Abstract
We develop a protocol for assessing the impact of an intervention aimed at improving sleep quality among university nursing students. The study is designed as a pilot randomized controlled trial to be applied during the 2022-23 academic year and is registered at Clinical Trials Gov website (NCT05273086). A total of 60 nursing students will be recruited from a Spanish university. They will be divided into two groups: (30) intervention group and (30) control group. The intervention group will attend two cognitive–behavioural therapy sleep programme sessions focused on knowledge of anatomical structures involved in sleep, chronotype, synchronization, and good sleeping habits. Subjective and objective sleep quality will be assessed before and after the intervention for both groups. In addition to sleep quality, socio-demographic parameters, physical activity, lifestyle habits, and anthropometric measures will be considered prior to intervention. Finally, a satisfaction questionnaire will be applied for posterior analysis. This study is an innovative, relevant intervention that aims to improve sleep quality among university nursing students. Both the approach and the use of objective and subjective validated outcome measurements are key features of this study.
Keywords:
nursing students; sleep quality; sleep hygiene; nursing; health education; programme; intervention 1. Introduction
Sleep has been defined as an essential brain state for maintaining energy and restoring bodily function [1]. Sleep quality has a huge impact on health [2], and it is considered a leading public health problem [3]. Although there has been interest in sleep quality in different disciplines such as nursing, medicine, and psychology, it has not yet been clearly defined from a neurophysiological point of view. The concept analysis by Nelson et al. [4] shows that sleep quality is determined by five components: (1) sleep efficiency, total sleep time-total time in bed ratio; (2) sleep disturbance; (3) sleep latency, defined as the time taken to pass from wakefulness to sleep; (4) sleep duration in 24 h; (5) and waking after sleep onset, or in other words, the total time awake from sleep onset to finally waking up.
Good sleep quality is a predictor of physical and mental health, well-being, and overall vitality [5]. However, poor sleep quality, determined by a negative subjective perception of sleep, sleep onset times, short sleep duration, and difficulties combining sleep and daytime activity [6], has been related to psychiatric disorders such as depression, anxiety, and cognitive difficulties, with reduced physical health, premature ageing, and lower efficiency at work [7].
University students are one of the population groups that suffer most sleep-related problems. Both lack of sleep and sleep disorders are the main characteristics involved in low sleep quality among university students [8]. Over time, it has been noted that the weekly sleep pattern of this group is determined by few hours sleeping during the week and recovering sleeping hours at the weekend [7,9]. This deregulation causes them to experience delayed sleep phase syndrome [10], which is characterised by difficulty falling asleep at a socially acceptable time of night and inability to wake easily in the morning [11]. This syndrome has been related to poor academic performance, behavioural, emotional, and psychological problems, as well as increased drug and alcohol consumption [12].
Nursing students face complex situations that can specifically affect their sleep quality [13]. Different factors have been identified as limiting the quality of sleep of this group, especially during the first year of professional training [14]. There were individual psychosocial factors [15,16,17], regarding the academic area and professional environment where they describe the possibility of making mistakes in care practice and handling equipment, as well as lack of knowledge and professional skills [18].
Several studies have implemented intervention programmes to improve sleep quality among the adult population without resorting to the use of drugs [19]. However, the published literature among the university student population with no prior sleep-related pathologies is scarce, despite the fact that they are considered a high-risk group. To the best of our knowledge, only one systematic review [20] and a meta-analysis [21] that address interventions to improve sleep in university students have been published so far. The latter includes 14 studies, of which six were conducted with university students and the rest with young students and adolescents.
Many interventions in both the general population and university and adolescent populations focus on treating insomnia and mental health problems such as anxiety and depression. These works have a practical approach to sleep quality, but they do not take into account fundamental elements such as circadian rhythms, motor activity, skin temperature, sleep phases and position in 24 hours, which are key to understanding sleep quality and being able to improve it [22,23,24].
Interventions to improve sleep quality generally have several fundamental cornerstones. First, students are unaware of how sleep deprivation or disturbance affects cognitive functioning [10]. This justifies educational interventions to understand how the brain regulates sleep function. Despite some studies suggesting that people suffering insomnia who receive theoretical sleep training can significantly improve sleep quality [25], the relationship between knowledge and better sleep quality is unclear [10]. Thus, interventions should have a multi-factor approach including different elements that provide attendees with tools to improve their sleep.
Several studies indicate that cognitive-behavioural therapy yields positive results in this type of intervention [26] as it involves improving sleep by modifying mindset and behaviour patterns. Therapy has different types of treatment that can be used individually or in combination, such as relaxation, stimulus control, restricting sleep and sleep hygiene [27]. Cognitive–behavioural therapy has a multi-component nature, so it can be used to improve health in relation to sleep quality when there is no associated pathology [20]. This is the case of specific sleep hygiene and stimulus control techniques related to sleep [26] which focus on health. Sleep hygiene appears to be a key factor in these interventions as it addresses a series of behavioural and environmental recommendations aimed at promoting healthy sleep from a psychoeducational perspective. During education on sleep hygiene, users learn about healthy sleep habits, which is a first-line intervention for promoting sleep health [26,28].
