Abstract
Background: The study aimed to explore the psychometric properties of two versions of the Patient Health Questionnaires (PHQ-9 and PHQ-2) on screening for Major Depressive Disorder (MDD) among Spanish-speaking Latin American adult immigrants in Santiago, and to explore factors associated with a higher risk of occurrence of MDD among them. Methods: A representative sample of 897 Spanish-speaking immigrants completed the PHQ-9. The Composite International Diagnostic Interview (CIDI) was employed to evaluate MDD. Internal consistency and structural validity were evaluated using Cronbach’s α coefficient and confirmatory factor analysis (CFA). Convergent validity with the 7-item General Anxiety Disorder Scale (GAD-7) was assessed using Spearman’s correlations. Sensitivity, specificity, positive predictive values, and area under the receiver operating characteristic (ROC) curve were calculated for different cut-off points. Logistic regression analysis was used to identify factors associated with the risk of MDD. Results: Cronbach’s α coefficient of the PHQ-9 was 0.90; item-total correlation coefficients ranged from 0.61 to 0.76 and correlation with the GAD-7 was moderate (r = 0.625; p < 0.001). CFA on three alternative models suggests a plausible fit in the overall sample and among two of the subsamples: Peruvians and Venezuelans. Taking the results of CIDI as the gold standard for MDD, the area under the ROC curve was 0.91 (95% confidence interval (CI): 0.83~1.0). When the cut-off score was equal to 5, values of sensitivity, specificity, and Youden’s index were 0.85, 0.90, and 0.75, respectively. Multivariate logistic regression analyses showed that the influence of having three or more children (OR = 3.91, 95% CI: 1.20~12.81; p < 0.05), residency in Chile of up to three years (OR = 1.79, 95% CI: 1.07~3.00; p < 0.05), active debt (OR = 2.74, 95% CI: 1.60~4.70; p < 0.001), a one (OR = 2.01, 95% CI: 1.03~3.94; p < 0.05) and two or more events of adversity during childhood (OR = 5.25, 95% CI: 1.93~14.3; p < 0.01) on the occurrence of MDD was statistically significant. Reliability (α = 0.62), convergent (r = 0.534; p < 0.01) and criterion (AUC = 0.85, 95% CI: 0.67~1.00) validity coefficients of the PHQ-2 were weaker than for the PHQ-9. Conclusions: The PHQ-2 and the PHQ-9 are reliable and valid instruments for use as screeners for MDD among Spanish-speaking populations of Latin America.
1. Background
Major Depressive Disorder (MDD) is one of the most prevalent mental health conditions in the general population [1], globally affecting an estimated 4.7% of individuals in the community [2]. It is also the most common psychiatric condition in people who die from suicide [3] and one of the leading causes of burden [4]. MDD, however, is frequently untreated, particularly in low- and middle-income countries [5].
The nine-item Patient Health Questionnaire (PHQ-9) is one of the most widely used screening questionnaires for MDD [6] and has been translated into more than 80 languages [7]. Its accuracy has been shown to be greater than unaided clinician diagnoses with much higher sensitivity (0.80) and specificity (0.92) [8] than the sensitivity (0.50) and specificity (0.81) of primary care providers’ diagnoses [9].
The Spanish version of the PHQ-9 [10] has been validated in some Latin American populations. Its psychometric properties and convergent validity with a structured clinical interview as a reference gold standard have been documented in clinical settings in Argentina [11,12], Colombia [13], Peru [14], and Chile [15,16] and its factor structure has been studied among several non-clinical subpopulations: college students in Colombia [17], Ecuador [18] and Peru [19], and teachers [20] and rural communities in Mexico [21]. The performance of the first two items of the PHQ (i.e., PHQ-2) versus all nine items has also been assessed in primary care in Colombia [22] and among non-clinical populations in Chile [23] and Mexico [21].
Chile has been increasingly receiving economic immigrants in the last decade. In 2017, the estimated number of immigrants was 700,000, representing 4.4% of the total population [24]. A large majority of immigrants (76%) originate from Spanish-speaking Latin American countries, with Peruvians, Colombians, and Venezuelans forming the first, second, and third largest groups (50.4% of all immigrants [24]). While a lower prevalence of MDD among immigrants compared to the native-born population has been documented in high-income countries [25,26,27,28], evidence suggests that, in some cases, the migration experience may have a negative impact on mental health [29,30].
Because of the growth in the number of Latin American immigrants arriving in Chile, and the layers of vulnerability they experience [31], it is important to understand if the available screening measures for MDD are valid to use among them.
To our knowledge, the Spanish version of the PHQ-9 has not been validated in non-clinical populations of Latin America with a reference gold standard and no studies have validated its screening characteristics among Spanish-speaking immigrants in Chile. To cover this gap, we designed the present study which analyses the psychometric properties of the PHQ-9 among a representative sample of native Spanish-speaking adult immigrants in Santiago, Chile. The primary aim focuses on the reliability of items (internal consistency), the dimensionality (structural validity), and convergence with a reference gold standard in identifying respondents with MDD (criterion validity). Secondary aims include (i) identifying factors associated with a higher risk of the occurrence of MDD in the Spanish-speaking immigrant population in Chile, and (ii) exploring the psychometric properties of the PHQ-2 among this population. The results of this study will provide evidence about the quality of this screening tool for MDD for this specific immigrant population as well as information about the prevalence of depressive symptoms and associated factors to MDD among them.
2. Material and Methods
2.1. Design
The Santiago Immigrant Wellbeing Study (STRING) is a population-based cross-sectional household mental health survey of 1115 first-generation adult immigrants residing in the Santiago Metropolitan Region (Región Metropolitana; RM) of Chile. The study was prospectively registered (ClinicalTrials.gov Identifier: NCT04114565; ISRCTN96875479) and approved by the Ethics Committee of the School of Medicine of the Pontificia Universidad Catolica de Chile (No. 170519004). Data was collected between August and October 2019.
