Musculoskeletal Pain in Undergraduate Students Is Significantly Associated with Psychological Distress and Poor Sleep Quality
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Participants
2.2. Sample Size Calculation
2.3. Outcomes
2.4. Study Tools
2.4.1. Socio-Demographic Data
2.4.2. Musculoskeletal Pain Assessment
2.4.3. Sleep Quality Assessment
2.4.4. Psychological Distress Assessment
2.5. Statistical Analysis
3. Results
3.1. Demographics
3.2. Psychological Distress
3.3. Sleep Quality Assessment
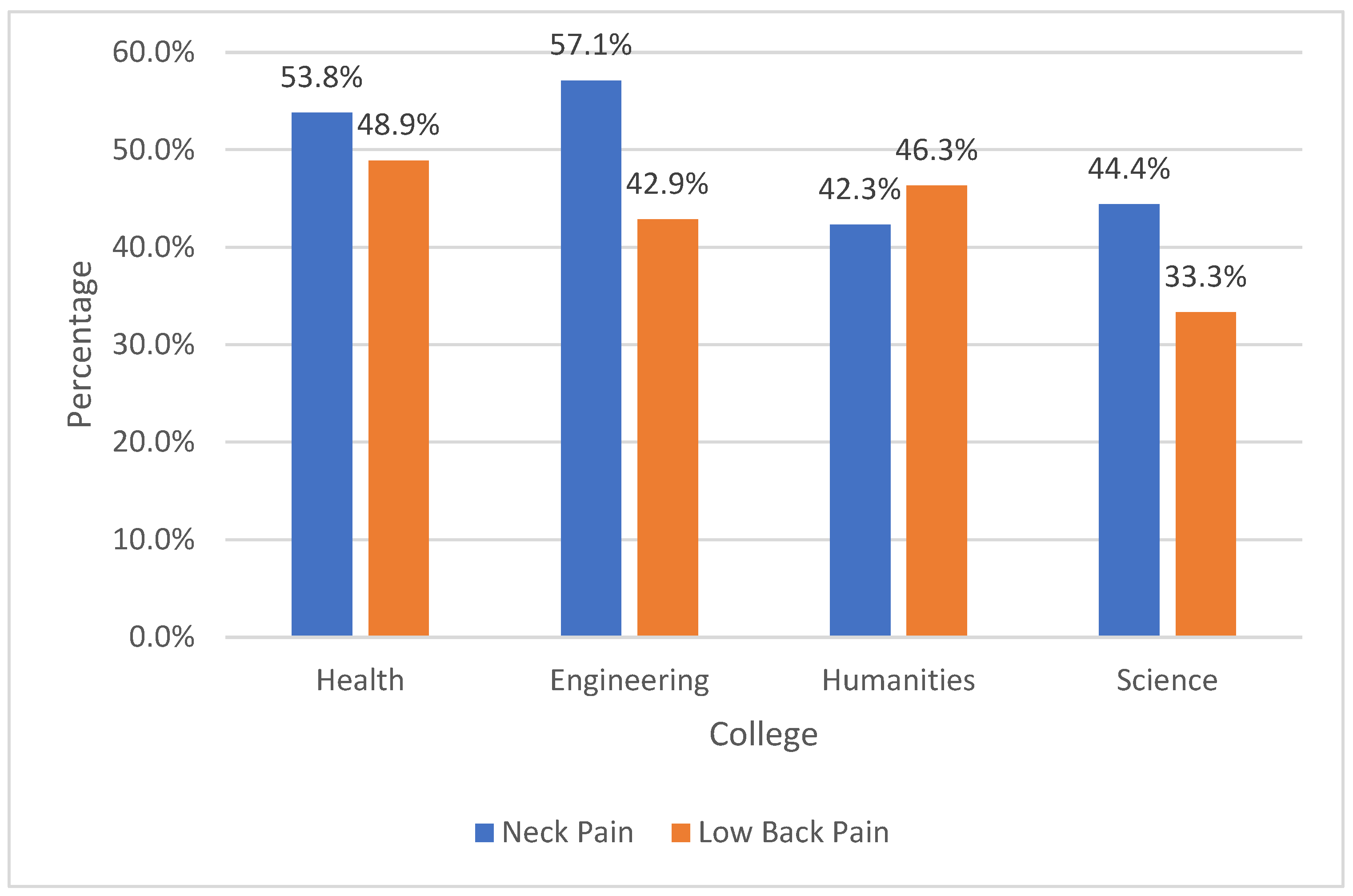
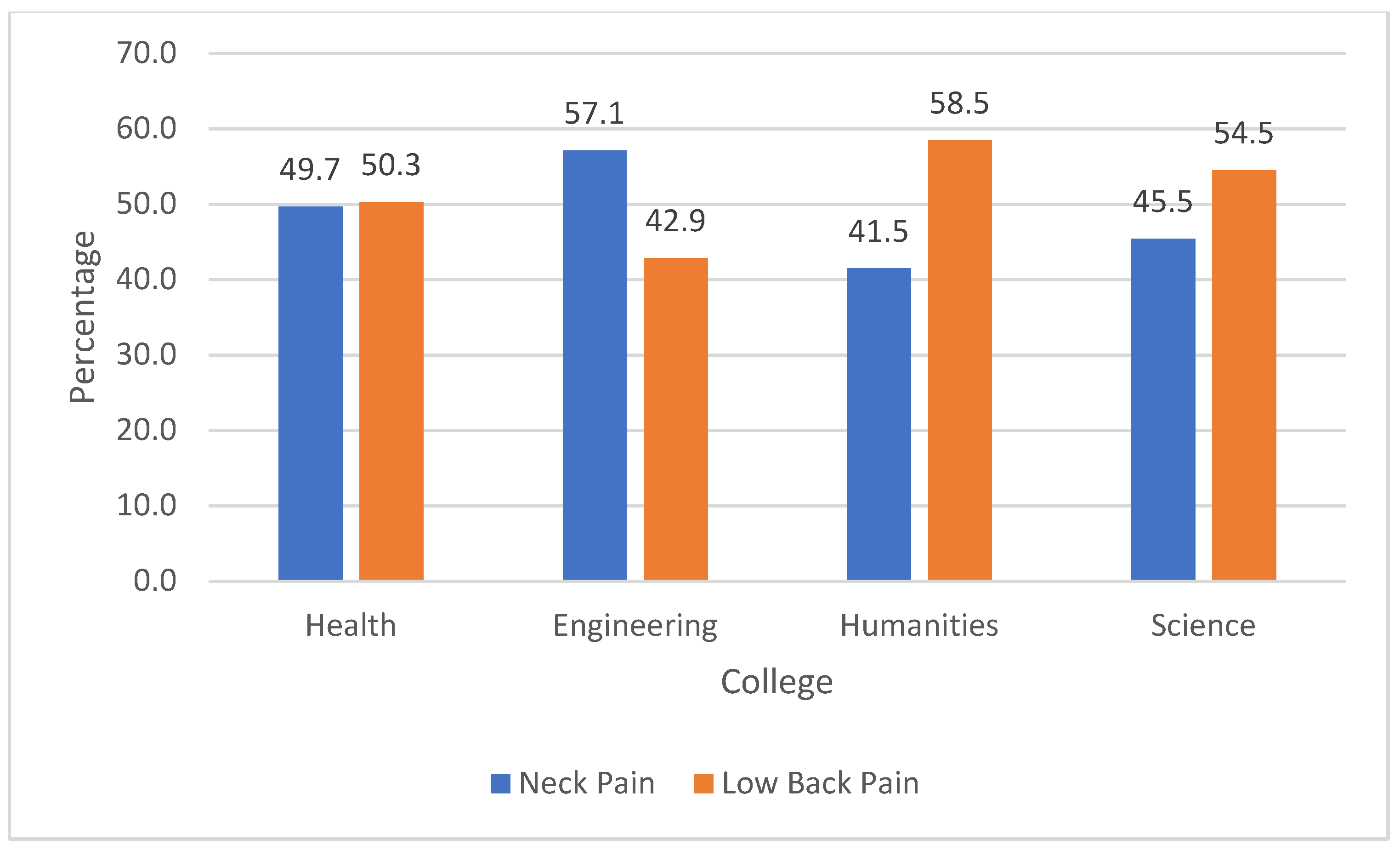
3.4. Musculoskeletal Pain Assessment
3.5. Association between Musculoskeletal Pain and Psychological Distress and Sleep Quality
4. Discussion
4.1. Study Implications
4.2. Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Prajapati, S.P.; Purohit, A. Prevalence of musculoskeletal disorder among college students in times of COVID-19 pandemic-an observational study. Int. J. Health Sci. Res. 2021, 11, 214–219. [Google Scholar] [CrossRef]
- Wohlmuth-Cohen, G.; León-Avila, F. Musculoskeletal pain in college students: A systematic review. Proc. Sci. Res. Univ. Anáhuac Multidiscip. J. Healthc. 2021, 1, 31–45. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef]
- Blyth, F.M.; Briggs, A.M.; Schneider, C.H.; Hoy, D.G.; March, L.M. The global burden of musculoskeletal pain—Where to from here? Am. J. Public Health 2019, 109, 35–40. [Google Scholar] [CrossRef]
- Castro, O.; Bennie, J.; Vergeer, I.; Bosselut, G.; Biddle, S.J.H. How sedentary are university students? A systematic review and meta-analysis. Prev. Sci. 2020, 21, 332–343. [Google Scholar] [CrossRef]
- Lubas, M.M.; Szklo-Coxe, M. A critical review of education-based sleep interventions for undergraduate students: Informing future directions in intervention development. Adolesc. Res. Rev. 2019, 4, 249–266. [Google Scholar] [CrossRef]
- Chun, M.Y.; Cho, B.J.; Yoo, S.H.; Oh, B.; Kang, J.S.; Yeon, C. Association between sleep duration and musculoskeletal pain: The Korea National Health and Nutrition Examination Survey 2010–2015. Medicine 2018, 97, e13656. [Google Scholar] [CrossRef]
- Ekpenyong, C.E.; Daniel, N.E.; Aribo, E. Associations between academic stressors, reaction to stress, coping strategies and musculoskeletal disorders among college students. Ethiop. J. Health Sci. 2013, 23, 98–112. [Google Scholar]