Assessing interventions to improve sleep quality is another issue that needs to be addressed. The complex nature of the construct requires the use of objective (external and metric assessment) and subjective (perception of sleep quality) aspects in its assessment. Polysomnography and actigraphy are two different methods used to measure sleep quality [4]. For a subjective sleep assessment, the Pittsburgh Sleep Quality Index, PSQI [20] is typically used. Polysomnography is the gold standard method [29], but its use is limited due to difficult availability and home monitoring, combined with the lack of other validated outpatient tools that can replace this test [30]. Studies often use actigraphy to assess sleep [21] because it has proven to be sensitive in its measurement, but again it is of limited use for certain parameters, such as wakefulness during the night. This means that it is not a complete measure for assessing sleep quality and cannot be considered validated like polysomnography [24]. There are no studies using both measures as complementary measures to obtain data on sleep quality in adults [19], and more specifically in young people and adolescents [26]. In fact, most of the systematic review studies mentioned above use PSQI or actigraphy, translating the results into total hours of sleep [20,21]. This leads to a partial and biased assessment of how these interventions affect sleep quality.
Lastly, despite numerous studies analysing the factors associated with poor sleep quality in nursing students [7,31], no intervention study was found in the literature to design, implement, and assess an interventional programme to improve sleep quality in this group.
The aim of this study is to develop a protocol for assessing the impact of an intervention aimed at improving sleep quality among nursing university students.
2. Materials and Methods
The study protocol is based on a randomized controlled trial. Participants will be randomly assigned to a control and an intervention group. Only participants in the latter group will receive the intervention based on two cognitive–behavioural therapy sleep programme sessions.
2.1. Hypotheses
We pose the conceptual hypothesis that participants in the intervention group will improve their sleep quality, measured by objective monitoring parameters, and their subjective perception.
2.2. Design
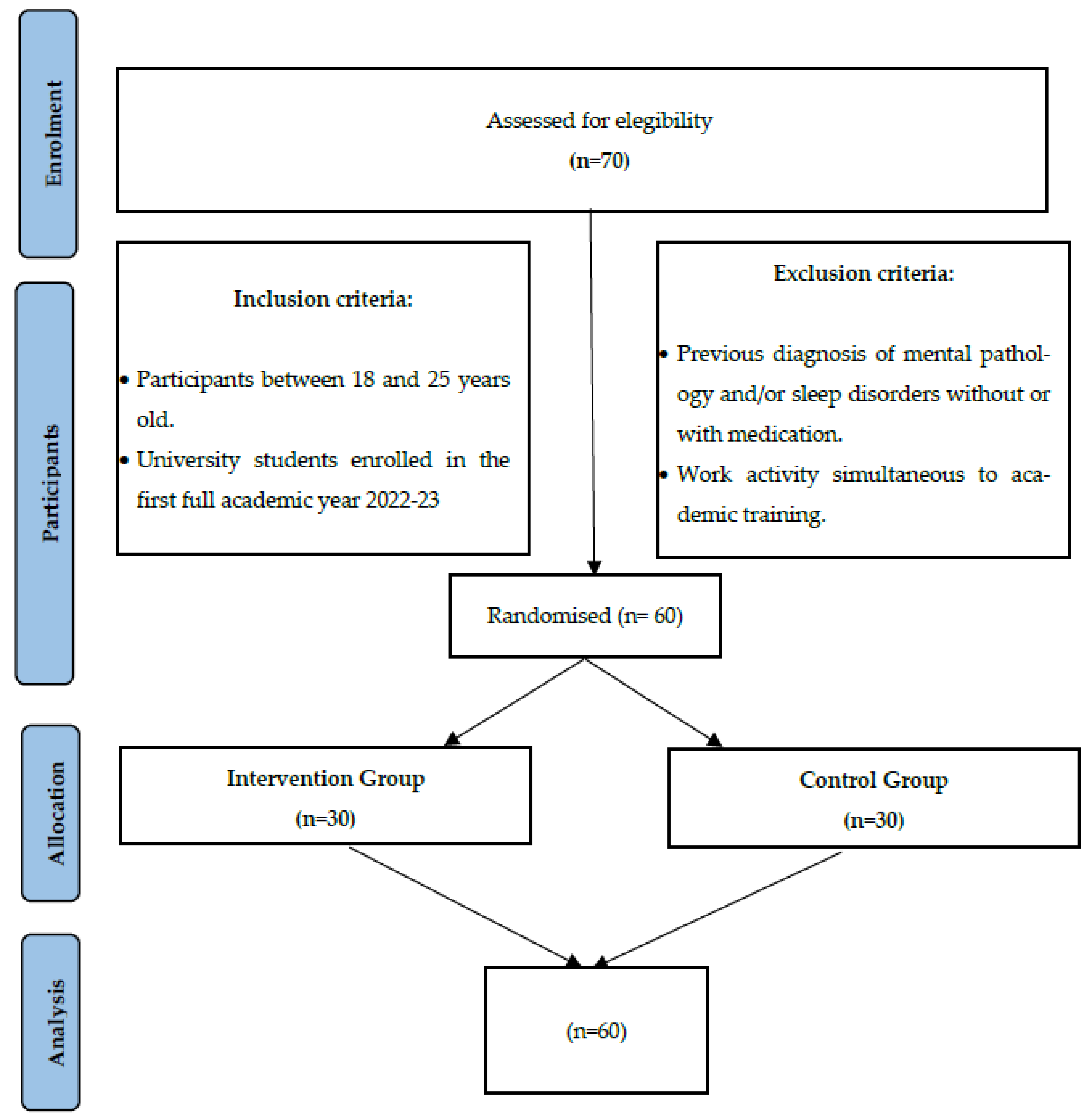
The study will be conducted at a Spanish university as a two-arm pilot randomized clinical trial (intervention and control). It will be single-centre and single-blind (data analysts), comparing two conditions: the intervention group (IG), with a specific intervention on sleep quality, and the control group (CG), with no intervention. Figure 1 shows the study flow chart. The random clinical trial report will follow the recommendations for interventional trials (SPIRIT) [32]. This protocol is registered at ClinicalTrials.gov (accessed on 15 September 2022) with reference number NCT05273086.
Figure 1.
Participant’s flowchart diagram.
2.3. Sample/Participants
The study will be conducted at a university in Madrid (Spain). The intervention environment will be exclusively affecting undergraduate students during the first term of the 2022-23 academic year (October 2022–February 2023).
2.3.1. Inclusion Criteria
- Students aged 18 to 25 years.
- Students enrolled in their first full year of a nursing degree, 2022-23.