2.2. Participants
The sampling framework of the Chilean National Institute of Statistics was used. Multi-stage random probability sampling, comparable to that of other household survey designs conducted in developing countries was employed [32]. Based on (i) the number of immigrants recorded in the RM in the 2017 Chilean Population Census [33], distributed in 120 conglomerates (i.e., clusters of 200 households with a mean number of 9.2 immigrants), and (ii) the density of the immigrant population in the RM, the minimum sample size to generate statistical inferences was set at 1104. The final sample was composed of 1115 participants, of which 1091 were interviewed in Spanish and 24 in Creole. To be eligible, participants had to: (i) be a community-residing adult (18+ years), (ii) be able to read and write, (iii) have been born outside of Chile (self-reported and providing a National ID number), and (iv) have been residing in Chile for at least six months.
This study aimed to explore the psychometric properties of the nine- and two-item Patient Health Questionnaires (i.e., PHQ-9 and PHQ-2) on screening for depression among the subsample of participants of the STRING study interviewed in Spanish and born in Spanish-speaking Latin American countries (n = 897).
2.3. Measures
The PHQ-9 is a nine-item self-reporting questionnaire that assesses the presence and severity of depressive symptoms (i. anhedonia, ii. depressed mood, iii. sleep problems, iv. low energy, v. appetite changes, vi. low self-esteem, vii. concentration difficulty, viii. psychomotor agitation or retardation and ix. suicidal ideation) in the last two weeks based on the DSM-IV criteria for MDD. Using a Likert scale, each item can be rated from 0 (not at all) to 3 (nearly every day) with total scores ranging from 0 to 27. Five categories of symptom severity have been proposed: 0–4 (minimum), 5–9 (mild), 10–14 (moderate), 15–19 (moderate to severe), 20–27 (serious) [6] and cut-off scores between 8 and 11 have been recommended for a probable case of MDD [34]. In this study, the Spanish version of the questionnaire was employed [10] and administered face-to-face.
The PHQ-2 is an ultra-brief version of the PHQ-9 which includes the first two items (i. anhedonia, ii. depressed mood). Total scores range from 0 to 6 and the recommended cut-off point for administering the full PHQ-9 or conducting a clinical interview to assess for MDD is a score of 3 or greater [35].
Symptoms of anxiety during the 2 weeks preceding the interview were assessed using the Spanish version of the 7-item General Anxiety Disorder (GAD–7) scale [36]. DSM-IV MDD in the last 12 months was assessed using two modules of the WHO Composite International Diagnostic Interview (WHO-CIDI) (CAPI 3.0): depression, and mania [37]. The WHO-CIDI is a gold standard for MDD diagnosis which has been used extensively in major epidemiological studies in Argentina [38], Chile [39,40], Colombia [5,41,42,43,44,45,46,47], Guatemala [48], Mexico [5,49,50,51] and Peru [5,52].
Childhood trauma was measured using the Spanish-translated version of the Adverse Childhood Experiences International Questionnaire (ACE-IQ) [53] and coded into 0, 1, or 2 or more adverse events.
Participants’ gender, age, country of birth, number of children aged under 18 years, duration of residency in Chile (up to 3 years; more than 3 years), highest educational level (primary: 8 years or less; secondary: 9 to 12 years; or higher: >12 years), employment status (unemployed or economically inactive versus employed), active debt status (with or without) was recorded.
2.4. Statistical Analysis
To characterize the representative immigrant population of Santiago, sampling weights assigned to the subjects were applied. For descriptive statistics, means, standard deviations, and frequencies were calculated for demographic and economic factors and for the number of childhood adversity events.
The normality distribution was tested using the Kolmogorov-Smirnov test. When variables were not found to have a normal distribution, Spearman’s Rho was used. For reliability, the internal consistency of the PHQ-9 was assessed using Cronbach’s alpha (α) coefficients and item-total correlations. For the PHQ-2, Spearman–Brown coefficients were calculated as an additional measure of reliability. Alpha coefficients above 0.70–0.80 were considered indicative of good internal consistency [54]. Correlations above 0.90, between 0.70 and 0.90, and between 0.50 and 0.70 were considered very high, high, and moderate, respectively [55].
To investigate the factor structure of the PHQ-9 items, Confirmatory factor analysis (CFA) with the maximum-likelihood procedure was conducted. Using CFA, three alternative models of the structure of the PHQ-9 were tested to understand the dimensionality of the scale: (i) the original one-factor model hypothesized by Kroenke [6], (ii) a two-factor model suggested by Krause [56] where three items (i.e., ‘sleep problems’, ‘low energy’ and ‘appetite changes’) are loaded on a somatic factor, and (iii) another two-factor model derived by Richardson and Richard [57] where the somatic factor also includes ‘concentration difficulties’ and ‘psychomotor agitation/retardation’ (Figure S1). In addition to the chi-square (χ2) and its degrees of freedom (df), models were compared using the following three model fit indices and their criteria: (i) the robust comparative fit index (CFI) with a value greater than 0.95 indicating a good model fit and values larger than 0.90 indicating a plausible model fit [58], (ii) the robust root mean square error of approximation (RMSEA) and its 90% confidence interval with a value lower than 0.05 indicating a good fit and values lower than 0.08 indicating a plausible fit [59], and (iii) the standardized root mean square residual (SRMR) with values less than 0.05 indicating a good fit well and values lower than 0.08 indicating a plausible fit [60]. A model was considered to fit well if two of the three criteria were met.
The convergent validity of the PHQ-2 and PHQ-9 was assessed using Spearman’s correlations with the GAD-7. To assess the accuracy of both forms of the PHQ as screening tools compared to the CIDI, the receiver operating characteristics (ROC) and AUC were analyzed. The optimum cut-off point for the PHQ-9 was determined considering validity indices: sensitivity (Se), specificity (Sp), positive and negative predictive value (PPV; NPV), Youden’s index, positive and negative likelihood ratios (LR), and ROC curve/AUC analysis. Two additional indices were used: clinically relevant rule in accuracy as estimated by the clinical utility index positive (CUI+) and rule out accuracy as estimated by the clinical utility index negative (CUI) [61].