- Emmanouil, A.A.; Rousanoglou, E.N.; Boudolos, K.D. Neck, shoulder and low back musculoskeletal pain in Greek physical education university students: A series of three cross-sectional studies. J. Prev. Med. Care 2018, 2, 32–42. [Google Scholar] [CrossRef]
- Cuenca-Martínez, F.; Suso-Martí, L.; Herranz-Gómez, A.; Varangot-Reille, C.; Calatayud, J.; Romero-Palau, M.; Blanco-Díaz, M.; Salar-Andreu, C.; Casaña, J. Effectiveness of telematic behavioral techniques to manage anxiety, stress and depressive symptoms in patients with chronic musculoskeletal pain: A systematic review and meta-analysis. Int. J. Environ. Health Res. 2022, 19, 3231. [Google Scholar] [CrossRef]
- Yona, T.; Weisman, A.; Gottlieb, U.; Masharawi, Y. High levels of self-reported depressive symptoms among physical therapists and physical therapist students are associated with musculoskeletal pain: A cross-sectional study. Phys. Ther. 2022, 102, pzab278. [Google Scholar] [CrossRef] [PubMed]
- Alsaadi, S.M.; McAuley, J.H.; Hush, J.M.; Maher, C.G. Prevalence of sleep disturbance in patients with low back pain. Eur. Spine J. 2011, 20, 737–743. [Google Scholar] [CrossRef]
- Alsaadi, S.M.; McAuley, J.H.; Hush, J.M.; Lo, S.; Lin, C.W.C.; Williams, C.M.; Maher, C.G. Poor sleep quality is strongly associated with subsequent pain intensity in patients with acute low back pain. Arthritis Rheumatol. 2014, 66, 1388–1394. [Google Scholar] [CrossRef]
- Murillo, C.; Vo, T.T.; Vansteelandt, S.; Harrison, L.E.; Cagnie, B.; Coppieters, I.; Chys, M.; Timmers, I.; Meeus, M. How do psychologically based interventions for chronic musculoskeletal pain work? A systematic review and meta-analysis of specific moderators and mediators of treatment. Clin. Psychol. Rev. 2022, 94, 102160. [Google Scholar] [CrossRef]
- Chang, J.R.; Wang, X.; Lin, G.; Samartzis, D.; Pinto, S.M.; Wong, A.Y. Are changes in sleep quality/quantity or baseline sleep parameters related to changes in clinical outcomes in patients with nonspecific chronic low back pain? A systematic review. Clin. J. Pain 2022, 38, 292–307. [Google Scholar] [CrossRef]
- Darwish, M.A.; Al-Zuhair, S.Z. Musculoskeletal Pain Disorders among Secondary School Saudi Female Teachers. Pain Res. Treat. 2013, 2013, 878570. [Google Scholar] [CrossRef] [PubMed]