2.3.2. Exclusion Criteria
- Prior mental pathology and/or sleep disorder diagnosis with or without medication (hypnotics, sedatives, and melatonin).
- Participants that use any drugs to sleep.
- Combining work and studying.
2.3.3. Sample Size Calculation
For a population size of 70, at least 60 samples are required to have a confidence level of 95% so that the real value is within ±5% of the measured/surveyed value. For two-group comparisons, at least 60 samples are required for an expected medium effect [33].
2.3.4. Randomization
An independent researcher who is unaware of the study characteristics will conduct the random assignment procedure. A computer-generated random number sequence (Sealed Envelope™ software version 1.21.0, London, UK), assigned to participants’ academic record number will be used to randomly designate participants to one of the two groups (IG or CG). Random permuted blocks will also be used to reduce the random sequence predictability and guarantee a 1:1 ratio. This sequence will be password-protected in a table and will be hidden from other researchers during the study.
2.3.5. Blinding Design
The study design does not allow the treatment assignment to be blind for the sleep experts facilitating the intervention and the participants. However, analysts will be blinded to the group-assigned treatment. To prevent interobserver variability bias, measurements will be taken by the same researcher in all cases.
2.4. Intervention
The intervention group will receive the programme sessions based on knowledge and cognitive–behavioural therapy to improve sleep quality, and the control group participants will continue with their normal routine. This programme will be developed with an active-constructive learning methodology in which students interact with the material so that their commitment to learning generates deeper knowledge [34]. For this reason, the intervention group will be subdivided into two groups of 10 participants. Reducing the group numbers in this way will enable greater participation and skills acquisition to improve sleep quality. This includes acquiring notions of chronobiology; locating nervous structures involved in biological rhythms, awareness of the existence of biological and social stimulus that determine human circadian rhythms and the importance of their synchronization, self-awareness of the chronotype; knowledge of variables that determine good sleep quality, knowledge of one’s own sleep pattern, routines that improve sleep quality, and resources to avoid variables that are detrimental to sleep quality.
The intervention will consist of face-to-face 90-min group sessions executed twice a week during November and December 2022. Each session will be divided into four parts focused on different aspects related to sleep quality. The first session will focus on knowledge of anatomical structures involved in sleep and their effect at a cognitive level. Students may also self-assess their sleep pattern so that strategies can be adapted to improve this pattern at the next session. The second session will focus on developing skills for better sleep hygiene, working on the students’ individual sleep routines and the results of their questionnaires and self-reports so that the elements of sleep hygiene can be adapted to each case. Table 1 specifies the objectives, session activities, required materials, and duration of the intervention.

