubMed]
- Matin, A.M.; Boie, E.T.; Moore, G.P. Survival after self-poisoning with sodium nitrite: A case report. J. Am. Coll. Emerg. Physicians Open 2022, 3, e12702. [Google Scholar] [CrossRef] [PubMed]
- Matteucci, O.; Diletti, G.; Prencipe, V.; Di Giannatale, E.; Marconi, M.M.; Migliorati, G. Two cases of methemoglobinaemia caused by suspected sodium nitrite poisoning. Veter. Ital. 2008, 44, 439–453. [Google Scholar]
- McCann, S.D.; Kennedy, J.M.; Tweet, M.S.; Bryant, S.M. Sodium Nitrite Ingestion: An Emerging Trend in Suicide Attempts Shared via Online Communities. J. Emerg. Med. 2021, 60, 409–412. [Google Scholar] [CrossRef] [PubMed]
- Mudan, A.; Repplinger, D.; Lebin, J.; Lewis, J.; Vohra, R.; Smollin, C. Severe Methemoglobinemia and Death From Intentional Sodium Nitrite Ingestions. J. Emerg. Med. 2020, 59, e85–e88. [Google Scholar] [CrossRef]
- Mun, S.H.; Park, G.J.; Lee, J.H.; Kim, Y.M.; Chai, H.S.; Kim, S.C. Two cases of fatal methemoglobinemia caused by self-poisoning with sodium nitrite: A case report. Medicine 2022, 101, e28810. [Google Scholar] [CrossRef]
- Neth, M.R.; Love, J.S.; Horowitz, B.Z.; Shertz, M.D.; Sahni, R.; Daya, M.R. Fatal Sodium Nitrite Poisoning: Key Considerations for Prehospital Providers. Prehospital Emerg. Care 2020, 25, 844–850. [Google Scholar] [CrossRef]
- Nushida, M.N.H. An Autopsy Case of Fatal Methemoglobinemia due to Ingestion of Sodium Nitrite. J. Forensic Res. 2015, 6, 1. [Google Scholar] [CrossRef]
- O’Neill, C.; Najjar, Z.; Ingleton, A.; Edwards, A.; Dawson, A.; Gupta, L. Methaemoglobinaemia associated with the atypical use of sodium nitrite as a food additive. Med. J. Aust. 2021, 215, 256–257.e1. [Google Scholar] [CrossRef]
- Sajko, N.; Finn, K.; Hill, J.; Khaira, G.K.; Duff, J.P.; Jiwani, F.; Allain, D.; Oliva, M.A. Near-fatal pediatric methemoglobinemia secondary to intentional sodium nitrite ingestion: A case report. Am. J. Emerg. Med. 2022, 59, 215.e1–215.e5. [Google Scholar] [CrossRef]
- Sohn, C.H.; Seo, D.W.; Ryoo, S.M.; Lee, J.H.; Kim, W.Y.; Lim, K.S.; Oh, B.J. Life-threatening methemoglobinemia after unintentional ingestion of antifreeze admixtures containing sodium nitrite in the construction sites. Clin. Toxicol. 2013, 52, 44–47. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.-F.; Lu, L.-H.; Hsu, T.-H.; Chang, S.-L.; Lin, R.-T. Successful treatment of methemoglobinemia in an elderly couple with severe cyanosis: Two case reports. J. Med. Case. Rep. 2012, 6, 290. [Google Scholar] [CrossRef] [PubMed]
- Taus, F.; Pigaiani, N.; Bortolotti, F.; Mazzoleni, G.; Brevi, M.; Tagliaro, F.; Gottardo, R. Direct and specific analysis of nitrite and nitrate in biological and non-biological samples by capillary ion analysis for the rapid identification of fatal intoxications with sodium nitrite. Forensic Sci. Int. 2021, 325, 110855. [Google Scholar] [CrossRef] [PubMed]
- Tomsia, M.; Głaz, M.; Nowicka, J.; Szczepański, M. Sodium nitrite detection in costal cartilage and vitreous humor–Case report of fatal poisoning with sodium nitrite. J. Forensic Leg. Med. 2021, 81, 102186. [Google Scholar] [CrossRef] [PubMed]
- Tung, S.-P.; How, C.-K.; Chern, C.-H. Methaemoglobinaemia secondary to the ingestion of sodium nitrite in mistake for common salt. Resuscitation 2006, 70, 168–169. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Teng, C.; Zhang, N.; Zhang, J.; Conway, G. A Family Clustered Nitrite Intoxication Investigation in Gaoxin District, Suzhou, China, 2013. Iran. J. Public. Health 2013, 42, 1465–1471. [Google Scholar] [PubMed]
- Thomas, K.; Chang, S.-S.; Gunnell, D. Suicide epidemics: The impact of newly emerging methods on overall suicide rates-a time trends study. BMC Public Health 2011, 11, 314. [Google Scholar] [CrossRef]
- Hegerl, U.; Wittenburg, L.; Arensman, E.; Van Audenhove, C.; Coyne, J.C.; McDaid, D.; Van Der Feltz-Cornelis, C.M.; Gusmão, R.; Kopp, M.; Maxwell, M.; et al. Optimizing Suicide Prevention Programs and Their Implementation in Europe (OSPI Europe): An evidence-based multi-level approach. BMC Public Health 2009, 9, 428. [Google Scholar] [CrossRef]
- Padmanathan, P.; Biddle, L.; Carroll, R.; Derges, J.; Potokar, J.; Gunnell, D. Suicide and Self-Harm Related Internet Use. Crisis 2018, 39, 469–478. [Google Scholar] [CrossRef]
- Biddle, L.; Derges, J.; Mars, B.; Heron, J.; Donovan, J.L.; Potokar, J.; Piper, M.; Wyllie, C.; Gunnell, D. Suicide and the Internet: Changes in the accessibility of suicide-related information between 2007 and 2014. J. Affect. Disord. 2016, 190, 370–375. [Google Scholar] [CrossRef]