- Tantawy, S.A.; Rahman, A.A.; Ameer, M.A. The relationship between the development of musculoskeletal disorders, body mass index, and academic stress in Bahraini University students. Korean J. Pain 2017, 30, 126–133. [Google Scholar] [CrossRef]
- Suleiman, K.H.; Yates, B.C.; Berger, A.M.; Pozehl, B.; Meza, J. Translating the Pittsburgh Sleep Quality Index into Arabic. West. J. Nurs. Res. 2010, 32, 250–268. [Google Scholar] [CrossRef]
- Backhaus, J.; Junghanns, K.; Broocks, A.; Riemann, D.; Hohagen, F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J. Psychosom. Res. 2002, 53, 737–740. [Google Scholar] [CrossRef]
- Moussa, M.T.; Lovibond, P.; Laube, R.; Megahead, H.A. Psychometric Properties of an Arabic Version of the Depression Anxiety Stress Scales (DASS). Res. Soc. Work Pract. 2017, 27, 375–386. [Google Scholar] [CrossRef]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scales, 2nd ed.; Psychology Foundation: Sydney, Australia, 1995. [Google Scholar]
- Felemban, R.A.; Sofi, R.A.; Alhebshi, S.A.; Alharbi, S.G.; Farsi, N.J.; Abduljabbar, F.H.; Farsi, J.M.A. Prevalence and predictors of musculoskeletal pain among undergraduate students at a dental school in Saudi Arabia. Clin. Cosmet. Investig. Dent. 2021, 13, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Zafar, H.; Almosa, N. Prevalence of work-related musculoskeletal disorders among dental students of King Saud University, Riyadh, Kingdom of Saudi Arabia. J. Contemp. Dent. Pract. 2019, 20, 449–453. [Google Scholar] [PubMed]
- Kamal, A.M.; Ahmed, D.R.M.; Habib, S.F.K.; Al-Mohareb, R.A. Ergonomics of preclinical dental students and potential musculoskeletal disorders. J. Dent. Educ. 2020, 84, 1438–1446. [Google Scholar] [CrossRef] [PubMed]
- Cavallari, J.M.; Ahuja, M.; Dugan, A.G.; Meyer, J.D.; Simcox, N.; Wakai, S.; Garza, J.L. Differences in the prevalence of musculoskeletal symptoms among female and male custodians. Am. J. Ind. Med. 2016, 59, 841–852. [Google Scholar] [CrossRef]
- Hendi, O.M.; Alturkistani, L.H.; Bajaber, A.S.; Alhamoud, M.A.; Mahmoud Mahfouz, M.E. Prevalence of musculoskeletal disorder and its relation to stress among medical student at Taif University, Saudi Arabia. Int. J. Prev. Med. 2021, 12, 98. [Google Scholar]