Table 1.
Distribution of the sessions of the sleep quality programme for nursing students.
The experts implementing the intervention will be a PhD candidate in biology specialized in the brain function of sleep, chronobiology, and circadian rhythms, and a registered nurse expert in health promotion and in healthy lifestyles education, who will conduct the particular part of the sessions related to sleep hygiene and nocturnal habits.
2.5. Data Collection
The assessment process will include self-assessment questionnaires in which participants must answer questions on their perception related to sleep quality, socio-demographic aspects and lifestyle.
2.5.1. Dependent Variables
- Sleep quality: Kronowise 3.0, Kronohealth, S.L., Spain. Kronowise 3.0 is a wrist device that conducts ambulatory circadian monitoring (ACM) based on thermometry, motor activity, and body position (TAP). TAP uses a combination of sensors in an algorithm that has been validated as ambulatory polysomnography. It was validated by comparing the assessment of these parameters with polysomnography in adults [35] and in patients diagnosed with Parkinson’s [36]. The device can measure sleep quality and circadian rhythms and identify circadian chronodisruption through parameters such as sleep latency, total sleep time (in minutes), sleep efficiency, number of awakenings and time between waking and sleep [35]. It can also identify sleep phases, nocturnal awakenings, temperature, exposure to infrared and blue light as well as other parameters such as time in bed, sleep onset, awake time, sleep interval, total time in movement, time in movement index, sleep acceleration index, wrist sleep temperature, napping time and napping frequency [36]. Participants will wear the device for seven consecutive days, including weekdays and weekends. Both groups will be measured twice (before and after the intervention), meaning that all participants will wear the device for a total of 14 days. Participants will be given appointments to fit and remove the devices. Information provided by the devices will be entered into the software that will be sent to Kronohealth S.L., Spain, which will produce reports of both measurements with the results of the parameters mentioned above, with the sleep quality indices established according to the device validation [35].
- Perceived sleep quality: Pittsburgh Sleep Quality Index, PSQI [37]. The PSQI contains 19 items and seven clinically important components related to sleep quality: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Responses will be reported based on a Likert-type scale from 0 to 4. Overall sleep scores of 5 or less will be considered good quality, whereas scores of 5 or more will be considered low quality. The PSQI version that will be used is validated into the Spanish university framework by De la Vega et al. [37] with a Cronbach’s alpha of 0.72. The questionnaire will be given to all participants twice (before and immediately following the intervention).
2.5.2. Independent Variables
All independent variables will be assessed before the intervention, except for the intervention group’s satisfaction questionnaire, which will be measured immediately afterward. Questionnaires on socio-demographic data and toxic habits are prepared ad hoc by the researchers.
- Socio-demographic data: Date of birth, age in years, gender and sleep habits during the study (alone or accompanied).
- Toxic habits: Tobacco consumption (cigarettes/day), alcohol consumption (daily, weekly, sporadic, glasses), drug consumption (yes/no and type), and stimulating drink consumption (coffee, sugary drinks, energy drinks).
- Physical exercise: The International Physical Activity Questionnaire (IPAQ), simplified version [38]. The questionnaire consists of seven questions on frequency, duration and intensity of activity (moderate and intense) in the last seven days, as well as walking and sitting time during a working day. The questionnaire is classified into the following levels: low, moderate, and high physical activity. The higher the score, the more physically active the profile. The questionnaire is validated with a mean reliability of 0.80 [38].
- Anthropometric variables: Participants will report their weight (kg) and height (cm).
- Satisfaction with the programme: Using a questionnaire adapted to the proposal by Azpeleta et al. [39] with 10 questions and responses based on a Likert-type scale from 1 to 10. Greater satisfaction will be awarded a higher score.
Table 2 shows the data collection and monitoring instruments.

Table 2.
Data collection and follow-up instruments.
2.6. Ethical Considerations
This study will be conducted according to the principles established in the Declaration of Helsinki, in the Convention on Human Rights and Biomedicine (Oviedo Convention), and in the UNESCO Universal Declaration on the Human Genome and Human Rights. This study has been approved by the Research Ethics Committee of Camilo José Cela University (code: 06-22-UCJC-Sleep).
All participants will be informed of the duration and characteristics of the study, and of its voluntary nature. After receiving a detailed explanation of the project, any doubts raised by participants will be answered before the students are asked to sign the informed consent form, which mandatorily must be signed to participate.
Participants may abandon the study at any time, with no further consequences. The highest professional conduct and absolute confidentiality will be always maintained, in accordance with European Regulation (EU) 2016/679 on the protection of natural persons and data processing and free movement, the Framework Act 3/2018 on personal data protection and the guarantee of digital rights, and Act 14/2007 on biomedical research. Only the principal researcher of the project will have access to the codified database.