To evaluate the association between demographic, economic, and adversity characteristics and a total PHQ-9 total score over the defined optimum cut-off point, age, and gender-adjusted logistic regression analyses were conducted.
The statistical analysis, excluding CFA, was performed using SPSS for Windows, version 20.0 (IBM Corp, Armonk, NY, USA). CFA was conducted using R 3.5.1 software (The R Foundation for Statistical Computing, Vienna, Austria). A p-value < 0.05 was considered significant.
3. Results
3.1. Sample Characteristics
Table 1 illustrates the sociodemographic, economic, and childhood adversity characteristics of the final sample (n = 897). The mean age of participants was 36.6 years (SD = 11.5); 478 (53.6%) had no children under the age of 18, 217 (22.7%) had one, 144 (16.2%) had two and 55 (7.5%) had three or more children. There were 509 women (53.8%) and 388 men (46.2%); 94 respondents had been born in Colombia (13.2%), 333 in Peru (26.6%), 375 in Venezuela (33.3%), and 95 (26.9%) in other Spanish-speaking Latin American countries (Bolivia, Cuba, Dominican Republic, Ecuador, and Mexico); 444 (50.3%) participants had migrated in the last three years and 453 (49.7%) more than three years ago.

Table 1.
Sociodemographic, economic, and childhood trauma characteristics of participants (n = 897).
Few participants (7.6%) were unemployed or economically inactive; 72 (7.2%) respondents had ≤8 years of education, 351 (41.6%) had between 9 and 12, and 471 (51.2%) had more than 12 years, and 201 (22.4%) held at least one debt at the moment of the interview. No events of childhood adversity were reported by most participants (68.6%), one event was reported by 15.7%, and two or more events by 15.7% of participants.
Only 34 (4.5%) participants scored above the PHQ-9 most common cut-off score (≥10), 42 (4.6%) respondents above the recommended cut-off score for the PHQ-2 (≥3), and only 6 (0.7%) participants met the criteria for DSM-IV MDD in the last 12 months (Table 2). Results for specific immigrant groups showed the proportion of PHQ-9 total scores ≥ 10 ranged from 1.7% among Venezuelans to 7.1% among Peruvians, and the proportion of PHQ-2 scores ≥ 3 ranged from 1.4% among other Latin Americans to 8.1% among Colombians (Table S1).

Table 2.
Distribution of PHQ scores and 12-month-CIDI Major Depressive Disorder (n = 897).
3.2. Reliability
Values of the reliability coefficient Cronbach’s α for the PHQ-9 and PHQ-2 were 0.904 and 0.746, indicating acceptable reliability. For both PHQ forms, corrected item-total correlations ranged from moderate to high (0.604–0.760), and the internal consistency of the PHQ-9 would not have improved with the deletion of later scale items. The Spearman–Brown between-item correlation coefficient for the PHQ-2 was significant but moderate (r = 0.62; p < 0.001) (Table S2). The reliability of the PHQ-9 was acceptable across immigrant groups (all α > 0.7) and corrected item-total correlations ranged from low to high (0.451–0.845) (Table S3). The reliability of the PHQ-2 was only acceptable for the Peruvian and other Latin American subsamples (all α > 0.7 and r > 0.70; p < 0.001) (Table S4).
3.3. Factor Structure
Confirmatory factor analysis (CFA) on three alternative models was performed: a one-factor model (model 1) and two two-factor models (models 2a and 2b). The goodness of fit indices suggest a plausible fit for the three models for the overall sample and the Peruvian subsample and for model 2a for the Venezuelan subsample, with CFI values larger than 0.90 and SRMS values lower than 0.08. The goodness of fit indices for the Colombian and the other Latin American subsamples demonstrate inadequate fit of all three models (Table S5). Overall results from the two-factor models showed that the somatic and affective factors were highly correlated (all p < 0.001).
3.4. Convergent Validity
In the overall sample, the PHQ-9 was moderately and positively correlated with the GAD-7 (r = 0.625; p < 0.001), which measures anxiety symptoms. Correlation between PHQ-2 and GAD-7 scores was weaker, but significant (r = 0.534; p < 0.01). Across immigrant groups, correlations between the GAD-7 and the PHQ-9 and PHQ-2 were moderate (all r ≥ 0.60; p < 0.001) and low-to-moderate (all r ≥ 0.44; p < 0.001), respectively. Convergent validity was, therefore, satisfied for both forms of the PHQ with our sample (Table S6).
3.5. Criterion Validity
The performance of the two versions of the PHQ was examined against the diagnosis of MDD according to the WHO-CIDI as a gold standard. The mean PHQ-9 and PHQ-2 scores for participants meeting the criteria for MDD were 9.14 (SD = 5.36) and 2.19 (SD = 1.39), respectively, whereas the mean scores for participants not meeting the criteria for MDD were 1.71 (SD = 3.68) and 0.38 (SD = 0.98), respectively.
Table 3 summarizes the operating characteristics of the PHQ-9 and PHQ-2 at different cut-off points for diagnosing MDD against the WHO-CIDI. For the PHQ-9, the cut-off of 5 yielded the best diagnostic performance in terms of maximizing sensitivity and specificity values based on the Youden J index (sensitivity = 85%; specificity 90%). Despite the excellent rule-out accuracy (CU− = 0.90) and NPV (NPV = 1.00) for this cut-off score, negative and positive likelihood ratios were moderate (LR+ = 8.73; LR− = 0.17) and PPV and rule-in accuracy were very poor (PPV = 0.06; CUI+ = 0.05). The ROC curve analysis estimated the area under the curve (AUC) for the PHQ-9 was 0.91 (95% CI: 0.83–1.00) (Figure 1), which accounts for outstanding classification accuracy.

Table 3.
Performance of PHQ-9 and PHQ-2 cut-off scores in detecting major depressive disorder.