- Malmborg, J.S.; Bremander, A.; Olsson, M.C.; Bergman, A.C.; Brorsson, A.S.; Bergman, S. Worse health status, sleeping problems, and anxiety in 16-year-old students are associated with chronic musculoskeletal pain at three-year follow-up. BMC Public Health 2019, 19, 1565. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sport. Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Andersen, J.H.; Haahr, J.P.; Frost, P. Risk factors for more severe regional musculoskeletal symptoms: A two-year prospective study of a general working population. Arthritis Rheumatol. 2007, 56, 1355–1364. [Google Scholar] [CrossRef]
- Jaracz, J.; Gattner, K.; Jaracz, K.; Górna, K. Unexplained Painful physical symptoms in patients with major depressive disorder: Prevalence, pathophysiology and management. CNS Drugs 2016, 30, 293–304. [Google Scholar] [CrossRef]
- IsHak, W.W.; Wen, R.Y.; Naghdechi, L.; Vanle, B.; Dang, J.; Knosp, M.; Dascal, J.; Marcia, L.; Gohar, Y.; Eskander, L.; et al. Pain and depression: A systematic review. Harv. Rev. Psychiatry 2018, 26, 352–363. [Google Scholar] [CrossRef]
- Michaelides, A.; Zis, P. Depression, anxiety and acute pain: Links and management challenges. Postgrad. Med. 2019, 26, 438–444. [Google Scholar] [CrossRef]
- Serbic, D.; Friedrich, C.; Murray, R. Psychological, social and academic functioning in university students with chronic pain: A systematic review. J. Am. Coll. Health, 2021; 1–15. [Google Scholar]
- Mehmood, M.; Yaqoob, U.; Ali, S.; Siddiqui, A. Freuency of musculoskeletal pain and associated factors among undergraduate students. Case Rep. Clin. Med. 2018, 7, 131–145. [Google Scholar]
- Auvinen, J.P.; Tammelin, T.H.; Taimela, S.P.; Zitting, P.J.; Järvelin, M.-R.; Taanila, A.M.; Karppinen, J.I. Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. Eur. Spine J. 2010, 19, 641–649. [Google Scholar] [CrossRef]
- Uyar, K.; Gündoğan, R.; Gürbüz, Ö.B.; Ozcakar, N. Status of fatigue and sleep quality in clinical medical students. Marmara Med. J. 2016, 29, 164–169. [Google Scholar] [CrossRef]
- King, N.B.; Fraser, V. Untreated pain, narcotics regulation, and global health ideologies. PLoS Med. 2013, 10, e1001411. [Google Scholar] [CrossRef]
- Morais, B.X.; Dalmolin, G.L.; Andolhe, R.; Dullius, A.; Rocha, L.P. Musculoskeletal pain in undergraduate health students: Prevalence and associated factors. Rev. Esc. Enferm. USP 2019, 53, e03444. [Google Scholar] [CrossRef]