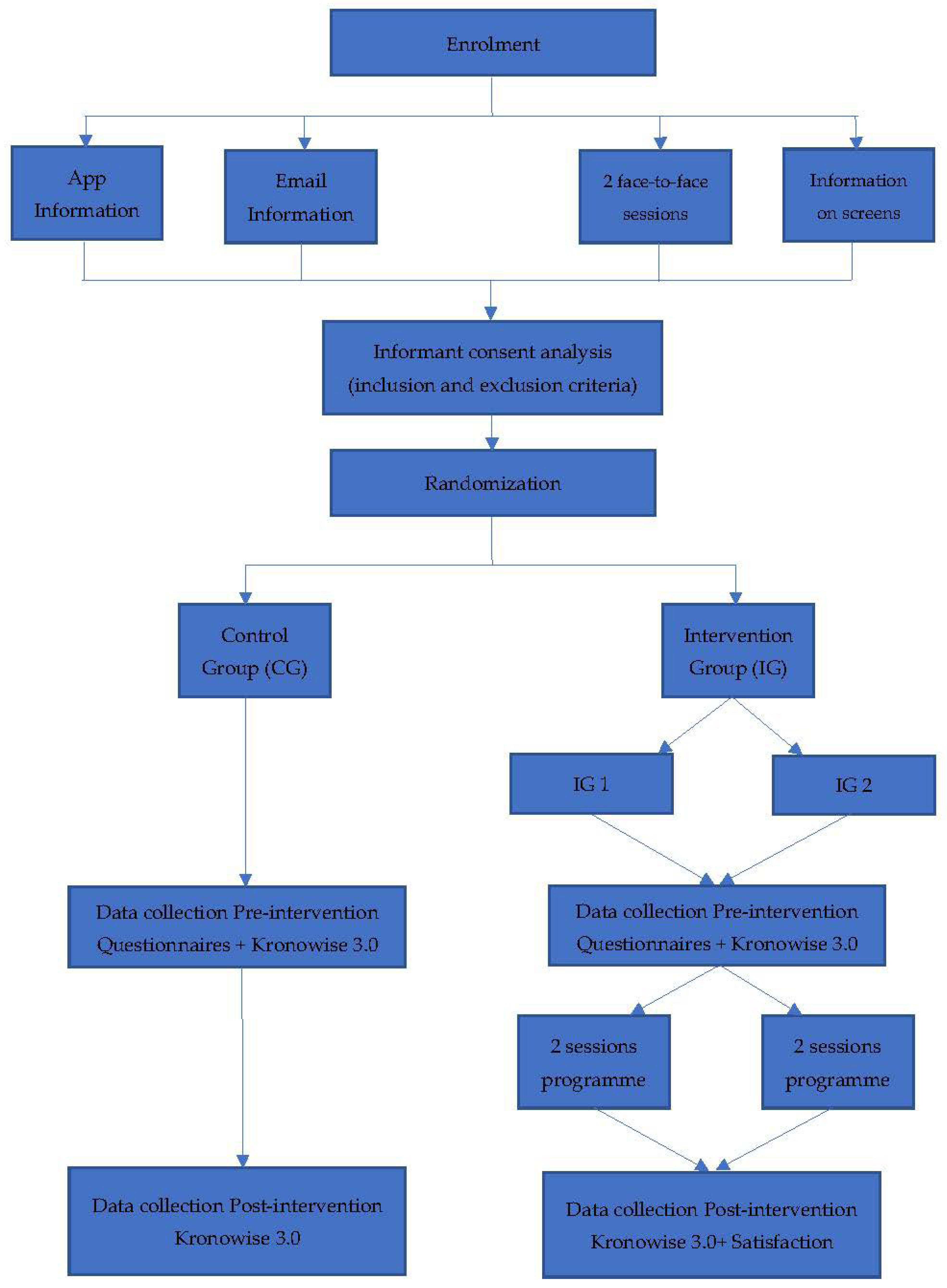
2.7. Study Procedure
Participants will be recruited over two weeks and via four channels. Information and informed consent that is mandatory for participation will be provided on the institution’s mobile app, in an institutional email and through two classroom sessions. Furthermore, information will be provided on informative posters on the electronic boards placed around the university premises.
After the two-week recruitment phase, all informed consent forms will be collected, and the inclusion/exclusion criteria applied. This will be conducted by a team researcher who will not take part in the intervention. Once the recruitment phase has been completed, students will be codified with their personal academic record number, and the intervention and control group will be randomly assigned. The intervention group will be divided into two groups (intervention group 1 and intervention group 2) according to session schedule preferences.