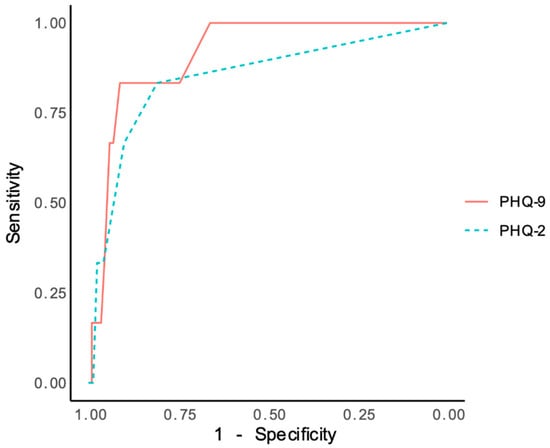
Figure 1.
Receptor operating characteristics (ROC) curves of the PHQ-9 and PHQ-2 compared with the Composite International Diagnostic Interview as a reference standard for MDD.
For the PHQ-2, optimal diagnostic performance was achieved at a cut-off score of 1, which best balances sensitivity and specificity (sensitivity = 73%; specificity 89%). Despite the high NPV (NPV = 1.00) and excellent rule-out accuracy (CU− = 0.89) for this cut-off score, likelihood ratios were moderate (LR+ = 6.58; LR− = 0.30) and PPV and rule-in accuracy were very poor (PPV = 0.04; CUI+ = 0.89). The AUC of PHQ-2 was 0.85 (95% CI: 0.67–1.00) which accounts for excellent accuracy [62].
3.6. Variables Associated with PHQ-9 Scores over the Optimal Cut-Off Score
As presented in Table 4, a total PHQ-9 score over the optimal cut-off score (i.e., ≥5) was strongly associated with the experience of adversity during childhood. Compared to participants reporting no childhood adversity, those reporting one or two or more events of adversity were twice (OR 2.01, 95% CI 1.03–3.94) and five times (OR 5.25, 95% CI 1.93–14.34) more likely to score ≥ 5 in the PHQ-9, respectively. A PHQ-9 score ≥ 5 was also associated with length of residency, active debt, and the number of children. The odds of reporting a score above the cut-off were higher among those who had immigrated in the last three years (OR 1.79, 95% CI 1.07–3.00) versus those who had been residing in Chile for over three years, among those reporting active debt (OR 2.74, 95% CI 1.07–3.00) and among those with three or more children (OR 3.91, 95% CI 1.20–12.81).

Table 4.
Variables independently associated with PHQ-9 ≥ 5 with respective adjusted odds ratios, 95% confidence intervals, and p-values.
4. Discussion
The present study is the first to analyze the psychometric properties of the PHQ-9 and PHQ-2 in a representative sample of Spanish-speaking adult immigrants in Chile. Its results expand the evidence of the validity, reliability, and accuracy of both versions of the PHQ to a specific non-clinical population and contribute to the literature about the prevalence of depressive and anxiety symptoms and associated factors among economic immigrants.
Consistent with findings from available primary care studies in Chile [15,16,64,65], good internal consistency of the PHQ-9 in the overall sample and across immigrant groups was demonstrated. As expected [66], the correlation between the PHQ-9 with the GAD-7 was significant but moderate indicating convergent validity and supporting the growing body of literature about the coexistence and comorbidity of depression and anxiety [67,68].
Contrary to Latin American validation studies of the PHQ-9 among clinical [16,66,69] and non-clinical populations [17,19,20,21], which have demonstrated a good fit for both one- and two-factor solutions using confirmatory factor analysis, the goodness of fit indices for the three models tested in this study only indicate a plausible fit in the overall sample and in two of the four subsamples: Peruvians and Venezuelans. Some studies in the US have reported a poor fit of the PHQ-9 among Hispanic participants [70] but the pattern of a plausible fit across models in the overall sample and an inadequate fit in the Colombian and other Latin American subsamples observed in this study indicate the need to expand research about the structure of the Spanish version of the PHQ-9 among non-clinical populations in Latin America.
The PHQ-9 demonstrated high diagnostic accuracy and adequate sensibility and specificity values, comparable to those reported in studies conducted in clinical populations in Chile using the CIDI as a gold standard [15,16]. As expected of a screener for a low prevalence condition, it performed better at correctly identifying individuals without MDD than at confirming the presence of MDD, with negative (NPV) and positive (PPV) predictive values for scores between 5 and 10 in the range of 0.99–1.00 and 0.06–0.04, respectively. The low PPV suggests that rather than indicate a probable MDD diagnosis, a high PHQ-9 score should be regarded as an indication of the need for a more thorough evaluation.
The optimal PHQ-9 cut-off score for detecting MDD in the present study was ≥5. This score is lower than the original cut-off score (≥10) [6]. It is also lower than reported in a recent individual participant data meta-analysis (IPDMA) based on data from 100 studies which concluded that a cut-off score of ≥8 maximized combined sensitivity and specificity for fully structured reference standards [71]. However, the comparison of these values is limited considering the questionnaire was originally developed using data from primary care [6], and the number of studies from non-clinical samples included in the recent meta-analysis is low (15%) [71].
Across parameters and subsamples, the PHQ-9 demonstrated better performance than the PHQ-2: higher internal consistency, stronger convergent validity with the GAD-7, better accuracy with regard to a gold standard, and higher sensitivity and specificity for the proposed cut-off scores. However, taking into account the brevity of the PHQ-2 and in consistency with findings from studies among clinical [22] and non-clinical [21] populations in Latin America, results from this study suggest its performance is acceptable.
Findings from this study suggest that the prevalence of depressive symptoms and MDD among and across Spanish-speaking immigrant groups is lower than among the native population of Chile and other Spanish-speaking Latin American countries, independent of the assessment method used. Results from general population studies using structured clinical interviews in Chile [39,40,72], Colombia [5,42,43], and Peru [73] have consistently reported a higher prevalence of MDD than observed in the present study. Results from a general population study conducted in Chile using the PHQ-9 [23] also report a higher prevalence of MDD than reported in the current study. This lower risk for MDD represents a mental health advantage similar to that observed among first-generation immigrants from Latin America in the United States [74] and may partly be explained by their high labor force participation and low level of exposure to adversity during childhood.