- Alsalameh, A.M.; Harisi, M.J.; Alduayji, M.A.; Almutham, A.A.; Mahmood, F.M. Evaluating the relationship between smartphone addiction/overuse and musculoskeletal pain among medical students at Qassim University. J. Fam. Med. Prim. Care 2019, 8, 2953–2959. [Google Scholar] [CrossRef]
| Demographic | n |
|---|---|
| Age (years) (mean ± SD) | 21 (±1.7) |
| Gender (Female) | 279 (82%) |
| BMI (kg/m2) (mean ± SD) | 22.3 (±4.6) |
| Caffeine intake (cup/day) (mean ± SD) | 1.0 (±0.89) |
| Smoker | |
| Yes | 37 (11%) |
| No | 302 (89%) |
| Marital status | |
| Single | 300 (88.5%) |
| Married | 39 (11.5%) |
| Divorced/Widowed | 0 |
| Live alone (No) | 311 (91.7%) |
| Specialty | |
| Health | 182 (54%) |
| Humanitarian | 123 (36%) |
| Science | 27 (8%) |
| Engineering | 7 (2%) |
| GPA (0–5) | |
| Fair | 5 (1.5%) |
| Good | 149 (44.2%) |
| Very good | 115 (34.1%) |
| Excellent | 68 (20.2%) |
| Parameter | Mean ± SD |
|---|---|
| Psychological distress | |
| Depression | 13.4 ± 10.4 |
| Anxiety | 11.1 ± 8.8 |
| Stress | 14.9 ± 10.4 |
| Sleep quality (PSQI score) | 8.8 ± 3.1 |
| Pain Area | During the Past 12 Months n (%) | During the Past 7 Days n (%) | Preventing Function n (%) | Seeing Physician for Pain n (%) |
|---|---|---|---|---|
| Neck | 185 (54.6) | 142 (41.9) | 51 (16.1) | 18 (5.6) |
| shoulders | 143 (44.7) | 120 (368) | 54 (17.1) | 23 (7.3) |
| Upper back | 113 (35.5) | 98 (30.2) | 52 (16.6) | 24 (7.5) |
| Elbow | 24 (7.6) | 32 (9.9) | 24 (7.6) | 19 (6.0) |
| Wrist/hands | 67 (21.2) | 61 (18.8) | 41 (12.9) | 18 (5.7) |
| Lower back | 158 (49.4) | 163 (48.2) | 73 (22.7) | 32 (10.1) |
| Hip/thigh | 65 (20.4) | 59 (18.2) | 36 (11.4) | 23 (7.3) |
| knees | 68 (21.2) | 71 (21.8) | 35 (11.0) | 24 (7.5) |
| Ankle/feet | 77 (24.1) | 69 (21.2) | 43 (13.5) | 32 (10.1) |
| Variable | MSK Pain | Statistic Test | p-Value | |
|---|---|---|---|---|
| Yes | No | |||
| Gender | ||||
| Male | 28 | 32 | 0.04 | 0.83 |
| Female | 126 | 153 | ||
| Smoke | ||||
| Yes | 22 | 14 | 2.23 | 0.13 |
| No | 136 | 148 | ||
| College | ||||
| Health | 89 | 89 | ||
| Humanities | 57 | 52 | ||
| Science | 18 | 9 | 3.1 | 0.36 |
| Engineering | 3 | 3 | ||
| GPA | ||||
| Fair | 1 | 4 | ||
| Good | 72 | 68 | ||