As shown in Figure 2, the following phases consist of the pre-intervention assessment for both groups, two behavioural–cognitive sessions with the intervention groups, and the post-intervention assessment.
Figure 2.
Study procedure.
Ten Kronowise 3.0 devices will be acquiring data a whole week for each student, so the different phases will be staggered for the groups. This means that the intervention protocol will last a total of 16 weeks (see Figure 2).
2.8. Data Analysis
For the statistical analysis, all variables will be coded by using IBM Statistics SPSS v.21 software (Chicago, USA) for Windows and revised twice. A protocol approach will be followed where missing data will not be included in the analysis.
All descriptive statistical parameters will be expressed as absolute (‘n’) and relative (‘%’) frequencies for each qualitative variable category. Quantitative variables will be analysed with the mean, median, and standard deviation to observe their behaviour at a confidence interval of 95%. Normal variable distribution will be analysed by using the Kolmogorov–Smirnov test with Shapiro–Wilk correction.
A repeated measures ANOVA will be used to compare mean differences between the intervention and control groups over time, considering the time–group interaction effect. The size of the effect will be analysed based on Cohen’s d [40]: 0–0.3 low, >0.3–0.8 moderate, and >0.8 large effect size. Any incomplete questionnaires will be excluded from the analysis. Results will be considered statistically significant when p < 0.05.
The PROCESS macro will be used to examine the mediating effects of sleep quality on the relationship between attending the sleep intervention or not. This analysis uses linear regression to estimate indirect effects according to Hayes and Rockwood’s methods recommended for clinical studies and focuses on two measurement moments [41]. Post-treatment scores will be added as mediators, and baseline scores for the outcome variables and mediators will be added to the models as covariates. Least-square path analysis will be used and the bootstrap confidence interval (5000 permutations) will be applied to estimate indirect effects.
3. Discussion
This research aims to promote healthier lifestyles in nursing undergraduate students. It is specifically addressed to target groups that share risk factors that can compromise sleep quality and to act at the educational level.
The main strength of this paper is the intervention itself, which is based on cognitive–behavioural therapy and improved understanding of the physiology of sleep. The physiology of sleep targets both the nervous structures involved in sleep and the self-knowledge of sleep patterns and sleep hygiene strategies, which are the cornerstones of the intervention [42]. It combines aspects to promote a cognitive process that consolidates the development of everyday life skills, providing positive patterns for healthy sleep. This intervention may be the first step to develop future studies with application in nurses to improve sleep disorders or work–life balance [43].
The assessment consists of objective and subjective components for a whole comprehensive approach to improve sleep quality. More specifically, the use of a TAP tool, validated as an ambulatory test using a wrist device vs. polysomnography, is an innovative added value of this study, as it will provide reliable, complete results on how the intervention affects sleep quality [35].
Lastly, the methodological design of the controlled clinical trial is crucial in this type of study to guarantee results on the effectiveness of the intervention.
Aside from the strengths already mentioned, other limitations should also be noted. First, the sample size may fall short of capturing differences between groups. However, the lack of prior studies and the complexity of developing the study depending on available devices, means that obtaining pilot study results will be enriching to analyse intervention barriers and facilitators for large-scale future implementation.
Additionally, we cannot guarantee a possible type two error, as randomization will be individual, and there may be contamination between the control and intervention groups as they interact during their studies.
Last, Kronowise 3.0 devices are highly useful for assessing the study despite their limited availability and cost. However, developing this pilot study will provide preliminary data which is crucial to apply for national or international external project funding to sustain the cost involved for interventions on a larger scale.
4. Conclusions
The methodological design of this study supports interventions that can favour better sleep quality in university nursing students. The intervention is a novel strategy combining cognitive learning about sleep as a physiological process, the use of technological devices to monitor sleep parameters, and addressing students’ knowledge about their individual habits through cognitive behavioural therapy. The research to be conducted using this protocol aims to demonstrate the positive effect of such an intervention on sleep quality in nursing students.
Author Contributions
C.R.-Z. and D.P.-M. are responsible for study design, conceptualization, and supervision. C.R.-Z., D.P.-M. and C.A.-N. are responsible for data management, writing article, and design. B.G.-I. and M.R.-L. are responsible for review and editing. C.R.-Z. and D.P.-M. are responsible for software and methodology. C.R.-Z., D.P.-M. and C.A.-N. are responsible for data collection. D.P.-M. and M.R.-L. are responsible for funding acquisition. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Camilo José Cela University.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of Camilo José Cela University (code: 06-22-UCJC-Sleep, approved on 23 March 2022).