Four factors predicted an increased risk of MDD among immigrants: the number of children (≤18 yrs), short length of residency in Chile (≤3 yrs), active debt, and exposure to childhood adversity. Contrary to evidence suggesting that an increase in the length of residency in the host country is associated with a higher risk of MDD among immigrants [75], the risk of MDD in this immigrant population was not predicted by a longer duration of residency. This lack of finding may be related to (i) the small proportion of participants who have been exposed to the prolonged effects of migration (only 12% have been residing in Chile for over 10 years), or (ii) the characteristics of the acculturation process shaped by high levels of cultural contiguity between Chile and other Latin American Spanish-speaking countries at the linguistic, religious, and ethnic level. Findings from this study support the well-established relationships between unsecured debt and mental health [76] and between adversity during childhood [77], having three or more children [78], and depression in adulthood.
Several limitations of this study should be acknowledged. First, the generalizability of the findings regarding the psychometric properties of both versions of the PHQ to non-native Spanish-speaking immigrants may be limited. Second, the generalizability regarding the prevalence of depressive symptoms and MDD and associated factors to non-economic migrants, migrants from high-income countries, from outside the Latin American region, or refugees may be limited because of differential exposure to stress throughout the migration process. Replication with more heterogeneous samples of immigrants such as individuals with a longer duration of residency in Chile, with clinical conditions, or service users is thus needed.
5. Conclusions
Findings from the present study indicate that both the PHQ-2 and PHQ-9 are psychometrically sound measures of depression for use among Spanish-speaking populations in Latin America. These results add to the evidence that they are brief, easy to use, and valid depression measures for use in clinical and non-clinical settings.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192113975/s1, Figure S1. Tested models of the Spanish version of PHQ-9; Table S1. Distribution of PHQ scores and 12 month-CIDI Major Depressive Disorder by immigrant group; Table S2. Internal consistency of the Chilean version of the PHQ-9 and PHQ-2 (n = 897); Table S3. Internal consistency of the Chilean version of the PHQ-9 by immigrant group; Table S4. Internal consistency of the Chilean version of the PHQ-2 by immigrant group; Table S5. Goodness of fit indices for PHQ-9 factor models by immigrant group; Table S6. Convergent validity coefficients of the PHQ-9 and PHQ-2 by immigrant group.
Author Contributions
Conceptualization, A.E.; Data curation, A.E.; Funding acquisition, A.E.; Methodology, A.E., R.B. and A.P.-S.; Project administration, A.E.; Supervision, A.E. and R.T.; Writing—original draft, A.E.; Writing—review and editing, A.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Agencia Nacional de Investigación y Desarrollo, grant number FONDECYT 11170828.
Institutional Review Board Statement
The study was approved by the Ethics Committee of the School of Medicine of the Pontificia Universidad Catolica de Chile on 10 January 2018 (No. 170519004).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study at the start of the interview.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kessler, R.C.; McGonagle, K.A.; Zhao, S.; Nelson, C.B.; Hughes, M.; Eshleman, S.; Wittchen, H.U.; Kendler, K.S. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch. Gen. Psychiatry 1994, 51, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.J.; Somerville, A.J.; Baxter, A.J.; Norman, R.; Patten, S.B.; Vos, T.; Whiteford, H.A. Global variation in the prevalence and incidence of major depressive disorder: A systematic review of the epidemiological literature. Psychol. Med. 2013, 43, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Hawton, K.; van Heeringen, K. Suicide. Lancet 2009, 373, 1372–1381. [Google Scholar] [CrossRef]
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Bromet, E.; Andrade, L.; Bruffaerts, R.; Williams, D. Major Depressive Disorder. In Mental Disorders around the World: Facts and Figures from the WHO World Mental Health Surveys; Scott, K.M., de Jonge, P., Stein, D.J., Kessler, R.C., Eds.; Cambridge University Press: Cambridge, UK, 2018; pp. 41–56. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Kroenke, K. Enhancing the clinical utility of depression screening. Can. Med. Assoc. J. 2012, 184, 281. [Google Scholar] [CrossRef]
- Gilbody, S.; Richards, D.; Brealey, S.; Hewitt, C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): A diagnostic meta-analysis. J. Gen. Intern. Med. 2007, 22, 1596–1602. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Vaze, A.; Rao, S. Clinical diagnosis of depression in primary care: A meta-analysis. Lancet 2009, 374, 609–619. [Google Scholar] [CrossRef]
- Diez-Quevedo, C.; Rangil, T.; Sanchez-Planell, L.; Kroenke, K.; Spitzer, R.L. Validation and Utility of the Patient Health Questionnaire in Diagnosing Mental Disorders in 1003 General Hospital Spanish Inpatients. Psychosom. Med. 2001, 63, 679–686. [Google Scholar] [CrossRef]
- Daray, F.M.; Hunter, F.; Anastasia, A.; Fornaro, M. Psychometric properties of the Patient Health Questionnaire nine-item version (PHQ-9) for use among hospitalized non-psychiatric medical patients. Gen. Hosp. Psychiatry 2019, 61, 69–75. [Google Scholar] [CrossRef]
- Urtasun, M.; Daray, F.M.; Teti, G.L.; Coppolillo, F.; Herlax, G.; Saba, G.; Rubinstein, A.; Araya, R.; Irazola, V. Validation and calibration of the patient health questionnaire (PHQ-9) in Argentina. BMC Psychiatry 2019, 19, 291. [Google Scholar] [CrossRef] [PubMed]