| Very good | 54 | 58 | 2 | 0.56 |
| Excellent | 31 | 32 | ||
| Caffeine intake (cup/day) | ||||
| 0 | 44 | 57 | ||
| 1–2 | 79 | 67 | ||
| 3–4 | 24 | 21 | 6.96 | 0.13 |
| >4 | 8 | 15 | ||
| Statistic test | p-value | |||
| Age | 0.06 | 0.42 | ||
| Depression | 0.01 | 0.49 | ||
| Anxiety | 0.05 | 0.002 | ||
| Stress | 0.03 | 0.03 | ||
| Sleep Quality | 0.1 | 0.04 | ||
| Variable | MSK Pain | Statistic Test | p-Value | |
|---|---|---|---|---|
| Yes | No | |||
| Gender | 0.29 | 0.58 | ||
| Male | 36 | 23 | ||
| Female | 159 | 119 | ||
| Smoke | 2.1 | 0.14 | ||
| Yes | 22 | 15 | ||
| No | 141 | 160 | ||
| College | 0.72 | 0.86 | ||
| Health | 85 | 96 | ||
| Humanities | 62 | 61 | ||
| Science | 12 | 15 | ||
| Engineering | 4 | 3 | ||
| GPA | 5.12 | 0.16 | ||
| Fair | 1 | 4 | ||
| Good | 75 | 74 | ||
| Very good | 49 | 67 | ||
| Excellent | 38 | 30 | ||
| Caffeine intake (cup/day) | 5.06 | 0.28 | ||
| 0 | 48 | 54 | ||
| 1–2 | 78 | 80 | ||
| 3–4 | 24 | 23 | ||
| >4 | 2 | 17 | ||
| Statistic test | p-value | |||
| Age | 0.09 | 0.15 | ||
| Depression | 0.03 | 0.004 | ||
| Anxiety | 0.05 | <0.001 | ||
| Stress | 0.05 | <0.001 | ||
| Sleep Quality | 0.03 | <0.001 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsaadi, S.M. Musculoskeletal Pain in Undergraduate Students Is Significantly Associated with Psychological Distress and Poor Sleep Quality. Int. J. Environ. Res. Public Health 2022, 19, 13929. https://doi.org/10.3390/ijerph192113929
Alsaadi SM. Musculoskeletal Pain in Undergraduate Students Is Significantly Associated with Psychological Distress and Poor Sleep Quality. International Journal of Environmental Research and Public Health. 2022; 19(21):13929. https://doi.org/10.3390/ijerph192113929
Chicago/Turabian StyleAlsaadi, Saad M. 2022. "Musculoskeletal Pain in Undergraduate Students Is Significantly Associated with Psychological Distress and Poor Sleep Quality" International Journal of Environmental Research and Public Health 19, no. 21: 13929. https://doi.org/10.3390/ijerph192113929
APA StyleAlsaadi, S. M. (2022). Musculoskeletal Pain in Undergraduate Students Is Significantly Associated with Psychological Distress and Poor Sleep Quality. International Journal of Environmental Research and Public Health, 19(21), 13929. https://doi.org/10.3390/ijerph192113929