Informed Consent Statement
Informed consent will be obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tembo, A.C.; Parker, V. Factors that impact on sleep in intensive care patients. Intensive Crit. Care Nurs. 2009, 25, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Yi, H.; Shin, K.; Shin, C. Development of the sleep quality scale. J. Sleep Res. 2006, 15, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Peltzer, K.; Pengpid, S. Sleep duration and health correlates among university students in 26 countries. Psychol. Health Med. 2016, 21, 208–220. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.L.; Davis, J.E.; Corbett, C.F. Sleep quality: An evolutionary concept analysis. Nurs. Forum 2002, 57, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.; Wickwire, E.M.; Hirshkowitz, M.; Albert, S.M.; Avidan, A.; Daly, F.J.; Vitiello, V. National Sleep Foundation’s sleep quality recommendations: First report. Sleep Health 2017, 3, 6–19. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.I.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Silva, M.; Chaves, C.; Duarte, J.; Amaral, O.; Ferreira, M. Sleep quality determinants among nursing students. Procedia-Soc. Behav. Sci. 2016, 217, 999–1007. [Google Scholar] [CrossRef]
- Yilmaz, D.; Tanrikulu, F.; Dikmen, Y. Research on sleep quality and the factors affecting the sleep quality of the nursing students. Curr. Health Sci. J. 2017, 43, 20–24. [Google Scholar] [CrossRef]
- Lack, L.C. Delayed sleep and sleep loss in university students. J. Am. Coll. Health 1986, 35, 105–110. [Google Scholar] [CrossRef]
- Brown, F.C.; Buboltz, W.C., Jr.; Soper, B. Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behav. Med. 2002, 28, 33–38. [Google Scholar] [CrossRef]
- Thorpy, M.J.; Korman, E.; Spielman, A.J.; Glovinsky, P.B. Delayed sleep phase syndrome in adolescents. J. Adolesc. Health Care 1988, 9, 22–27. [Google Scholar] [CrossRef]
- Curcio, G.; Ferrara, M.; Gennaro, L. Sleep loss, learning capacity and academic performance. Sleep Med. Rev. 2006, 10, 323–337. [Google Scholar] [CrossRef]
- Mattos, T.C.; Figueiredo, M.M.; Girnos, J.; De Faria, A.L.; De Almeida, E.F. Sleep quality and chronotype of nursing students. Acta Paul. Enferm. 2016, 29, 658–663. [Google Scholar] [CrossRef][Green Version]
- Benavente, S.B.T.; Silva, R.M.D.; Higashi, A.B.; Guido, L.D.A.; Costa, A.L.S. Influence of stress factors and socio-demographic characteristics on the sleep quality of nursing students. Rev. Esc. Enferm. USP 2014, 48, 514–520. [Google Scholar] [CrossRef]
- Oner, H.; Ustun, B. The Stress Sources of Nursing Students. Educ. Sci. Theory Pract. 2013, 13, 760–766. [Google Scholar] [CrossRef]
- Orzech, K.M.; Salafsky, D.B.; Hamilton, L.A. The state of sleep among college students at a Large Public University. J. Am. Coll. Health 2011, 59, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Timmins, F.; Kaliszer, M. Aspects of nurse education programmes that frequently cause stress to nursing students: Fact-finding sample survey. Nurse Educ. Today 2002, 22, 203–211. [Google Scholar] [CrossRef]
- Chan, C.K.L.; So, W.K.W.; Fong, D.Y.T. Hong Kong baccalaureate nursing students’ stress and their coping strategies in clinical practice. J. Prof. Nurs. 2009, 25, 307–313. [Google Scholar] [CrossRef]
- Murawski, B.; Wade, L.; Plotnikoff, R.C.; Lubans DRDuncan, M.J. A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Med. Rev. 2018, 40, 160–169. [Google Scholar] [CrossRef]
- Friedrich, A.; Schlarb, A.A. Let’s talk about sleep: A systematic review of psychological interventions to improve sleep in college students. J. Sleep Res. 2018, 27, 4–22. [Google Scholar] [CrossRef]
- Griggs, S.; Conley, S.; Batten, J.; Grey, M. A systematic review and meta-analysis of behavioral sleep interventions for adolescents and emerging adults. Sleep Med. Rev. 2020, 54, 101356. [Google Scholar] [CrossRef] [PubMed]
- Blazquez, A.; Martinez, A.; Salazar, F.J.; Rol, M.A.; Madrid, J.A. Wrist skin temperature, motor activity, and body position as determinants of the circadian pattern of blood pressure. Chronobiol. Int. 2012, 29, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Krauchi, K.; Deboer, T. The interrelationship between sleep regulation and thermoregulation. Front. Biosci. 2010, 15, 604–625. [Google Scholar] [CrossRef]