- Cassiani-Miranda, C.A.; Cuadros-Cruz, A.K.; Torres-Pinzón, H.; Scoppetta, O.; Pinzón-Tarrazona, J.H.; López-Fuentes, W.Y.; Paez, A.; Cabanzo-Arenas, D.F.; Ribero-Marulanda, S.; Llanes-Amaya, E.R. Validity of the Patient Health Questionnaire-9 (PHQ-9) for depression screening in adult primary care users in Bucaramanga, Colombia. Rev. Colomb. Psiquiatr. 2021, 50, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Calderón, M.; Gálvez-Buccollini, J.; Cueva, G.; Ordoñez, C.; Bromley, C.; Fiestas, F. Validation of the Peruvian version of the PHQ-9 for diagnosing depression. Rev. Peru. Med. Exp. Y Salud Pública 2012, 29, 578–579. [Google Scholar] [CrossRef] [PubMed]
- Saldivia, S.; Aslan, J.; Cova, F.; Vicente, B.; Inostroza, C.; Rincón, P. Propiedades psicométricas del PHQ-9 (Patient Health Questionnaire) en centros de atención primaria de Chile. Rev. Médica Chile 2019, 147, 53–60. [Google Scholar] [CrossRef]
- Aslan, J.; Cova, F.; Saldivia, S.; Bustos, C.; Inostroza, C.; Rincón, P.; Ortiz, C.; Bühring, V. Psychometric Properties of the Patient Health Questionnaire-9 in Elderly Chilean Primary Care Users. Front. Psychiatry 2020, 11, 555011. [Google Scholar] [CrossRef]
- Miranda, C.A.C.; Scoppetta, O. Factorial structure of the Patient Health Questionnaire-9 as a depression screening instrument for university students in Cartagena, Colombia. Psychiatry Res. 2018, 269, 425–429. [Google Scholar] [CrossRef]
- López-Guerra, V.M.; López-Núñez, C.; Vaca-Gallegos, S.L.; Torres-Carrión, P.V. Psychometric Properties and Factor Structure of the Patient Health Questionnaire-9 as a Screening Tool for Depression Among Ecuadorian College Students. Front. Psychol. 2022, 13, 813894. [Google Scholar] [CrossRef]
- Huarcaya-Victoria, J.; De-Lama-Morán, R.; Quiros, M.; Bazán, J.; López, K.; Lora, D. Propiedades psicométricas del Patient Health Questionnaire (PHQ-9) en estudiantes de medicina en Lima, Perú. Rev. Neuro-Psiquiatr. 2020, 83, 72–78. [Google Scholar] [CrossRef]
- Familiar, I.; Ortiz-Panozo, E.; Hall, B.; Vieitez, I.; Romieu, I.; Lopez-Ridaura, R.; Lajous, M. Factor structure of the Spanish version of the Patient Health Questionnaire-9 in Mexican women. Int. J. Methods Psychiatr. Res. 2015, 24, 74–82. [Google Scholar] [CrossRef]
- Arrieta, J.; Aguerrebere, M.; Raviola, G.; Flores, H.; Elliott, P.; Espinosa, A.; Reyes, A.; Ortiz-Panozo, E.; Rodriguez-Gutierrez, E.G.; Mukherjee, J.; et al. Validity and utility of the Patient Health Questionnaire (PHQ)-2 and PHQ-9 for screening and diagnosis of depression in rural Chiapas, Mexico: A cross-sectional study. J. Clin. Psychol. 2017, 73, 1076–1090. [Google Scholar] [CrossRef]
- Scoppetta, O.; Cassiani-Miranda, C.A.; Arocha-Díaz, K.N.; Cabanzo-Arenas, D.F.; Campo-Arias, A. Validity of the patient health questionnaire-2 (PHQ-2) for the detection of depression in primary care in Colombia. J. Affect. Disord. 2021, 278, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Caneo, C.; Toro, P.; Ferreccio, C. Validity and Performance of the Patient Health Questionnaire (PHQ-2) for Screening of Depression in a Rural Chilean Cohort. Community Ment. Health J. 2020, 56, 1284–1291. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estadísticas. Características Sociodemográficas de la Inmigración Internacional en Chile Censo 2017; Instituto Nacional de Estadísticas: Santiago, Chile, 2018. Available online: http://www.censo2017.cl/descargas/inmigracion/181126-sintesis.pdf (accessed on 26 October 2022).
- Salas-Wright, C.P.; Vaughn, M.G.; Goings, T.C.; Miller, D.P.; Schwartz, S.J. Immigrants and mental disorders in the united states: New evidence on the healthy migrant hypothesis. Psychiatry Res. 2018, 267, 438–445. [Google Scholar] [CrossRef]
- Edwards, J.; Hu, M.; Thind, A.; Stranges, S.; Chiu, M.; Anderson, K.K. Gaps in Understanding of the Epidemiology of Mood and Anxiety Disorders among Migrant Groups in Canada: A Systematic Review. Can. J. Psychiatry 2019, 64, 595–606. [Google Scholar] [CrossRef] [PubMed]
- Markkula, N.; Lehti, V.; Gissler, M.; Suvisaari, J. Incidence and prevalence of mental disorders among immigrants and native Finns: A register-based study. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 1523–1540. [Google Scholar] [CrossRef] [PubMed]
- De Wit, M.A.; Tuinebreijer, W.C.; Dekker, J.; Beekman, A.J.; Gorissen, W.H.; Schrier, A.C.; Penninx, B.W.; Komproe, I.H.; Verhoeff, A.P. Depressive and anxiety disorders in different ethnic groups: A population based study among native Dutch, and Turkish, Moroccan and Surinamese migrants in Amsterdam. Soc. Psychiatry Psychiatr. Epidemiol. 2008, 43, 905–912. [Google Scholar] [CrossRef]
- Bhugra, D. Migration and mental health. Acta Psychiatr. Scand. 2004, 109, 243–258. [Google Scholar] [CrossRef]
- Close, C.; Kouvonen, A.; Bosqui, T.; Patel, K.; O’Reilly, D.; Donnelly, M. The mental health and wellbeing of first generation migrants: A systematic-narrative review of reviews. Glob. Health 2016, 12, 47. [Google Scholar] [CrossRef]
- Blukacz, A.; Cabieses, B.; Markkula, N. Inequities in mental health and mental healthcare between international immigrants and locals in Chile: A narrative review. Int. J. Equity Health 2020, 19, 197. [Google Scholar] [CrossRef]
- Pettersson, H.V. Design of master sampling frames and master samples for household surveys in developing countries. In Household Sample Surveys in Developing and Transition Countries; Department of Economic and Social Affairs: New York, NY, USA, 2005. [Google Scholar]
- Instituto Nacional de Estadísticas (INE). Censo de Población y Vivienda 2017; Instituto Nacional de Estadísticas: Santiago, Chile, 2017. Available online: https://www.ine.cl/estadisticas/sociales/censos-de-poblacion-y-vivienda (accessed on 21 October 2022).