- Lopez-Agudo, L.A. The association between internet searches and suicide in Spain. Psychiatry Res. 2020, 291, 113215. [Google Scholar] [CrossRef]
- Barros, J.M.; Melia, R.; Francis, K.; Bogue, J.; O’Sullivan, M.; Young, K.; Bernert, R.A.; Rebholz-Schuhmann, D.; Duggan, J. The Validity of Google Trends Search Volumes for Behavioral Forecasting of National Suicide Rates in Ireland. Int. J. Environ. Res. Public Health 2019, 16, 3201. [Google Scholar] [CrossRef] [PubMed]
- Becker, M.; Correll, C.U. Suicidality in Childhood and Adolescence. Dtsch. Arztebl. Int. 2020, 117, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Hawton, K.; Hill, N.; Gould, M.; John, A.; Lascelles, K.; Robinson, J. Clustering of suicides in children and adolescents. Lancet Child Adolesc. Health 2019, 4, 58–67. [Google Scholar] [CrossRef]
- Bradberry, S.M.; Aw, T.-C.; Williams, N.R.; Vale, J.A. Occupational Methaemoglobinaemia. Occup. Environ. Med. 2001, 58, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Solin, P.; Tamminen, N.; Partonen, T. Suicide prevention training: Self-perceived competence among primary healthcare professionals. Scand. J. Prim. Health Care 2021, 39, 332–338. [Google Scholar] [CrossRef]
- D’Errico, S.; Zanon, M.; Radaelli, D.; Concato, M.; Padovano, M.; Scopetti, M.; Frati, P.; Fineschi, V. Acute Kidney Injury (AKI) in Young Synthetic Cannabinoids Abusers. Biomedicines 2022, 10, 1936. [Google Scholar] [CrossRef] [PubMed]
- Park, M.J.; Kim, O.; Ha, H. Death by Nitrite Intoxication: Report of 14 Cases. Korean J. Leg. Med. 2020, 44, 96–101. [Google Scholar] [CrossRef]
- D’Errico, S.; Zanon, M.; Peruch, M.; Concato, M.; Padovano, M.; Santurro, A.; Scopetti, M.; Fineschi, V. Mors Gaudet Succurrere Vitae. The Role of Clinical Autopsy in Preventing Litigation Related to the Management of Liver and Digestive Disorders. Diagnostics 2021, 11, 1436. [Google Scholar] [CrossRef] [PubMed]
- Hathazi, D.; Scurtu, F.; Bischin, C.; Mot, A.; Attia, A.A.A.; Kongsted, J.; Silaghi-Dumitrescu, R. The Reaction of Oxy Hemoglobin with Nitrite: Mechanism, Antioxidant-Modulated Effect, and Implications for Blood Substitute Evaluation. Molecules 2018, 23, 350. [Google Scholar] [CrossRef] [PubMed]
- Coleman, M.D.; Coleman, N.A. Drug-Induced Methaemoglobinaemia Treatment Issues. Drug. Saf. 1996, 14, 394–405. [Google Scholar] [CrossRef]
- Varlet, V.; Ryser, E.; Augsburger, M.; Palmiere, C. Stability of postmortem methemoglobin: Artifactual changes caused by storage conditions. Forensic Sci. Int. 2018, 283, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Rodkey, F.; O’Neal, J.D. Effects of carboxyhemoglobin on the determination of methemoglobin in blood. Biochem. Med. 1974, 9, 261–270. [Google Scholar] [CrossRef]
- Sato, K.; Katsumata, Y.; Aoki, M.; Oya, M.; Yada, S.; Suzuki, O. A practical method for the accurate determination of methemoglobin in blood containing carboxyhemoglobin. Forensic Sci. Int. 1981, 17, 177–184. [Google Scholar] [CrossRef]
- Ishiwata, Y.; Arima, Y.; Fujishiro, M.; Ohtawa, T.; Izawa, H.; Sobue, H.; Taira, R.; Umezawa, H.; Lee, X.P.; Sato, K. Long-term storage of blood at freezing temperatures for methemoglobin determination: Comparison of storage with and without cryo-protectant. Showa Univ. J. Med. Sci. 2008, 20, 123–129. [Google Scholar] [CrossRef][Green Version]
- Saleh, D.; Lucyk, S.; McGillis, E. Methemoglobinemia caused by sodium nitrite overdose. CMAJ 2022, 194, E1066–E1067. [Google Scholar] [CrossRef] [PubMed]
- La Russa, R.; Fineschi, V.; Di Sanzo, M.; Gatto, V.; Santurro, A.; Martini, G.; Scopetti, M.; Frati, P. Personalized Medicine and Adverse Drug Reactions: The Experience of An Italian Teaching Hospital. Curr. Pharm. Biotechnol. 2017, 18, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Cerretani, D.; Riezzo, I.; Fiaschi, A.I.; Centini, F.; Giorgi, G.; D’Errico, S.; Fiore, C.; Karch, S.B.; Neri, M.; Pomara, C.; et al. Cardiac oxidative stress determination and myocardial morphology after a single ecstasy (MDMA) administration in a rat model. Int. J. Legal. Med. 2008, 122, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Bugelli, V.; Tarozzi, I.; Manetti, A.C.; Stefanelli, F.; Di Paolo, M.; Chericoni, S. Four cases of sodium nitrite suicidal ingestion: A new trend and a relevant Forensic Pathology and Toxicology challenge. Leg. Med. 2022, 59, 102146. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).