- Ortiz, E.; Martinez, A.; Albares, J.; Segarra, F.; Campos, M.; Estivill, E.; Madrid, J.A. Ambulatory circadian monitoring (ACM) based on thermometry, motor activity and body position (TAP): A comparison with polysomnography. Physiol. Behav. 2014, 126, 30–38. [Google Scholar] [CrossRef]
- Murtagh, D.R.; Greenwood, K.M. Identifying effective psychological treatments for insomnia: A meta-analysis. J. Consult. Clin. Psychol. 1995, 63, 79–89. [Google Scholar] [CrossRef]
- Blake, M.J.; Sheeber, L.B.; Youssef, G.J.; Raniti, M.B.; Allen, N.B. Systematic review and meta-analysis of adolescent cognitive–behavioral Sleep interventions. Clin. Child Fam. Psychol. Rev. 2017, 20, 227–249. [Google Scholar] [CrossRef]
- Edinger, J.D.; Means, M.K. Cognitive-behavioral therapy for primary insomnia. Clin. Psychol. Rev. 2005, 25, 539–558. [Google Scholar] [CrossRef]
- Irish, L.A.; Kline, C.E.; Gunn, H.E.; Buysse, D.J.; Hall, M.H. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med. Rev. 2015, 22, 23–36. [Google Scholar] [CrossRef]
- Kryger, M.H.; Roth, T.; Dement, W.C. Principles and Practice of Sleep Medicine, 5th ed.; Elsevier: Amsterdam, The Netherlands, 2010. [Google Scholar] [CrossRef]
- Parker, K.P.; Bliwise, D.L.; Ribeiro, M.; Jain, S.R.; Vena, C.I.; Kohles-Baker, M.K.; Rogatko, A.; Xu, Z.; Harris, W.B. Sleep/wake patterns of individuals with advanced cancer measured by ambulatory polysomnography. J. Clin. Oncol. 2008, 26, 2464–2472. [Google Scholar] [CrossRef]
- Chae, Y.R.; Choi, D.H.; Yu, S.J. Predictors of poor sleep quality among nursing students. J. Korean Biol. Nurs. Sci. 2014, 16, 98–104. [Google Scholar] [CrossRef][Green Version]
- Chan, A.W.; Tetzlaff, J.M.; Gøtzsche, P.C.; Altman, D.G.; Mann, H.; Berlin, J.A.; Moher, D. SPIRIT 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ 2013, 8, 346. [Google Scholar] [CrossRef]
- Allen, J.R.; John, C. Sample size calculation for two independent groups: A useful rule of thumb. Proc. Singap. Healthc. 2011, 20, 138–140. [Google Scholar] [CrossRef]
- Chi, M.T.; Wylie, R. The ICAP framework: Linking cognitive engagement to active learning outcomes. Educ. Psychol. 2014, 49, 219–243. [Google Scholar] [CrossRef]
- Ortiz, E.; Martinez, A.; Campos, M.; Rol, M.A.; Madrid, J.A. A new integrated variable based on thermometry, actimetry and body position (TAP) to evaluate circadian system status in humans. PLoS Comput. Biol. 2010, 6, e1000996. [Google Scholar] [CrossRef]
- Madrid, C.J.; Puertas, F.J.; Escamilla, F.; Campos, M.; Ruiz Abellan, F.; Rol, M.A.; Madrid, J.A. Validation of a device for the ambulatory monitoring of sleep patterns: A pilot study on Parkinson’s disease. Front. Neurol. 2019, 10, 356. [Google Scholar] [CrossRef]
- De la Vega, R.; Tomé-Pires, C.; Solé, E.; Racine, M.; Castarlenas, E.; Jensen, M.P.; Miró, J. The Pittsburgh Sleep Quality Index: Validity and factor structure in young people. Psychol. Assess. 2015, 27, e22–e27. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.; Marshall, A.; Sjöström, M.; Bauman, A.; Booth, M.; Ainsworth, B. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sport. Exerc. 2013, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Azpeleta, C.; Santos, P.; Sobrado, A.; Lesmes, M.; Gal, B. Forcing a change: A learn-by-doing workshop on circadian rhythms to understand the complexities of human physiology. Adv. Physiol. Educ. 2021, 45, 437–444. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717e731. [Google Scholar] [CrossRef]
- Mitchell, L.J.; Bisdounis, L.; Ballesio, A.; Omlin, X.; Kyle, S.D. The impact of cognitive behavioural therapy for insomnia on objective sleep parameters: A meta-analysis and systematic review. Sleep Med. Rev. 2019, 47, 90–102. [Google Scholar] [CrossRef]
- Shiffer, D.; Minonzio, M.; Dipaola, F.; Bertola, M.; Zamuner, A.R.; Dalla Vecchia, L.A.; Barbic, F. Effects of clockwise and counterclockwise job shift work rotation on sleep and work-life balance on hospital nurses. Int. J. Environ. Res. Public Health 2018, 15, 2038. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).