- Manea, L.; Gilbody, S.; McMillan, D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis. CMAJ 2012, 184, E191–E196. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef]
- García-Campayo, J.; Zamorano, E.; Ruiz, M.A.; Pardo, A.; Pérez-Páramo, M.; López-Gómez, V.; Freire, O.; Rejas, J. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual. Life Outcomes 2010, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Robins, L.N.; Wing, J.; Wittchen, H.U.; Helzer, J.E.; Babor, T.F.; Burke, J.; Farmer, A.; Jablenski, A.; Pickens, R.; Regier, D.A.; et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch. Gen. Psychiatry 1988, 45, 1069–1077. [Google Scholar] [CrossRef] [PubMed]
- Cía, A.H.; Stagnaro, J.C.; Aguilar Gaxiola, S.; Vommaro, H.; Loera, G.; Medina-Mora, M.E.; Sustas, S.; Benjet, C.; Kessler, R.C. Lifetime prevalence and age-of-onset of mental disorders in adults from the Argentinean Study of Mental Health Epidemiology. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud (MINSAL). Informe Encuesta Nacional de Salud 2016–2017. Salud Mental 1: Trastorno del ánimo: Depresión y Bipolaridad I y II; Ministerio de Salud: Santiago, Chile, 2018. Available online: http://epi.minsal.cl/wp-content/uploads/2021/08/Informe_Trastornos_del_Animo_ENS_2016_17.pdf (accessed on 21 October 2022).
- Vicente, B.; Kohn, R.; Rioseco, P.; Saldivia, S.; Levav, I.; Torres, S. Lifetime and 12-month prevalence of DSM-III-R disorders in the Chile psychiatric prevalence study. Am. J. Psychiatry 2006, 163, 1362–1370. [Google Scholar] [CrossRef]
- Gómez-Restrepo, C.; Bohórquez, A.; Pinto Masis, D.; Gil Laverde, J.F.; Rondón Sepúlveda, M.; Díaz-Granados, N. The prevalence of and factors associated with depression in Colombia. Rev. Panam. Salud Publica 2004, 16, 378–386. [Google Scholar] [CrossRef]
- Gómez-Restrepo, C.; Tamayo Martínez, N.; Bohórquez, A.; Rondón, M.; Medina Rico, M.; Rengifo, H.; Bautisa, N. Depression and Anxiety Disorders and Associated Factors in the Adult Colombian Population, 2015 National Mental Health Survey. Rev. Colomb. Psiquiatr. 2016, 45 (Suppl. 1), 58–67. [Google Scholar] [CrossRef]
- Posada-Villa, J.; Aguilar-Gaxiola, S.; Magaña, C.G.; Gómez, L.C. Prevalencia de trastornos mentales y uso de servicios: Resultados preliminares del Estudio Nacional de Salud Mental. Colombia, 2003. Rev. Colomb. Psiquiatr. 2004, 33, 241–262. [Google Scholar] [CrossRef]
- Torres de Galvis, Y.; Agudelo-Martínez, A.; Sierra-Hincapié, G.; Salas-Zapata, C. Prevalencia de trastornos mentales en población general del municipio de Itagüí (Colombia), 2012. CES Med. 2014, 28, 49–60. [Google Scholar]
- Torres de Galvis, Y.; Castaño Pérez, G.; Sierra Hincapié, G.; Salas Zapata, C.; Bareño Silva, J. Estudio de Salud Mental Medellín 2019; Editorial CES: Medellín, Colombia, 2020. [Google Scholar]
- Torres de Galvis, Y.; Restrepo Bernal, D.; Castaño Pérez, G.; Bareño Silva, J.; Sierra Hincapié, G.; Salas Zapata, C.; Buitrago Salazar, C. Estudio Poblacional de Salud Mental Sabaneta 2018; Editorial CES: Medellín, Colombia, 2018. [Google Scholar]
- Torres de Galvis, Y.; Restrepo, D.; Castaño, G.; Sierra, G.; Buitrago, C.; Carolina, C.; Bareño, J. Estudio Poblacional de Salud Mental Envigado 2017; Editorial CES: Medellín, Colombia, 2018. [Google Scholar]
- Puac-Polanco, V.; Lopez-Soto, V.; Kohn, R.; Xie, D.; Richmond, T.; Branas, C. Previous violent events and mental health outcomes in Guatemala. Am. J. Public Health 2015, 105, 764–771. [Google Scholar] [CrossRef]
- Andrade, L.; Caraveo-Anduaga, J.J.; Berglund, P.; Bijl, R.V.; De Graaf, R.; Vollebergh, W.; Dragomirecka, E.; Kohn, R.; Keller, M.; Kessler, R.C.; et al. The epidemiology of major depressive episodes: Results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int. J. Methods Psychiatr. Res. 2003, 12, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Salgado de Snyder, V.; Díaz-Pérez, M. Los trastornos afectivos en la población rural = Affective disorders in the rural population. Salud Ment. 1999, 22, 68–74. [Google Scholar]
- Slone, L.B.; Norris, F.H.; Murphy, A.D.; Baker, C.K.; Perilla, J.L.; Diaz, D.; Rodriguez, F.G.; Gutiérrez Rodriguez Jde, J. Epidemiology of major depression in four cities in Mexico. Depress. Anxiety 2006, 23, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Fiestas, F.; Piazza, M. Lifetime prevalence and age of onset of mental disorders in Peru: Results of the World Mental Health Study, 2005. Rev. Peru. Med. Exp. Salud Publica 2014, 31, 39–47. [Google Scholar]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Cronbach’s alpha. BMJ 1997, 314, 572. [Google Scholar] [CrossRef] [PubMed]
- Hinkle, D.E.; Wiersma, W.; Jurs, S.G. Applied Statistics for the Behavioral Sciences; Houghton Mifflin College Division: Boston, MA, USA, 2003; Volume 663. [Google Scholar]
- Krause, J.S.; Bombardier, C.; Carter, R.E. Assessment of depressive symptoms during inpatient rehabilitation for spinal cord injury: Is there an underlying somatic factor when using the PHQ? Rehabil. Psychol. 2008, 53, 513. [Google Scholar] [CrossRef]
- Richardson, E.J.; Richards, J.S. Factor structure of the PHQ-9 screen for depression across time since injury among persons with spinal cord injury. Rehabil. Psychol. 2008, 53, 243–249. [Google Scholar] [CrossRef]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef]
- Steiger, J.H. Structural Model Evaluation and Modification: An Interval Estimation Approach. Multivar. Behav. Res. 1990, 25, 173–180. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Mitchell, A.; Coyne, J. Screening for Depression in Clinical Practice: An Evidence-Based Guide; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013; Volume 398. [Google Scholar]
- Staples, L.G.; Dear, B.F.; Gandy, M.; Fogliati, V.; Fogliati, R.; Karin, E.; Nielssen, O.; Titov, N. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: The PHQ-2, GAD-2, and K-6. Gen. Hosp. Psychiatry 2019, 56, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Baader, M.T.; Molina, F.J.L.; Venezian, B.S.; Rojas, C.C.; Farías, S.R.; Fierro-Freixenet, C.; Backenstrass, M.; Mundt, C. Validación y utilidad de la encuesta PHQ-9 (Patient Health Questionnaire) en el diagnóstico de depresión en pacientes usuarios de atención primaria en Chile. Rev. Chil. Neuro-Psiquiatr. 2012, 50, 10–22. [Google Scholar] [CrossRef]
- Borghero, F.; Martínez, V.; Zitko, P.; Vöhringer, P.A.; Cavada, G.; Rojas, G. Tamizaje de episodio depresivo en adolescentes. Validación del instrumento PHQ-9. Rev. Médica Chile 2018, 146, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Quiñonez-Freire, C.; Vara, M.D.; Tomás, J.; Baños, R. Psychometric properties of the Spanish version of the Patient Health Questionnaire-9 in users of the Ecuadorian public health care system. Rev. Latinoam. Psicol. 2021, 53, 210–217. [Google Scholar] [CrossRef]
- Hirschfeld, R.M. The Comorbidity of Major Depression and Anxiety Disorders: Recognition and Management in Primary Care. Prim. Care Companion J. Clin. Psychiatry 2001, 3, 244–254. [Google Scholar] [CrossRef]
- Hanel, G.; Henningsen, P.; Herzog, W.; Sauer, N.; Schaefert, R.; Szecsenyi, J.; Löwe, B. Depression, anxiety, and somatoform disorders: Vague or distinct categories in primary care? Results from a large cross-sectional study. J. Psychosom. Res. 2009, 67, 189–197. [Google Scholar] [CrossRef]
- Smith, M.L.; Sanchez, S.E.; Rondon, M.; Gradus, J.L.; Gelaye, B. Validation of the Patient Health Questionnaire-9 (PHQ-9) for Detecting Depression Among Pregnant Women in Lima, Peru. Curr. Psychol. 2022, 41, 3797–3805. [Google Scholar] [CrossRef]
- Krause, J.S.; Saunders, L.L.; Bombardier, C.; Kalpakjian, C. Confirmatory Factor Analysis of the Patient Health Questionnaire-9: A Study of the Participants From the Spinal Cord Injury Model Systems. PMR 2011, 3, 533–540. [Google Scholar] [CrossRef]
- Negeri, Z.F.; Levis, B.; Sun, Y.; He, C.; Krishnan, A.; Wu, Y.; Bhandari, P.M.; Neupane, D.; Brehaut, E.; Benedetti, A.; et al. Accuracy of the Patient Health Questionnaire-9 for screening to detect major depression: Updated systematic review and individual participant data meta-analysis. BMJ 2021, 375, n2183. [Google Scholar] [CrossRef]
- Araya, R.; Rojas, G.; Fritsch, R.; Acuña, J.; Lewis, G. Common mental disorders in Santiago, Chile: Prevalence and socio-demographic correlates. Br. J. Psychiatry 2001, 178, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Piazza, M.; Fiestas, F. Annual prevalence of mental disorders and use of mental health services in Peru: Results of the World Mental Health Survey, 2005. Rev. Peru. Med. Exp. Salud Publica 2014, 31, 30–38. [Google Scholar] [PubMed]
- Alegría, M.; Álvarez, K.; DiMarzio, K. Immigration and Mental Health. Curr. Epidemiol. Rep. 2017, 4, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Ikonte, C.O.; Prigmore, H.L.; Dawson, A.Z.; Egede, L.E. Trends in prevalence of depression and serious psychological distress in United States immigrant and non-immigrant populations, 2010–2016. J. Affect. Disord. 2020, 274, 719–725. [Google Scholar] [CrossRef] [PubMed]
- Richardson, T.; Elliott, P.; Roberts, R. The relationship between personal unsecured debt and mental and physical health: A systematic review and meta-analysis. Clin. Psychol. Rev. 2013, 33, 1148–1162. [Google Scholar] [CrossRef]
- Nelson, J.; Klumparendt, A.; Doebler, P.; Ehring, T. Childhood maltreatment and characteristics of adult depression: Meta-analysis. Br. J. Psychiatry 2017, 210, 96–104. [Google Scholar] [CrossRef]
- Giannelis, A.; Palmos, A.; Hagenaars, S.P.; Breen, G.; Lewis, C.M.; Mutz, J. Examining the association between family status and depression in the UK Biobank. J. Affect. Disord. 2021, 279, 585–598. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).